Abstract
Background
The white coat effect (defined as the difference between blood pressure [BP] measurements taken at the physician’s office and those taken outside the office) is an important determinant of misdiagnosis of hypertension, but little is known about the mechanisms underlying this phenomenon. We tested the hypothesis that the white coat effect may be a conditioned response as opposed to a manifestation of general anxiety.
Methods
A total of 238 patients in a hypertension clinic wore ambulatory blood pressure monitors on 3 separate days 1 month apart. At each clinic visit, BP readings were manually triggered in the waiting area and the examination room (in the presence and absence of the physician) and were compared with the mercury sphygmomanometer readings taken by the physician in the examination room. Patients completed trait and state anxiety measures before and after each BP assessment.
Results
A total of 35% of the sample was normotensive, and 9%, 37%, and 19% had white coat, sustained, and masked hypertension, respectively. The diagnostic category was associated with the state anxiety measure (F3,237 = 6.4, P < .001) but not with the trait anxiety measure. Patients with white coat hypertension had significantly higher state anxiety scores (t = 2.67, P < .01), with the greatest difference reported during the physician measurement. The same pattern was observed for BP changes, which generally paralleled the changes in state anxiety (t = 4.86, P < .002 for systolic BP; t = 3.51, P < .002 for diastolic BP).
Conclusions
These findings support our hypothesis that the white coat effect is a conditioned response. The BP measurements taken by physicians appear to exacerbate the white coat effect more than other means. This problem could be addressed with uniform use of automated BP devices in office settings.
Physicians’ offices are the venues in which most interactions with patients occur, including the measurement of blood pressure (BP) and the delivery of diagnoses. The surroundings in which these transactions occur hold great emotional import for some patients, who may have, at one time or another, received frightening information about their health, increasing their anxiety and BP during subsequent visits and hence biasing the assessment of their hypertension status. The introduction of ambulatory BP monitoring has made it clear that the traditionally measured office BP is usually somewhat higher than the pressure during the rest of the day, particularly in patients who have been diagnosed with hypertension or labeled as being hypertensive.1 It is also well established that ambulatory BP predicts cardiovascular events better than office BP.2–4 If the office BP readings are in the hypertensive range and the ambulatory BP is normal, this leads to a diagnosis of white coat hypertension, which occurs in 10% to 20% of hypertensive patients.5,6 Although controversial, this condition may be considered benign because the risk of cardiovascular disease in this group of patients is comparable to that in normotensive patients,5,7 and thus antihypertensive drug treatment is generally considered to be unnecessary. The white coat effect (defined as the difference between BP measurements taken at the physician’s office and those taken outside the office, using ambulatory monitoring) is, however, also strongly positive in most hypertensive patients and tends to increase with age.8 In contrast, in persons whose office BP is normal, the white coat effect is typically absent or negative,8 which may be explained by the fact that physical and mental activities are higher during normal daily activities than during office BP measurement. Alternatively, it suggests that, for some persons, the physician’s office has not become a stimulus cue for anxiety or, furthermore, may even represent a relaxing situation. Either or both of these possibilities may account for the phenomenon of masked hypertension (elevated ambulatory BP and normal office BP).9 Masked hypertension is estimated to occur in 10% to 20% of the general population9,10 (in contrast to white coat hypertension, which has a similar prevalence but only within the diagnosed hypertensive population, a much smaller group). Masked hypertension has been associated with target organ damage11 and elevated cardiovascular risk.9 However, it is usually not detected or treated. Because of the public health significance and treatment implications of these diagnostic categories, it is important to understand the underlying mechanisms that may lead to disagreements between in-office and out-of-office BP measurements.
The focus of the present study is on the mechanisms underlying the white coat effect, which is an important determinant of misdiagnosis. Thus, the purpose of this study is to investigate the causes of the disagreement observed between office and ambulatory BP measures.
