Abstract
Papular acantholytic dyskeratosis (PAD), also known as acantholytic dermatosis of the vulvocrural (or anogenital) area, is an uncommon eruption reported predominantly in women. This entity manifests with pruritic papules in the groin/anogenital area and less commonly on the chest. The pathobiology of PAD is uncertain. A 62-year old woman presented with multiple verrucous-appearing lesions in the groin and on the chest showing acantholytic dyskeratosis on histopathology. Given histological similarity of these PAD lesions to Darier disease (DD) due to inherited ATP2A2 mutation, we screened affected and normal tissue and peripheral blood in our patient for mutations in ATP2A2. We found an identical ATP2A2 p.706D>N mutation in multiple independent PAD lesions that was not present in uninvolved skin or peripheral blood DNA. These findings establish somatic mosaicism of ATP2A2 mutations as a genetic cause for PAD.
Introduction
Papular acantholytic dyskeratosis (PAD), also known as acantholytic dermatosis of the vulvocrural (or anogenital) area is an uncommon and frequently misdiagnosed eruption seen more commonly in women than in men. Typically, patients present as adults with pruritic papules in the groin area; some patients also report lesions on the chest. Many are diagnosed on clinical grounds as having genital warts; due to inconsistent history and/or failure to respond appropriately to treatment, a biopsy leads to the alternative diagnosis of PAD. Although there has been speculation about a possible relationship to the autosomal dominant genodermatoses of DD and Hailey-Hailey disease (HHD), comprehensive genetic testing of affected and unaffected tissue in addition to blood has not previously been performed in a patient with PAD.
Report of a Patient
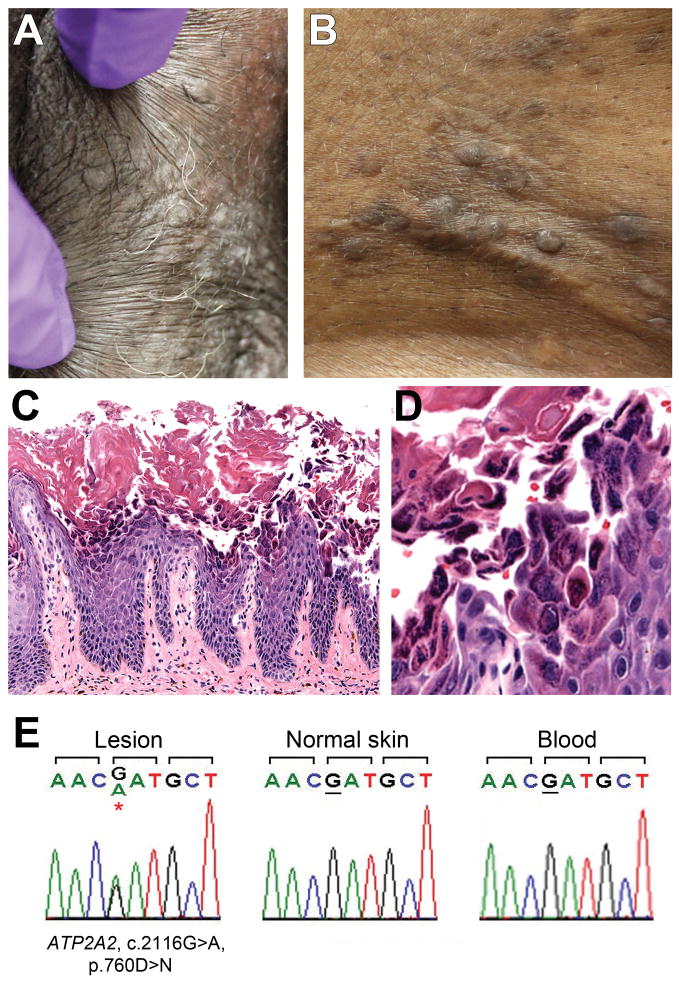
A 62 year-old woman reported a greater than five-year history of itchy bumps in the groin. A family history was negative for similar lesions. On examination she had multiple, bilateral, skin-coloured papules on the mons pubis, external labia, inguinal folds and upper medial thighs with fewer, similar papules on the central chest and inframammary areas (Fig. 1). The papules were scattered and focally aggregated, but were not arrayed in a linear or Blaschkoid pattern. The remainder of the exam was normal, including nails, mucosae, palms and soles. Initial biopsies taken for diagnosis from the groin showed acantholytic dyskeratosis. Human papilloma virus (HPV) was not detected by in situ hybridization with a panel of common HPV types.
