Abstract
Background
Hypertension is the leading cause of cardiovascular disease and premature death worldwide. The prevalence of this public health problem is increasing in low-and-middle income countries (LMICs) both in urban and rural communities.
Objective
To examine hypertension prevalence, awareness, treatment, and control in adults 35-74 years old from urban and rural communities in LMICs in Africa, Asia and South America.
Methods
We analyzed data from 7 population-based cross-sectional studies in selected communities in nine LMICs that were conducted between 2008 and 2013. Age-gender standardized prevalence of pre-hypertension and hypertension were calculated. The prevalence of awareness, treatment and control of hypertension were estimated overall and by subgroups of age, gender and educational level.
Results
In selected communities, age-gender standardized prevalence of hypertension (95% confidence interval) among men and women aged 35-74 years was 49.9% (42.3, 57.4) in Kenya, 54.9% (51.3, 58.4) in South Africa, 52.5% (50.1, 54.8) in China, 32.5% (31.7, 33.3) in India, 42.3% (40.4, 44.2) in Pakistan, 45.4% (43.6, 47.2) in Argentina, 39.9% (37.8, 42.1) in Chile, 19.2% (17.8, 20.5) in Peru, and 44.1% (41.6, 46.6) in Uruguay. The proportion of awareness varied from 33.5% in India to 69.0% in Peru; the proportion of treatment among those who were aware of their hypertension varied from 70.8% in South Africa to 93.3% in Pakistan; and the proportion of blood pressure control varied from 5.3% in China to 45.9% in Peru.
Conclusions
Prevalence of hypertension varies widely in different communities. The rate of awareness, treatment and control also differs in different settings. There is a clear need to focus on increasing hypertension awareness and control in LMICs.
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death worldwide, and hypertension is the most important preventable risk factor for CVD (1). High blood pressure is associated with at least 7.6 million deaths per year worldwide (13.5% of all deaths) (2). High blood pressure causes significant morbidity, accounting for 7·0% of all global DALYs lost, mostly in low and middle income countries (LMICs) (3). Suboptimal blood pressure represents about 10% of the world’s overall healthcare expenditures (4). However, more than 90% of the expenditures on antihypertensive treatment, amounting about $50 billion each year (5), are spent in high-income countries. (6)
Additionally, it is estimated that three out of four individuals who suffer from hypertension live in LMICs. (7) Recently, many countries have undertaken large-scale health surveys and epidemiological studies that include measures of cardiovascular risk factors. (8) Hypertension prevalence is difficult to determine in such population surveys, however, since many of them are based on self-report only. Moreover, hypertension awareness and control are not possible to examine with self-report data. Thus, using data from multiple sources seems to be a useful way of retrieving information to tackle this relevant problem in public health.
The U.S. National Heart, Lung, and Blood Institute and the UnitedHealth (NHLBI/UHG) Chronic Disease Initiative have funded a global network of Centers of Excellence (COE) to help combat chronic diseases in developing countries. (9) Each center included a research institution in a developing country paired with at least one partner academic institution in a developed country. These COEs developed infrastructure for research and training, and conducted population-based and clinical research to monitor, prevent, or control chronic diseases. In seven of the studies conducted by these centers, blood pressure (BP) measurements were taken in random samples from the general population following standardized procedures. We sought to evaluate the original data from those studies with the aim of generating valuable information about the prevalence, awareness, treatment and control of hypertension in selected communities in Africa, Asia, and Latin America. (10-12)
POPULATION AND METHODS
In this study, we conducted a cross-sectional analysis using baseline data from seven population-based surveys from 44 communities in Kenya, South Africa, India, Pakistan, Peru and the Southern Cone of Latin America, including Argentina, Chile and Uruguay, and 120 villages from five provinces in China. The general characteristics of the surveys included are shown in Table 1. (13-17)
Table 1.
General Characteristics of the Studies from Nine Countries Included in the Analysis
| Africa | Asia | South America | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kenya | South Africa | China | India§ | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Survey year | 2012-2013 | 2008-2009 | 2012 | 2010-2012 | 2010-2011 | 2010-2011 | 2010-2011 | 2010-2012 | 2010-2011 |
|
| |||||||||
| Number of communities included in the survey |
1 | 4 | 120 villages (5 provinces) |
28 villages and 2 cities |
3 | 2 | 1 | 4 | 1 |
|
| |||||||||
| Urban/rural or semi-rural, n |
0/1 | 4/0 | 0/120 | 2/28 | 3/0 | 2/0 | 1/0 | 2/2 | 1/0 |
|
| |||||||||
| Sampling method | Random sampling |
Multistage probability sampling |
Random sampling |
Random sampling |
Multistage probability sampling |
Multistage probability sampling |
Multistage probability sampling |
Stratified random sampling |
Multistage probability sampling |
|
| |||||||||
| Number of respondents |
300 | 1,099 | 5922 | 19,549 | 4,016 | 3,990 | 1,950 | 3601 | 1,584 |
|
| |||||||||
| Response rate, % | 100 | 86.0 | 78.0 | 83.6-94.1 | 94.1 | 73.4* | 73.4* | 75.0 | 73.4* |
|
| |||||||||
| BP Device | Automated BP monitor |
Automated BP monitor |
Automated BP monitor |
Automated BP monitor |
Electronic sphygmoman ometer |
Standard aneroid sphygmoman ometer |
Standard aneroid sphygmoman ometer |
Automated BP monitor |
Standard aneroid sphygmoman ometer |
|
| |||||||||
| BP measurement setting |
Home and Clinic |
Home and Community |
Clinic | Home and camps |
Home and camps |
Clinic | Clinic | Clinic | Clinic |
|
| |||||||||
| Number of BP measurements, |
3 | 3 | 2 | 3 | 3 | 3 | 3 | 3 | 3 |
|
| |||||||||
| Resting time before BP measurement, min |
15-30 | 5 | 15 | 5-10 | 5 | 5 | 5 | 5 | 5 |
|
| |||||||||
| Resting time between BP measurements, min |
10-20 | 2 | 5 | 0.5 -5 | 0.5 | 5 | 5 | 5 | 5 |
Includes data from one study in Bangalore, and one study in New Delhi and Chennai.
Pooled estimate for Argentina, Chile and Uruguay
Study participants
We included men and women between 35 and 74 years old that were randomly selected from the general population in each of the studies. The response rate of each study included in the analysis was above 70%.
Data collection
Standard sphygmomanometers or automatic BP monitors were used for BP measurements by trained research personnel in all the studies. In 6 studies, BP was measured at a clinic visit while in 2 studies BP measurements were taken both at home and at a clinic visit. All surveys had at least 2 BP measurements recorded with the participant in the seated position after at least 5 min of rest, and the average value was calculated to define the BP measurement at baseline. The rest period between BP measurements was 30 seconds in one study, and varied between 2 and 10 minutes in the rest of the surveys.
Hypertension was defined as systolic BP (SBP) ≥140 and/or diastolic BP (DBP) ≥90 mmHg, or report of current use of antihypertensive medication. Hypertension awareness was defined as the number of individuals who reported either having been diagnosed with hypertension by a health professional or taking medication for high BP, divided by the total number of hypertensives. Prevalence of treatment was calculated in two different ways: 1- as the number of hypertensive individuals who reported taking medication for high BP, divided by the total number of hypertensives that were aware of their condition, and 2- the number of hypertensive individuals who reported taking medication for high BP, divided by the total number of hypertensives. Hypertension control was also expressed in two different ways: 1- as the number of hypertensive individuals with SBP < 140 mmHg and DBP < 90 mmHg divided by the total number of hypertensives who reported taking medication at the time of the interview, and 2- as the number of hypertensive individuals with SBP < 140 mmHg and DBP < 90 mmHg divided by the total number of hypertensive subjects. Pre-hypertension was defined as SBP between 120-139 mm Hg and/or DBP between 80-89 mmHg in the absence of a diagnosis of hypertension or treatment with medication for high BP.
