Introduction: Targeting Non-communicable Diseases in Low- and Middle-Income Countries
Between 1990 and 2010 the global non-communicable diseases (NCDs) burden increased from 43% to 54% of the total disease burden.1 In 2012, globally, almost three quarters (74%) of all the NCD burden occurred in low- and middle-income countries.2 Population growth and population aging have contributed substantially to the expanding NCD burden trends – both of which are rapidly occurring within low and middle income country populations.3, 4 Effectively tackling this growing NCD burden in low- and middle-income country settings presents a major challenge, yet, is an achievable task.2, 3, 5
Today, many effective NCD interventions are available. The World Economic Forum and World Health Organization (WHO) recently developed a report targeted at decision makers, civil society, and the private sector, that provides assessments of the economic impact of noncommunicable diseases and costs of scaling up a core of proven-effective interventions within low- and middle income counties.6 However, responding to these challenges in low- and middle-income countries will need local research capacity building,7 so that interventions are driven by in-country knowledge-bases provided through research performed in low- and middle-income countries. Yet, research infrastructure and outputs in low and middle income countries are woefully inadequate, and the data from these settings are scarce.3, 8 This situation poses problems both for implementation of known interventions and also for tackling low- and middle-income country disease patterns, phenotypes that might differ from high-income countries.
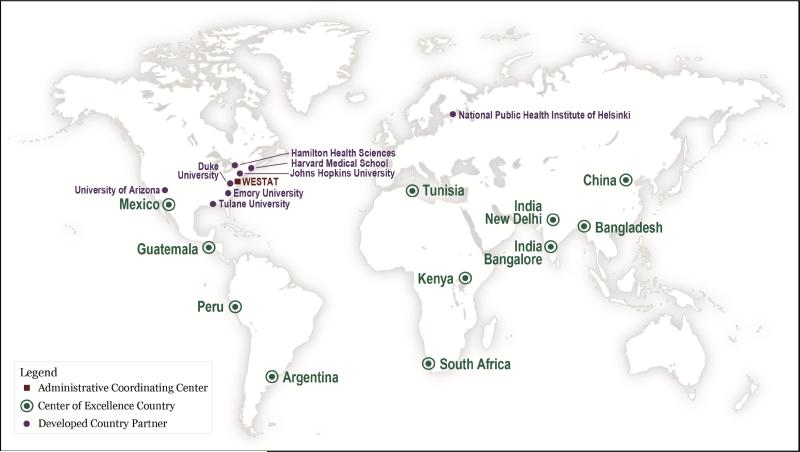
To address research needs for NCDs in low- and middle-income countries, in 2009, the National Heart, Lung, and Blood Institute (NHLBI) and UnitedHealth Group (UHG) engaged in a Chronic Disease Initiative (2009-2014), previously described,9, 10 which supported a network of eleven low- and middle-income country-based research centers – six of which were supported by both institutions - based in ten countries. (Figure 1) This public-private partnership created the NHLBI-UnitedHealth Global Health Centers of Excellence (COE) Program (referred to hereafter as the Program). The Program's overall goal was to contribute to the reduction of cardiovascular and lung disease burdens by catalyzing in-country research institutions to develop a global network of biomedical research centers that conduct collaborative research, train researchers, and advise on policy. Our purpose here is to describe an overview of achievements and lessons learned from the eleven COEs supported by the Program, based in Argentina, Bangladesh, China, Guatemala, India (2 centers), Kenya, Mexico, Peru, South Africa and Tunisia. A formal evaluation of the Program is underway and is planned for completion in 2016.
Figure 1.
National Heart, Lung, and Blood Institute-UnitedHealth Global Health Centers of Excellence Program country location of centers, and name and location of the primary developed country partners and the administrative coordinating center
Forming the Program: Capturing the Elements of Team Science
The Program was established with advice from global experts in the areas of cardiovascular and pulmonary diseases, epidemiology, biostatistics, health services and outcomes research, clinical trials, and international health promotion and disease prevention. COEs funded by NHLBI were located within institutions that were National Institutes of Health (NIH) Fogarty International Clinical Research Fellows and Scholars sites. In addition to the COEs, a U.S. based administrative coordinating center (Westat) provided administrative, logistical, and data management support, and coordination of key activities (e.g., site establishment, institutional review board coordination and tracking, and protocol registration). Finally, each COE partnered with at least one developed (high-income) country academic institution based in the United States, Canada, Europe, or Australia and with local partner organizations such as health care institutions, universities and research institutions, non-governmental agencies, and government bodies. Developed country partners provided technical and research support to facilitate growth of each center's research capacity and capability.
This initiative built on best practices of collaborative scientific work, yet was far more innovative in terms of capacity building and empowerment, both scientifically and administratively. The Program was designed so that the low- and middle-income country applicants were the prime recipient of the award. Many of the COEs had to quickly mature scientifically and bring their administrative and grant management procedures to international standards. In so doing, the COE platform lifted not only the scientific potential of partners, but their ability to improve financial, managerial, legal and accounting procedures. These major in-country gains proactively countered the pervasive model of “parachuting” research – all too common within international collaborations.
Developing Research Platforms: Collaboration Based Approach
Each COE developed its research platform, collaboration network, and priority research areas for heart and lung diseases. The characteristics of each COE and its developed country partner and local partner institutions varied, resulting in each platform having unique features. The research focused on disease epidemiology, prevention and control along with training future investigators (e.g., graduate, postdoctoral).
Program governance was led by a Steering Committee which included NHLBI, UHG and Westat leadership and both COE and develop country partner principal investigators. It provided: scientific oversight and advice on network activities; facilitated collaboration across COEs to ensure that mechanisms and strategies led to achieving program goals; advice on partnerships and global health opportunities; a venue for sharing research accomplishments, as well as generating common policies, guidelines, and procedures for the network. NIH best practices and guidelines for research, training, ethics, and data policies and procedures were adopted Program-wide. Working subcommittees of the Steering Committee were composed of investigators and staff from the COEs, developed country partners, NHLBI, UGH, and Westat. Subcommittees were created for training, epidemiology, pulmonary diseases, and community health workers.
