Abstract
Capsaicin became an indispensable tool in pain research after the discovery of its unique pharmacological actions by Nicholas (Miklós) Jancsó Jr. in the late 1940s. This “History Article” introduces his achievements leading to the foundation of “sensory pharmacology” and subsequent research in that field at the University of Szeged, Hungary.
Keywords: capsaicin; chemosensitive primary afferent neurons; neurogenic inflammation; pain; sensory neurotoxin; thermoregulation; transient receptor potential vanilloid type 1 receptor; nociception, TRPV1
Abbreviations: RES, reticuloendothelial system; TRPV1, transient receptor potential vanilloid type 1; DRG, dorsal root ganglion
Motto: “Die Geschichte einer Wissenschaft ist die Wissenschaft selbst.” (Goethe)
Capsaicin became an indispensable tool in pain research after the discovery of its unique pharmacological actions by Nicholas (Miklós) Jancsó Jr. (Fig. 1) in the late 1940s. This ”History Article” introduces his achievements leading to the foundation of “sensory pharmacology” and subsequent research in that field at the University of Szeged, Hungary.
Nicholas (Miklós) Jancsó Jr. was born in Kolozsvár, Hungary (now Cluj-Napoca, Romania) in 1903 as the only son of Nicholas (Miklós) Jancsó Sr. and Fatime Paula Halász. His father was a professor of internal medicine and a renowned researcher of malaria at Ferenc József University in Kolozsvár. He paid special attention to bringing up his son to be prepared for a scientific career from his early youth. After WW1, the family moved to Szeged, where a new university was inaugurated as the legal successor of Ferenc József University in Kolozsvár. Jancsó studied at the Medical Faculty of this university in Szeged and, after finishing his studies in 1928, took up a position in the Department of Pharmacology headed by Béla Issekutz Sr., who supported Jancsó's career in many ways. After Professor Issekutz left for Budapest in 1937, Jancsó was appointed head of the Department of Pharmacology, a position which he held until his death in 1966. He was elected a member of the Hungarian Academy of Sciences in 1946.
Studies on Chemotherapeutic Action
Jancsó was initially engaged in studies dealing with problems of the chemotherapeutic action of trypanocidal compounds. He spent a 2-year (1929-31) fellowship at the Robert Koch Institute in Berlin, where he was very successful in the study of the mechanisms of action of chemotherapeutic agents. It is beyond the scope of this short review to cover in full the aspects of his research in chemotherapy, but it is worth mentioning that, by using fluorescent acridine compounds, he was the first to demonstrate that systemically injected chemotherapeutic agents accumulate in and exert their effects directly on parasites, as suggested by Paul Ehrlich. Further, he showed that resistant trypanosomes failed to accumulate the acridine compounds. These studies led to the development of a new class of trypanocidal agents on a purely theoretical basis, a discovery which was considered one of the most interesting discoveries in chemotherapy by J. H. Gaddum in his 1954 article “Discoveries in therapeutics.”
The Phenomenon of Capsaicin Desensitization
In the course of his experiments on the mode of action of chemotherapeutic agents, Jancsó became interested in the role of the reticuloendothelial system (RES) in the defense mechanisms of the organism. By developing a technique for blocking the function of the RES, he studied the significance of the RES in immunity and chemotherapeutic action. In a paper published in Nature in 1947,1 he reported that histamine is the natural activator of the RES. In that paper, he also showed that histamine activates endothelial cells, resulting in an increased vascular permeability, which could be visualized through the phenomenon of angiopexis or vascular labeling. As he put it, by using histamine it is possible to “write” onto the skin of animals injected with colloidal carbon (Indian ink). In histological preparations, many carbon-labeled small blood vessels (mainly postcapillary venules) could be visualized following painting of the skin with histamine after the prior intravenous injection of Indian ink. This histamine-induced inflammatory reaction, i.e., vascular labeling, could be prevented by repeated painting of the skin with solutions of histamine of increasing concentrations, a procedure termed local histamine desensitization.
