Abstract
Background
Over a quarter of the world’s adult population has hypertension, yet achieving adequate treatment or control targets remain a challenge.
Objective
To identify, longitudinally, characteristics associated with antihypertensive treatment and blood pressure (BP) control among individuals with hypertension.
Methods
Data from individuals enrolled in the population-based CRONICAS Cohort Study (adults ≥35 years, living in four different rural/urban and coastal/high-altitude Peruvian settings) with hypertension at baseline was used. Antihypertensive treatment and BP control were assessed at baseline and at 15 months. Multinomial logistic regressions were used to estimate relative-risk ratios (RRR) and 95% confidence intervals (95% CI) of factors associated with antihypertensive treatment and BP control at follow-up.
Results
At baseline, among 717 individuals with hypertension (53% female, mean age 61.5±12.4 years), 28% were unaware of their hypertension status, 30% were aware but untreated, 16% were treated but uncontrolled, and 26% were treated and controlled. At follow-up, 89% of unaware and 82% of untreated individuals persisted untreated, and only 58% of controlled individuals remained controlled. Positive predictors of receiving treatment at follow-up included age (RRR 0.81, 95% CI: 0.73–0.91 for every 5 years) and family history of a chronic disease (RRR 0.53, 95% CI: 0.31–0.92, vs. no history); whereas Puno rural site (RRR 16.51, 95% CI: 1.90–143.56, vs. Lima) and male sex (RRR 2.59, 95% CI: 1.54–4.36) were risk factors. Systolic BP at baseline (RRR 1.27, 95% CI: 1.16–1.39 for every 5 mmHg) and male sex (RRR 1.75, 95% CI: 1.02–2.98) were risk factors for being uncontrolled at follow-up.
Conclusion
Large gaps in treatment of hypertension were observed. Targeting specific populations such as men, younger individuals or those without family history of disease may increase coverage of antihypertensive treatment. Also, targeting male individuals or those with higher systolic BP could yield better rates of BP control in the short term.
Keywords: arterial hypertension, awareness, control, treatment, Peru
INTRODUCTION
Worldwide, over a quarter of the adult population has hypertension, with a disproportionate burden on developing countries [1, 2]. Despite hypertension-related mortality has decreased around the world [3, 4], hypertension still remains as a leading cause of global mortality [5].
Achieving optimal BP control is an important goal of hypertension management. It has been estimated that only 50–75% of hypertensive individuals are aware of their diagnosis, and 12–41% of those diagnosed receive treatment or achieve control targets [6–9]. In Peru, the prevalence of hypertension varies from 11% in rural areas to 29% in urban populations [10]. However, it has been estimated that only 6% of individuals with hypertension receive treatment and are adequately controlled with blood pressure (BP) level <140/90 [11].
Hypertension management is a long-term process that is commonly challenging for patients and healthcare providers. A combination of lifestyle modification and pharmacologic treatment with antihypertensive medication is essential to achieving adequate BP control [12–14], yet nearly half of patients discontinue their antihypertensive regimens within the first year [15]. Poor BP control may be explained by unawareness of hypertension diagnosis, lack of knowledge of target BP goals, nonadherence to pharmacologic treatment [16], and unhealthy lifestyles [17]. Information from prospective studies from low- and middle-income country settings revealing the characteristics of individuals at risk of not taking medication or achieving BP control is scant.
Identifying predictors of BP treatment and control is needed to adequately design and implement interventions to improve treatment and BP control rates. In this study, we aimed to characterize factors associated with the use of antihypertensive medication and BP control in the short-term, according to previous awareness, treatment, and BP control status.
METHODS
Study design and setting
This study is an analysis in a sample of participants of the CRONICAS Cohort Study, a longitudinal, population-based study aimed to determine progression towards cardiovascular and chronic pulmonary diseases in Peru. The original study design, have been described elsewhere [18]. Briefly, a random age- and sex-stratified sample of individuals aged 35 years and above was selected from four different sites, spanning three regions that differ by degree of urbanization and elevation. These regions include: 1) Pampas de San Juan de Miraflores, a highly-urbanized periurban community on the coast of Lima; 2) Puno, located in the Andes at 3,825 meters above sea-level, which contributed with both urban and rural sites; and 3) Tumbes, a semi-urban group of villages in the northern coast of Peru. Health indicators in Puno were worse than those in Tumbes and Lima. According to Peru’s national 2007 census, only 27% of Puno’s population have a health insurance; followed by 37% in San Juan de Miraflores, and 48% in Tumbes [19]. In 2010, there were 1,412 inhabitants per physician in Puno, 1,184 in Tumbes, and 355 in Lima [20].
Study participants
For this study, we restrict our analysis to those participants who were classified as hypertensive at baseline and in whom complete data on BP, antihypertensive medication and cardiometabolic risk factors evaluation were available. Hypertension was defined as 1) measured systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg, or 2) self-reported diagnosis of hypertension (performed by a physician), or 3) current use of antihypertensive medication. All subjects were informed of their BP levels and those with elevated BP readings were recommended to seek medical care at their nearest health facilities.
Procedures
Evaluation of participants was completed by trained and standardized research staff. At baseline, the protocol included a questionnaire to collect information about socio-demographic characteristics, cardiometabolic and behavioral risk factors, antihypertensive treatment, as well as personal and family medical history of cardiovascular disease and other chronic diseases. BP was measured in triplicate after a 5-minute period of rest using an automatic blood pressure device (OMRON HEM-780). For the analysis, the mean value of the second and third measurements was used [21]. Anthropometric measures and laboratory analyses were conducted following standard procedures [18]. The protocol at 15-month follow-up was similar than the one used at baseline.
Exposure variables at baseline
Socio-demographic variables included sex, age (years), study site (Lima, urban Puno, rural Puno and Tumbes), and education level [primary or less (<6 years), secondary (6–12 years), and superior (≥12 years)]. Socioeconomic status was divided into three categories corresponding to tertiles of the assets and household facilities dimensions of the composite wealth index score [22].