Education was categorized into three groups: no formal education, any school, and university or higher. Age was categorized into four groups: 35-44, 45-54, 55-64 and 65-74 years old. Body Mass Index (BMI) was categorized into three groups: < 25, 25-30, and >30 kg/m2. Central obesity was defined as waist circumference ≥102 cm for men or ≥88 cm for women. (18) For India and Pakistan, central obesity was defined waist circumference ≥90 cm for men or ≥80 cm for women. (19)
STATISTICAL ANALYSIS
Datasets and data dictionaries from each study were collected and analyzed centrally by the Administrative Coordinating Center of the COE program. A standardized process of harmonization was carried out which yielded a Common Data Base of parallel variables that were selected and recoded as a basis for aggregated research. (Uchechukwu Global Heart 2015 Theme Issue) Results are presented as absolute frequency and percentages for categorical variables and mean ± standard deviation for continuous variables. Weighted prevalence and its 95% confidence interval were calculated for each site using appropriate weights according to the sampling method employed in each of the 7 studies. (20) To enable comparison among sites, we conducted age and sex direct standardization using the World Health Organization (WHO) world population in 2010. (21, 22) All data analyses were conducted using SAS 9.3 (SAS Institute, Cary NC) and Stata 13.0 (StataCorp. 2013. College Station, TX: StataCorp LP)
RESULTS
Characteristics of the study population
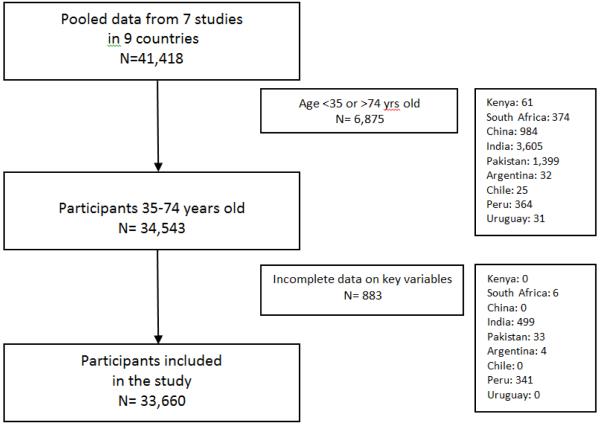
Our pooled database contained 42,011 participants from 7 epidemiological studies conducted in 9 countries. We then excluded participants who were not between 35 and 74 years old (n=7,468). We further excluded 883 individuals from the analysis due to incomplete data on SBP or DBP in the pooled dataset. Our final analysis included 33,660 individuals. The final sample sizes for individual studies ranged from 239 in selected communities in Kenya to 14,813 in India. Our inclusion/exclusion scheme is shown in Figure 1. In all the countries the proportion of men in the sample was lower than women. The number of individuals included with no formal education ranged from 0% in communities from Kenya to almost 33% in communities from Pakistan. Conversely, the percentage of people with university level or higher varied from 0% in communities from Kenya and South Africa to 32.5% in Temuco, Chile. The percentage of current smokers varied between 25.9% and 38.5% across sites. The percentage of current alcohol drinkers was lowest in communities from Pakistan (1.7%), and ranged from 7.1% to 56.1% in the rest of the sites. (Table 2)
Figure 1.
Population from the harmonized common database included in the study.
Table 2.
Characteristics of the Study Participants
| Africa | Asia | South America | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kenya | South Africa | China | India | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Number of participants | 239 | 736 | 4,938 | 14,813 | 2,584 | 3,954 | 1,925 | 2,918 | 1,553 |
|
| |||||||||
| Gender | |||||||||
| Men | 89 (37.2%) | 269 (36.5%) | 2,395 (48.5%) | 7,056 (47.6%) | 1,213 (46.9%) | 1,576 (39.9%) | 918 (47.7%) | 1,404 (48.1%) | 642 (41.3%) |
| Women | 150 (62.8%) | 467 (63.5%) | 2,543 (51.5%) | 7,757 (52.4%) | 1,371 (53.1%) | 2,378 (60.1%) | 1,007 (52.3%) | 1,514 (51.9%) | 911 (58.7%) |
|
| |||||||||
| Age groups, years | |||||||||
| 35-44 | 39 (16.3%) | 260 (35.3%) | 320 (6.5%) | 5,760 (38.9%) | 1,096 (42.4%) | 884 (22.4%) | 461 (24.0%) | 729 (25.0%) | 344 (22.1%) |
| 45-54 | 58 (24.3%) | 251 (34.1%) | 638 (12.9%) | 4,391 (29.6%) | 792 (30.7%) | 1,140 (28.8%) | 536 (27.8%) | 822 (28.2%) | 396 (25.5%) |
| 55-64 | 72 (30.1%) | 149 (20.3%) | 2,155 (43.6%) | 2,847 (19.2%) | 463 (17.9%) | 1,179 (29.8%) | 494 (25.7%) | 826 (28.3%) | 441 (28.4%) |
| 65-74 | 70 (29.3%) | 76 (10.3%) | 1,825 (37.0%) | 1,815 (12.3%) | 233 (9.0%) | 751 (19.0%) | 434 (22.5%) | 541 (18.5%) | 372 (24.0%) |
|
| |||||||||
| Education | |||||||||
| None | 0 (0%) | 95 (12.9%) | 1,088 (22.1%) | 4,354 (29.4%) | 850 (32.9%) | 52 (1.3%) | 9 (0.5%) | 168 (5.8%) | 12 (0.8%) |
| Any School | 239 (100%) | 641 (87.1%) | 3,835 (77.8%) | 9,046 (61.1%) | 1,407 (54.4%) | 3,120 (79.6%) | 1,277 (67.0%) | 2,123 (72.7%) | 1,359 (88.7%) |
| University/Higher | 0 (0%) | 0 (0%) | 7 (0.1%) | 1,413 (9.5%) | 327 (12.7%) | 750 (19.1%) | 621 (32.5%) | 627 (21.5%) | 161 (10.5%) |
|
| |||||||||
| Body-mass Index, kg/m2 | |||||||||
| < 25 | 48 (20.1%) | 227 (30.8%) | 2,942 (59.6%) | 9,165 (68.5%) | 839 (42.7%) | 945 (24.0%) | 368 (19.1%) | 818 (28.0%) | 416 (26.9%) |
| 25-30 | 116 (48.5%) | 151 (20.5%) | 1,662 (33.7%) | 2,913 (21.8%) | 684 (34.8%) | 1,409 (35.7%) | 873 (45.4%) | 1,286 (44.1%) | 518 (33.5%) |
| ≥30 | 75 (31.4%) | 358 (48.6%) | 332 (6.7%) | 1,302 (9.7%) | 442 (22.5%) | 1,592 (40.3%) | 683 (35.5%) | 814 (27.9%) | 612 (39.6%) |
|
| |||||||||
| Central Obesity | (*) | 422 (57.4%) | (*) | 5,792 (39.4%) | 1,777 (69.3%) | 2,172 (55.0%) | 1,073 (55.8%) | 1,234 (42.3%) | 968 (62.5%) |
|
| |||||||||
| Current Smoking | (*) | 190 (25.9%) | 1,492 (30.2%) | 5,703 (38.5%) | 756 (29.3%) | 1,038 (26.3%) | 525 (27.3%) | (*) | 426 (27.9%) |
|
| |||||||||
| Current Alcohol Intake | 17 (7.1%) | (*) | 1,068 (21.6%) | 2401 (16.2%) | 45 (1.7%) | 1,622 (41.4%) | 738 (38.6%) | 1,637 (56.1%) | 723 (47.1%) |
Values are expressed as n (%). (*) Information not available
Blood pressure measures
There was significant variation in SBP and DBP among sites. The mean values of SBP and DBP were highest in communities from Kenya and China, both for men and women, and lowest in Peru. Other features of the study population, including heart rate, height, weight, and waist circumference by gender are shown in Table 3.
Table 3.