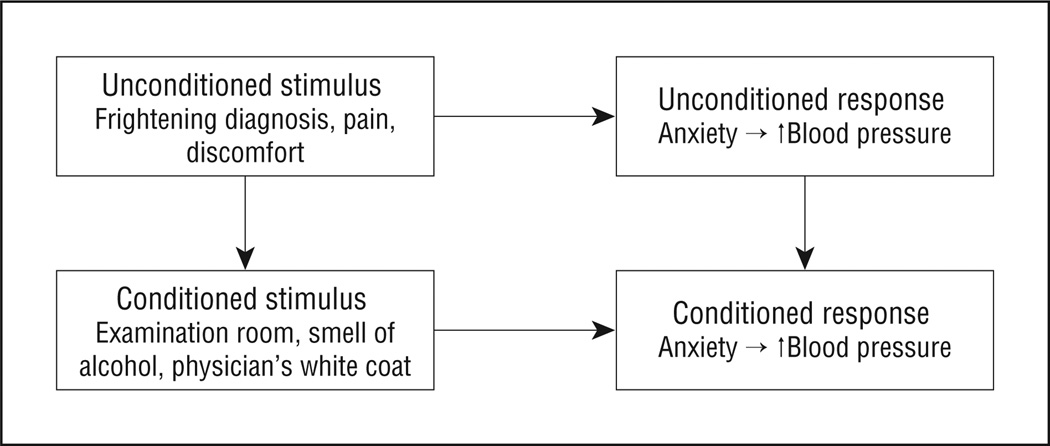
Two competing theories, related to patients’ anxiety levels in the physician’s office, have been put forth to explain the occurrence of white coat hypertension and the white coat effect. First, the generalized anxiety theory asserts that patients with a general, stable (ie, “trait”) tendency to be anxious are more likely to be diagnosed with white coat hypertension.12 Several studies,12–15 however, have failed to find a relationship between trait measures of anxiety and office BP. Second, the classical (or respondent) conditioning model provides a useful alternative model by which to understand the cause of the elevated office BP and the attendant risk of misdiagnosis. A classical conditioning model suggests that patients with white coat hypertension have been exposed to unpleasant experiences, such as unwelcome medical diagnoses and/or painful medical procedures (in the classical conditioning model, these are referred to as “unconditioned stimuli”), in 1 or more physicians’ offices, which may lead to transient anxiety and a concomitant BP increase (referred to as the “unconditioned response”).16–18 With repeated exposure, the cues associated with the unconditioned stimuli, for example, the physician’s white coat and the appearance of the examination room (which tends to be similar across medical offices), are all potential conditioned stimuli to the extent that they acquire the power to themselves elicit anxiety and elevated BP. Figure 1 shows the hypothesized classical conditioning process that may lead to white coat hypertension. An interesting example of conditioning is seen in patients with cancer undergoing chemotherapy. One consequence of this therapy is nausea, an unconditioned response. Several studies19 have reported that many such patients experience nausea in the period preceding their therapy, indicating that the nausea has become a conditioned response. It is only under specific conditions that the nausea occurs, however (in this case, represented by temporality and, possibly, the clinic milieu). We suggest that the classical conditioning model, compared with the general anxiety theory, provides a more useful explanation of the white coat effect.
Figure 1.
Schematic drawing of the hypothesized conditioning process that may lead to white coat hypertension. Upward arrow indicates increase.
Although both hypotheses specify anxiety as the cause of BP elevation in the physician’s office, the general anxiety hypothesis assumes that persons with higher trait anxiety would be expected to have elevated BP regardless of the setting, that is, both inside and outside the physician’s office. The conditioning hypothesis, in contrast, posits that the anxiety response is specific to a particular set of circumstances and thus predicts that BP measurements taken only under those circumstances will be elevated. If correct, this theory suggests that the reason that past studies have failed to find an association between anxiety and white coat hypertension is that they have failed to measure the anxiety that occurs in the specific situation in which the BP measurements are being taken.