For analytic purposes, variables of interest were categorized using commonly reported cutoffs, when available. Three cardiometabolic and one behavioral factor were dichotomized according to the recommendations of the American Heart Association’s (AHA) ideal cardiovascular health metrics [23]. Body mass index (BMI) was divided into healthy (18.5–24.9 kg/m2) and excess of weight (≥25.0 kg/m2), total serum cholesterol into healthy (<200 mg/dL without cholesterol lowering medication) and unhealthy (≥200 mg/dL or cholesterol lowering medication use), fasting blood glucose was divided into healthy (<100mg/dL without glucose-lowering medication use) and unhealthy (≥100mg/dL or glucose-lowering medication use), and tobacco use into never/former smoker (not smoking even one cigarette for the last year or more) and current smoker (self-report of currently smoking). Physical activity, assessed using the leisure time domain of the International Physical Activity Questionnaire (IPAQ), was used to classify participants as active (≥75 min/week vigorous intensity or ≥150 min/week moderate and vigorous intensity activity) or inactive (less than that amount), self-report of fruit and vegetable intake was used to classify participants as having a healthy (≥4.5 cups of fruits and vegetables/day) or unhealthy (<4.5 cups of fruits and vegetables/day) diet, and alcohol consumption, which was assessed using the Alcohol Use Disorders Identification Test (AUDIT), was used to divide drinking patterns into not-hazardous (AUDIT score ≤7) and hazardous (AUDIT score ≥8) [24, 25]. Personal history of disease included a diagnosis of heart disease or stroke by a physician. Family history of disease was based on self-report of a relative with a cardiometabolic disease such as high BP, heart disease, high serum cholesterol, diabetes, stroke, or other chronic disease like tuberculosis, asthma, chronic bronchitis, chronic obstructive pulmonary disease or lung cancer.
To incorporate hypertension awareness, antihypertensive treatment, and BP control (A-T-C) into a single analysis, a composite measure was created which yielded the following categories: 1) the unaware group (participants with SBP ≥140 mmHg or DBP ≥90 mmHg, without a physician diagnosis of hypertension and without antihypertensive treatment), 2) the untreated group (participants with a diagnosis of hypertension by a physician, without antihypertensive treatment), 3) the uncontrolled group (participants taking antihypertensive treatment with SBP ≥140 mmHg or DBP ≥90 mmHg), and 4) the controlled group (participants taking antihypertensive treatment with SBP <140 mmHg and DBP <90 mmHg).
Study outcome
At 15-month follow-up, antihypertensive treatment and BP control status were assessed and incorporated into a single 3-categories outcome (untreated, uncontrolled and controlled). A participant was included in the untreated category if he/she did not take at least one antihypertensive medication, once per week, during the last month. Uncontrolled BP was defined as SBP ≥140 mmHg or DBP ≥90 mmHg among participants taking antihypertensive medication. Awareness was not considered at follow-up because all participants included in the analysis had to satisfy the definition of hypertension at baseline and were informed of their hypertension diagnosis.
Statistical Power
Using a two-tailed alpha level of 0.05, with 717 participants, the study had 80% of power to detect risk ratios of treatment and BP control of 1.55 or higher, or 0.64 or lower. Statistical power was calculated using Power Analysis and Sample Size PASS software (version 11, NCSS LLC, Kaysville, Utah, USA).
Statistical Analysis
A description of sociodemographic, cardiometabolic and behavioral characteristics was performed for each of the four baseline A-T-C groups. Continuous variables are presented as mean (±standard deviation) and categorical variables are presented as proportions. Associations between baseline characteristics and treatment and BP control at follow-up were assessed using chi-squared for categorical variables and t-student or ANOVA tests for continuous variables. Those characteristics statistically associated with the outcome of interest were included in a nested multinomial logistic regression model [26] to identify potential baseline risk factors associated with treatment and BP control at follow-up. The Akaike information criterion (AIC) was used to select the variables with the better fitting model. Unadjusted and adjusted relative risk ratios (RRR), with 95% confidence intervals (95% CI), of being untreated, uncontrolled, and controlled at follow-up were estimated. Because BP measurements were only conducted during one visit, a sensitivity analysis was performed using higher thresholds for SBP (145 mmHg and 150 mmHg) to define unawareness status. This was done to minimize the possibility of including individuals without hypertension in the study. All analyses considered a two-tailed p-value less than 0.05 to be statistically significant. Stata 12.1 (Stata Corporation, College Station, Texas, USA) was used for data analyses.
Ethical Considerations
All participants of the CRONICAS Cohort Study provided verbal informed consent. Verbal consent was chosen over written consent due to high rates of illiteracy especially in rural areas. The CRONICAS Cohort Study was approved by the Institutional Review Boards at Universidad Peruana Cayetano Heredia and A.B. PRISMA, in Lima, Peru, and at the Bloomberg School of Public Health, Johns Hopkins University, in Baltimore, USA.
RESULTS
Participants
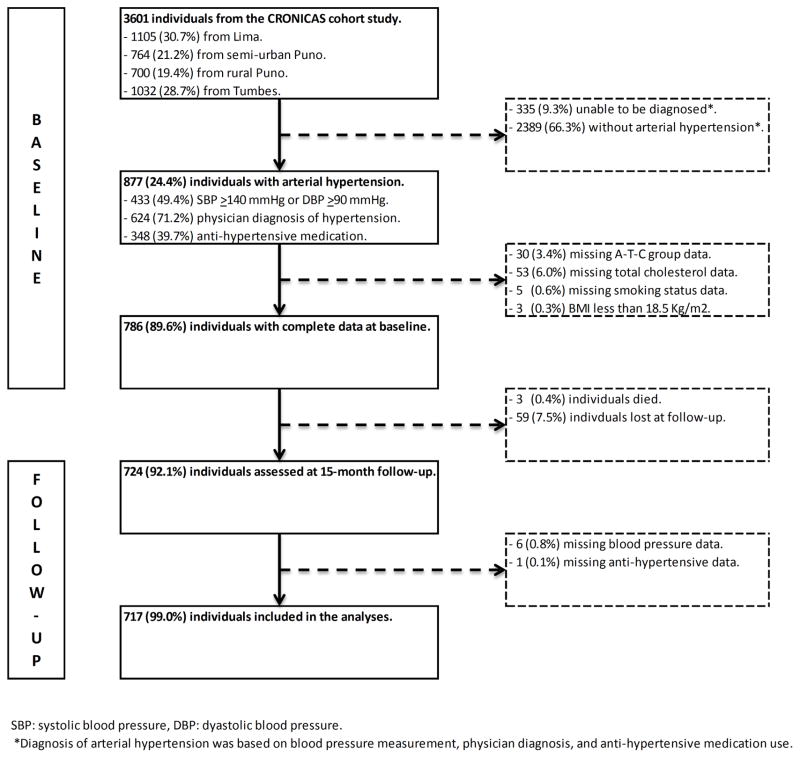
A total of 3601 individuals were enrolled into the study. At baseline, 877 (24.4%) individuals with hypertension were identified. However, 88 individuals were excluded because they did not have complete data, and 3 because their BMI was lower than 18.5 kg/m2. Of the 786 eligible participants at follow-up, 3 (0.4%) individuals were dead, 59 were lost to follow-up and 7 did not have BP data or antihypertensive treatment. Therefore, 717 individuals (82% response rate), 53.4% female, mean age 61.5 years (SD: 12.4) were included in the analyses (Figure 1).