Figure 1.
Clinical, histopathological and sequencing findings.
Top panel: Skin-colored papules on the left external labia majora (a) and central chest (b). Central panel: Hematoxylin and eosin stains of lesional tissue at low power (c) and high power (d) show acanthosis and papillomatosis, with acantholysis and dyskeratosis of keratinocytes. Lower panel: Chromatograms (e) demonstrate mutation of ATP2A2 in affected epidermis with wild-type sequence in unaffected epidermis and peripheral blood.
Materials and Methods
Under a protocol approved by the Yale University Human Research Protection Program, seven biopsies of separate verrucous papules from the groin (including labia majora, inguinal crease, upper thigh) and one from the chest were obtained; a biopsy of normal skin was taken from the low abdomen/mons pubis. The chest sample was formalin-fixed, paraffin-embedded; the remaining eight biopsies were snap-frozen and embedded in Optimal Cutting Temperature compound. All samples were evaluated by light microscopy. Six samples with the most marked histopathological changes were selected for laser-dissection of affected epidermis and a portion of dermis as a control; epidermis was also laser-dissected from the biopsy of normal skin. DNA was prepared from these samples, whole genome amplification performed, followed by PCR and sequencing of the ATP2A2 gene in parallel with DNA from blood.
Results
Evaluation by light microscopy of the papular lesions from the groin and chest revealed epidermal acanthosis with patchy acantholysis and scattered dyskeratotic cells (Fig. 1). No epidermal abnormalities were seen in the biopsy of normal skin.
Sequencing of six samples of lesional tissue revealed a missense mutation in exon 15 of ATP2A2 not present in peripheral blood or normal tissue (c.2116G>A, p.706D>N) (Fig. 1). This mutation occurs at a residue which is 100% conserved in vertebrates.
Discussion
PAD is an under-recognized entity easily mistaken for condyloma because of its verrucous appearance and predilection for the genital area.1 Misdiagnosis can cause significant patient distress.
There are at least 16 reports of compatible cases in adult female patients,1–16 in which multiple lesions were reported as showing both acantholysis and dyskeratosis. In an additional 8 women, the lesions were solitary and therefore are of uncertain relevance.5, 17, 18 One report described positive direct immunofluorescence, in contrast to other published cases.19 There are also 6 similar reports in men,20–23 and 3 in children.24–26 None of these reports indicated a positive family history. These cases have been published under various names, many as papular acantholytic dyskeratosis/dermatosis, others as acantholytic dermatosis of the vulvocrural/anogenital area; some cases have been published under the names of histopathologically similar entities such as multiple warty dyskeratomas,11 with subsequent commentary suggesting reclassification into the PAD spectrum.12 Lesions have been reported on the genital mucosa, external genitalia, and surrounding skin of the groin and upper thigh. Two reports also involved the chest,6, 7 prompting the suggested alternate terminology “intertriginous acantholytic dermatosis,”7 although this name has not been adopted. The findings in our patient were similar to these latter reports, with papules both in the groin and on the chest. Although a relationship to DD and HHD has been proposed, comprehensive testing of affected and unaffected tissue in addition to blood has not previously been performed. The results of this study indicate that somatic mosaic mutations in ATP2A2, the gene encoding the sarco-endoplasmic reticulum calcium-pumping ATPase (type 2) mutated in DD, can result in the clinical phenotype referred to as PAD.
The mutation identified in our patient was previously reported in an Italian patient with germline DD manifesting as acrokeratosis verruciformis (AKV) with nail changes.27 There is evidence that AKV and DD are allelic disorders with variable expression of overlapping features.28 Mutations in the same codon of ATP2A2 have resulted in clinical phenotypes of AKV and DD in separate individuals.29 The p.706D>N mutation falls within a domain regulating enzymatic phosphorylation required for calcium conductance and is known to reduce phosphorylation rate and calcium flux.30 Aberrant calcium flux has been shown to cause loss of epidermal integrity, a hallmark of DD and PAD.
Mutations resulting in segmental disease occur spontaneously during embryogenesis. This study indicates that mosaic mutation in ATP2A2 can cause PAD. Timing of the mutational event in embryogenesis likely determines the distribution and extent of tissue involvement. Study of a patient with segmental DD revealed that mutation in 37% of cells within a region of skin was sufficient to produce cutaneous manifestations; the minimum threshold is expected to be slightly less.31 Our findings of variable percentages of mutated DNA within samples showing normal or affected histopathology correlate with this concept and may partly represent admixture with normal tissue given the sampling approach employed.