A means of testing the conditioning vs anxiety hypotheses is provided by the duration of the BP elevation after the departure of the physician (the conditioned stimulus) from the examination room. A conditioning explanation can readily account for rapid BP changes as a function of a change in the stimulus conditions (eg, moving from a waiting room into an examination room); however, a general anxiety explanation cannot. If trait anxiety were the cause, the elevated level of anxiety throughout the situation would dominate compared with marked increases and decreases when moving from neutral to conditioned circumstances. Thus, the 2 mechanisms are differentiated by the time courses of the anxiety and the BP response.
METHODS
PATIENTS
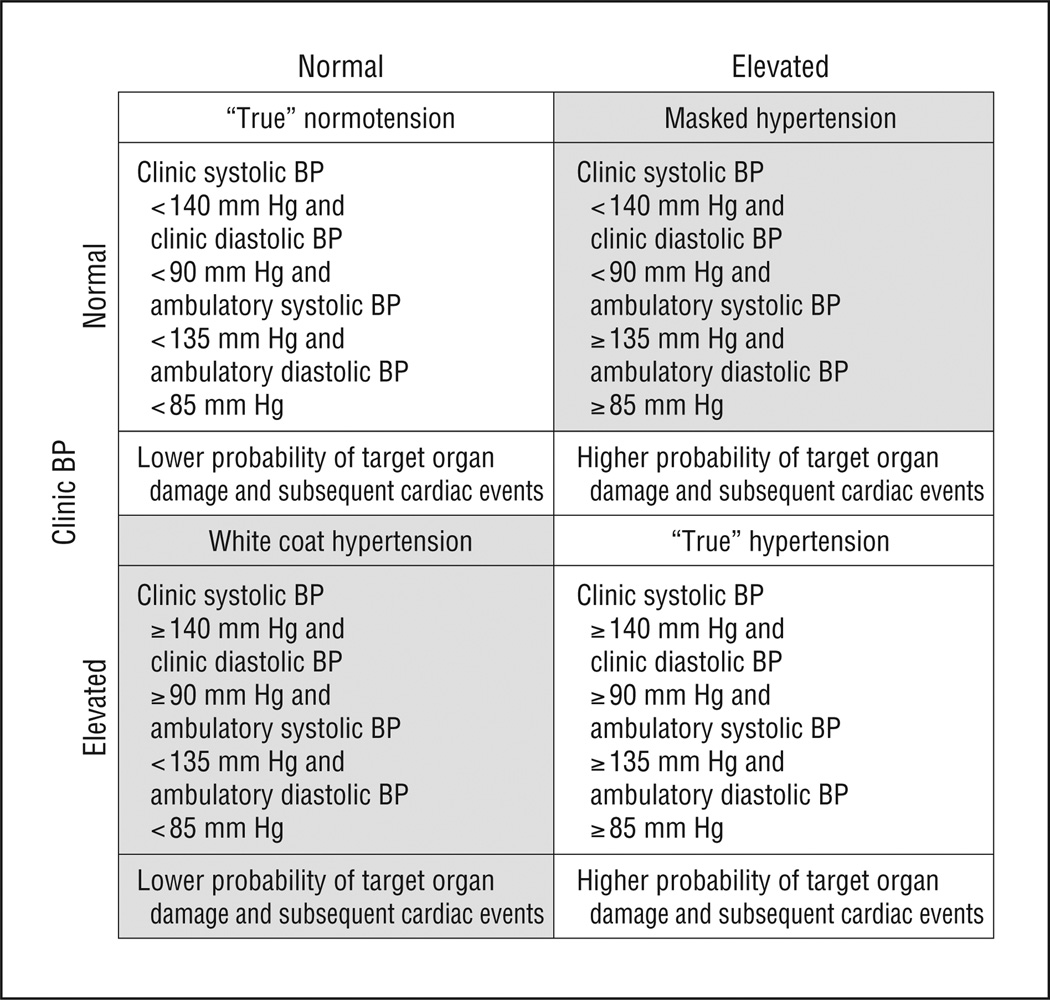
A total of 277 patients completed the study. Eligibility criteria included age of 18 to 80 years; willingness of the patient, with his/her physician’s permission, to stop taking antihypertensive medication for the 8-week study duration; no previous cardiovascular morbid event; no major medical problems other than hypertension; body mass index (calculated as weight in kilograms divided by height in meters squared) below 32.5; and English speaking. For study purposes, a diagnosis of hypertension was established only after participants had undergone 36-hour ambulatory BP monitoring. Based on office and ambulatory measurements, patients were categorized as normotensive (35%), sustained hypertensive (37%), white coat hypertensive (9%), or masked hypertensive (19%). Figure 2 shows the algorithm by which hypertension status was diagnosed, and Table 1 gives the sample’s demographic characteristics. The sample was drawn from physician referrals to the Weill Cornell Hypertension Center of New York Presbyterian Hospital and through media advertisements. Eligible patients were referred into the study by 3 participating physicians (T.G.P. and others) at the center, and the study procedures were approved by the hospital’s institutional review board.
Figure 2.
Diagnostic categories and associated target organ damage, based on the joint assessment of clinic and ambulatory blood pressure (BP).
Table 1.
Demographic Characteristics of the Diagnostic Groupsa
| Characteristic | Normotensive | White Coat Hypertensive | Sustained Hypertensive | Masked Hypertensive |
|---|---|---|---|---|
| Age, mean (SD), yb | 45.9 (13) (n = 85) | 56.3 (14) (n = 20) | 56.0 (13) (n = 90) | 52.2 (17) (n = 43) |
| BMI, mean (SD) | 26.7 (6) (n = 78) | 27.6 (6) (n = 19) | 27.1 (5) (n = 87) | 27.0 (5) (n = 40) |
| Race, No. (%) | ||||
| White, non-Hispanic | 38 (45) | 15 (75) | 58 (64) | 24 (56) |
| White, Hispanic | 8 (9) | 1 (5) | 6 (7) | 2 (5) |
| Black, non-Hispanic | 25 (29) | 3 (15) | 14 (15) | 11 (26) |
| Black, Hispanic | 3 (4) | 0 | 3 (3) | 2 (5) |
| Asian/Indian/Pacific Islander | 6 (7) | 1 (5) | 4 (4) | 3 (7) |
| Native American/Alaskan Native | 1 (1) | 0 | 0 | 0 |
| Other | 4 (5) | 0 | 6 (7) | 1 (2) |
| Total | 85 (100) | 20 (100) | 91 (100) | 43 (100) |
| Female, No. (%)c | 52 (62) | 14 (70) | 37 (41) | 20 (46) |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Data on age missing from 3 study participants; data on BMI missing from 2 study participants.
P < .001 (these variables are included as covariates in the analyses).
P < .05.