Figure 1.
Inclusion of participants in the study
Characteristics of study participants at baseline
At baseline, 362 (50.5%) individuals had high levels of SBP and/or DBP, 505 (70.4%) had a diagnosis by a physician, and 298 (41.6%) were taking antihypertensive medication. Moreover, 204 (28.4%) individuals were unaware of their hypertension status, 215 (30%) were untreated, 115 (16%) were uncontrolled, and only 183 (25.5%) were controlled.
Sociodemographic, cardiometabolic and behavioral characteristics according to A-T-C groups at baseline are presented in Table 1. The highest proportion of male individuals was in the unaware group (70%); it decreases in the untreated group and becomes the lowest in the controlled group (32%). Age varied across groups without a clear trend. Socioeconomic status were similar between A-T-C groups. The predominant educational level was primary or less (58%). The untreated group had the highest proportions of secondary (29%) and superior (23%) education level. Only 10.5% of individuals met 4-to-6 of the ideal cardiovascular health metrics. Personal history of heart disease and stroke were infrequent (10.7% and 1.3%, respectively). Family history of disease was more frequent and increased with awareness, treatment and BP control.
Table 1.
Characteristics of population with hypertension at baseline.
| Socio-demographic factors | Unaware
|
Aware, not treated
|
Treated and uncontrolled
|
Treated and controlled
|
|
||||
|---|---|---|---|---|---|---|---|---|---|
| n=204 | % | n=215 | % | n=115 | % | n=183 | % | p-value | |
| Age (years) * | 62.4 | ±12.9 | 56.7 | ±11.6 | 67.9 | ±10.2 | 62.0 | ±11.8 | <0.001 |
| Sex | <0.001 | ||||||||
| Female | 61 | 30% | 125 | 58% | 73 | 63% | 124 | 68% | |
| Male | 143 | 70% | 90 | 42% | 42 | 37% | 59 | 32% | |
| Site | <0.001 | ||||||||
| Lima | 64 | 31% | 96 | 45% | 39 | 34% | 62 | 34% | |
| Urban Puno | 14 | 7% | 46 | 21% | 6 | 5% | 18 | 10% | |
| Rural Puno | 43 | 21% | 18 | 8% | 2 | 2% | 6 | 3% | |
| Tumbes | 83 | 41% | 55 | 26% | 68 | 59% | 97 | 53% | |
| Socioeconomic status | 0.757 | ||||||||
| Lowest | 80 | 39% | 68 | 32% | 41 | 36% | 62 | 34% | |
| Middle | 60 | 29% | 70 | 33% | 34 | 30% | 53 | 29% | |
| Highest | 64 | 31% | 77 | 36% | 40 | 35% | 68 | 37% | |
|
| |||||||||
|
Cardiometabolic factors
| |||||||||
| Blood Pressure | |||||||||
| SBP, mm Hg* | 148.9 | ±16.5 | 121.9 | ±19.3 | 156.9 | ±15.9 | 121.1 | ±11.6 | <0.001 |
| DBP, mm Hg* | 90.1 | ±12.0 | 75.9 | ±12.8 | 88.7 | ±10.3 | 73.1 | ±8.2 | <0.001 |
| Body mass index | 0.002 | ||||||||
| Healthy | 60 | 29% | 34 | 16% | 22 | 19% | 31 | 17% | |
| Excess of weight | 144 | 71% | 181 | 84% | 93 | 81% | 152 | 83% | |
| Total serum cholesterol | 0.014 | ||||||||
| Healthy | 102 | 50% | 92 | 43% | 38 | 33% | 69 | 38% | |
| Unhealthy | 102 | 50% | 123 | 57% | 77 | 67% | 114 | 62% | |
| Fasting plasma glucose | 0.001 | ||||||||
| Healthy | 131 | 64% | 151 | 70% | 57 | 50% | 103 | 56% | |
| Unhealthy | 73 | 36% | 64 | 30% | 58 | 50% | 80 | 44% | |
|
| |||||||||
|
Behavioral factors
| |||||||||
| Alcohol (AUDIT score), % | <0.001 | ||||||||
| Not-hazardous drinking | 166 | 81% | 190 | 88% | 110 | 96% | 174 | 95% | |
| Hazardous drinking | 38 | 19% | 25 | 12% | 5 | 4% | 9 | 5% | |
| Smoking status, % | 0.057 | ||||||||
| Never/former smoker | 172 | 84% | 189 | 88% | 104 | 90% | 170 | 93% | |
| Current smoker | 32 | 16% | 26 | 12% | 11 | 10% | 13 | 7% | |
| Fruit and vegetables consumption, % | 0.003 | ||||||||
| Healthy | 5 | 2% | 24 | 11% | 5 | 4% | 13 | 7% | |
| Unhealthy | 199 | 98% | 191 | 89% | 110 | 96% | 170 | 93% | |
| Leisure time physical activity, % | 0.384 | ||||||||
| Active | 9 | 4% | 10 | 5% | 2 | 2% | 11 | 6% | |
| Inactive | 195 | 96% | 205 | 95% | 113 | 98% | 172 | 94% | |
|
| |||||||||
|
History of disease
| |||||||||
| Personal history of heart disease | <0.001 | ||||||||
| No previous history | 197 | 97% | 194 | 90% | 10 | 9% | 147 | 80% | |
| Heart disease diagnosed by physician | 7 | 3% | 21 | 10% | 13 | 11% | 36 | 20% | |
| Personal history of stroke | 0.019 | ||||||||
| No previous history | 204 | 100% | 214 | 100% | 113 | 98% | 177 | 97% | |
| Stroke diagnosed by physician | 0 | 0% | 1 | 0% | 2 | 2% | 6 | 3% | |
| Family history of cardiometabolic disease** | <0.001 | ||||||||
| No previous history | 125 | 61% | 99 | 46% | 33 | 29% | 56 | 31% | |
| At least one cardiometabolic disease | 79 | 39% | 116 | 54% | 82 | 71% | 127 | 69% | |
| Family history of a chronic disease*** | <0.001 | ||||||||
| No family history | 116 | 57% | 82 | 38% | 30 | 26% | 50 | 27% | |
| At least one relative with any disease | 88 | 43% | 133 | 62% | 85 | 74% | 3 | 73% | |
Mean ± Standard deviation
Include: hypertension, heart disease, high cholesterol, diabetes and stroke.