It is not established why there is a predilection for women and for the genital area in PAD; however, a moist, high-friction environment has been suggested as a predisposing factor.5 It stands to reason that conditions known to exacerbate DD could promote expression of the disease in a mosaic patient. The age of PAD onset/manifestation reported in the literature is variable, with multiple examples in each decade of life, including patients in their 60s. Similarly, cases of late “onset” germline DD, including at 50 and 75 years of age29, 32 have been reported.
Treatment of PAD is challenging. Topical and oral retinoids are favored in case reports.5, 24, 33 This observation is supported by their known utility in DD. Ablative treatments including lasers have shown success;5, 9, 14 this might be explained by preferential healing of treated areas with a predominance of wild-type keratinocytes.
There are reports where a relationship to HHD has been favored over DD.33–35 Predominantly HHD-like histopathology has been seen in a minority of cases.22, 35–38 Mutation in the ATP2C1 gene (affected in HHD) has been demonstrated in tissue from a patient with an extensive vulvocrural eruption showing HHD-like pathology; however sequencing of blood was not performed, therefore, it is not possible to exclude a constitutional mutation in this case.33 Similarly, a mother and daughter each with adult onset of pruritic genitoperineal papules, were found to harbour identical heterozygous mutations in the ATP2C1 gene, presumably germline mutations in both patients.35 It remains possible, even probable, that mosaic forms of both DD and HHD (as well as formes frustes of these germline diseases) might eventuate in the clinical pattern currently recognized as PAD. The appearance of the pathology can help to guide the genetic evaluation of such cases.
We report a case of PAD demonstrating mosaic mutation of the gene affected in DD. Dermatologists and pathologists should be aware of this diagnosis and its genetic underpinnings. Histopathological examination of suggestive genital lesions is important to allow for appropriate patient counseling and treatment, including consideration that DD could be transmitted to offspring in whom the entire body could be affected..
Acknowledgments
Funding/Support: This study was supported in part by NIH training grant 5 T32 AR07016-34 (E.K.), a Doris Duke Charitable Clinical Scientist Development Award (K.C.), and NIH K08 AR056305 (K.C.).
We are indebted to Vincent Klump, clinical technologist (Yale University), for sharing his expert histotechnical skills, and to Anita Farhi, RN (Yale University), for her superb assistance in patient recruiting. No compensation was provided for their contributions.
Footnotes
Conflicts of interest/financial disclosures: None reported.
References
- 1.Browne F, Keane H, Walsh M, Maw R. Papular acantholytic dyskeratosis presenting as genital warts. Int J STD AIDS. 2007;18(12):867. doi: 10.1258/095646207782716938. [DOI] [PubMed] [Google Scholar]
- 2.Chorzelski TP, Kudejko J, Jablonska S. Is papular acantholytic dyskeratosis of the vulva a new entity? Am J Dermatopathol. 1984;6(6):557. doi: 10.1097/00000372-198412000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Coppola G, Muscardin LM, Piazza P. Papular acantholytic dyskeratosis. Am J Dermatopathol. 1986;8(4):364. doi: 10.1097/00000372-198608000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Barrett JF, Murray LA, MacDonald HN. Darier’s disease localized to the vulva. Case report. Br J Obstet Gynaecol. 1989;96(8):997. doi: 10.1111/j.1471-0528.1989.tb03363.x. [DOI] [PubMed] [Google Scholar]