PROCEDURE
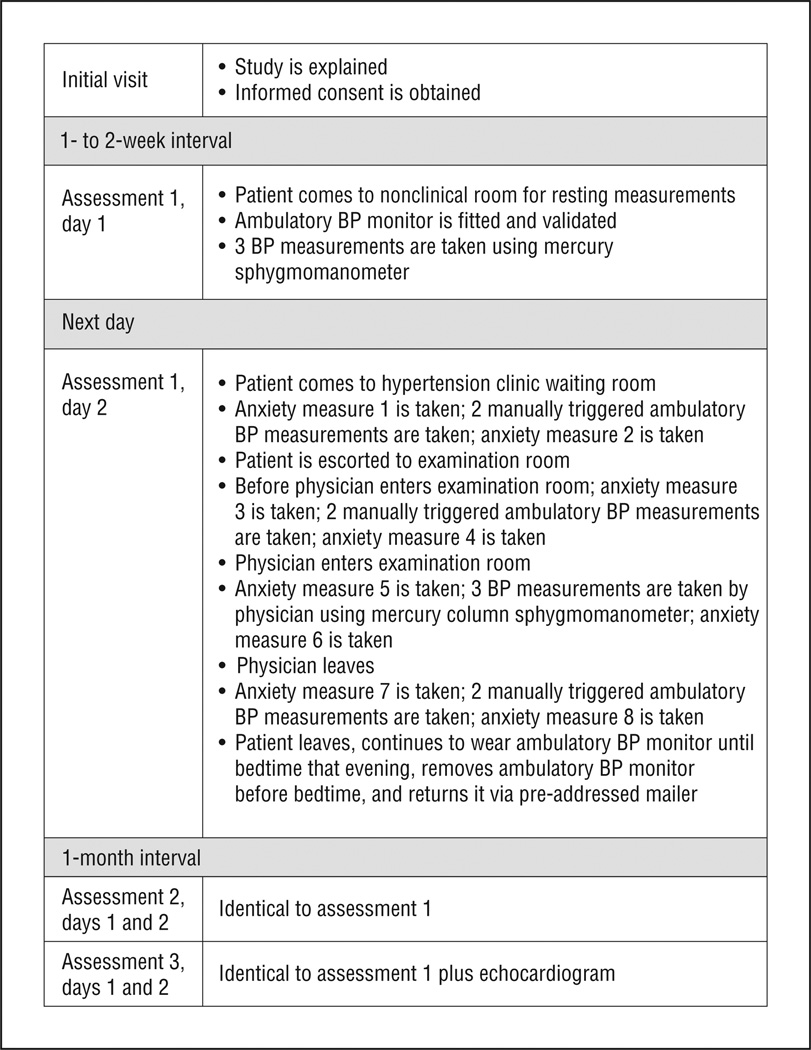
An initial recruitment visit was followed by 3 assessments that lasted for 2 days each, occurring at 1-month intervals. Figure 3 shows the study timeline and procedures.
Figure 3.
Study timeline. BP indicates blood pressure.
Day 1 Visit
The patient was fitted with an arm cuff for an ambulatory BP monitor (model 90207; Spacelabs, Redmond, Washington). This monitor has been previously validated, satisfying the British Hypertension Society protocol.20 During the fitting, 3 calibration readings were taken in accordance with the British Hypertension Society guidelines. Next, a research assistant took 3 BP measurements using a mercury sphygmomanometer according to the American Heart Association guidelines.21 These measurements provided the means to evaluate their comparability with manually triggered ambulatory BP measurements. The patient was told that he/she would wear the monitor until bedtime the following day, at which point the patient would remove the arm cuff. Blood pressure measurements were taken every 15 minutes until 10 pm and every hour between 10 pm and 6 am the next morning, after which the sampling interval reverted to 15 minutes.
Day 2 Visit
The patient (still wearing the ambulatory monitor) was met by the research assistant at the clinic waiting area, where he/she was asked to sit and relax. After a 5-minute rest, the research assistant assessed anxiety, using the Brief Symptom Inventory, Spielberger Trait Anxiety Scale, and the Taylor Manifest Anxiety Scale (trait measures; taken only once). A single-item measure of state anxiety, using a visual analog scale, was taken at several points during the protocol. The research assistant then manually triggered 2 BP measurements using the ambulatory monitor 2minutes apart. State anxiety was then assessed a second time. Figure 3 shows the ordering of the procedures.
Ten to 15 minutes later, patients were taken to the examination room, where the research assistant assessed their state anxiety a third time and then triggered 2 more BP measurements, using the ambulatory monitor, separated by 2 minutes. The research assistant then assessed state anxiety a fourth time. Within 5 minutes of the patient being seated in the examination room, the physician entered the room. State anxiety was assessed a fifth time; the physician then took 3 BP measurements using a mercury column sphygmomanometer, and, with the physician still present, the patient’s anxiety was assessed a sixth time. The physician left the room, and the seventh anxiety assessment was administered. After this, 2 BP measurements were taken by manually triggering the ambulatory monitor followed by a final (eighth) anxiety assessment. The patient then left the hypertension center still wearing the ambulatory monitor.
DATA REDUCTION
The BP and state anxiety scores were averaged for the 3 assessments. When data were missing on any given variable at 1 of the assessments, the remaining data were averaged; when data were missing at 2 of the assessments, the values from the remaining session were used as the score. A list-wise deletion procedure was used in which patients with missing data on more than 1 key variable were excluded from the analysis. Awake ambulatory BP was based on diary entries, which provided bedtime and awake-time information. Manually triggered ambulatory BP measurements were excluded from the calculation of a wake ambulatory means.
STATISTICAL ANALYSES
Analysis of covariance was used to estimate the significance of the effects of a patient’s diagnostic category on BP and anxiety, and the Tukey highly significant difference post hoc test was used to determine the significance of differences among groups when the omnibus test result was statistically significant. The Mauchly test of sphericity was used when repeated-measures designs tested more than 2 conditions, and the Green-house-Geisser correction to degrees of freedom was used when the Mauchly test result was statistically significant. t Tests were used to compare mean change scores. Analyses were performed using a commercially available software program (SPSS, version 11).22 As mentioned previously, the algorithm by which patients were assigned to 1 of the 4 diagnostic categories is shown in Figure 2.