A total of 38 original research activities were conducted between 2009 and 2014. (Table 1) Three study approaches were employed: single COE led studies that were driven by unique local needs and opportunities conducted in one (25 studies) or multiple sites (7 studies) within a center and multi-COEs studies harmonized across centers addressing a common health priority issue (6 studies). The type of study designs included epidemiological (43%), behavioral (21%), interventional (17%), and other types (19% encompassing health economics, model development, and feasibility studies). (Table 1) The number of primary research studies conducted by each COE ranged from two (Argentina, India-New Delhi, Mexico, and Tunisia) to seven (Guatemala). These original studies yielded a substantial number of publications (peer-reviewed scientific journals, reports, press releases, and news articles), presentations, media coverage, and involvement of COE trainees in research efforts. (Table 2)
Table 1.
National Heart, Lung, and Blood Institute-UnitedHealth Global Health Centers of Excellence Program descriptions for 38 primary studies.
| Lead COE | Short Title | Study Design | Study Population (Setting) | Intervention | Outcomes Measured |
|---|---|---|---|---|---|
| Argentina* | Cardio Risk Factors Detection | Randomized multi-stage stratified cluster sample | MF 35-74 y (community) | N/A | Events, prevalence, RF control |
| Argentina* | Lower Respiratory Tract Illness in Children Related to IAP | Retrospective cohort | Household with child ≤5 y or stillborn (households with high biomass exposure) | N/A | IAP exposure, history of pregnancy, births, respiratory infections |
| Bangladesh | COPD and HT on Households | Cross-sectional descriptive | MF ≥18 y with COPD, HT (households) | N/A | Prevalence, cost of care, health seeking behaviors |
| Bangladesh | Determinants of COPD | Prospective longitudinal cohort | MF ≥40 y (community) | N/A | Function, prevalence, coping strategies |
| Bangladesh | Prevalence of Arterial HT | Prospective cohort | MF ≥20 y (rural/urban surveillance sites) | Health messages, medical referrals | BP, prevalence, RFs, |
| Bangladesh | Chronic Disease in Matlab | Quantitative survey-Health/demographic surveillance system | Poor households (rural) | N/A | Socioeconomic consequences of CD; mortality distribution |
| Bangladesh* | Cook stoves and IAP with Women and Children | Prospective cohort | F ≥18 y & children ≤5 y (rural households) | gas cook stoves | CVD RFs, respiratory morbidity, lung function |
| China | CV Risk Mgmt Arm, Salt Reduction Arm | Factorial cluster-RCT | M ≥50 y F ≥60 y (villages in 5 provinces) | Low-cost CVD prevention/control package with incentive | Events, prevalence, adherence, cost of care |
| China | CRHI: Salt Reduction Arm | Factorial cluster-RCT | Villages (townships in 5 provinces) | Community salt reduction; health promotion prog | Sodium-potassium ratio, BP, proportion HT |
| China** | Effects of SimCard-China/India | Cluster-randomized controlled intervention trial | MF ≥40 y with HD, stroke, DM, or SBP ≥160 mmHg (poor villages) | Simplified CVD management prog for high-risk individuals | changes in high-risk patients treated with diuretics |
| Guatemala | Dietary Factors Assoc with CVD | Cross-sectional | Children 7-12 y and parents (schools-poor peri-urban areas) | N/A | Prevalence |
| Guatemala | CV Risk Factors in Children, | Qualitative study | school children 7-12 y; parents, teachers; health providers; community leaders (poor peri-urban areas) | N/A | Knowledge & attitudes on CVD determinants |
| Guatemala | CV Risk Factors in Children | Characterization of CVD RFs | school children 7-12 y (Poor peri-urban areas) | N/A | Prevalence of CVD RFs |
| Guatemala | CV Risk Factors in Children | Pre/post single sample design pilot | Children 7-12 y & parents (schools in poor peri-urban areas) | Multilevel-CV intervention model | Feasibility, short-term effectiveness of model |
| Guatemala* | CV Risks in Persons with DM2/HT | Quasi-experimental design, model development | Patients with DM and HBP (PCC in Mexico/Costa Rica) | Validated CVD intervention model | Feasibility, acceptability, short term efficacy |
| Guatemala** | mHealth Technology | Validation of intervention pilot | MF 30-60 y non HT/DM (PCC in poor urban areas in 3 countries | SMS messages, | mHealth technology for SMS. One-to-one calls |
| Guatemala** | mHealth Technology | RCT proof-of-concept intervention | Pre-HT MF (PCC in poor urban areas in 3 countries | Intensive lifestyle modification prog. | Feasibility, acceptability, implementation |
| India, Bangalore | PREPARE | Multi-center, household cluster-randomized trial | Households (rural regions) | Clinic visits, counseling by CHW | BMI, waist/hip circumference, BP, INTERHEART risk score, BP medication |
| India, Bangalore | SPREAD | Multi-center randomized open trial | Patients with ACS (hospitals) | CHW education/visits physician referrals | Adherence to pharmacotherapy, incidence of CV events, RF assessment |
| India, Bangalore | INSPIRE | Multi-center randomized open trial | Stroke patients (secondary & tertiary hospitals) | N/A | Clinical outcomes, clinical practice patterns for care, secondary prevention |
| India, New Delhi* | CARRS Surveillance Study | Multi-stage cluster random sampling survey | MF 20-59 y (urban households) | N/A | CVD prevalence, RF, incidence of morbidity and mortality |
| India, New Delhi* | CARRS Translational Trial | Multi-site, individually randomized controlled translation trial | DM2 patients (out-patient clinics) | Multi-factorial CVD risk reduction intervention | assess intervention feasibility, patient evaluation |
| Kenya | IAP in Western Kenya | Cross-sectional | Females ≥35 y (hospital) | N/A | Isolated right heart failure prevalence |
| Kenya | Cardiac Heart Failure | Case-control | Case: MF ≥40 y with HF, control: without (hospital) | N/A | Prevalence |
| Kenya | HT, DM & Organ Damage | Pop-based cross-sectional | MF ≥18 y (households) | N/A | Prevalence |
| Kenya** | IAP in Kenya/Bangladesh | Pre-post intervention RCT | Women & children ≤10 y (rural households) | Low-emission cook stoves; education prog | Pulmonary function, respiratory symptoms, stove acceptance |