Include: cardiometabolic diseases, tuberculosis, asthma, chronic bronchitis, chronic obstructive pulmonary disease or lung cancer.
SBP: systolic blood pressure, DBP: diastolic blood pressure, BMI: body mass index.
Factors associated with ttreatment and control of hypertension at follow-up
Individuals were followed on average for 15.5 months (±3.5 months). At follow-up, 408 (56.9%) individuals were untreated, 127 (17.7%) were uncontrolled, and 182 (25.4%) were controlled.
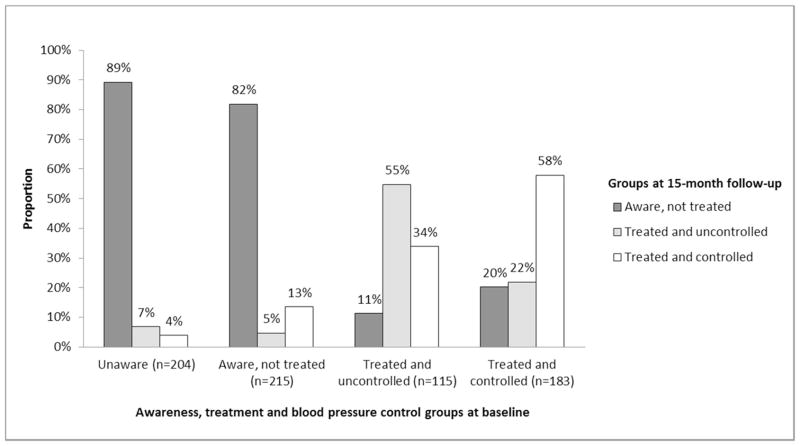
A quarter of all individuals (n=190, 26.5%) moved from their baseline A-T-C groups to other groups at follow-up. From the unaware group at baseline, 22 (10.8%) individuals became treated at follow-up, but only 8 (3.9%) had their BP controlled. From the untreated group at baseline, 39 (18.1%) individuals became treated at follow-up, and 29 (13.5%) had their BP controlled.
On the other hand, 39 (33.9%) individuals from the uncontrolled group at baseline became controlled at follow-up, but other 13 (11.3%) became untreated. From the controlled group at baseline, only 106 (57.9%) remained controlled, and 37 (20.2%) became untreated (Figure 2).
Figure 2.
Antihypertensive treatment and blood pressure control at follow-up according to baseline status (N=717)
Factors associated with treatment and BP control are presented in Table 2. Being female, having unhealthy cardiometabolic factors, personal and family history of disease were associated with taking treatment and achieving BP control at follow-up. Smoking and hazardous alcohol drinking at baseline were associated with being untreated at follow-up. Even, if individuals were treated at follow-up, they were more likely to have their BP uncontrolled.
Table 2.
Baseline characteristics associated with antihypertensive treatment and blood pressure control at follow-up.
| Socio-demographic factors | N | Aware, not treated
|
Treated and uncontrolled
|
Treated and controlled
|
|
|||
|---|---|---|---|---|---|---|---|---|
| n=408 | % | n=127 | % | n=182 | % | p-value | ||
| Age (years) * | 717 | 58.9 | ±12.4. | 66.7 | ±12.2 | 63.6 | ±10.8 | <0.001 |
| Sex | <0.001 | |||||||
| Female | 383 | 178 | 46% | 72 | 19% | 133 | 35% | |
| Male | 334 | 230 | 69% | 55 | 16% | 49 | 15% | |
| Site | <0.001 | |||||||
| Lima | 261 | 149 | 57% | 38 | 15% | 74 | 28% | |
| Urban Puno | 84 | 62 | 74% | 6 | 7% | 16 | 19% | |
| Rural Puno | 69 | 65 | 94% | 3 | 4% | 1 | 1% | |
| Tumbes | 303 | 132 | 44% | 80 | 26% | 91 | 30% | |
| Socioeconomic status | 0.643 | |||||||
| Lowest | 251 | 140 | 56% | 47 | 19% | 64 | 25% | |
| Middle | 217 | 130 | 60% | 39 | 18% | 48 | 22% | |
| Highest | 249 | 138 | 55% | 41 | 16% | 70 | 28% | |
|
| ||||||||
|
Cardiometabolic factors
| ||||||||
| Blood Pressure | ||||||||
| SBP, mm Hg* | 717 | 132.7 | ±21.7 | 150.5 | ±22.4 | 129.3 | ±18.4 | <0.001 |
| DBP, mm Hg* | 717 | 81.8 | ±13.7 | 85.4 | ±11.8 | 77.3 | ±12.8 | <0.001 |
| Body mass index | 0.084 | |||||||
| Healthy | 147 | 93 | 63% | 27 | 18% | 27 | 18% | |
| Excess of weight | 570 | 315 | 55% | 100 | 18% | 155 | 27% | |
| Total serum cholesterol | <0.001 | |||||||
| Healthy | 301 | 199 | 66% | 40 | 13% | 62 | 21% | |
| Unhealthy | 416 | 209 | 50% | 87 | 21% | 120 | 29% | |
| Fasting plasma glucose | 0.001 | |||||||
| Healthy | 442 | 272 | 62% | 61 | 14% | 109 | 25% | |
| Unhealthy | 275 | 136 | 49% | 66 | 24% | 73 | 27% | |
|
| ||||||||
|
Behavioral factors
| ||||||||
| Alcohol (AUDIT score), % | <0.001 | |||||||
| Not-hazardous drinking | 640 | 346 | 54% | 117 | 18% | 177 | 28% | |
| Hazardous drinking | 77 | 62 | 81% | 10 | 13% | 5 | 6% | |
| Smoking status, % | 0.011 | |||||||
| Never/former | 635 | 351 | 55% | 112 | 18% | 172 | 27% | |
| Current smoker | 82 | 57 | 70% | 15 | 18% | 10 | 12% | |
| Fruit and vegetables consumptions, % | 0.209 | |||||||
| Healthy | 47 | 31 | 66% | 4 | 9% | 12 | 26% | |
| Unhealthy | 670 | 377 | 56% | 123 | 18% | 170 | 25% | |
| Leisure time physical activity, % | 0.705 | |||||||
| Active | 32 | 20 | 63% | 4 | 13% | 8 | 25% | |
| Inactive | 685 | 388 | 57% | 123 | 18% | 174 | 25% | |
|
| ||||||||
|
History of disease
| ||||||||
| Personal history of heart disease | <0.001 | |||||||
| No previous history | 640 | 379 | 59% | 112 | 18% | 149 | 23% | |
| Heart disease diagnosed by physician | 77 | 29 | 38% | 15 | 19% | 33 | 43% | |
| Personal history of stroke | <0.001 | |||||||
| No previous history | 708 | 408 | 58% | 125 | 18% | 175 | 25% | |
| Stroke diagnosed by physician | 9 | 0 | 0% | 2 | 22% | 7 | 78% | |
| Family history of cardiometabolic disease** | <0.001 | |||||||
| No previous history | 313 | 220 | 70% | 44 | 14% | 49 | 16% | |
| At least one cardiometabolic disease | 404 | 188 | 47% | 83 | 21% | 133 | 33% | |
| Family history of disease*** | <0.001 | |||||||
| No family history | 278 | 196 | 71% | 41 | 15% | 41 | 15% | |
| At least one relative with any disease | 439 | 212 | 48% | 86 | 20% | 141 | 32% | |
Mean ± Standard deviation
Include: hypertension, heart disease, high cholesterol, diabetes and stroke.