RESULTS
COMPARISON OF AMBULATORY AND SPHYGMOMANOMETER BP MEASUREMENTS
The physician-taken BP measurements were made using a mercury sphygmomanometer because this is the standard basis for a diagnosis of hypertension, according to the American Heart Association criteria. However, the remaining BP measurements were taken by the ambulatory monitor. To assess the comparability between measurements taken using the different devices, we compared the measurements taken in the laboratory on day 1 using a mercury sphygmomanometer and the manually triggered ambulatory BP readings. The average systolic/diastolic BP using the manometer was 129.3/77.8 mm Hg compared with 129.6/77.9 mm Hg using the ambulatory monitor. Pearson correlations were 0.95 (systolic) and 0.92 (diastolic) (P < .001 for both). These results suggest that a valid comparison may be made between the measurements using the 2 methods.
COMPARISON OF ANXIETY MEASURES BY DIAGNOSIS
Table 2 gives the scores for the various anxiety measures broken down by diagnostic category. The final column shows the mean state anxiety ratings made during the day 2 visit. As with previous studies, diagnostic category was not associated with the trait measures of anxiety. As predicted, the only measure on which diagnosis did have an effect was the state measure (F3,237 = 6.4, P < .001). A planned contrast indicated that patients in the white coat hypertension group had significantly higher state anxiety scores than any of the other 3 categories (t = 2.67, P < .01).
Table 2.
Mean (SD) Anxiety Scores by Diagnostic Category
| Diagnosis | Brief Symptom Inventory |
Spielberger Trait Anxiety Scale |
Taylor Manifest Anxiety Scale |
State Anxietya |
|---|---|---|---|---|
| Normotension | 3.3 (3.3) | 19.6 (9.0) | 7.1 (4.4) | 14.5 (15.6) |
| White coat hypertension | 2.5 (2.0) | 16.2 (9.2) | 5.9 (4.5) | 30.6 (25.4) |
| Sustained hypertension | 3.2 (3.4) | 18.6 (9.6) | 6.7 (4.5) | 24.5 (23.3) |
| Masked hypertension | 2.1 (1.8) | 15.6 (8.9) | 6.0 (3.6) | 15.9 (15.0) |
P < .001.
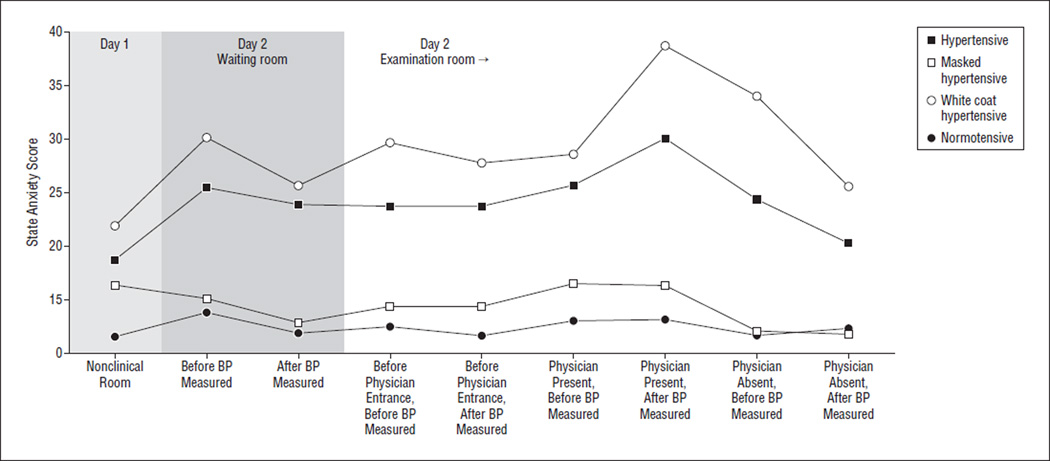
To further explore the effect of diagnosis on the state anxiety measures, we examined the pattern of the scores across the session (Figure 4). A repeated-measures analysis of covariance, controlling for age and sex, showed that the interaction between the circumstance under which the measurement was made (ie, in the waiting room, in the examination room, physician absent or present) and the diagnostic category had a statistically significant effect on state anxiety (F15.4,1083 = 1.69, P < .05). The only other statistically significant outcome was the main effect of diagnosis (F3,228 = 5.15, P < .01).
Figure 4.
Mean visual analog scale scores before and after the physician’s entrance to the examination room for the 4 diagnostic categories. BP indicates blood pressure.
We next examined the 2 state anxiety scores taken when the physician entered and exited the examination room. Planned contrasts (controlling for age and sex) were used to examine the differences in the changes as a function of diagnosis. The comparisons showed that the white coat hypertension group had the largest increase in anxiety compared with the other 3 diagnostic categories immediately after the physician took their BP measurements (t = 3.15, P = .002).