| Kenya | Hand held echocardiogram Study | Convenience sample | Echocardiography patients (rural hospital) | HHE; physical exam | HHE diagnosis of cardiac diseases |
| Kenya | Impact of Clean Cook stoves | Community-based randomized intervention trial | Children ≤5 y (rural households) | Low-emission cook stoves | Household air pollution. Pneumonia (severity) |
| Mexico | Meta-Salud Chronic Disease Prevention | Pre & post-test evaluation | Adults MF average age 42 y (SD 10.6) (low resource urban area) | Community-based training on NCD prevention by CHW | Clinical/behavioral-lifestyle outcomes: BMI, waist/hip circumference, weight, triglycerides, LDL cholesterol |
| Mexico | Meta-Salud: Chronic Disease Prevention | Process evaluation design | Stakeholders involved in the research study (participants, CHW, clinic staff) | Community-based training on NCD prevention by CHW | Intervention improvement and refinement |
| Peru | Geo Variation/Progression of NCDs | Longitudinal cohort | MF ≥35 y (4 geographical settings in Peru) | N/A | BP, blood glucose, lung function; RF mortality, incidence; prevalence |
| Peru** | Cook stoves-Peru/Kenya/Nepal | Multi-country, community feasibility intervention trial | Females 20-49 y (rural households) | Improved cook stoves with chimney | Respiratory symptoms, expiratory flow/volume, exhaled CO, 24hr particulate matter, pulmonary function |
| Peru* | Lung Ultrasound and Improved Cook stoves | Diagnostic accuracy study | Children <3 y with WHO ALRI criteria (poor settings- Peru & Nepal) | Lung ultrasound | O2 saturation, pneumonia misclassification rates |
| South Africa | CRIBSA | Cross sectional survey in a random pop sample | Black Africans (peri-urban townships) | N/A | N/A |
| South Africa | Tools to Manage Chronic NCDs | Pragmatic cluster RCT | PCPs (PCC in underserved communities) | Novel guideline-based training prog. | Treatment intensification, CV and pulmonary disease care, processes/outcomes, cost effectiveness |
| South Africa** | Eval of CHW in SA/Bangl/Guat/Mexico | Quasi-experimental design pilot | MF ≥25 y (PCC in 4 countries) | Screening by CHW, clinic referrals | CHW/professionals CVD risk scores; referral Effectiveness |
| Tunisia | Effectiveness NCD risk factors control | Quasi experimental design pre/post with control group | MF 18-65 y (community); MF 18-65 y (workplaces); MF 12-17 y (schools) | Healthy life style; peer education; media | RF (smoking, unhealthy diet, physical inactivity) control |
| Tunisia | Kindergarten healthy lifestyles intervention | Quasi experimental design pre/post with control group | MF 4-5 y (kindergarten school children) | Healthy life style intervention; health education | RF (unhealthy diet, physical inactivity) control |
Abbreviations: ACS, acute coronary syndrome; BP, blood pressure; HBP, high blood pressure; SBP, systolic blood pressure; CHW, community health workers; CV, cardiovascular; CVD, cardiovascular disease; CRHI, China Rural Health Initiative, DM, diabetes; DM2, type 2 diabetes; HD, heart disease; HF, heart failure; HT, hypertension; IAP, indoor air pollution; LDL, low-density lipoprotein cholesterol; MF, males and females; PCC, primary care clinic; RF, risk factor; RCT, randomized controlled trial; y, year
Led by a COE with multiple sites within their collaboration network (7 studies)
A collaboration across multiple COEs (6 studies) addressing a common health priority issue
Table 2.
National Heart, Lung, and Blood Institute-UnitedHealth Global Health Centers of Excellence Program metrics, 2009-2014.
| Center of Excellence | Primary research studies | Publications | Presentations | Media coverage events | Trainees |
|---|---|---|---|---|---|
| Argentina | 2 | 12 | 25 | 60 | 16 |
| Bangladesh | 5 | 32 | 65 | 20 | 24 |
| China | 3 | 38 | 77 | 38 | 104 |
| Guatemala | 7 | 16 | 29 | 2 | 148 |
| India-Bangalore | 3 | 6 | 3 | 1 | 65 |
| India-New Delhi | 2 | 78 | 2 | 0 | 112 |
| Kenya | 7 | 3 | 45 | 0 | 36 |
| Mexico | 2 | 8 | 24 | 6 | 10 |
| Peru | 3 | 50 | 19 | 8 | 42 |
| South Africa | 2 | 42 | 36 | 13 | 16 |
| Tunisia | 2 | 12 | 52 | 3 | 140 |
| Total | 38 | 297 | 377 | 151 | 713 |
The program provided network-wide interactions (four structured exchanges each year, two being face to face) and flexibility that promoted creativity, cooperation and enhanced training. Additional supplemental funding provided resources to support strategic collaborative studies and by year two of the Program, the dynamics of the group transformed from being a group of funded institutions conducting their own research into a network of colleagues working together in synchrony where the whole was much greater than the sum of its parts.
Research Training: High Priority Pipeline for Future Investigators
A key component of the Program was training future researchers. The objectives of the training efforts were to: i) develop staff capable of conducting independent and/or collaborative research, ii) train future cardiovascular and pulmonary investigators at the doctoral and postdoctoral levels; and iii) stimulate clinical, epidemiologic, health services, health policy, and behavioral research. Each institution developed training plans that responded to skill gaps within their country settings. Some training opportunities were the result of single COE efforts while others involved collaboration with developed country partners, other COEs, and local partners. While training activities within individual COEs were tailored to meet local needs, there were several common elements employed throughout the Program. The breadth and depth of the training component were evident across the entire Program and reflected the high level of commitment to this objective as described in this issue of the Journal.11
High Level Collaboration: Development of a Program Wide Harmonized Data Commons
During the active research phase of the Program, several collaborations received supplemental funding to address common priority topics across COEs including, but not limited to, community health workers, 12, 13 clean cookstoves, 14 and NCD risk stratification and management. 15, 16 . Others took advantage of the well characterized cohorts to ask fundamental basic science questions such as a comparative analysis of the pulmonary microbiome within biomass fuel exposed and unexposed populations.