Include: cardiometabolic diseases, tuberculosis, asthma, chronic bronchitis, chronic obstructive pulmonary disease or lung cancer.
SBP: systolic blood pressure, DBP: diastolic blood pressure, BMI: body mass index.
Multinomial regression analyses
Results from the nested regression model are presented in Table 3. All models used the treated and controlled group at follow-up as the reference category.
Table 3.
Relative-risk ratios of taking antihypertensive treatment and having blood pressure control at follow-up.
| N | Aware but untreated vs Treated and controlled
|
Treated but uncontrolled vs Treated and controlled
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted RRR | 95% CI | Adjust ed RRR** | 95% CI | Unadjusted RRR | 95% CI | Adjust ed RRR** | 95% CI | ||
| Groups at baseline | |||||||||
| Treated and controlled | 183 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Treated but uncontrolled | 115 | 0.95 | (0.46 – 1.98) | 2.17 | (0.85 – 5.50) | 4.28 | (2.49 – 7.35) * | 0.95 | (0.43 – 2.08) |
| Aware but untreated | 215 | 17.39 | (10.11 – 29.91) * | 16.03 | (8.83 – 29.10) * | 0.91 | (0.41 – 2.04) | 0.50 | (0.20 – 1.25) |
| Unaware | 204 | 65.18 | (29.26 – 145.17) * | 81.78 | (30.74 – 217.54) * | 4.64 | (1.81 – 11.89) * | 0.65 | (0.20 – 2.12) |
| Systolic blood pressure (5 mmHg) | 717 | 1.04 | (1.00 – 1.09) | 0.92 | (0.85 – 1.00) | 1.25 | (1.18 – 1.33) * | 1.27 | (1.16 – 1.39) * |
| Site | |||||||||
| Lima | 261 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Urban Puno | 84 | 1.92 | (1.04 – 3.56) * | 2.13 | (0.97 – 4.70) | 0.73 | (0.26 – 2.02) | 0.88 | (0.28 – 2.72) |
| Rural Puno | 69 | 32.28 | (4.39 – 237.24) * | 16.51 | (1.90 – 143.56) * | 5.84 | (0.59 – 58.08) | 6.54 | (0.61 – 70.41) |
| Tumbes | 303 | 0.72 | (0.49 – 1.06) | 0.93 | (0.55 – 1.58) | 1.71 | (1.05 – 2.80) * | 1.64 | (0.95 – 2.83) |
| Sex | |||||||||
| Female | 383 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Male | 334 | 3.51 | (2.39 – 5.14) * | 2.59 | (1.54 – 4.36) * | 2.07 | (1.28 – 3.35) * | 1.75 | (1.02 – 2.98) * |
| Age (5 years) | 717 | 0.85 | (0.79 – 0.92) * | 0.81 | (0.73 – 0.91) * | 1.12 | (1.02 – 1.23) * | 0.97 | (0.86 – 1.09) |
| Serum cholesterol | |||||||||
| Unhealthy | 416 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Healthy | 301 | 1.84 | (1.28 – 2.65) * | 1.64 | (0.99 – 2.71) | 0.89 | (0.55 – 1.44) | 0.69 | (0.40 – 1.19) |
| Family history of a chronic disease | |||||||||
| No family history | 278 | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| At least one relative with any disease | 439 | 0.31 | (0.21 – 0.47) * | 0.53 | (0.31 – 0.92) * | 0.61 | (0.37 – 1.01) | 0.58 | (0.32 – 1.05) |
p-value < 0.05
Model adjusted for all other factors simultaneously.
Risk factors for being untreated at follow-up were A-T-C status at baseline, living in rural Puno, and male sex. Increasing age and family history of chronic disease were found to be protective factors.
Among those receiving treatment at follow-up, SBP levels at baseline (for each 5 mmHg increase) and male sex were predictors of not meeting BP control targets.
Sensitivity Analysis
Using a SBP cut-off of 145 mmHg to diagnose unawareness, the distribution and the predictors of treatment and BP control at follow-up remained unchanged.
Using an SBP cut-off of 150 mmHg, the proportion of individuals untreated at follow-up increased only 1% at the expense of the controlled ones. Additionally, having healthy total serum cholesterol at baseline gained marginal statistical significance as predictor of being untreated at follow-up (RRR: 1.71, 95% CI: 1.01–2.87).
DISCUSSION
Main findings
The proportion of controlled individuals who became uncontrolled or untreated at follow-up was much higher than the proportion of unaware and untreated individuals who became treated or achieved BP control. Becoming untreated was more frequently observed among previously controlled individuals. Predictors of taking antihypertensive treatment or achieving BP control in the short-term were not the same. A-T-C status, younger age, living in Puno, and lack of family history of a chronic disease at baseline were risk factors for being untreated 15 months later; while higher SBP at baseline was risk factor of being uncontrolled in the short term. Male sex was the only predictor of both, not taking treatment and being uncontrolled 15 months later.
Comparison with other studies
In newly diagnosed hypertensive patients from developed countries, incidence of antihypertensive treatment initiation varies widely from 80% in 3 months to 40% in 4 years [27–30]. This range is much higher than the 10.8% found in our study. In addition, persistence of treatment within one year after diagnosis has been reported around 50% [31–33].
Our study shows a low rate of BP control at follow-up, even in patients with previously controlled BP. In contrast, studies from Japan and Turkey have reported BP control rates from 16% to 48% in previously uncontrolled, and from 35% to 72% in previously controlled individuals [34, 35]. However, their BP goals for patients with diabetes or older age were lower than ours.