COMPARISON OF BP MEASUREMENTS BY DIAGNOSIS
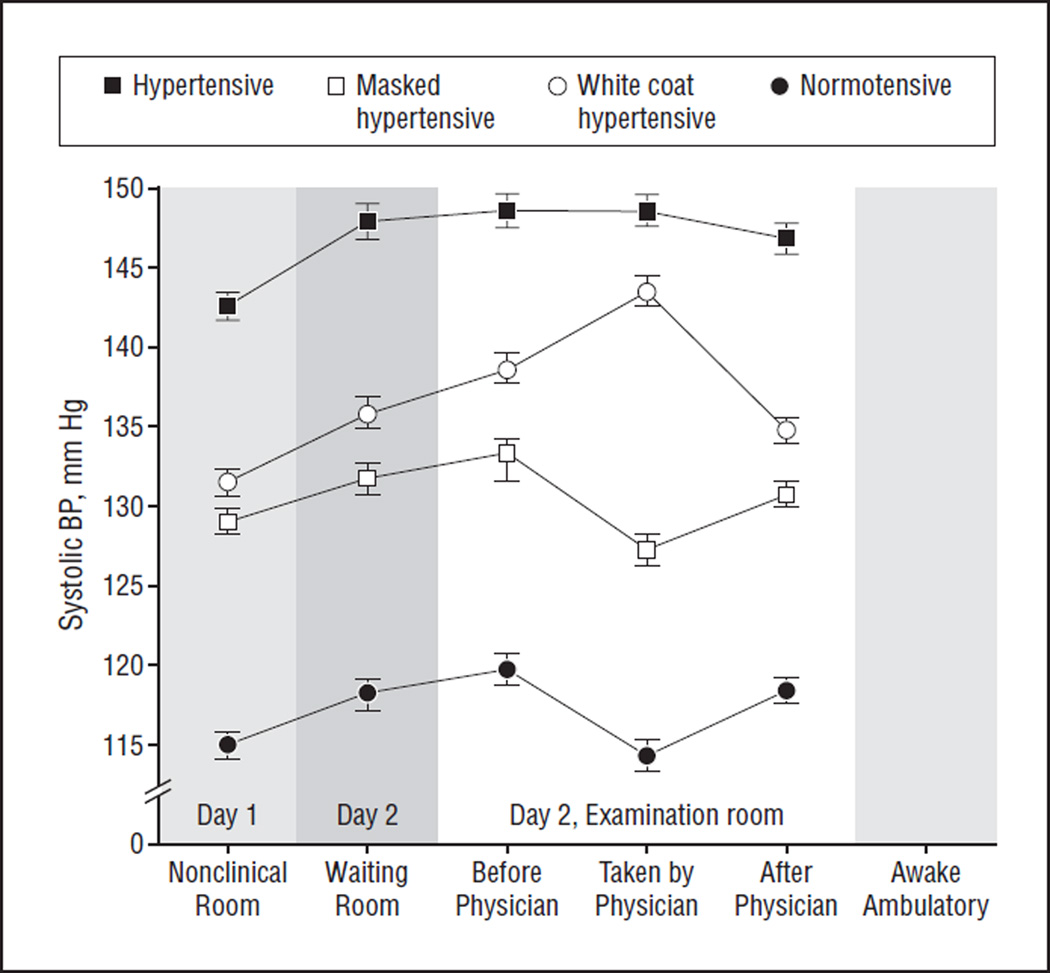
Figure 5 shows the mean systolic BP (the diastolic BP pattern was similar) for each of the diagnostic categories taken on day 1 and at the 4 time points in the clinic on day 2. Relatively little variability was seen in the measurement means for the essential hypertension patient group, and the BP of the normotensive patients and masked hypertensive patients decreased when the physician entered the room. Only the white coat hypertension group showed an increase in BP in the presence of the physician. We used analysis of covariance to examine the significance of the differences, with the 4 BP measures taken in the clinic as a repeated-measures factor and diagnosis as a between-patient factor. Age and sex were included as covariates. The analysis showed that for systolic and diastolic pressure the interaction between setting and diagnosis was statistically significant (F6.4,490.8 = 6.58, P < .001 for systolic BP and F6.9,532.4 = 3.24, P < .01 for diastolic BP).
Figure 5.
Mean systolic blood pressure (BP) before and after the physician’s entrance to the examination room and before and after the physician’s exit from the examination room for the 4 diagnostic categories. Error bars indicate standard errors.
To further explore the interaction, we examined the BP changes among the measurements taken just before the physician entered the examination room, the measurements taken by the physician, and the measurements taken just after the physician left the room. A planned contrast (controlling for age and sex) was used to examine the differences in the BP changes as a function of diagnosis. The comparisons showed that the white coat hypertension group had the largest increase in both systolic and diastolic BP compared with the other 3 diagnostic categories between the readings taken before and after the physician had entered the room (t = 4.86, P < .001 for systolic BP and t = 3.51, P = .002 for diastolic BP). A similar pattern was observed for the BP changes that occurred when the physician exited the examination room. The planned contrast confirmed that the white coat hypertension group had the largest decrease in BP compared with the other 3 diagnostic categories associated with the physician exiting the room (t = 4.57, P < .001 for systolic BP and t = 4.07, P = .001 for diastolic BP).