Jancsó noted that, besides histamine, many chemical irritants can elicit the phenomenon of vascular labeling by producing cutaneous inflammation. Among the irritants, capsaicin, the pungent agent in red peppers (paprika) and mustard oil (allyl isothiocyanate), also produced vascular labeling. Since histamine desensitization prevented the development of this reaction, Jancsó at first believed that the responses elicited by irritants may also be mediated through the release of histamine. The next step, i.e., to prevent the capsaicin-induced inflammatory response by repeated local applications of the irritant, appeared obvious, at least in retrospect. The experiments showed that the capsaicin-induced inflammatory response could be largely inhibited by prior repeated administrations of the drug, a procedure termed capsaicin desensitization. Some authors who commented on these observations suggested that this discovery might be seen as a typical case of serendipity. In our opinion, this interpretation is mistaken, since, as described above, this discovery was a result of a series of well-thought out experiments where observations and experience obtained in previous experiments on the actions of histamine were consciously applied to resolve a new scientific issue. N. Jancsó's own comments on these experiments in his monograph “Speicherung”2 support this conclusion: “Unser Befund, dass die scharfschmeckenden Verbindungen die kleinen venösen Gefässe ebenso aktivieren wie das Histamin, erweckte den Gedanken, dass ähnliche Gewöhnungserscheinungen auch bei dieser Stoffgruppe vorkommen könnten. Der Einfall erwies sich als fruchtbar: es ist uns tatsächlich gelungen, das interessante Phänomen der Capsaicindesensibilisierung zu entdecken.” (“Our finding that pungent compounds activate small venules like histamine, raised the idea that analogous adaptation phenomena may also occur in the case of these agents. This idea proved fruitful: in fact, we succeeded in discovering the interesting phenomenon of capsaicin desensitization.”) These experiments laid the foundations of future research conducted with ingenious insight into the pharmacological effects of capsaicin, leading to the establishment of new fields in pharmacology and neuroscience, sensory pharmacology and the neurobiology of nociceptors.
It is worthy of mention that studies on the pharmacological effects of capsaicin on sensory functions were initiated at Ferenc József University in Kolozsvár (now the “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania [it is interesting to note that I. Hatieganu was a pupil and assistant of N. Jancsó Sr.]) and its legal successor, Ferenc József University in Szeged (after 1945 the University Medical School, and after 1990 the University of Szeged). The first observations on the actions of capsaicin were made by Endre Hőgyes in Kolozsvár in the 1870s. His most important suggestion was that capsaicin exerts its effect through its action on sensory nerves. In the 1920s, the renowned chemist T. Széky undertook systematic studies on the relation of pungency and chemical structure. Several compounds synthesized by Széky were later used by Jancsó for structure-activity studies of the irritancy and desensitizing properties of capsaicin congeners.
Activation and Desensitization of Pain Receptors by Capsaicin
The first results on the unique effects of capsaicin were communicated by N. Jancsó (Fig. 2) and his wife Aurelia Jancsó-Gábor at the annual meeting of the Hungarian Physiological Society in Budapest in 1949. It is relevant to cite a section of the abstract of this contribution here because it gives a brief, succint summary of the salient actions of capsaicin on nociceptive primary sensory neurons (translated from the Hungarian by one of the authors [G. J.] of this article).
“Certain agents affect sensory nerve endings in a hitherto unknown way, as they are capable of the desensitization of sensory nerve endings to chemical stimuli without causing true local anesthesia. It is characteristic of the desensitization of sensory nerve endings that, while reflexes elicited by their physical (mechanical) stimulation can be promptly elicited, the desensitized area is mostly or completely insensitive toward the stimulating effects of certain chemical agents. Such a desensitizing agent is capsaicin, the effect of which lasts for days and is chemically non-specific. If a solution of capsaicin is instilled repeatedly into the eyes of rats or guinea pigs, it will desensitize the eye and, finally, the animals fail to experience the irritant effect of this agent. The eyes treated in this way have also become insensitive to other types of strong irritants and lachrymose agents: the sensitivity of the eye may decrease as much as 1000-fold. Using repeated treatments, we succeeded in desensitizating the sensory nerve endings of the skin and the airways too.”