A network-wide collaboration allowed the Program to develop a data commons of harmonized variables across several COE studies. This approach provided opportunities to maximize use of established datasets and increase the impact of the work supported by the Program. This aligned well with NHLBI's call for more innovative uses of data across all research investments.17-19
Forty data collection instruments from 14 primary research studies were reviewed to identify common variables anticipated as valuable for multiple site analyses. Not all variables were available within each research activity, and specific criteria and methodology were created for multisite analyses. A master codebook was developed and data files were shared for planned analyses.
Data harmonization required expert knowledge of the research, database structure, data management, programming, researcher commitment, and consensus on standardized variables. Many of these challenges are common to meta-analysis and other data pooling efforts.20, 21 Some of the key lessons during this process included: anticipating and planning common studies across sites upfront; using common protocols and data collection instruments with standardized variables across sites when possible (e.g., Clinical Data Interchange Standards Consortium20); employing data management best practices at all sites to minimize errors in data submitted for harmonization; and, allowing time and resources during the lifetime of the Program for talent exchange and targeted resource support to foster high quality outputs and collaboration between groups.
Yet, in spite of all these challenges, a harmonized data commons provided many opportunities. Additional research questions – those not answerable solely from the individual site data – now can be tackled in more depth and breath. Some advantages to this approach include: the ability to make unique global comparisons across countries and continents and assess common issues in highly varied contexts in much more depth than other global studies,1 better precision for estimates with larger samples that allow more detailed analyses; and finally, promoting greater collaboration and efficiencies in future research efforts. To date, this global harmonized data commons has led to at least 5 studies, including some featured in this issue of the Journal that offer insight into cardiovascular disease,22-24 diabetes,25 and obesity.26
In addition to this harmonized data commons, all Program data have been submitted to the NIH for compilation, consistent with the agency's policy.27, 28 Data sets were de-identified and redaction plans were developed for creation of public use datasets. In September, 2016, datasets are planned to be made available in the public domain via NHLBI's data repository, BioLINCC
Discussion
This Program embraced a strategic approach for tackling non-communicable diseases in lowand middle-income countries. With the growing burden of non-communicable diseases in this setting and a knowledge base of effective interventions available, the need to gain locally-driven research efforts that can identify and address priority health issues in specific country settings is essential.
The Program built both research and administrative capacity while training the next generation of U.S. and low- and middle-income country-based researchers. For example, the Program pioneered capacity development for conducting NCD surveillance, which at the country level remains a major weakness. In addition, Program efforts created an instrument for assessing county-level capability to respond to NCDs.29, 30 COEs have also catapulted development of innovative interventions and their implementation- much needed in both low- and middle-income countries.15 Supplementary grants promoted cross-collaboration between COEs and resulted in fast-track development and testing of state-of-the-art interventions combining technology with implementation in real-world settings. An example is technology-driven CVD risk ascertainment by community health workers in India and China.16
The U.S. Council on Foreign Relation's call to engage in global health is driven by the fact that the burden of death and disability is heavily NCD-related within many low and middle-income countries, and because non-communicable diseases are undermining the effectiveness of existing U.S. global health investments.27 This has led to their call for the U.S. government to build on existing U.S. global health platforms that can achieve sustainable reductions in premature death and disability that disproportionately affect the poor.
A unique component of this Program is that it was led by institution and investigators in lowand middle-income countries. The investigators developed and executed the research programs engaging local and global partners, ultimately creating a south to-south driven research collaborative network unique within the world. This organizational structure fostered in-country capacity development and training components. Both capacity and training are essential in assuring that a sound research platform and a skilled research workforce is produced. Through providing context specific evidence, this Program will guide future research and disease prevention and control efforts. The funding structure of the program allowed for very frequent direct interactions between funding institutions (NHLBI, UHG) and the COEs. This also resulted in a benefit to the funders, as they were able to appreciate and fully understand the challenges faced by researchers in low- and middle-income countries, and therefore strengthen instructional capacity for future funding of research conducted in these settings.
Another key element this Program embraced was collaborations—multiple partners and bidirectional, diverse collaborations—across all levels. This is very consistent with recent calls for more team science, which has been shown to be impactful, foster innovation and productivity, and obtain more broad reach and uptake.31-33 Even at the Program's genesis, the innovative public-private partnership between NHLBI and UHG led the way. The collaborative network that subsequently developed had three key dimensions. First, the low- and middle-income country researchers joined with developed country partners. Second, peer to peer collaboration and learning across the Program network between in-country researchers—those who experienced very similar challenges—was invaluable for sharing lessons learned while working across highly diverse environments. Finally, development of a data commons and harmonizing data for multisite analyses represents one of the highest levels of collaboration, where skills, resources, and data are shared—resulting in highly unique analyses and outputs. In addition, other partners joined the network. The U.S. Centers for Disease Control and Prevention (CDC), the American Thoracic Society, and Medtronic Foundation capitalized on the network structure and contributed financially and technically to the Program. While many challenges arose and lessons were learned during both the Program's creation and during analytic efforts, the returns were substantial – reflected in several dimensions including publications, presentation, media coverage, and trainee experiences. (Table 2)
A legacy of collaboration now continues. First, the 11 COEs have created the Global Research Against Non-communicable Disease (GRAND South) Network15 to continue sharing experiences and conducting relevant NCD research, capacity building, and policy engagement. The GRAND South Network goal is to combat non-communicable diseases at local and global levels by conducting innovative research to identify, understand, and overcome barriers to the adoption, adaptation, integration, scale-up and sustainability of evidence-based interventions and policies. Second, Emory University has led development of the Network of U.S. Investigators in Global Non-communicable Diseases which targets US academic institution investigators34 and launched The Atlanta Declaration: A 21st Century Vision for U.S.-based Global NCD Research with the goal of creatively supporting the next generation of scientists in the global NCD arena through larger and sustained investments in global NCD research and encouraging non-tradition career paths that achieve innovation.35 Finally, much of the initial work for the creation of a cardiac care unit and division in Kenya was facilitated by the energy and attention that the Kenya NHLBI COE program fostered. 36
Beyond this global Program, NHLBI is engaged in many other areas 37 including the Global Alliance for Chronic Disease,38 the Global Alliance for Clean Cookstoves,39 and the Medical Education Partnership Initiative, 40 and is crafting a strategic way forward by incorporating NHLBI's Global Health Strategic Plan,41 recommendations from a NHLBI Global Health Think Tank42, and the ongoing NHLBI Strategic Visioning Initiative,43 the latter focusing on identifying compelling research questions and critical research challenges for the next decade.