COMMENT
The results provide support for the hypothesis that anxiety and/or BP is a conditioned response to a specific set of stimuli, notably, the presence of the physician. Our results suggest that white coat hypertension is not a result of trait anxiety; on both state and trait anxiety measures, as in previous studies, persons diagnosed with white coat hypertension scored no higher than persons in any of the other diagnostic categories. If anxiety is conditioned, however, one would not expect to observe such differences. Rather, we would expect that the differences are only evident when assessed under the specific stimulus conditions that occasion the response. This was clearly seen in the differences in the state anxiety measures administered during the clinic assessment. Patients with white coat hypertension exhibited greater anxiety, on average, than those in any of the other diagnostic categories, were highest at every point during the clinic assessment of anxiety (Figure 4), and had a significantly greater elevation in anxiety when their BP was measured by the physician. The BP data followed a similar pattern. When the physician entered the examination room, patients with essential hypertension showed little change when the physician took their BP, and the BP of normotensive and masked hypertensive patients tended to decrease somewhat under this condition. As with the anxiety data, however, patients with white coat hypertension exhibited a substantial BP increase when the physician took the measurements.
Interestingly, the data in the present study suggest that patients with masked hypertension responded much like true normotensive patients in terms of both their anxiety in the examination room and their BP responses to the physician. We speculate that 1 source of the unconditioned anxiety is the hypertension diagnosis itself. This may suggest that the absence of a diagnosis of hypertension fails to produce the conditioned responses observed in those with white coat hypertension. Eighteen years ago, Rostrup et al23 showed that individuals who were hypertensive at screening but had never been diagnosed with hypertension, once given a diagnosis of hypertension, had substantially elevated BP on their next clinic visit compared with a randomly assigned group who were not told that their BP was high. These data suggest that simply being labeled as “hypertensive” may set the stage for the conditioning processes that we hypothesize are occurring here. Thus, our data indicate that the 2 “unlabeled” groups (normotensive and masked hypertensive patients) exhibit the lowest levels of anxiety compared with patients with true and white coat hypertension who have been given diagnostic labels.
The purpose of the study was to test the hypothesis that the white coat effect may be a conditioned response as opposed to a manifestation of general anxiety. We have shown previously that one of the major determinants of white coat effect is having been diagnosed with hypertension,1 which is consistent with a conditioned response. The data presented herein also support this mechanism since the patients with white coat hypertension did not differ from the other groups in terms of the trait measures of anxiety but differed markedly in the levels of anxiety reported in the medical setting, with the greatest difference reported during the physician measurement. The same pattern was observed with the BP changes, which generally paralleled the changes in anxiety.
CONCLUSION
White coat hypertension is an important clinical problem given its potential to result in misdiagnosis and possibly inappropriate drug treatment. Although ambulatory and home BP measurements are more accurate and predictive of target organ damage, physicians’ office measurements continue to be the criterion standard. That being the case, the sources of measurement error that occur in the office setting remain an impediment to the accurate diagnosis and treatment of hypertension. Data from several studies show that who takes the BP and how it is taken (ie, by a person or an automated device) have a substantial effect on the measurement.24 Our findings indicate that measurements taken by physicians appear to exacerbate the white coat effect more than other means. We suggest that one way of addressing this problem is to modify the method by which BP is measured in the office setting given the wide availability of reliable and validated automated BP monitors that are suitable for both office and home use. Similarly, home BP monitoring has been shown to predict target organ damage as well as (or better than) ambulatory monitoring25 and, thus, is superior in this regard to traditional office measurements. Thus, BP taken by an automatic device, while the patient is alone in the physician’s office, may provide the best means of avoiding a hypertension misdiagnosis.
Acknowledgments
Funding/Support: This study was supported in part by grants PO1-HL47540 and R24-HL76857 from the National Heart, Lung, and Blood Institute, National Institutes of Health (Dr Pickering).
Role of the Sponsors: The sponsor played no role in the study design, in the collection, analysis, or interpretation of the data, in the writing of the present report, or in the decision to submit the paper for publication.
Footnotes
Author Contributions: Study concept and design: Ogedegbe, Pickering, and Gerin. Acquisition of data: Albanese and Gerin. Analysis and interpretation of data: Ogedegbe, Clemow, Chaplin, Spruill, and Gerin. Drafting of the manuscript: Ogedegbe, Spruill, and Gerin. Critical revision of the manuscript for important intellectual content: Pickering, Clemow, Chaplin, Spruill, Albanese, Eguchi, and Gerin. Statistical analysis: Chaplin and Gerin. Obtained funding: Gerin. Administrative, technical, and material support: Clemow, Spruill, and Albanese. Study supervision: Gerin.
Financial Disclosure: None reported.