Anthropometric and Blood Pressure Measures by Gender
| Africa | Asia | South America | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kenya | South Africa | China | India | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Men | |||||||||
| SBP, mm Hg | 146.2 (140.0, 152.4) |
135.8 (132.9, 138.7) |
142.8 (141.9, 143.7) |
127.7 (127.2, 128.2) |
127.2 (126.0, 128.3) |
129.1 (128.2, 130.0) |
129.7 (128.5, 131.0) |
122.1 (121.3, 123.0) |
131.7 (130.1, 133.2) |
| DBP, mm Hg | 83.6 (80.5, 86.7) |
85.2 (83.6, 86.8) |
87.3 (86.8, 87.9) |
82 (81.7, 82.3) |
82.9 (82.2, 83.6) |
86.7 (86.1, 87.3) |
83.4 (82.6, 84.3) |
75.8 (75.3, 76.4) |
83.6 (82.6, 84.5) |
| Heart rate, beats/min | 82.0 (79.5, 84.5) |
67.4 (65.9, 68.9) |
74.4 (73.9, 74.9) |
79.1 (78.7, 79.6) |
80.1 (79.4, 80.8) |
67.4 (66.9, 67.9) |
65.7 (65.1, 66.4) |
68.3 (67.7, 68.8) |
68.3 (67.4, 69.1) |
| Height, cm | 157.0 (155.2, 158.8) |
169.5 (168.7, 170.4) |
165.8 (165.5, 166.0) |
163.3 (163.2, 163.5) |
166.4 (166.0, 166.8) |
170.7 (170.3, 171.1) |
168.8 (168.2, 169.3) |
162.8 (162.5, 163.2) |
171.1 (170.6, 171.7) |
| Weight, kg | 70.3 (68.0, 72.6) |
70.9 (68.9, 73.0) |
66.2 (65.8, 66.6) |
59.9 (59.6, 60.3) |
69.2 (68.3, 70.2) |
83.7 (82.8, 84.7) |
81.4 (80.4, 82.4) |
71.6 (71.0, 72.3) |
81.7 (80.3, 83.1) |
| Waist Circumference, cm |
(*) | 88.4 (86.7, 90.1) |
(*) | 84.8 (84.4, 85.1) |
93.4 (92.7, 94.2) |
98.6 (97.8, 99.3) |
98.5 (97.7, 99.3) |
93.2 (92.7, 93.8) |
98.5 (97.4, 99.7) |
|
| |||||||||
| Women | |||||||||
| SBP, mm Hg | 149.7 (144.9, 154.6) |
129.1 (126.9, 131.3) |
147.2 (146.3, 148.0) |
125.1 (124.6, 125.5) |
123.6 (122.4, 124.9) |
126.0 (125.1, 126.8) |
122.7 (121.5, 123.9) |
113.3 (112.4, 114.3) |
127.5 (126.1, 128.8) |
| DBP, mm Hg | 86.1 (83.6, 88.6) |
84.6 (83.4, 85.8) |
86.4 (85.9, 87.0) |
80.2 (80.0, 80.5) |
82.1 (81.4, 82.8) |
81.8 (81.3, 82.3) |
79.3 (78.5, 80.0) |
71.4 (70.8, 71.9) |
79.8 (79.1, 80.6) |
| Heart rate, beats/min | 82.2 (80.2, 84.2) |
72.4 (71.3, 73.5) |
77.7 (77.3, 78.2) |
81.8 (81.3, 82.2) |
82.3 (81.7, 82.9) |
67.7 (67.3, 68.2) |
69.4 (68.8, 70.0) |
71.9 (71.4, 72.4) |
70.7 (70.0, 71.3) |
| Height, cm | 156.8 (155.8, 157.8) |
158.5 (157.9, 159.1) |
153.5 (153.2, 153.7) |
150.7 (150.6, 150.9) |
152.3 (152.0, 152.7) |
156.8 (156.4, 157.1) |
155.7 (155.3, 156.2) |
150.3 (150.0, 150.6) |
157.7 (157.3, 158.1) |
| Weight, kg | 68.9 (67.3, 70.6) |
85.5 (83.6, 87.5) |
58.5 (58.1, 58.9) |
53.5 (53.1, 53.8) |
63.6 (62.7, 64.4) |
70.7 (70.0, 71.4) |
71.0 (70.1, 71.9) |
64.7 (64.1, 65.3) |
73.3 (72.2, 74.4) |
| Waist Circumference, cm |
(*) | 99.7 (98.4, 100) |
(*) | 79.3 (79.0, 79.6) |
89.6 (88.9, 90.3) |
92.0 (91.3, 92.6) |
94.3 (93.5, 95.2) |
91.1 (90.5, 91.6) |
98.4 (97.3, 99.5) |
Values are expressed in units of measurement (95%CI). (*) Information not available
Crude and standardized prevalence of hypertension
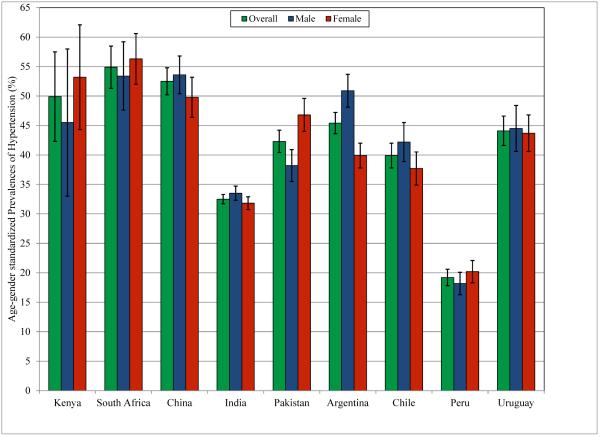
Table 4 shows the age-gender standardized and weighted prevalence of hypertension, overall and by gender, age group and educational level for each study. Figure 2 shows the age-standardized prevalence of hypertension by gender for each study. In Africa, in the village from Kenya, the age-gender standardized prevalence of hypertension among adults aged 35-74 years was 49.9% (95%CI 42.3, 57.4) while in South Africa, the pooled age-gender standardized prevalence from the four urban communities included in the survey was 54.9% (95%CI 51.3, 58.4). In Asia, in the communities included in China, the prevalence of hypertension was 52.5% (95%CI 50.1, 54.8) while in those communities included in India and Pakistan, it reached 32.5% (31.7, 33.3) and 42.3% (95%CI 40.4, 44.2), respectively. In Latin America, in the 4 cities from 3 countries of the Southern Cone (Argentina, Chile and Uruguay) the prevalence of hypertension was 45.4% (95%CI 43.6, 47.2), 39.9% (95%CI 37.8-42.1), and 44.1% (95%CI 41.6, 46.6), respectively. In the study from Peru that included 4 communities, two urban and two semi-rural/rural, the age-standardized prevalence of hypertension was 19.2% (95%CI 17.8, 20.5).
Table 4.
Age-Gender Standardized Prevalence of Hypertension
| Africa | Asia | South America | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kenya | South Africa | China | India | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Unstandardized weighted total |
53.6 (47.2, 59.9) | 55.3 (51.7, 58.9) | 65.6 (64.3, 66.9) | 32.1 (31.3, 32.9) | 40.8 (38.9, 42.7) | 45.5 (43.7, 47.4) | 38.5 (36.2, 40.8) | 22.4 (20.9, 23.9) | 46.5 (43.9, 49.1) |
|
| |||||||||
| Age-gender standardized total |
49.9 (42.3, 57.4) | 54.9 (51.3, 58.4) | 52.5 (50.1, 54.8) | 32.5 (31.7, 33.3) | 42.3 (40.4, 44.2) | 45.4 (43.6, 47.2) | 39.9 (37.8, 42.1) | 19.2 (17.8, 20.5) | 44.1 (41.6, 46.6) |
|
| |||||||||
| Sex | |||||||||
| Men | 45.5 (33.0, 58.0) | 53.4 (47.6, 59.2) | 53.6 (50.4, 56.9) | 33.5 (32.3, 34.7) | 38.2 (35.5, 40.9) | 50.9 (48.1, 53.8) | 42.2 (38.9, 45.4) | 18.2 (16.3, 20.2) | 44.5 (40.6, 48.3) |
| Women | 53.2 (44.3, 62.0) | 56.3 (52.0, 60.6) | 49.8 (46.4, 53.2) | 31.8 (30.7, 32.9) | 46.8 (44.0, 49.6) | 39.9 (37.8, 42.0) | 37.7 (34.9, 40.4) | 20.2 (18.3, 22.0) | 43.7 (40.6, 46.7) |
|
| |||||||||
| Age groups, years | |||||||||
| 35-44 | 35.0 (18.9, 51.1) | 36.5 (30.4, 42.6) | 38.2 (32.9, 43.5) | 21.7 (20.5, 22.8) | 27.4 (24.6, 30.1) | 28.5 (25.1, 31.9) | 21.9 (18.1, 25.6) | 9.2 (7.1, 11.3) | 22.2 (17.8, 26.7) |
| 45-54 | 62.0 (49.0, 75.0) | 61.2 (54.8, 67.5) | 48.6 (44.3, 52.8) | 32.6 (31.1, 34.1) | 42.8 (39.3, 46.3) | 43.3 (40.0, 46.6) | 37.6 (33.4, 41.7) | 16.4 (13.9, 19.0) | 43.2 (38.3, 48.2) |
| 55-64 | 53.7 (41.7, 65.7) | 69.5 (61.9, 77.1) | 66.6 (64.6, 68.6) | 42.5 (40.5, 44.4) | 57.7 (53.1, 62.2) | 60.3 (57.2, 63.3) | 56.1 (51.7, 60.5) | 26.6 (23.6, 29.6) | 63.3 (58.8, 67.9) |
| 65-74 | 54.2 (42.6, 65.8) | 69.4 (58.8, 80.0) | 73.8 (71.7, 75.9) | 48.6 (46.1, 51.0) | 61.0 (54.0, 67.9) | 74.8 (71.2, 78.4) | 71.3 (67.1, 75.5) | 42.6 (38.5, 46.8) | 78.0 (73.7, 82.2) |
|
| |||||||||
| Education | |||||||||
| None | (**) | 62.6 (51.8, 73.3) | 51.4 (40.7, 62.0) | 27.1 (25.6, 28.6) | 39.1 (35.6, 42.7) | 44.0 (25.9, 62.0) | 64.8 (31.8, 97.7) | 20.6 (6.0, 35.3) | 59.8 (45.1, 74.4) |
| Any School | 49.9 (42.3, 57.4) | 53.8 (49.9, 57.6) | 51.9 (49.5, 54.3) | 33.2 (32.1, 34.3) | 43.4 (40.8, 46.1) | 47.0 (44.9, 49.0) | 41.6 (38.8, 44.4) | 19.5 (17.9, 21.1) | 45.3 (42.6, 48.0) |
| University/Higher | (**) | (**) | 57.7 (38.1, 77.3) | 43.0 (40.1, 45.9) | 39.4 (33.7, 45.1) | 41.1 (37.5, 44.8) | 36.0 (32.4, 39.5) | 18.0 (1.0, 21.1) | 33.5 (26.9, 40.1) |
Values are percentage (95% confidence interval). (**) Not applicable.