Conclusions
As the Institute of Medicine recently affirmed, reducing the burden of cardiovascular and other chronic diseases worldwide - especially in low- and middle-income countries - is an achievable goal.5 Tackling this challenge and achieving the Global Sustainable Development Goals for 2016 to 2030 44 will require innovative strategies that invest in country-based research capacity development, create global networks of researchers, and expand collaboration between the U.S. and low- and middle-income countries. Such efforts can lead to scaling-up of the National Economic Forum's and World Health Organization's “best buys” - effective, affordable interventions for specific real world settings guided by country-driven health priorities.5, 45, 46 The GRAND South Network and it successes clearly illustrates that it can be done.
Highlights.
A public-private partnership created the Program.
Forming the Program captured all the elements of team science.
The Program used best practices of collaborative scientific.
Research training for future investigators was a high priority.
Acknowledgements
We want to express our deep thanks to all Programs staff across all institutions for their outstanding efforts, dedication, and commitment that made this collaboration successful. They are acknowledged here:
ARGENTINA: Institute for Clinical Effectiveness and Health Policy (Buenos Aires, Argentina) Gabriela Matta, Laura Gutierrez, Natalia Elorriaga, Rosana Poggio, Vilma Irazola; Tulane University (New Orleans, Louisiana, USA) Lydia Bazzano. BANGLADESH: International Centre for Diarrhoeal Disease Research, Bangladesh (Dhaka, Bangladesh) Abbas Bhuiya, Abdul Wazed, Alfazal Khan, Ali T Siddiquee, Anwar Islam, Jahangir AM Khan, Jasim Uddin, Khaled Hasan, Masuma A Khanam, Mohammad Yunus, Muhammad AH Chowdhury, Nazratun N Monalisa, Nurul Alam, Peter K Streatfield, Shyfuddin Ahmed, Sonia Parvin, Taslim Ali, Current addresses: Alejandro Cravioto (International Vaccine Institute, Seoul, Rep of Korea), Louis W Niessen (Liverpool School of Tropical Medicine, Liverpool, UK), Mohammad D Hossain (BRAC University, Dhaka, Bangladesh), Tracey LP Koehlmoos (Uniformed Services University of the Health Sciences, Bethesda, MD, USA); Institute of Development Studies (Brighton, UK) Hilary Standing, Henry Lucas; Johns Hopkins University (Baltimore, MD, USA) Sara N Bleich, Gerard F Anderson, Antonio J Trujillo, Andrew J Mirelman. CHINA: The George Institute for Global Health (Beijing, China) Jesse Hao, Jing Zhang, Maoyi Tian, Polly Huang, Rong Luo, Weigang Fang, Xian Li; Changzhi Medical College (Changzhi, China): Xiangxian Feng, Zhifang Li; Duke University (Durham, North Carolina, USA) Kelly Deal, Eric Peterson; Elizabeth DeLong, First Hospital of China Medical University (Shenyang, China): Bo Zhou, Jingpu Shi; The George Institute for Global Health (Sydney, Australia) Bruce Neal, Stephen Jan, Nicole Li, Stephen McMahon; Hebei Province Center for Disease Prevention and Control (Shijiazhuang, Hebei, China) Jianxin Zhang, Jixin Sun; Imperial College London, (London, UK) Paul Elliot; Ningxia Medical University (Ningxia, China) Yi Zhao, Yuhong Zhang; Peking University Health Science Center (Beijing, China) Chen Yao, Ningling Huang Sun, Qide Han, Ruqun Shen, Wenyi Niu, Yanfang Wang, Yang Ke, Yining Huang; University of Sydney (Sydney, Australia) Stephen Leeder; University of Queensland (Queensland, Australia) Alan Lopez; Xi'an Jiaotong University (Xi'an, China) Ruijuan Zhang, Yan Yu. GUATEMALA: Instituto de Nutrición de Centro América y Panamá (Guatemala City, Guatemala) Ana V Roman, Carlos Mendoza, Dina Roche, Gabriela Mejicano, Maria A Cordova, Maria F Kroker, Meredith Fort, Paola Letona, Rebecca Kanter, Regina Garcia, Sandra Murillo, Violeta Chacon; Universidad Autónoma de Santo Domingo (Santo Domingo, Dominican Republic) Rafael Montero; Universidad de Ciencias y Artes de Chiapas (Chiapas, Mexico) Erika J Lopez, Liz Peña, Maricruz Castro; Universidad de Costa Rica (San José, Costa Rica) Ana L Dengo, Emilce Ulate, Nadia Alvarado; Universidad de El Salvador (San Salvador, El Salvador) Josefina Sibrian; Universidad Nacional Autónoma de Honduras (Tegucigalpa, Honduras) Astarte Alegria; Universidad Nacional Autónoma de Nicaragua (Managua, Nicaragua) Ana M Gutierrez; Universidad de Panamá (Panama City, Panama) Flavia Fontes. INDIA, BANGALORE: St. John's Research Institute (Bangalore, India) Alben Sigamani, Deepak Kamath, Freeda Xavier, KB Deepthi, M Anupama, Nandini Mathu, Nisha George, Pranjali Rahul, Prem Pais, Preeti Girish, Seena Thomas, T Usha, Tinku Thomas; All India Institute of Medical Sciences (Bhopal, India) Rajnish Joshi; Annamalali University (Chidambaram, India) N Chidambaram; Fortis Escorts Hospital (Jaipur, India) Rajeev Gupta; The George Institute for Global Health (Sydney, Australia) Clara Chow; Population