- 5.Cooper PH. Acantholytic dermatosis localized to the vulvocrural area. J Cutan Pathol. 1989;16(2):81. doi: 10.1111/j.1600-0560.1989.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 6.Van Joost T, Vuzevski VD, Tank B, Menke HE. Benign persistent papular acantholytic and dyskeratotic eruption: a case report and review of the literature. Br J Dermatol. 1991;124(1):92. doi: 10.1111/j.1365-2133.1991.tb03290.x. [DOI] [PubMed] [Google Scholar]
- 7.Leverkus M, Rose C, Bröcker EB, Hamm H. Intertriginous acantholytic dyskeratosis: abortive form of Darier disease or a specific entity? Hautarzt. 1999;50(10):733. doi: 10.1007/s001050051059. [DOI] [PubMed] [Google Scholar]
- 8.Peştereli HE, Karaveli S, Oztekin S, Zorlu G. Benign persistent papular acantholytic and dyskeratotic eruption of the vulva: a case report. Int J Gynecol Pathol. 2000;19(4):374. doi: 10.1097/00004347-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Bell HK, Farrar CW, Curley RK. Papular acantholytic dyskeratosis of the vulva. Clin Exp Dermatol. 2001;26(5):386. doi: 10.1046/j.1365-2230.2001.00840.x. [DOI] [PubMed] [Google Scholar]
- 10.Krishnan RS, Ledbetter LS, Reed JA, Hsu S. Acantholytic dermatosis of the vulvocrural area. Cutis. 2001;67(3):217. [PubMed] [Google Scholar]
- 11.Abramovits W, Abdelmalek N. Treatment of warty dyskeratoma with tazarotenic acid. J Am Acad Dermatol. 2002;46(2 Suppl Case Reports):S4. doi: 10.1067/mjd.2002.104963. [DOI] [PubMed] [Google Scholar]
- 12.Hsu S, Ledbetter LS, Krishnan RS, Reed JA. Acantholytic dermatosis of the vulvocrural area. J Am Acad Dermatol. 2003;48(4):638. doi: 10.1067/mjd.2003.242. [DOI] [PubMed] [Google Scholar]
- 13.Roh MR, Choi YJ, Lee KG. Papular acantholytic dyskeratosis of the vulva. J Dermatol. 2009;36(7):427. doi: 10.1111/j.1346-8138.2009.00660.x. [DOI] [PubMed] [Google Scholar]
- 14.Dittmer CJ, Hornemann A, Rose C, Diedrich K, Thill M. Successful laser therapy of a papular acantholytic dyskeratosis of the vulva: case report and review of literature. Arch Gynecol Obstet. 2010;281(4):723. doi: 10.1007/s00404-009-1313-8. [DOI] [PubMed] [Google Scholar]
- 15.Chen AF, Stirling L, Spock C, Milikowski C. Numerous white papules on the vulva. Arch Dermatol. 2012;148(6):755. [PubMed] [Google Scholar]
- 16.Montis-Palos MC, Acebo-Marinas E, Caton-Santaren B, Soloeta-Arechavala R. Papular acantholytic dermatosis in the genito-crural region: a localized form of Darier disease or Hailey-Hailey disease? Actas Dermosifiliogr. 2013;104(2):170. doi: 10.1016/j.ad.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 17.Evron S, Leviatan A, Okon E. Familial benign chronic pemphigus appearing as leukoplakia of the vulva. Int J Dermatol. 1984;23(8):556. doi: 10.1111/j.1365-4362.1984.tb04212.x. [DOI] [PubMed] [Google Scholar]
- 18.Duray PH, Merino MJ, Axiotis C. Warty dyskeratoma of the vulva. Int J Gynecol Pathol. 1983;2(3):286. doi: 10.1097/00004347-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Güneş AT, Ilknur T, Pabuççuoğlu U, Lebe B, Altiner DD. Papular acantholytic dyskeratosis of the anogenital area with positive direct immunofluorescence results. Clin Exp Dermatol. 2007;32(3):301. doi: 10.1111/j.1365-2230.2007.02385.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee SH, Jang JG. Papular acantholytic dyskeratosis of the genitalia. J Dermatol. 1989;16(4):312. doi: 10.1111/j.1346-8138.1989.tb01270.x. [DOI] [PubMed] [Google Scholar]
- 21.Wong TY, Mihm MC. Acantholytic dermatosis localized to genitalia and crural areas of male patients: a report of three cases. J Cutan Pathol. 1994;21(1):27. doi: 10.1111/j.1600-0560.1994.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 22.Verma SB. Papular acantholytic dyskeratosis localized to the perineal and perianal area in a young male. Indian J Dermatol. 2013;58(5):393. doi: 10.4103/0019-5154.117317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xiao XM, Xu HX, Xu XL, et al. Papular acantholytic dermatosis of the anogenital areas. Eur J Dermatol. 2013;23(6):886. doi: 10.1684/ejd.2013.2174. [DOI] [PubMed] [Google Scholar]