Figure 2.
Age-gender Standardized Prevalence of Hypertension by Country (95% Confidence Interval).
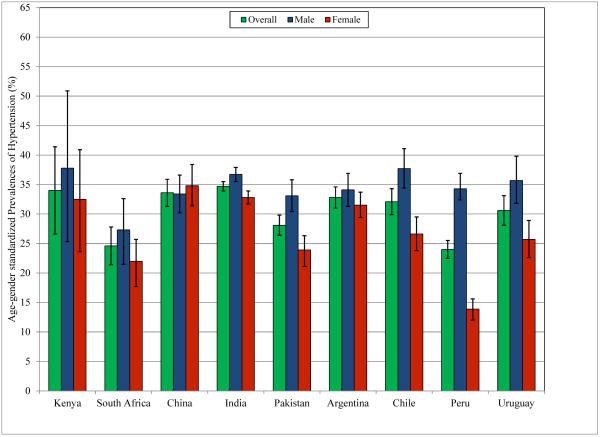
Crude and standardized prevalence of pre-hypertension
Table 5 shows the age-gender standardized and weighted prevalence of pre-hypertension, overall and by gender, age group and educational level for each study. Figure 3 shows the age-standardized prevalence of pre-hypertension by gender. The overall age-gender standardized prevalence of pre-hypertension ranged from 24.0% in the sites from Peru, and 24.6% in South Africa to values near or above 30% in those communities included in Pakistan, Uruguay, Chile, Argentina, China, Kenya and India.
Table 5.
Age-Gender Standardized Prevalence of Pre-hypertension
| Africa | Asia | South America | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kenya | South Africa | China | India | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Unstandardized weighted total |
31.0 (25.1, 36.8) | 24.0 (21.0, 27.1) | 25.7 (24.5, 26.9) | 34.7 (33.9, 35.5) | 28.2 (26.4, 29.9) | 31.2 (30.2, 32.3) | 31.9 (29.6, 34.2) | 24.2 (22.7, 25.8) | 29.7 (27.2, 32.2) |
|
| |||||||||
| Age-gender standardized total |
34.0 (26.6, 41.3) | 24.6 (21.4, 27.9) | 33.6 (31.3, 35.9) | 34.7 (33.9, 35.5) | 28.1 (26.4, 29.9) | 32.8 (31.0, 34.6) | 32.1 (29.9, 34.3) | 24.0 (22.5, 25.6) | 30.6 (28.1, 33.2) |
|
| |||||||||
| Sex | |||||||||
| Men | 37.8 (24.7, 50.9) | 27.3 (22, 32.6) | 33.4 (30.2, 36.6) | 36.7 (35.5, 37.9) | 33.1 (30.4, 35.8) | 34.1 (31.3, 36.9) | 37.7 (34.3, 41.0) | 34.3 (31.7, 36.9) | 35.7 (31.6, 39.7) |
| Women | 32.5 (24.1, 40.8) | 22.0 (18.3, 25.7) | 34.8 (31.2, 38.3) | 32.8 (31.7, 33.9) | 23.9 (21.5, 26.4) | 31.5 (29.3, 33.7) | 26.6 (23.7, 29.5) | 13.9 (12.2, 15.7) | 25.7 (22.5, 28.8) |
|
| |||||||||
| Age groups, years | |||||||||
| 35-44 | 48.8 (31.3, 66.2) | 32.5 (26.6, 38.4) | 41.9 (36.5, 47.2) | 38.2 (36.9, 39.6) | 30.2 (27.4, 33.1) | 37.5 (33.9, 41.1) | 35.7 (31.4, 40.0) | 21.8 (19.0, 24.7) | 37.9 (32.7, 43.0) |
| 45-54 | 23.8 (12.2, 35.3) | 22.8 (17.3, 28.3) | 36.1 (32.0, 40.2) | 34.6 (33.1, 36.2) | 29.5 (26.3, 32.7) | 35.9 (32.7, 39.1) | 32.6 (28.6, 36.5) | 24.9 (22.0, 27.8) | 31.9 (27.2, 36.5) |
| 55-64 | 31.1 (20.0, 42.1) | 17.8 (11.4, 24.1) | 26.3 (24.4, 28.2) | 31.4 (29.6, 33.2) | 25.4 (21.4, 29.3) | 28.6 (25.7, 31.4) | 32.8 (28.7, 36.9) | 26.7 (23.7, 29.7) | 23.5 (19.5, 27.5) |
| 65-74 | 28.5 (18.0, 39.0) | 17.2 (8.4, 26.0) | 19.4 (17.5, 21.3) | 30.4 (28.2, 32.6) | 26.1 (19.8, 32.4) | 18.5 (15.3, 21.8) | 19.2 (15.5, 22.9) | 24.1 (20.5, 27.6) | 18.4 (14.4, 22.4) |
|
| |||||||||
| Education | |||||||||
| None | (**) | 20.6 (11.1, 30.0) | 38.1 (26.7, 49.5) | 38.1 (26.7, 49.5) | 26.8 (23.4, 30.2) | 20.4 (6.0, 34.7) | 35.2 (2.3, 68.2) | 17.2 (8.0, 26.4) | 10.6 (0.0, 25.2) |
| Any School | 34 (26.6, 41.3) | 25.4 (21.9, 28.9) | 33.8 (31.4, 36.1) | 33.8 (31.4, 36.1) | 28.1 (25.7, 30.5) | 31.9 (29.8, 34) | 32.3 (29.5, 35.2) | 24.1 (22.3, 26) | 29 (26.2, 31.7) |
| University/Higher | (**) | (**) | 43.0 (29.3, 56.8) | 34.5 (31.6, 37.3) | 28.2 (22.9, 33.5) | 35.8 (31.9, 39.7) | 32.1 (28.4, 35.8) | 23 (19.9, 26.2) | 42.6 (35.3, 49.9) |
Values are percentage (95% confidence interval). (**) Not applicable.
Figure 3.
Age-gender Standardized Prevalence of Pre-Hypertension by country (95% Confidence Interval).
Awareness, treatment and control
Table 6 shows the age-gender standardized prevalence of hypertension awareness, treatment and control, overall and by gender, age group and educational level for each study. Awareness of hypertension was higher in the sites from Peru, Chile, South Africa, Pakistan, Uruguay and Argentina (69.0, 65.9, 61.5, 62.4, 64.5 and 52.7%, respectively), and was lower in the sites from China, and India (38.9 and 33.5%, respectively). Across all sites analyzed, the proportion of participants aware of their condition that were receiving treatment was around or above 75%, while between 33% and 63% of the total number of hypertensive subjects were receiving pharmacological treatment in different communities. Blood pressure control rates among treated subjects varied broadly between 16.2% in the communities in China to 71.2% in communities from Peru. Among all hypertensives, the control rate varied from very low rates in communities in China (5.3%) and India (10.1%) through 45.9% in Peru. No data were available for Kenya.
Table 6.