This study shows that being female and older age were associated with taking treatment, which has been reported in other cross-sectional studies [36–38]. The protective role of healthier lifestyles including practicing leisure time physical activity and absence of smoking, as reported in other studies [38, 39], was not reproduced in our study.
Cross-sectional studies have shown the role of weight [39, 40] and lifestyle modification [41] on BP control. One recent study showed that weight gain, elevated baseline LDL cholesterol, and no reduction in fasting glucose were predictors for failing to maintain BP goals [42]. However, in our study, no cardiometabolic or behavioral factors were associated with BP control. In addition, being male was the only socio-demographic associated with uncontrolled BP in our study [36, 40, 41].
Findings interpretation
The group with unaware status at baseline may have incorporated individuals without established clinical hypertension, e.g. white-coat hypertension, elevated BP values in the presence of a health care worker but not in the home environment [43–45]; or, regression to the mean phenomena, i.e. initial elevated BP values that later turn into lower BP values without any intervention [46, 47]. These two particularities would partially explain the lack of treatment initiation at follow-up. Yet, only when SBP was set as the 150 mmHg cut-off, minimal changes were observed, showing the robustness of our results. In addition, the untreated group had a similar behavior at follow-up, suggesting that other reasons could explain this lack of treatment initiation. A qualitative study may help to elucidate if the low treatment initiation rate is because the disease is asymptomatic, the non-acceptance of having a chronic disease, the rejection to start medication [48–50], or preference to behavioral changes rather than medication [51], or if the driving of non-adherence is poor execution or non-persistence once treatment has been initiated [15]. Treatment discontinuation is a big problem since it is usually an intentional decision, and restarting treatment on these individuals is more difficult [52].
Living in rural Puno was associated with not taking treatment, which could be explained by its low-income level [38], the rural setting [39], or the low education level [53]. However, non-communicable diseases are so related with low socioeconomic status that other potential explanations need to be further explored [54]. For example, barriers for access to health care and treatment in Lima include: difficulties to get a medical appointment, low affordability of medication, reduced treatment adherence and low access to self-monitoring equipment [55]. It is expected to find low treatment rates in Puno, where 73% of population do not have a health insurance [19] and the number of inhabitants per physician is four times that of Lima [20]. Individuals with personal history of cardiovascular diseases or with family history of other chronic diseases were more likely to be treated and controlled. It suggests that having other diseases and/or other health-related experiences could influence on acceptance of disease, decision to take treatment and treatment compliance [50, 51]. Despite this observation, a warning signal comes from other longitudinal studies that have shown that hypertensive populations without other medical comorbidities are less likely to achieve BP control targets [35, 56].
Limitation and strengths
Our study has some limitations that merit consideration. Selection bias, due to individuals excluded because incomplete data, cannot be ruled out. Nevertheless, our findings about awareness, treatment and BP control prevalence are similar to other community-based studies in Latin-American population supporting the validity of our results [7, 57]. In line with previous studies, the definition of hypertension was based on BP measurements taken on a single visit [8, 37, 39, 40, 57] which could misclassify healthy individuals as unaware of their hypertension condition. As previous recommendations [21], BP measurements should be taken in two or more visits to avoid potential overestimation of hypertension status. Duration of disease and adherence to treatment was not ascertained with precision, but on the contrary, our study benefited from a large population-based study unraveling major proportions of unawareness of hypertension status and initiation of treatment in the short term.
Also, the prospective design of our study allowed the identification of protective factors as well as risk factors for well-defined profiles of treatment and control over time. These factors, albeit not modifiable, are easy to be recognized and could inform and frame resource allocation of future public health interventions targeting groups at risk. This study emphasizes the importance of identifying and distinguishing among risk factors that help to predict antihypertensive treatment from those that help to predict adequate BP control after 15 months. These characteristics should be taken in account in order to detect which patients would need more or strongest interventions to achieve goals of treatment or BP control.
CONCLUSIONS
Large treatment gaps were observed on a short-term 15-month evaluation of Peruvian adults with hypertension. Many missed opportunities for advancing BP treatment and control were identified including i) getting patients on pharmacological treatment, e.g. more than 80% of patients potentially aware of their hypertension status were not receiving treatment, ii) improving the proportion of patients on treatment that achieve control, e.g. nearly 60% of those treated at baseline remain uncontrolled, and iii) protecting the gains of those controlled, e.g. nearly 40% of those controlled at baseline discontinued treatment or were not controlled at follow up. Targeting specific populations such as men, younger individuals or those without family history of disease may increase coverage of antihypertensive treatment. Also, targeting male individuals or those with higher systolic BP could yield better rates of BP control in the short term. Better strategies, including implementation designs tailored to each of the groups studied given their risk profile paired with patient’s challenges and needs, are required to ensure better treatment coverage and control rates.
HIGHLIGHTS.
The majority of subjects with hypertension correspond to the unaware (28%) or aware but untreated (30%) categories.
Between of 80–90% of patients in these two groups remain untreated at 15 months.
42% of individuals whose blood pressure was controlled at baseline no longer do so at follow-up.
Implementation designs tailored to groups according to their risk profile together with patient’s challenges and needs are required.
Acknowledgments
The authors are indebted to all participants who kindly agreed to participate in the study. Special thanks to all field teams for their commitment and hard work, especially to Lilia Cabrera, Rosa Salirrosas, Viterbo Aybar, Sergio Mimbela, and David Danz for their leadership in each of the study sites, to Marco Varela for data coordination, as well as to Chris Meinzen for his help with the writing.
Funding: This Seed Grant has been funded in whole with federal funds by the United States National Heart, Lung and Blood Institute (NHLBI), National Institutes of Health, Department of Health and Human Services, under contract No. HHSN268200900034C and Purchase Order No. 8693-PO-011.
The CRONICAS cohort study was supported by the National Heart, Lung, and Blood Institute Global Health Initiative under the contract Global Health Activities in Developing Countries to Combat Non-Communicable Chronic Diseases (project number 268200900033C-1-0-1).
CRONICAS Cohort Study Group
Cardiovascular Disease: Antonio Bernabé-Ortiz, Juan P. Casas, George Davey Smith, Shah Ebrahim, Héctor H. García, Robert H. Gilman, Luis Huicho, Germán Málaga, J. Jaime Miranda, Víctor M. Montori, Liam Smeeth; Chronic Pulmonary Disease: William Checkley, Gregory B. Diette, Robert H. Gilman, Luis Huicho, Fabiola León-Velarde, María Rivera, Robert A. Wise; Training and Capacity Building: William Checkley, Héctor H. García, Robert H. Gilman, J. Jaime Miranda, Katherine Sacksteder.