Health Research Institute (Hamilton, Canada) Janice Pogue, Martin O'Donnell, PJ Devereaux; St. John's Medical College (Bangalore, India) Dominic Misquith, Twinkle Agrawal, Farah N Fathima; INDIA, NEW DELHI: Public Health Foundation of India (New Delhi, India) Kolli Srinath Reddy, Roopa Shivashankar, Vamadevan S Ajay; Aga Khan University (Karachi, Pakistan) Hassan M Khan, M Masood Kadir, Muhammad Q Masood, Zafar Fatmi; All India Institute of Medical Sciences (New Delhi, India) Anand Krishnan, Kavita Singh, Nikhil Tandon, Rajesh Khadgawat; Amrita Institute of Medical Sciences (Kochi, India) V Usha Menon; Bangalore Endocrinology and Diabetes Research Centre (Bangalore, India) Mala Dharmalingam; Care Hospital, (Hyderabad, India) Bipin Kumar Sethi; Chellaram Diabetes Institute, (Pune, India) A.G. Unnikrishnan; Emory University (Atlanta, GA, USA) Mark L. Hutcheson, Mohammed K. Ali, Solveig A Cunningham, Shivani A Patel, Unjali Gujral; Goa Medical College, Bambolim, (Goa, India) Ankush Desai; Madras Diabetes Research Foundation (Chennai, India) Deepa Mohan, R Guha Pradeepa, V Mohan; MV Hospital for Diabetes Pvt. Ltd. (Chennai, India) Vijay Viswanathan; Osmania Medical College (Hyderabad, India) Rakesh Sahay; Reproductive Health Access Project, (New York, NY, USA) Seema Shah; St. Johns Medical College (Bangalore, India) Ganapathi Bantwal; Topiwala National Medical College (Mumbai, India) Premlata K Varthakavi; Nuffield Department of Population Health, University of Oxford (Oxford, UK ) Manisha Nair. KENYA: Moi University Teaching and Referral Hospital (Eldoret, Kenya) Constantine Akwanalo, David Lagat, Felix Barasa, Myra Koech, Wilson Sugut, Belinda Korir, Priscah Mosol, Shamim Ali; Brown University (Providence, RI, USA) Charles B. Sherman, Jane Carter; Duke University (Durham, NC, USA) Gerald Bloomfield, Cynthia Binanay; Icahn School of Medicine at Mount Sinai, (New York, NY, USA) Rajesh Vedanthan. PERU: Universidad Peruana Cayetano Heredia (Lima, Peru) A Bernabé-Ortiz, F León-Velarde, George D Smith, Germán Málaga, Héctor H García, Juan P Casas, Katherine Sacksteder, Liam Smeeth, Luis Huicho, María Rivera, Raúl Gamboa, Shah Ebrahim, Víctor M Montori; Johns Hopkins University (Baltimore, MD, USA) Robert A Wise, William Checkley, Gregory B Diette. SOUTH AFRICA: Center of Excellence Chronic Disease Initiative in Africa (Cape Town, South Africa) Beatrice Nojilana, Buyelwa Majikela-Dlangamandla, Carmelita Sylvester, Johanna Malan, Katherine Murphy, Krisela Steyn, Lindi van Niekerk, Robert Mash, Thandi Puoane; Brigham & Women's Hospital (Boston, MA, USA) Grace Kim; Harvard University (Boston, MA, USA) Ankur Pandya; Shafika Abrahams-Gessel; Stellenbosch University (Stellenbosch, South Africa) Hilary Rhode, Michael Pather; University of Cape Town (Cape Town, South Africa) Alvaro R Andrade, Beatriz Garcia, Carlos Velasco, David Medina, Delia Bravo, Diana Munguia, Eric Bateman, Francisco Castro, Helen Schneider, Ilse Ibarra, Jabulisiwe Zulu, Joel Felix, Karla Tribe, , Kirsten Bobrow, Lara Fairall, Naomi Folb, Norma Murillo, Norma Pacheco, Paloma Rodriguez, Paola Navarro, Reyna Flores, Richard Van Zyl Smit, Rosario Meddoza, Sameer Surka, Serena Van Haght, Yanira Hernandez; University of Western Cape (Cape Town, South Africa) Lungiswa Tsolekile. TUNISIA: University Hospital Farhat Hached (Sousse, Tunisia) Gouider Jeridi, Imed Harrabi, Jihen Maatoug, Lamia Boughammoura, Larbi Chaieb, Nejib Mrizek, Rafika Gaha; Faculty of Medicine of Sousse (Sousse, Tunisia) Khalifa Limam; Group of Occupational Health of Sousse (Sousse, Tunisia) Souad Amimi; Tunisian Association of Life and Earth Sciences Teachers, (Sousse, Tunisia) Karima Gaha, Tunisian Heart Foundation (Monastir, Tunisia) Habib Gamra. Duluth Medical research Institute, University of Minnesota (Duluth, USA) Mustafa al'Absi,National Institute for Health and Welfare (Helsinki, Finland) Erkki Vartiainen NATIONAL HEART, LUNG, AND BLOOD INSTITUTE: (Bethesda, MD, USA) Cornelius Moore, Debi Spillan, Kristiane Cooper, Megan Mitchell, Ruth Kirby, Yunling Gao. WESTAT: (Rockville, MD, USA) Emmanuel Aluko.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
The collaborators who made primary contributions to this report were Michael M Engelgau, Uchechukwu K. Sampson, Cristina Rabadan-Diehl, Richard Smith, Jaime Miranda, Gerald S. Bloomfield, Deshiree Belis, and K.M.Venkat Narayan.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, National Institutes of Health, the U.S. Department of Health and Human Services, or the UnitedHealth Group..
Conflict of Interest Disclosure: None
National Health, Lung, and Blood Institute-UnitedHealth Global Health Centers of Excellence Collaborators
ARGENTINA: Institute for Clinical Effectiveness and Health Policy (Buenos Aires, Argentina), Adolfo Rubinstein; Tulane University (New Orleans, Louisiana, USA) Jiang He.