Age-Gender Standardized Prevalence of Awareness, Treatment and Control of Hypertension, Overall and by Participants’ Characteristics§
| Africa | Asia | South America | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| South Africa | China | India | Pakistan | Argentina | Chile | Peru | Uruguay | |
| Awareness | ||||||||
|
| ||||||||
| Overall | 61.5 (56.7, 66.3) | 38.9 (35.9, 41.8) | 33.5 (32.0, 35.0) | 62.4 (59.4, 65.4) | 52.7 (49.6, 55.7) | 65.9 (61.8, 70.0) | 69.0 (64.4, 73.5) | 64.5 (59.9, 69.1) |
|
| ||||||||
| Sex | ||||||||
| Men | 46.1 (38.4, 53.7) | 31.6 (28.3, 34.9) | 26.3 (24.3, 28.2) | 50.0 (45.1, 54.9) | 43.6 (39.3, 47.9) | 56.0 (50.3, 61.6) | 51.4 (44.2, 58.7) | 49.9 (42.9, 56.9) |
| Women | 76.3 (70.7, 81.9) | 45.5 (40.0, 50.9) | 40.7 (38.4, 43.0) | 75.2 (71.6, 78.8) | 61.9 (57.5, 66.2) | 76.6 (70.5, 82.7) | 87.1 (82.0, 92.1) | 80.1 (74.6, 85.6) |
|
| ||||||||
| Age groups, years | ||||||||
| 35-44 | 44.4 (35.1, 53.7) | 17.6 (10.7, 24.5) | 23.9 (21.2, 26.6) | 57.6 (51.8, 63.4) | 40.7 (33.8, 47.5) | 51.6 (41.9, 61.4) | 60.6 (50.8, 70.4) | 56.8 (46.7, 66.9) |
| 45-54 | 64.9 (57.0, 72.7) | 45.8 (39.6, 51.9) | 35.7 (33.0, 38.4) | 61.6 (56.3, 66.8) | 51.2 (46.3, 56.0) | 71.6 (65.5, 77.7) | 76.2 (69.2, 83.3) | 61.3 (54.1, 68.5) |
| 55-64 | 71.9 (62.9, 80.8) | 52.2 (49.6, 54.7) | 43.7 (40.6, 46.7) | 68.4 (62.8, 74.0) | 64.8 (60.9, 68.7) | 74.5 (69.4, 79.5) | 72.1 (66.4, 77.8) | 76.7 (71.6, 81.8) |
| 65-74 | 84.8 (74.8, 94.7) | 60.5 (57.8, 63.2) | 39.7 (36.2, 43.2) | 70.7 (63.3, 78.0) | 72.1 (67.8, 76.4) | 83.5 (79.3, 87.6) | 74.3 (68.7, 79.9) | 78.9 (74.2, 83.6) |
|
| ||||||||
| Education | ||||||||
| None | 56.3 (44.8, 67.8) | 30.6 (23.6, 37.6) | 21.3 (18.5, 24.0) | 54.4 (48.2, 60.6) | 24.3 (1.0, 47.6) | 53.0 (47.8, 58.2) | 83.9 (64.9, 100) | (**) |
| Any School | 62.3 (57.0, 67.5) | 38.9 (35.8, 41.9) | 35.7 (33.8, 37.6) | 64.2 (60.4, 68.0) | 52.5 (49.0, 56.0) | 66.9 (61.7, 72.0) | 63.0 (57.6, 68.4) | 64.0 (59.1, 68.9) |
| University/Higher | (**) | (**) | 52.2 (47.6, 56.7) | 65.5 (56.1, 74.9) | 55.6 (48.9, 62.3) | 64.5 (57.4, 71.5) | 85.5 (78.7, 92.3) | 66.0 (50.6, 81.3) |
|
| ||||||||
| Treatment1 | ||||||||
|
| ||||||||
| Overall | 70.8 (63.8, 77.8) | 81.2 (74.0, 88.5) | 89.9 (87.7, 92.0) | 93.3 (90.9, 95.8) | 78.2 (73.8, 82.6) | 78.9 (73.7, 84.1) | 90.8 (87.1, 94.4) | 87.3 (82.6, 92.1) |
|
| ||||||||
| Sex | ||||||||
| Men | 62.3 (48.1, 76.5) | 78.0 (65.1, 90.8) | 88.8 (85.1, 92.4) | 92.4 (87.7, 97.0) | 70.9 (63.6, 78.2) | 67.6 (59.2, 76.1) | 84.4 (75.8, 93.0) | 83.3 (73.9, 92.6) |
| Women | 77.3 (70.8, 83.8) | 85.5 (76.8, 94.2) | 90.7 (88.1, 93.2) | 94.8 (92.4, 97.2) | 85.3 (80.6, 90.0) | 89.9 (84.2, 95.6) | 96.1 (94.0, 98.2) | 90.6 (86.1, 95.2) |
|
| ||||||||
| Age groups, years | ||||||||
| 35-44 | 62.8 (44.9, 80.8) | 74.1 (53.8, 94.5) | 86.0 (80.8, 91.2) | 89.8 (83.7, 95.9) | 66.8 (56.4, 77.1) | 66.5 (54.0, 79.0) | 92.2 (82.3, 100) | 83.4 (70.6, 96.1) |
| 45-54 | 74.6 (64.4, 84.8) | 84.0 (77.9, 90.1) | 88.1 (84.6, 91.7) | 93.6 (89.6, 97.7) | 76.1 (69.5, 82.6) | 82.2 (75.7, 88.6) | 85.8 (78.5, 93.2) | 88.1 (81.5, 94.7) |
| 55-64 | 68.8 (57.3, 80.2) | 87.1 (84.7, 89.6) | 94.5 (92.4, 96.7) | 98.5 (96.7, 100) | 90.1 (87.1, 93.2) | 87.0 (82.4, 91.6) | 92.2 (87.8, 96.7) | 87.2 (82.4, 92.0) |
| 65-74 | 81.3 (70.1, 92.5) | 89.7 (87.5, 91.9) | 96.3 (94.0, 98.6) | 96.4 (92.4, 100) | 96.4 (94.3, 98.5) | 93.8 (90.8, 96.7) | 91.8 (87.6, 96.1) | 94.5 (91.5, 97.6) |
|
| ||||||||
| Education | ||||||||
| None | 79.2 (66.1, 92.3) | 84.9 (75.1, 94.7) | 85.4 (77.9, 92.9) | 91.4 (85.5, 97.3) | 89.2 (79.4, 99.0) | 71.9 (62.1, 81.7) | 94.8 (78.2, 100) | (**) |
| Any School | 70.6 (63.1, 78.1) | 80.7 (73.4, 88.0) | 90.6 (87.9, 93.3) | 95.0 (92.2, 97.8) | 78.1 (73.0, 83.2) | 75.6 (69.0, 82.2) | 90.4 (85.7, 95.2) | 87.0 (81.8, 92.2) |
| University/Higher | (**) | (**) | 92.3 (88.3, 96.3) | 86.3 (76.7, 95.9) | 78.9 (70.2, 87.5) | 84.8 (76.6, 93) | 91.9 (86.2, 97.5) | 91.3 (80.3, 100) |
|
| ||||||||
| Treatment2 | ||||||||
|
| ||||||||
| Overall | 45.2 (40.5, 50.0) | 32.9 (30.1, 35.6) | 41.0 (39.0, 43.0 | 56.0(52.9, 59.2) | 43.0 (40.2, 45.7) | 54.3 (50.3, 58.2) | 63.2 (58.6, 67.8) | 57.0 (52.4, 61.6) |
|
| ||||||||
| Sex | ||||||||
| Men | 30.4 (23.5, 37.3) | 25.7 (22.7, 28.6) | 32.0 (29.3, 34.6) | 42.4 (37.4, 47.4) | 33.1 (29.4, 36.7) | 40.0 (34.9, 45.1) | 43.4 (36.3, 50.5) | 42.1 (35.4, 48.8) |
| Women | 59.4 (53.1, 65.6) | 39.8 (34.7, 44.9) | 49.9 (46.9, 52.9) | 70.3 (66.4, 74.1) | 53.3 (49.0, 57.5) | 69.3 (62.8, 75.8) | 83.6 (78.3, 88.9) | 72.6 (66.5, 78.7) |
|
| ||||||||
| Age groups, years | ||||||||
| 35-44 | 29.4 (20.9, 37.9) | 13.3 (7.1, 19.4) | 24.7 (21.0, 28.3) | 48.0 (42.0, 54.0) | 28.4 (22.3, 34.5) | 36.5 (27.1, 45.9) | 57.9 (48.3, 67.4) | 48.8 (38.6, 58.9) |
| 45-54 | 50.7 (43.1, 58.3) | 38.7 (32.6, 44.8) | 41.0 (37.5, 44.5) | 55.9 (50.4, 61.3) | 39.9 (35.3, 44.5) | 59.9 (53.5, 66.3) | 66.3 (58.6, 74.0) | 54.2 (46.9, 61.6) |
| 55-64 | 50.0 (40.3, 59.7) | 45.9 (43.3, 48.4) | 56.4 (52.4, 60.3) | 65.9 (60.0, 71.7) | 58.3 (54.3, 62.3) | 65.5 (60.2, 70.9) | 67.0 (61.1, 72.9) | 67.1 (61.5, 72.7) |