Footnotes
Competing Interests: The authors report no conflicts of interest (financial or non-financial).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22(1):11–9. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tao L, Pu C, Shen S, Fang H, Wang X, Xuan Q, et al. Tendency for age-specific mortality with hypertension in the European Union from 1980 to 2011. Int J Clin Exp Med. 2015;8(2):1611–23. [PMC free article] [PubMed] [Google Scholar]
- 5.Mendis S, Puska P, Norrving B World Health Organization., World Heart Federation., World Stroke Organization. Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization; 2011. [Google Scholar]
- 6.Ma WJ, Tang JL, Zhang YH, Xu YJ, Lin JY, Li JS, et al. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern China. Am J Hypertens. 2012;25(5):590–6. doi: 10.1038/ajh.2012.11. [DOI] [PubMed] [Google Scholar]
- 7.Hernandez-Hernandez R, Silva H, Velasco M, Pellegrini F, Macchia A, Escobedo J, et al. Hypertension in seven Latin American cities: the Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) study. J Hypertens. 2010;28(1):24–34. doi: 10.1097/HJH.0b013e328332c353. [DOI] [PubMed] [Google Scholar]
- 8.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. Jama. 2013;310(9):959–68. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 9.Bersamin A, Stafford RS, Winkleby MA. Predictors of hypertension awareness, treatment, and control among Mexican American women and men. J Gen Intern Med. 2009;24(Suppl 3):521–7. doi: 10.1007/s11606-009-1094-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miranda JJ, Gilman RH, Smeeth L. Differences in cardiovascular risk factors in rural, urban and rural-to-urban migrants in Peru. Heart. 2011;97(10):787–96. doi: 10.1136/hrt.2010.218537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lerner AG, Bernabe-Ortiz A, Gilman RH, Smeeth L, Miranda JJ. The “rule of halves” does not apply in Peru: awareness, treatment, and control of hypertension and diabetes in rural, urban, and rural-to-urban migrants. Crit Pathw Cardiol. 2013;12(2):53–8. doi: 10.1097/HPC.0b013e318285ef60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 13.Rees K, Dyakova M, Wilson N, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2013;12:CD002128. doi: 10.1002/14651858.CD002128.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saito I, Suzuki H, Kageyama S, Saruta T. Effect of antihypertensive treatment on cardiovascular events in elderly hypertensive patients: Japan’s Benidipine Research on Antihypertensive Effects in the Elderly (J-BRAVE) Clin Exp Hypertens. 2011;33(2):133–40. doi: 10.3109/10641963.2010.546467. [DOI] [PubMed] [Google Scholar]
- 15.Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336(7653):1114–7. doi: 10.1136/bmj.39553.670231.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prugger C, Keil U, Wellmann J, de Bacquer D, de Backer G, Ambrosio GB, et al. Blood pressure control and knowledge of target blood pressure in coronary patients across Europe: results from the EUROASPIRE III survey. J Hypertens. 2011;29(8):1641–8. doi: 10.1097/HJH.0b013e328348efa7. [DOI] [PubMed] [Google Scholar]
- 17.Wu Y, Tai ES, Heng D, Tan CE, Low LP, Lee J. Risk factors associated with hypertension awareness, treatment, and control in a multi-ethnic Asian population. J Hypertens. 2009;27(1):190–7. doi: 10.1097/hjh.0b013e328317c8c3. [DOI] [PubMed] [Google Scholar]
- 18.Miranda JJ, Bernabe-Ortiz A, Smeeth L, Gilman RH, Checkley W, Group CCS. Addressing geographical variation in the progression of non-communicable diseases in Peru: the CRONICAS cohort study protocol. BMJ Open. 2012;2(1):e000610. doi: 10.1136/bmjopen-2011-000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Censos Nacionales 2007: XI de Población y VI de Vivienda. Lima, Perú: INEI; 2007. Instituto Nacional de Estadistica e Informatica. Available from: http://censos.inei.gob.pe/Censos2007/IDSE/ [Google Scholar]
- 20.Instituto Nacional de Estadística e Informática. Número de habitantes por cada médico, según departamento. Available from: http://www.inei.gob.pe/estadisticas/indice-tematico/sociales/
- 21.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 22.Howe LD, Galobardes B, Matijasevich A, Gordon D, Johnston D, Onwujekwe O, et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol. 2012;41(3):871–86. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 24.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG World Health Organization. Dept. of Mental Health and Substance Dependence. AUDIT: the Alcohol Use Disorders Identification Test: guidelines for use in primary health care. 2. Geneva: World Health Organization; 2001. [Google Scholar]
- 25.De Silva P, Jayawardana P, Pathmeswaran A. Concurrent validity of the alcohol use disorders identification test (AUDIT) Alcohol and alcoholism. 2008;43(1):49–50. doi: 10.1093/alcalc/agm061. [DOI] [PubMed] [Google Scholar]
- 26.Hausman J, McFadden D. Specification tests for he multinomial logit model. Econometrica. 1984;52(5):1219–40. [Google Scholar]
- 27.Neutel CI, Campbell NR. Antihypertensive medication use by recently diagnosed hypertensive Canadians. Can J Cardiol. 2007;23(7):561–5. doi: 10.1016/s0828-282x(07)70801-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mazzaglia G, Mantovani LG, Sturkenboom MC, Filippi A, Trifiro G, Cricelli C, et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens. 2005;23(11):2093–100. doi: 10.1097/01.hjh.0000186832.41125.8a. [DOI] [PubMed] [Google Scholar]
- 29.Johnson HM, Thorpe CT, Bartels CM, Schumacher JR, Palta M, Pandhi N, et al. Antihypertensive medication initiation among young adults with regular primary care use. J Gen Intern Med. 2014;29(5):723–31. doi: 10.1007/s11606-014-2790-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baggarly SA, Kemp RJ, Wang X, Magoun AD. Factors associated with medication adherence and persistence of treatment for hypertension in a Medicaid population. Res Social Adm Pharm. 2014;10(6):e99–112. doi: 10.1016/j.sapharm.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Lemstra M, Alsabbagh MW. Proportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysis. Patient Prefer Adherence. 2014;8:211–8. doi: 10.2147/PPA.S55382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corrao G, Soranna D, La Vecchia C, Catapano A, Agabiti-Rosei E, Gensini G, et al. Medication persistence and the use of generic and brand-name blood pressure-lowering agents. J Hypertens. 2014;32(5):1146–53. doi: 10.1097/HJH.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 33.Hasford J, Mimran A, Simons WR. A population-based European cohort study of persistence in newly diagnosed hypertensive patients. J Hum Hypertens. 2002;16(8):569–75. doi: 10.1038/sj.jhh.1001451. [DOI] [PubMed] [Google Scholar]