BANGLADESH: International Centre for Diarrhoeal Disease Research, Bangladesh (Dhaka, Bangladesh) Dewan S Alam (current address: Centre for Global Health Research (Toronto, Canada), Johns Hopkins University (Baltimore, MD, USA) David H Peters. CHINA: The George Institute for Global Health (Beijing, China) Yangfeng Wu; Lijing L Yan; Duke Global Health Institute (Durham, North Carolina, USA) Michael Merson. GUATEMALA: Institute of Nutrition of Central America and Panama (Guatemala City, Guatemala) Manuel Ramirez; Johns Hopkins University (Baltimore, Maryland, USA), Benjamin Caballero. INDIA, BANGALORE: St. John's Research Institute (Bangalore, India) Denis Xavier; Population Health Research Institute (Ontario, Canada) Salim Yusuf. INDIA, NEW DELHI: Public Health Foundation of India, (New Delhi, India) Dorairaj Prabhakaran; Emory University (Atlanta, GA, USA) K.M.Venkat Narayan KM. KENYA: Moi University School of Medicine (Eldoret, Kenya) Sylvester Kimaiyo; Duke University (Durham, NC, USA) Eric Velazquez. MEXICO: El Colegio de Sonora (Hermosillo, Mexico) Catalina A Denman, Elsa Cornejo; University of Arizona (Tucson, AZ, USA) Jill de Zapien, Cecilia Rosales. PERU: Universidad Peruana Cayetano Heredia (Lima, Peru) J. Jaime Miranda; Johns Hopkins University (Baltimore, MD, USA) Robert H. Gilman. SOUTH AFRICA: University of Cape Town (Cape Town, South Africa) Naomi Levitt; Brigham and Women's Hospital (Boston, MA, USA) Thomas A Gaziano. TUNISIA: University Hospital Farhat Hached (Sousse, Tunisia) Hassen Ghannem; National Institute for Health and Welfare (Helsinki, Finland) Tiina Laatikainen. NATIONAL HEART, LUNG, AND BLOOD INSTITUTE (Bethesda, MD, USA): Cristina Rabadan-Diehl (current address: Office of Global Affairs, U.S. Department of Health & Human Services. Washington, DC); Michael M Engelgau, Deshiree Belis, Uchechukwu Sampson. UNITEDHEALTH GROUP (London, UK): Richard Smith (current address: International Centre for Diarrhoeal Disease Research, Bangladesh (London, UK). WESTAT: (Rockville, MD, USA) Nancy L Dianis, Tracy L Wolbach.
References
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Global Health Estimates: Deaths by Cause, Age, Sex, and Country, 2000-2012. Geneva: 2014. accessed. [Google Scholar]
- 3.Engelgau MME-SS, Kudesia P, Rajan V, Rosenhouse S, Okamoto K. Tackling Noncommunicable Diseases in South Asia. World Bank; Washington DC: 2011. Capitalizing on the Demographic Transition. [Google Scholar]
- 4.Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. The New England journal of medicine. 2015;372(14):1333–41. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine . Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. National Academies Press; Washington, DC: 2010. [PubMed] [Google Scholar]
- 6.World Economic Forum and World Health Organization From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries 2011. 2015 Feb 15; http://www3.weforum.org/docs/WEF_WHO_HE_ReducingNonCommunicableDiseases_2011.pdf.
- 7.World Health Organization [August 12 2015];Global action plan for the prevention and control of noncommunicable diseases 2013–2020. 2013 http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1.
- 8.Bloomfield GS, Baldridge A, Agarwal A, et al. Disparities in cardiovascular research output and citations from 52 African countries: a time-trend, bibliometric analysis (1999-2008). Journal of the American Heart Association. 2015;4(4) doi: 10.1161/JAHA.114.001606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UnitedHealth/ National Heart Lung Blood Institute Centers of Excellence Global response to non-communicable disease. Bmj. 2011;342:d3823. doi: 10.1136/bmj.d3823. [DOI] [PubMed] [Google Scholar]
- 10.UnitedHealth Group/National Heart, Lung Blood Institute Centres of Excellence A global research network for non-communicable diseases. Lancet. 2014;383(9927):1446–7. doi: 10.1016/S0140-6736(13)61808-5. [DOI] [PubMed] [Google Scholar]
- 11.Bloomfield GS. Xavier, Belis. COE Training Paper to be added. Global Heart. 2015;xx(xx):xx–xx. [Google Scholar]
- 12.Abrahams-Gessel S, Denman CA, Montano CM, et al. The training and fieldwork experiences of community health workers conducting population-based, noninvasive screening for CVD in LMIC. Glob Heart. 2015;10(1):45–54. doi: 10.1016/j.gheart.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaziano TA, Abrahams-Gessel S, Denman CA, et al. An assessment of community health workers' ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. The Lancet Global health. 2015;3(9):e556–63. doi: 10.1016/S2214-109X(15)00143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhodes EL, Dreibelbis R, Klasen EM, et al. Behavioral attitudes and preferences in cooking practices with traditional open-fire stoves in Peru, Nepal, and Kenya: implications for improved cookstove interventions. International journal of environmental research and public health. 2014;11(10):10310–26. doi: 10.3390/ijerph111010310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Checkley W, Ghannem H, Irazola V, et al. Management of NCD in low- and middle-income countries. Glob Heart. 2014;9(4):431–43. doi: 10.1016/j.gheart.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian M, Ajay VS, Dunzhu D, et al. A Cluster-Randomized, Controlled Trial of a Simplified Multifaceted Management Program for Individuals at High Cardiovascular Risk (SimCard Trial) in Rural Tibet, China, and Haryana, India. Circulation. 2015;132(9):815–24. doi: 10.1161/CIRCULATIONAHA.115.015373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khoury MJ, Lam TK, Ioannidis JP, et al. Transforming epidemiology for 21st century medicine and public health. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22(4):508–16. doi: 10.1158/1055-9965.EPI-13-0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauer MS. Time for a creative transformation of epidemiology in the United States. Jama. 2012;308(17):1804–5. doi: 10.1001/jama.2012.14838. [DOI] [PubMed] [Google Scholar]