| 65-74 | 68.9 (56.3, 81.5) | 54.3 (51.5, 57.0) | 63.2 (57.7, 68.6) | 66.7 (59.2, 74.3) | 69.5 (65.1, 73.9) | 78.3 (73.7, 82.9) | 68.5 (62.6, 74.4) | 74.5 (69.5, 79.6) |
|
| ||||||||
| Education | ||||||||
| None | 46.9 (35.9, 57.9) | 27.7 (20.8, 34.6) | 33.2 (28.5, 37.8) | 47.1 (40.8, 53.4) | 24.3 (1.0, 47.6) | 43.0 (28.2, 57.8) | 75.5 (49.4, 100) | (**) |
| Any School | 45.4 (40.2, 50.6) | 32.5 (29.6, 35.3) | 40.1 (37.6, 42.5) | 58.8 (54.8, 62.8) | 42.7 (39.6, 45.8) | 53.2 (48.4, 58.0) | 58.0 (52.6, 63.3) | 56.4 (51.5, 61.2) |
| University/Higher | (**) | (**) | 48.5 (43.7, 53.3) | 55.0 (44.8, 65.2) | 45.9 (39.7, 52.1) | 56.6 (49.7, 63.5) | 78.8 (71.0, 86.5) | 60.1 (44.1, 76.1) |
|
| ||||||||
| Control1 | ||||||||
|
| ||||||||
| Overall | 54.2 (45.0, 63.4) | 16.2 (9.5, 22.8) | 43.2 (39.4, 47.1) | 46.2 (41.6, 50.8) | 37.1 (31.9, 42.3) | 50.0 (42.8, 57.2) | 71.2 (65.6, 76.7) | 51.2 (44.5, 57.9) |
|
| ||||||||
| Sex | ||||||||
| Men | 46.9 (28.1, 65.8) | 19.6 (6.1, 33.0) | 38.4 (32.4, 44.5) | 45.8 (37.7, 53.9) | 30.4 (21.8, 39.0) | 48.4 (36.7, 60.1) | 72.6 (66.4, 78.7) | 45.1 (32.4, 57.8) |
| Women | 57.3 (48.6, 66.0) | 13.5 (5.9, 21.0) | 46.5 (41.6, 51.3) | 46.9 (41.7, 52.1) | 42.9 (36.6, 49.1) | 52.0 (43.2, 60.8) | 74.7 (68.1, 81.3) | 57.2 (49.9, 64.4) |
|
| ||||||||
| Age groups, years | ||||||||
| 35-44 | 48.7 (25.1, 72.4) | 15.1 (0.0, 35) | 49.3 (40.5, 58.1) | 49.6 (40.1, 59.1) | 39.8 (27.2, 52.4) | 54.2 (36.4, 72.0) | 90.5 (83.0, 98.0) | 67.0 (49.6, 84.3) |
| 45-54 | 53.3 (39.5, 67.1) | 18.4 (11.0, 25.8) | 41.0 (35.5, 46.5) | 46.8 (38.5, 55.1) | 37.3 (29.7, 44.8) | 48.9 (39.7, 58.1) | 72.3 (62.2, 82.4) | 41.8 (31.3, 52.3) |
| 55-64 | 52.4 (37.4, 67.4) | 16.4 (13.5, 19.2) | 36 (30.7, 41.3) | 46.7 (38.6, 54.7) | 31.6 (26.7, 36.5) | 56.2 (48.8, 63.6) | 61.7 (53.6, 69.8) | 36 (29.2, 42.8) |
| 65-74 | 59.1 (43.0, 75.2) | 16.3 (13.3, 19.2) | 36.8 (30.4, 43.3) | 35.2 (24.3, 46.1) | 34.5 (29.2, 39.9) | 31.4 (25.5, 37.2) | 47.2 (39.5, 54.9) | 52.7 (45.8, 59.6) |
|
| ||||||||
| Education | ||||||||
| None | 58.3 (33.7, 82.8) | 14.9 (1.2, 28.6) | 48.7 (34.4, 63.1) | 53.7 (42.8, 64.5) | 54.7 (41.0, 68.4) | (**) | 73.2 (44.7, 100) | (**) |
| Any School | 53.7 (43.9, 63.5) | 16.6 (9.8, 23.3) | 42.8 (38.0, 47.6) | 44.3 (38.4, 50.2) | 39.3 (33.3, 45.2) | 51.1 (41.8, 60.4) | 69.6 (62.5, 76.7) | 50.8 (43.6, 57.9) |
| University/Higher | (**) | (**) | 45.3 (37.5, 53.2) | 47.8 (33.1, 62.5) | 30.2 (20.4, 40.0) | 52.1 (40.3, 63.8) | 73.0 (63.5, 82.6) | 62.9 (46.4, 79.4) |
|
| ||||||||
| Control2 | ||||||||
|
| ||||||||
| Overall | 25.1 (21, 29.2) | 5.3 (4.1, 6.5) | 10.1 (9.1, 11.1) | 24.4 (21.7, 27.0) | 15.9 (14.1, 17.8) | 27.1 (23.6, 30.7) | 45.9 (40.9, 50.8) | 29.4 (25.1, 33.6) |
|
| ||||||||
| Sex | ||||||||
| Men | 15.6 (10.2, 21.0) | 4.9 (3.5, 6.4) | 7.1 (6.0, 8.2) | 17.9 (14.2, 21.6) | 10.0 (7.8, 12.1) | 17.8 (13.7, 22.0) | 29.0 (22.1, 35.9) | 17.5 (12.2, 22.9) |
| Women | 34.1 (28.2, 40.0) | 5.7 (3.5, 7.9) | 13.2 (11.5, 14.9) | 31.0 (27.1, 35.0) | 22.2 (18.9, 25.5) | 36.2 (30.0, 42.3) | 62.6 (55.6, 69.7) | 41.6 (35.0, 48.2) |
|
| ||||||||
| Age groups, years | ||||||||
| 35-44 | 15.7 (9.0, 22.5) | 1.7 (0.0, 4.0) | 8.2 (6.2, 10.1) | 22.0 (17.4, 26.7) | 12.3 (8.2, 16.5) | 19.1 (11.0, 27.2) | 49.6 (38.6, 60.6) | 34.2 (24.3, 44.1) |
| 45-54 | 28.5 (21.8, 35.2) | 7 (3.8, 10.1) | 10.8 (9.0, 12.5) | 24.8 (20.1, 29.5) | 15.7 (12.6, 18.9) | 30.7 (24.6, 36.7) | 49.3 (41.3, 57.2) | 22.9 (16.7, 29.1) |
| 55-64 | 26.5 (18.1, 34.9) | 7.5 (6.1, 8.8) | 12.3 (10.3, 14.3) | 29.4 (23.8, 35.1) | 18.6 (15.5, 21.7) | 37.4 (31.8, 42.9) | 42.1 (35.8, 48.4) | 25.2 (20.3, 30.1) |
| 65-74 | 40.9 (27.4, 54.5) | 8.7 (7.1, 10.2) | 11.0 (8.8, 13.2) | 22.8 (14.9, 30.7) | 24.1 (20.1, 28.1) | 24.6 (19.8, 29.4) | 33.5 (27.7, 39.4) | 39.8 (34.2, 45.4) |
|
| ||||||||
| Education | ||||||||
| None | 29.4 (18.3, 40.5) | 3.1 (2.0, 4.2) | 5.8 (3.9, 7.7) | 22.5 (17.3, 27.7) | 19.4 (0.0, 42.4) | (**) | 60.0 (36.4, 83.5) | (**) |
| Any School | 24.8 (20.3, 29.3) | 5.4 (4.1, 6.8) | 10.8 (9.4, 12.1) | 25.1 (21.6, 28.6) | 16.6 (14.4, 18.7) | 27.4 (23.0, 31.7) | 41.6 (36.1, 47.1) | 29.0 (24.6, 33.4) |
| University/Higher | (**) | (**) | 20.5 (16.8, 24.1) | 24.9 (15.8, 34) | 15.1 (11, 19.2) | 29.1 (22.5, 35.7) | 56.7 (46.6, 66.8) | 35.3 (19.6, 51.1) |
Values are percentage (95% confidence interval). Awareness was defined as self-report of a prior diagnosis of hypertension by a healthcare professional. Treatment1 was defined as self-reported use of antihypertensive medications among patients aware of their condition. Treatment2 was defined as self-reported use of antihypertensive medication among total hypertensive patients.Control1 was defined as systolic BP <140 mmHg and diastolic BP <90 mmHg among hypertensive patients on antihypertensive medications. Control2 was defined as systolic BP <140 mmHg and diastolic BP <90 mmHg among total hypertensive patients.
Data not available for Kenya.
(**) Not applicable.