- 24.Salopek TG, Krol A, Jimbow K. Case report of Darier disease localized to the vulva in a 5-year-old girl. Pediatr Dermatol. 1993;10(2):146. doi: 10.1111/j.1525-1470.1993.tb00042.x. [DOI] [PubMed] [Google Scholar]
- 25.Sáenz AM, Cirocco A, Avendaño M, González F, Sardi JR. Papular acantholytic dyskeratosis of the vulva. Pediatr Dermatol. 2005;22(3):237. doi: 10.1111/j.1525-1470.2005.22312.x. [DOI] [PubMed] [Google Scholar]
- 26.Wang L, Yang XC, Hao F, Mei Y, Ye QY. Papular acantholytic dyskeratosis of the vulva. Eur J Dermatol. 2009;19(4):402. doi: 10.1684/ejd.2009.0697. [DOI] [PubMed] [Google Scholar]
- 27.Pedace L, Barboni L, Pozzetto E, et al. Molecular characterization of 11 Italian patients with Darier disease. Eur J Dermatol. 2011;21(3):334. doi: 10.1684/ejd.2011.1339. [DOI] [PubMed] [Google Scholar]
- 28.Bergman R, Sezin T, Indelman M, Helou WA, Avitan-Hersh E. Acrokeratosis verruciformis of Hopf showing P602L mutation in ATP2A2 and overlapping histopathological features with Darier disease. Am J Dermatopathol. 2012;34(6):597. doi: 10.1097/DAD.0b013e31823f9194. [DOI] [PubMed] [Google Scholar]
- 29.Ueo D, Hamada T, Hashimoto T, Hatano Y, Okamoto O, Fujiwara S. Late-onset Darier’s disease due to a novel missense mutation in the ATP2A2 gene: a different missense mutation affecting the same codon has been previously reported in acrokeratosis verruciformis. J Dermatol. 2013;40(4):280. doi: 10.1111/1346-8138.12058. [DOI] [PubMed] [Google Scholar]
- 30.Dode L, Andersen JP, Leslie N, Dhitavat J, Vilsen B, Hovnanian A. Dissection of the functional differences between sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA) 1 and 2 isoforms and characterization of Darier disease (SERCA2) mutants by steady-state and transient kinetic analyses. J Biol Chem. 2003;278(48):47877. doi: 10.1074/jbc.M306784200. [DOI] [PubMed] [Google Scholar]
- 31.Harboe TL, Willems P, Jespersgaard C, Mølgaard Poulsen ML, Sørensen FB, Bisgaard ML. Mosaicism in segmental Darier disease: an in-depth molecular analysis quantifying proportions of mutated alleles in various tissues. Dermatology. 2011;222(4):292. doi: 10.1159/000328404. [DOI] [PubMed] [Google Scholar]
- 32.Miyauchi Y, Daiho T, Yamasaki K, et al. Comprehensive analysis of expression and function of 51 sarco(endo)plasmic reticulum Ca2+-ATPase mutants associated with Darier disease. J Biol Chem. 2006;281(32):22882. doi: 10.1074/jbc.M601966200. [DOI] [PubMed] [Google Scholar]
- 33.Lipoff JB, Mudgil AV, Young S, Chu P, Cohen SR. Acantholytic dermatosis of the crural folds with ATP2C1 mutation is a possible variant of Hailey-Hailey Disease. J Cutan Med Surg. 2009;13(3):151. doi: 10.2310/7750.2008.08005. [DOI] [PubMed] [Google Scholar]
- 34.Langenberg A, Berger TG, Cardelli M, Rodman OG, Estes S, Barron DR. Genital benign chronic pemphigus (Hailey-Hailey disease) presenting as condylomas. J Am Acad Dermatol. 1992;26(6):951. doi: 10.1016/0190-9622(92)70140-b. [DOI] [PubMed] [Google Scholar]
- 35.Pernet C, Bessis D, Savignac M, Tron E, Guillot B, Hovnanian A. Genitoperineal papular acantholytic dyskeratosis is allelic to Hailey-Hailey disease. Br J Dermatol. 2012;167(1):210. doi: 10.1111/j.1365-2133.2012.10810.x. [DOI] [PubMed] [Google Scholar]
- 36.Hazelrigg DE, Stoller LJ. Isolated familial benign chronic pemphigus. Arch Dermatol. 1977;113(9):1302. [PubMed] [Google Scholar]
- 37.King DT, Hirose FM, King LA. Simultaneous occurrence of familial benign chronic pemphigus (Hailey-Hailey disease) and syringoma on the vulva. Arch Dermatol. 1978;114(5):801. doi: 10.1001/archderm.1978.01640170095037. [DOI] [PubMed] [Google Scholar]
- 38.van der Putte SC, Oey HB, Storm I. Papular acantholytic dyskeratosis of the penis. Am J Dermatopathol. 1986;8(4):365. doi: 10.1097/00000372-198608000-00022. [DOI] [PubMed] [Google Scholar]