- 19.Sorlie PD, Sholinsky P, Lauer MS. Reinvestment in Government-Funded Research: A Great Way to Share. Circulation. 2014 doi: 10.1161/CIRCULATIONAHA.114.014204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huser V, Sastry C, Breymaier M, Idriss A, Cimino JJ. Standardizing data exchange for clinical research protocols and case report forms: An assessment of the suitability of the Clinical Data Interchange Standards Consortium (CDISC) Operational Data Model (ODM). Journal of biomedical informatics. 2015 doi: 10.1016/j.jbi.2015.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jeong S, Kim HH, Park YR, Kim JH. Clinical Data Element Ontology for Unified Indexing and Retrieval of Data Elements across Multiple Metadata Registries. Healthcare informatics research. 2014;20(4):295–303. doi: 10.4258/hir.2014.20.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.al GTe Non-blood based CVD risk assessment. Global Heart. 2015;xx(xx):xx. [Google Scholar]
- 23.al Ie Hypertension Global Heart. 2015;xx(xx):xx. [Google Scholar]
- 24.Carillo-Larco High CVD Risk. Global Heart. 2015;xx(xx):xx. [Google Scholar]
- 25.al Se Diabetes. Global Heart. 2015;xx(xx):xx. [Google Scholar]
- 26.al Pe Obesity. Global Heart. 2015;xx(xx):xx. [Google Scholar]
- 27.Council on Foreign Relations The emerging global health crisis: Noncommunicable diseases in low- and middle-income countries. Independent Task Force Report No 72. 2014 accessed. [Google Scholar]
- 28.Ross JS, Lehman R, Gross CP. The importance of clinical trial data sharing: toward more open science. Circulation Cardiovascular quality and outcomes. 2012;5(2):238–40. doi: 10.1161/CIRCOUTCOMES.112.965798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.C3 Health [Oct 20, 2015];Global Health Score Care. http://www.ncdglobalscorecard.org/
- 30.Roman AV, Perez W, Smith R, South G. A scorecard for tracking actions to reduce the burden of non-communicable diseases. Lancet. 2015;386(9999):1131–2. doi: 10.1016/S0140-6736(15)00197-X. [DOI] [PubMed] [Google Scholar]
- 31.Falk-Krzesinski HJ, Borner K, Contractor N, et al. Advancing the science of team science. Clinical and translational science. 2010;3(5):263–6. doi: 10.1111/j.1752-8062.2010.00223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hall KL, Vogel AL, Stipelman B, Stokols D, Morgan G, Gehlert S. A Four-Phase Model of Transdisciplinary Team-Based Research: Goals, Team Processes, and Strategies. Translational behavioral medicine. 2012;2(4):415–30. doi: 10.1007/s13142-012-0167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogel AL, Stipelman BA, Hall KL, Nebeling L, Stokols D, Spruijt-Metz D. Pioneering the Transdisciplinary Team Science Approach: Lessons Learned from National Cancer Institute Grantees. Journal of translational medicine & epidemiology. 2014;2(2) [PMC free article] [PubMed] [Google Scholar]
- 34.Jaacks LM, Ali MK, Bartlett J, et al. Global Noncommunicable Disease Research: Opportunities and Challenges. Annals of internal medicine. 2015 doi: 10.7326/M15-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. [September 11, 2015];Health Affairs The Atlanta Declaration: A 21st Century Vision For US-Based Global Noncommunicable Disease Research. http://healthaffairs.org/blog/2015/09/09/the-atlanta-declaration-a-21st-century-vision-for-us-based-global-noncommunicable-disease-research/
- 36.Binanay CA AC, Aruasa W, Barasa FA, Corey GF, Crowe S, Esamai F, Einterz R, Foster MC, Gardner A, Kibosia J, Kimaiyo S, Koech M, Korir B, Lawrence JE, Lukas S, Manji I, Maritim P, Ogaro F, Park P, Pastakia SD, Sugut W, Vedanthan R, Yanoh RS, Velazquez EJ, Bloomfield GS. Building Sustainable Capacity for Cardiovascular Care at a Public Hospital in Western Kenya. J Am Coll Cardiol. 2015;66(22):2550–60. doi: 10.1016/j.jacc.2015.09.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Engelgau MM, Peprah E, Sampson UK, Mensah GA. A global health strategy to capitalize on proven-effective interventions for heart, lung, and blood diseases. Glob Heart. 2015;10(1):87–91. doi: 10.1016/j.gheart.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. [Feb 15 2015];Global Alliance for Chronic Diseases. http://www.gacd.org/
- 39. [Feb 15 2015];Global Alliance for Clean Cookstoves. http://cleancookstoves.org/
- 40. [Feb 15 2015];Medical Education Partnership Initiative. http://www.fic.nih.gov/programs/Pages/medical-education-africa.aspx.
- 41.National Heart Lung and Blood Institute [Feb 15 2015]; http://www.nhlbi.nih.gov/about/org/globalhealth/resources/OGHStrategicPlan%2007022012%20-%20FINAL.pdf. [PubMed]
- 42.National Heart L, and Blood Institute Global Health Think Tank Summary Statements and Recommendations [August 8, 2015]; http://www.nhlbi.nih.gov/research/reports/2014-global-health.
- 43.Mensah GA, Kiley J, Mockrin SC, et al. National Heart, Lung, and Blood Institute Strategic Visioning: Setting an Agenda Together for the NHLBI of 2025. American journal of public health. 2015:e1–e4. doi: 10.2105/AJPH.2015.302605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brende B, Hoie B. Towards evidence-based, quantitative Sustainable Development Goals for 2030. Lancet. 2015;385(9964):206–8. doi: 10.1016/S0140-6736(14)61654-8. [DOI] [PubMed] [Google Scholar]
- 45.Mayosi BM. The 10 'Best Buys' to combat heart disease, diabetes and stroke in Africa. Heart. 2013;99(14):973–4. doi: 10.1136/heartjnl-2013-304130. [DOI] [PubMed] [Google Scholar]
- 46.Vedanthan R. Global health delivery and implementation research: a new frontier for global health. MtSinai JMed. 2011;78(3):303–5. doi: 10.1002/msj.20250. [DOI] [PubMed] [Google Scholar]