DISCUSSION
In this multi-national study with pooled data from the NHLBI/UHG COE program, we described hypertension prevalence, awareness, treatment, and control for sites across Latin America, Africa and Asia. We analyzed data from 7 population-based studies conducted in 148 villages and 18 cities from 9 LMICs that represent 40% of the world population. Our key findings are that there is high heterogeneity in terms of prevalence of hypertension not only across communities and regions but also among urban, rural and semi-rural areas, and that awareness and control are still dismally low except in a few locations. Our findings are consistent with the considerable variation among countries and geographic regions observed in other studies. (23-26) For example, in Africa, the age-standardized prevalence of hypertension was high in the village included in the Kenyan study (49.9%) and in urban settings in South Africa (54.9%) in accordance with other studies. (27) In Asia, the estimated age-gender standardized prevalence for rural population in the five provinces included in the study from China was also high (52.5%), while in the studies from India and Pakistan, a prevalence of 32.5 and 42.3% respectively, were seen. These results show a high degree of heterogeneity as in previous studies in China (28-36) and India (25, 37-39). In the Southern Cone of Latin America, the prevalence of HTN was high in the cities included in Argentina, Chile and Uruguay (45.4%, 39.9%, and 44.1%, respectively). However, in the communities included in Peru, the age-gender standardized prevalence of HTN was comparatively low (19.2%), which may be related to the fact that all the population included in the Southern Cone was urban while two of the four communities from Peru were semi-rural. The CARMELA study had showed a prevalence of hypertension in Lima of 12.6% in 2003-2005. (40)
In the communities from China and India, and the sites from the Southern Cone of Latin America, the age-gender standardized prevalence of hypertension was higher in men compared to women while the opposite was seen in Kenya, South Africa, and Pakistan. In those towns from Peru, the prevalence was similar in both genders. These findings are consistent with several studies, some of them showing gender differences while others not. (41)
The overall prevalence of hypertension treatment among those individuals that were aware of their condition was higher than the results obtained in other studies. However, the prevalence of treatment among all hypertensives was lower, and consistent with the findings of other authors. (42-44) There was a gap between both detection and control of hypertension across all countries studied, but the magnitude of the gap varied widely among different settings. This may be associated with differences in individual habits and risk behaviors, access to the health system and medication, and other contextual factors such as culture, beliefs, practices and value judgments. However, these variables have not been measured in this study, and hence could not been adjusted for. As a whole, women had significantly higher rates of awareness, treatment and control than men in all countries, which may be related to a higher health-seeking behavior. (45) Only in the rural villages of China, did men seem to show a slightly better control. Noteworthy, the global rate of control in the villages in China was extremely low as it was shown in other studies conducted in different regions of this country. (28-36, 40) There was no clear gradient according to educational level in contrast to other studies. (44) However, this result should be interpreted with caution since the education categories considered in the analysis may have had a limited discriminative value.
STRENGTHS AND LIMITATIONS
Some strengths of this report should be highlighted. This study is based on a set of harmonized data from epidemiological studies conducted over the same period of time across LMICs in three continents as part of a collaborative network to address non-communicable diseases. Rigorous procedures were followed during the harmonization process to ensure optimal matching and definition of variables. In all cases the appropriate sampling weights were applied to ensure valid estimates for each site. Standardization of the estimated prevalence using the WHO world population distribution for the countries involved also allows comparison among studies adjusting for age and gender, two variables that are known to affect the presence of hypertension. Finally, all the surveys included in this study were conducted under rigorous research protocols that ensured accuracy and reliability of the estimates.
This study also has some limitations. There was heterogeneity among the individual studies in terms of population, sample size, sampling methods and data collection. Some of the studies included exclusively urban locations, others were conducted in rural settings, and others included a mix of urban and rural or semi-rural communities, which may differ in terms of culture, social context, health systems, and geographic location. Both the number of sites and the sample size in each site also varied greatly. Although all the original studies were population-based and used random sampling techniques, the number of sampling stages and conditions of proportionality differed by study. Additionally, although in all the studies multiple measurements of BP were taken after a rest period of at least 5 minutes, different kinds of BP monitors were used, and BP was measured in different conditions, either at home or at a clinic visit, and the time interval between measurements was not the same for all studies. Actually, we found that the response rates in those studies where BP measurements were taken at a clinic were lower (73.4% to 78%) than those where BP measurements were taken at home or camps in the community (84 to 91%). Although this difference may have introduced some bias in the final results, it is remarkable that response rates were high for all the studies, given the population-based nature of the sampling. Furthermore, differences between countries may be due to other relevant factors, such as multiple cardiovascular risk factors, socio-economic features, and comorbidities, which were not examined here. Finally, it is important to emphasize that the individual surveys included in this study were not nationally representative, and thus the prevalence estimates reported here should not be applied to countries but only to those communities participating in the original studies.
CONCLUSION
Prevalence of hypertension varies widely in different communities across selected LMICs. The prevalence of awareness, treatment and control also differs in different settings. Our results highlight a clear need to focus on increasing hypertension awareness and control in LMICs. These results should impact how clinicians, epidemiologists and policy makers address this public health problem in order to reduce the burden of NCDs in developing countries.
Highlights.
Prevalence of hypertension varies widely in different communities across selected LMICs.
Globally, awareness of hypertension varies between 33% and 69%.
Although the proportion of individuals aware of their condition who receive treatment is above 70%, the overall hypertension control rate is still low.
ACKNOWLEDGEMENTS
The authors want to gratefully acknowledge WESTAT for their work on merging the individual datasets, as well as the participants in each study for their collaboration, and the field teams and data managers and statisticians in each country for their hard work.
Funding: This project has been funded in part with Federal funds from the United States National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services under Contract Number HHSN268200900030C. The funding source played no role in the study design, data collection, data analysis and interpretation, or writing of the report. The funding source contractually required review and approval of the manuscript prior to submission for publication and no changes were requested.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaziano T, Bittonc A, Shuchi A, Weinstein M. The global cost of nonoptimal blood pressure. Journal of Hypertension. 2009;27:1472–1477. doi: 10.1097/HJH.0b013e32832a9ba3. [DOI] [PubMed] [Google Scholar]
- 5.Riley S. The cardiovascular market outlook to 2011. Business Insights Ltd; London: 2006. [Google Scholar]
- 6.Lawes CM. Global burden of blood-pressure-related disease, 2001. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 7.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2008;9623:1513–1518. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 8.Tibazarwa KB, Damasceno AA. Hypertension in developing countries. Can J Cardiol. 2014 May;30(5):527–33. doi: 10.1016/j.cjca.2014.02.020. doi: 10.1016/j.cjca.2014.02.020. Epub 2014 Mar 4. [DOI] [PubMed] [Google Scholar]; Can J Cardiol. 2014 Jul;30(7):834. Review. Erratum in: [Google Scholar]
- 9.UnitedHealth, National Heart, Lung, and Blood Centres of Excellence Global response to non-communicable disease. BMJ. 2011;342:76–78. doi: 10.1136/bmj.d3823. [DOI] [PubMed] [Google Scholar]
- 10.Checkley W, Ghannem H, Irazola V, Kimaiyo S, Levitt NS, Miranda JJ, Niessen L, Prabhakaran D, Rabadán-Diehl C, Ramirez-Zea M, Rubinstein A, Sigamani A, Smith R, Tandon N, Wu Y, Xavier D, Yan LL, GRAND South Network, UnitedHealth Group/National Heart, Lung, and Blood Institute Centers of Excellence Management of NCD in low- and middle-income countries. Glob Heart. 2014 Dec;9(4):431–43. doi: 10.1016/j.gheart.2014.11.003. doi: 10.1016/j.gheart.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Heart, Lung, and Blood Institute UHG/NHLBI collaborating centers of excellence. Available at: http://www.nhlbi.nih.gov/about/globalhealth/centers/index.htm. Accessed June 14, 2015. [Google Scholar]
- 12.UnitedHealth Group/National Heart, Lung, and Blood Institute Centres of Excellence A global research network for non-communicable diseases. Lancet. 2014 Apr 26;383(9927):1446–7. doi: 10.1016/S0140-6736(13)61808-5. doi: 10.1016/S0140-6736(13)61808-5. Epub 2013 Oct 3. [DOI] [PubMed] [Google Scholar]
- 13.Nair M, Ali MK, Ajay VS, Shivashankar R, Mohan V, Pradeepa R, et al. CARRS Surveillance study: design and methods to assess burdens from multiple perspectives. BMC Public Health. 2012;12:701. doi: 10.1186/1471-2458-12-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rubinstein AL, Irazola VE, Poggio R, Bazzano L, Calandrelli M, Lanas Zanetti FT, et al. Detection and follow-up of cardiovascular disease and risk factors in the Southern Cone of Latin America: the CESCAS I study. BMJ Open. 2011;1(1):e000126. doi: 10.1136/bmjopen-2011-000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miranda JJ, Bernabe-Ortiz A, Smeeth L, Gilman RH, Checkley W. Addressing geographical variation in the progression of non-communicable diseases in Peru: the CRONICAS cohort study protocol. BMJ Open. 2012;2(1):e000610. doi: 10.1136/bmjopen-2011-000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan LL, Fang W, Delong E, Neal B, Peterson ED, Huang Y, et al. Population impact of a high cardiovascular risk management program delivered by village doctors in rural China: design and rationale of a large, cluster-randomized controlled trial. BMC Public Health. 2014;14:345. doi: 10.1186/1471-2458-14-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fathima FN, Joshi R, Agrawal T, Hegde S, Xavier D, Misquith D, et al. Rationale and design of the Primary pREvention strategies at the community level to Promote Adherence of treatments to pREvent cardiovascular diseases trial number (CTRI/2012/09/002981) Am Heart J. 2013;166(1):4–12. doi: 10.1016/j.ahj.2013.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 19.Alberti KG1, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006 May;23(5):469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 20.Lehtonen Risto, Pahkinen Erkki. Practical Methods for Design and Analysis of Complex Surveys. second Wiley; 2004. [Google Scholar]
- 21.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age Standardization of Rates: a New WHO Standard. Global Programme on Evidence for Health Policy, World Health Organization; Geneva, Switzerland: 2000. GPE Discussion Paper No. 31. [Google Scholar]
- 22.Age standardization of rates: Anew WHO Standard. GPE Discussion Paper Series: No.31 EIP/GPE/EBD World Health Organization 2001.