- 34.Yokokawa H, Sanada H, Goto A, Watanabe T, Felder RA, Jose PA, et al. Characteristics of antihypertensive medication and change of prescription over 1 year of follow up in Japan: Fukushima Research of Hypertension (FRESH) Am J Hypertens. 2010;23(12):1299–305. doi: 10.1038/ajh.2010.175. [DOI] [PubMed] [Google Scholar]
- 35.Aydogan U, Doganer YC, Atik A, Rohrer JE, Engin Gok D, Cirpan E, et al. Blood pressure control in patients with hypertension: a retrospective cohort study. J Eval Clin Pract. 2015;21(2):313–9. doi: 10.1111/jep.12318. [DOI] [PubMed] [Google Scholar]
- 36.Agyemang C, Bruijnzeels MA, Owusu-Dabo E. Factors associated with hypertension awareness, treatment, and control in Ghana, West Africa. J Hum Hypertens. 2006;20(1):67–71. doi: 10.1038/sj.jhh.1001923. [DOI] [PubMed] [Google Scholar]
- 37.Polonia J, Martins L, Pinto F, Nazare J. Prevalence, awareness, treatment and control of hypertension and salt intake in Portugal: changes over a decade. The PHYSA study. J Hypertens. 2014;32(6):1211–21. doi: 10.1097/HJH.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 38.Ferreira RA, Barreto SM, Giatti L. Self-reported hypertension and non-adherence to continuous-use medication in Brazil: a population-based study. Cad Saude Publica. 2014;30(4):815–26. doi: 10.1590/0102-311x00160512. [DOI] [PubMed] [Google Scholar]
- 39.Wang H, Zhang X, Zhang J, He Q, Hu R, Wang L, et al. Factors associated with prevalence, awareness, treatment and control of hypertension among adults in Southern China: a community-based, cross-sectional survey. PLoS One. 2013;8(5):e62469. doi: 10.1371/journal.pone.0062469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43(1):116–28. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Balijepalli C, Bramlage P, Losch C, Zemmrich C, Humphries KH, Moebus S. Prevalence and control of high blood pressure in primary care: results from the German Metabolic and Cardiovascular Risk Study (GEMCAS) Hypertens Res. 2014;37(6):580–4. doi: 10.1038/hr.2014.40. [DOI] [PubMed] [Google Scholar]
- 42.Suarez C, Galgo A, Mantilla T, Leal M, Escobar C. Variables associated with change in blood pressure control status after 1-year follow up in primary care: a retrospective analysis: the TAPAS study. Eur J Prev Cardiol. 2014;21(1):12–20. doi: 10.1177/2047487313483609. [DOI] [PubMed] [Google Scholar]
- 43.Kang YY, Li Y, Huang QF, Song J, Shan XL, Dou Y, et al. Accuracy of home versus ambulatory blood pressure monitoring in the diagnosis of white-coat and masked hypertension. J Hypertens. 2015;33(8):1580–7. doi: 10.1097/HJH.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 44.Sipahioglu NT, Sipahioglu F. Closer look at white-coat hypertension. World J Methodol. 2014;4(3):144–50. doi: 10.5662/wjm.v4.i3.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Niiranen TJ, Jula AM, Kantola IM, Reunanen A. Prevalence and determinants of isolated clinic hypertension in the Finnish population: the Finn-HOME study. J Hypertens. 2006;24(3):463–70. doi: 10.1097/01.hjh.0000209982.21112.bc. [DOI] [PubMed] [Google Scholar]
- 46.Ambrosio GB, Dowd JE, Strasser T, Tuomilehto J. The dynamics of blood pressure in populations and hypertensive cohorts. Bull World Health Organ. 1986;64(1):93–9. [PMC free article] [PubMed] [Google Scholar]
- 47.Linden A. Assessing regression to the mean effects in health care initiatives. BMC Med Res Methodol. 2013;13:119. doi: 10.1186/1471-2288-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morrell RW, Park DC, Kidder DP, Martin M. Adherence to antihypertensive medications across the life span. Gerontologist. 1997;37(5):609–19. doi: 10.1093/geront/37.5.609. [DOI] [PubMed] [Google Scholar]
- 49.Yiannakopoulou E, Papadopulos JS, Cokkinos DV, Mountokalakis TD. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12(3):243–9. doi: 10.1097/00149831-200506000-00010. [DOI] [PubMed] [Google Scholar]
- 50.Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165(10):1147–52. doi: 10.1001/archinte.165.10.1147. [DOI] [PubMed] [Google Scholar]
- 51.Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61(1):133–55. doi: 10.1016/j.socscimed.2004.11.063. [DOI] [PubMed] [Google Scholar]
- 52.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34(28):2159–219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 53.Wang W, Lau Y, Loo A, Chow A, Thompson DR. Medication adherence and its associated factors among Chinese community-dwelling older adults with hypertension. Heart Lung. 2014;43(4):278–83. doi: 10.1016/j.hrtlng.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 54.Diaz-Perera G, Bacallao J, Alemany E. Subpopulations with particular epidemiologic profiles and risks in Havana, Cuba: diabetes, hypertension, and tobacco-related illnesses. Rev Panam Salud Publica. 2012;32(1):9–14. doi: 10.1590/s1020-49892012000700002. [DOI] [PubMed] [Google Scholar]
- 55.Cardenas M, Moran D, Beran D, Miranda J. Identifying the barriers for access to care and treatment for arterial hypertension and diabetes in Lima, Peru-Executive summary. CRONICAS Center of Excellence in Chronic Diseases, Universidad Peruana Cayetano Heredia; 2014. [Google Scholar]
- 56.Yokokawa H, Goto A, Sanada H, Watanabe T, Felder RA, Jose PA, et al. Association between control to target blood pressures and healthy lifestyle factors among Japanese hypertensive patients: longitudinal data analysis from Fukushima Research of Hypertension (FRESH) Obes Res Clin Pract. 2014;8(4):e364–73. doi: 10.1016/j.orcp.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 57.Sorlie PD, Allison MA, Aviles-Santa ML, Cai J, Daviglus ML, Howard AG, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793–800. doi: 10.1093/ajh/hpu003. [DOI] [PMC free article] [PubMed] [Google Scholar]