REFERENCES
- 1.Spruill TM, Pickering TG, Schwartz JE, et al. The impact of perceived hypertension status on anxiety and the white coat effect. Ann Behav Med. 2007;34(1):1–9. doi: 10.1007/BF02879915. [DOI] [PubMed] [Google Scholar]
- 2.Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressures. JAMA. 1983;249(20):2792–2798. [PubMed] [Google Scholar]
- 3.Devereux RB, Pickering TG. Relationship between the level, pattern and variability of ambulatory blood pressure and target organ damage in hypertension. J Hypertens Suppl. 1991;9(8):S34–S38. [PubMed] [Google Scholar]
- 4.Björklund K, Lind L, Zethelius B, Andren B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107(9):1297–1302. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- 5.Pickering TG, Coats A, Mallion JM, Mancia G, Verdecchia P, Task Force V. White-coat hypertension. Blood Press Monit. 1999;4(6):333–341. doi: 10.1097/00126097-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Márquez Contreras E, Casado Martinez JJ, Pardo Alvarez J, Vazquez I, Guevara B, Rodriguez J. Prevalence of white-coat hypertension and masked hypertension in the general population, through home blood pressure measurement. Aten Primaria. 2006;38(7):392–398. doi: 10.1016/S0212-6567(06)70531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kario K, Pickering TG. White-coat hypertension or white-coat hypertension syndrome: which is accompanied by target organ damage? Arch Intern Med. 2000;160(22):3497–3498. doi: 10.1001/archinte.160.22.3497. [DOI] [PubMed] [Google Scholar]
- 8.Pickering TG, Schwartz AR, Gerin W. What is the white-coat effect and how should it be measured? Blood Press Monit. 2002;7(6):293–300. doi: 10.1097/00126097-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40(6):795–796. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- 10.Hara A, Ohkubo T, Kikuya M, et al. Detection of carotid atherosclerosis in individuals with masked hypertension and white-coat hypertension by self-measured blood pressure at home: the Ohasama study. J Hypertens. 2007;25(2):321–327. doi: 10.1097/HJH.0b013e3280115bbf. [DOI] [PubMed] [Google Scholar]
- 11.Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med. 1999;131(8):564–572. doi: 10.7326/0003-4819-131-8-199910190-00003. [DOI] [PubMed] [Google Scholar]
- 12.Donner-Banzhoff N, Chan Y, Szalai JP, Hilditch JR. Is the ‘clinic-home blood pressure difference’ associated with psychological distress? a primary care-based study. J Hypertens. 1997;15(6):585–590. doi: 10.1097/00004872-199715060-00003. [DOI] [PubMed] [Google Scholar]
- 13.Gerardi RJ, Blanchard EB, Andrasik F, McCoy GC. Psychological dimensions of “office hypertension”. Behav Res Ther. 1985;23(5):609–612. doi: 10.1016/0005-7967(85)90109-3. [DOI] [PubMed] [Google Scholar]
- 14.Coelho R, Santos A, Ribeiro L, et al. Differences in behavior profile between normotensive subjects and patients with white-coat and sustained hypertension. J Psychosom Res. 1999;46(1):15–27. doi: 10.1016/s0022-3999(98)00054-3. [DOI] [PubMed] [Google Scholar]
- 15.Friedman R, Schwartz JE, Schnall PL, et al. Psychological variables in hypertension: relationship to casual or ambulatory blood pressure in men. Psychosom Med. 2001;63(1):19–31. doi: 10.1097/00006842-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Reiff S, Katkin ES, Friedman R. Classical conditioning of the human blood pressure response. Int J Psychophysiol. 1999;34(2):135–145. doi: 10.1016/s0167-8760(99)00071-9. [DOI] [PubMed] [Google Scholar]
- 17.Dykman RA, Gantt WH. Experimental psychogenic hypertension: blood pressure changes conditioned to painful stimuli (schizokinesis) Integr Physiol Behav Sci. 1997;32(3):272–287. doi: 10.1007/BF02688625. [DOI] [PubMed] [Google Scholar]
- 18.Miller NE, Dworkin BR. Effects of learning on visceral functions–biofeedback. N Engl J Med. 1977;296(22):1274–1278. doi: 10.1056/NEJM197706022962210. [DOI] [PubMed] [Google Scholar]
- 19.Stockhorst U, Steingrueber HJ, Enck P, Klosterhalfen S. Pavlovian conditioning of nausea and vomiting. Auton Neurosci. 2006;129(1–2):50–57. doi: 10.1016/j.autneu.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien E, Pickering T, Asmar R, et al. Working Group on Blood Pressure Monitoring of the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002;7(1):3–17. doi: 10.1097/00126097-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals, part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 22.Norušis MJ. SPSS 11.0 Advanced Statistical Procedures Companion. Upper Saddle River, NJ: Prentice Hall; 2006. [Google Scholar]
- 23.Rostrup M, Kjeldsen SE, Eide IK. Awareness of hypertension increases blood pressure and sympathetic responses to cold pressor test. Am J Hypertens. 1990;3(12, pt 1):912–917. doi: 10.1093/ajh/3.12.912. [DOI] [PubMed] [Google Scholar]
- 24.Gerin W, Marion RM, Friedman R, James GD, Bovbjerg DH, Pickering TG. How should we measure blood pressure in the doctor’s office? Blood Press Monit. 2001;6(5):257–262. doi: 10.1097/00126097-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Jula A, Puukka P, Karanko H. Multiple clinic and home blood pressure measurements versus ambulatory blood pressure monitoring. Hypertension. 1999;34(2):261–266. doi: 10.1161/01.hyp.34.2.261. [DOI] [PubMed] [Google Scholar]