- 23.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 24.Vlahov D, Freudenberg N, Proietti F, Ompad D, Quinn A, Nandi V, et al. Urban as a determinant of health. J Urban Health. 2007;84:i16–i26. doi: 10.1007/s11524-007-9169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prince MJ, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y, Jacob KS, Jimenez-Velazquez IZ, Rodriguez JL, Salas A, Sosa AL, Williams JD, Gonzalez-Viruet M, Jotheeswaran AT, Liu Z. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2012 Jan;30(1):177–87. doi: 10.1097/HJH.0b013e32834d9eda. [DOI] [PubMed] [Google Scholar]
- 26.WHO Global Status Report on Non-Communicable Diseases 2014. Available at http://www.ifa-fiv.org/global-status-report-on-non-communicable-diseases-2014/. Accessed July 11, 2015.
- 27.Malhotra R, Puoane T, Hoyo C, Hughes G, Ostbye T. Prevalence and awareness of hypertension in an urban township of South Africa: compelling need for action. Ethn Dis. 2008;18(4):401–402. Autumn;18. [PubMed] [Google Scholar]
- 28.Whelton PK, He J, Muntner P. Prevalence, awareness, treatment and control of hypertension in North America, North Africa and Asia. China. J Hum Hypertens. 2004 Aug;18(8):545–51. doi: 10.1038/sj.jhh.1001701. [DOI] [PubMed] [Google Scholar]
- 29.Fan L, Feng SX, Han B, Wang CC, Gao L, Feng HF, Qi XY, Zhou G. Prevalence, awareness, treatment and control of hypertension in Henan Province, China. Aust J Rural Health. 2014 Oct;22(5):264–9. doi: 10.1111/ajr.12116. doi: 10.1111/ajr.12116. [DOI] [PubMed] [Google Scholar]
- 30.Ke L, Ho J, Feng J, Mpofu E, Dibley MJ, Li Y, Feng X, Van F, Lau W, Brock KE. Prevalence, awareness, treatment and control of hypertension in macau: results from a cross-sectional epidemiological study in Macau, China. Am J Hypertens. 2015 Feb;28(2):159–65. doi: 10.1093/ajh/hpu121. doi: 10.1093/ajh/hpu121. Epub 2014 Jul 25. [DOI] [PubMed] [Google Scholar]
- 31.Bi Z, Liang X, Xu A, Wang L, Shi X, Zhao W, Ma J, Guo X, Zhang X, Zhang J, Ren J, Yan L, Lu Z, Wang H, Tang J, Cai X, Dong J, Zhang J, Chu J, Engelgau M, Yang Q, Hong Y, Wang Y. Hypertension prevalence, awareness, treatment, and control and sodium intake in Shandong Province, China: baseline results from Shandong-Ministry of Health Action on Salt Reduction and Hypertension (SMASH), 2011. Prev Chronic Dis. 2014 May 22;11:E88. doi: 10.5888/pcd11.130423. doi: 10.5888/pcd11.130423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao Y, Yan H, Marshall RJ, Dang S, Yang R, Li Q, Qin X. Trends in population blood pressure and prevalence, awareness, treatment, and control of hypertension among middle-aged and older adults in a rural area of Northwest China from 1982 to 2010. PLoS One. 2013 Apr 16;8(4):e61779. doi: 10.1371/journal.pone.0061779. doi: 10.1371/journal.pone.0061779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang J, Zhang L, Wang F, Liu L, Wang H, China National Survey of Chronic Kidney Disease Working Group Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014 Nov;27(11):1355–61. doi: 10.1093/ajh/hpu053. doi: 10.1093/ajh/hpu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dong C, Ge P, Ren X, Fan H, Yan X. Prevalence, awareness, treatment and control of hypertension among adults in rural north-western China: a cross-sectional population survey. J Int Med Res. 2013 Aug;41(4):1291–300. doi: 10.1177/0300060513488498. doi: 10.1177/0300060513488498. [DOI] [PubMed] [Google Scholar]
- 35.Ma WJ1, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, Lao XQ, Tam WW, Wong MC, Yu IT. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens. 2012 May;25(5):590–6. doi: 10.1038/ajh.2012.11. doi: 10.1038/ajh.2012.11. [DOI] [PubMed] [Google Scholar]
- 36.Meng XJ1, Dong GH, Wang D, Liu MM, Lin Q, Tian S, Xu LX, Hou H, Ren YF, Lee YL. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens. 2011 Jul;29(7):1303–10. doi: 10.1097/HJH.0b013e328347f79e. doi: 10.1097/HJH.0b013e328347f79e. [DOI] [PubMed] [Google Scholar]
- 37.Kaur P1, Rao SR, Radhakrishnan E, Rajasekar D, Gupte MD. Prevalence, awareness, treatment, control and risk factors for hypertension in a rural population in South India. Int J Public Health. 2012 Feb;57(1):87–94. doi: 10.1007/s00038-011-0303-3. doi: 10.1007/s00038-011-0303-3. [DOI] [PubMed] [Google Scholar]
- 38.Thankappan KR, Shah B, Mathur P, et al. 2010;131:53e63. [Google Scholar]
- 39.Zachariah MG, Thankappan KR, Alex SC, Sarma PS, Vasan RS. Prevalence, correlates, awareness, treatment, and control of hypertension in a middle-aged urban population in Kerala. Indian Heart J. 2003;55:245e251. [PubMed] [Google Scholar]
- 40.Hernández-Hernández R1, Silva H, Velasco M, Pellegrini F, Macchia A, Escobedo J, Vinueza R, Schargrodsky H, Champagne B, Pramparo P, Wilson E, CARMELA Study Investigators Hypertension in seven Latin American cities: the Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) study. J Hypertens. 2010 Jan;28(1):24–34. doi: 10.1097/HJH.0b013e328332c353. Pereira. [DOI] [PubMed] [Google Scholar]
- 41.Doumas M1, Papademetriou V, Faselis C, Kokkinos P. Gender differences in hypertension: myths and reality. Curr Hypertens Rep. 2013 Aug;15(4):321–30. doi: 10.1007/s11906-013-0359-y. doi: 10.1007/s11906-013-0359-y. [DOI] [PubMed] [Google Scholar]
- 42.Li D, Lv J, Liu F, Yang X, Feng Y, Chen G, Hao M. Hypertension burden and control in mainland China: Analysis of nationwide data 2003-2012. Int J Cardiol. 2015 Apr 1;184:637–44. doi: 10.1016/j.ijcard.2015.03.045. doi: 10.1016/j.ijcard.2015.03.045. Epub 2015 Mar 4. [DOI] [PubMed] [Google Scholar]
- 43.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–975. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 44.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, Bahonar A, Chifamba J, Dagenais G, Diaz R, Kazmi K, Lanas F, Wei L, Lopez-Jaramillo P, Fanghong L, Ismail NH, Puoane T, Rosengren A, Szuba A, Temizhan A, Wielgosz A, Yusuf R, Yusufali A, McKee M, Liu L, Mony P, Yusuf S, PURE (Prospective Urban Rural Epidemiology) Study investigators Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013 Sep 4;310(9):959–68. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 45.Courtenay WH. Constructions of masculinity and their influence on men's well-being: a theory of gender and health. Social Science & Medicine. 2000;50(10):1385–1401. doi: 10.1016/s0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]