Subsequent studies disclosed that the systemic administration of capsaicin to rats, mice, guinea pigs and dogs produces a long-lasting insensitivity to capsaicin and other pain-producing irritants with diverse chemical structures. The sensitivity to non-noxious and noxious mechanical stimuli was preserved. These findings describing the unique desensitization of nociceptive afferents by capsaicin were communicated only as a short abstract by N. Jancsó and A. Jancsó-Gábor in 1959.3 Electrophysiological studies conducted by J. Pórszász and N. Jancsó supported a selective effect of capsaicin on sensory C-fibers and pointed to a peripheral site of action of the drug.4 The term “sensory neuron blocking agent” was coined by Jancsó to denote the selective effect of capsaicin on nociceptive primary afferent neurons.
Studies on the Mechanisms of Neurogenic Inflammation
Detailed studies on the mechanism of inflammatory reactions, such as the vasodilatation and plasma protein extravasation evoked by capsaicin and some other irritants, including mustard oil and xylene, revealed that they are produced through the activation of sensory nerve endings. Desensitization with capsaicin abolished these vascular reactions collectively termed the neurogenic inflammatory response. Similarly, capsaicin or mustard oil-induced plasma extravasation was completely abolished by chronic sensory denervation. Jancsó hypothesized that these vascular phenomena are of neurogenic origin and are mediated by a “neurohumour” released from sensory nerve endings which are sensitive to capsaicin. He also suggested that these chemosensitive nerve endings possess a dual function: they transmit nociceptive information toward the central nervous system, and they also release a neurohumour from their peripheral endings, which produces local vasodilatation and an increase in vascular permeability, i.e. neurogenic inflammation. This concept differed significantly from the classical axon reflex theory of Lewis, although neurogenic inflammation and especially neurogenic sensory vasodilatation are related phenomena. Whereas the axon reflex theory hypothesized separate axon collaterals with afferent and efferent functions, respectively, Jancsó suggested that the sensory axon collaterals are similar and, if stimulated, propagate action potentials conveying nociceptive information toward the central nervous system and concomitantly release vasoactive mediators which produce the neurogenic inflammatory response in the periphery. He also showed that local anesthetics inhibited the transmission of nociceptive information, but failed to affect the neurogenic inflammation. Extensive study of the functions of these particular chemosensitive afferent nerves sensitive to capsaicin revealed that they are involved in a variety of functions of many organs and tissues of the body, now generally referred to as the sensory efferent or local regulatory function of sensory nerves (for a review and references, see ref. 5).
Acording to N. Jancsó, the depletion of the “neurohumour,” later identified as neuropeptides such as substance P and calcitonin gene-related peptide contained in primary afferent neurons, may explain the characteristic features of desensitization following the administration of large doses of capsaicin. Although the mechanisms of capsaicin desensitization turned out to be more complex, and still not clarified in all details, this contention is still valid as far as the sensory efferent/local regulatory functions of nociceptors are considered.
Effects of Capsaicin on Thermoregulation
The first report on the thermoregulatory effects of capsaicin and related compounds was published by N. Jancsó in “Speicherung.”2 This monograph gave a thorough account of the extensive research which he had pursued over a period of about 20 years on the functions of tissue macrophages, the RES and the storage function of kidney tubular cells. Several chapters dealt with issues concerning the mechanisms of neurogenic inflammation elicited with capsaicin and other irritants. He studied the effects of a number of related compounds in order to determine the structural requirements for compounds to meet to be able to activate the pain receptors. It was established that the presence of a substituted aromatic ring and the acylamide bond is essential for the induction of activation and the subsequent desensitization of pain receptors.
In the course of the study of the mechanism of capsaicin desensitization, the effects of capsaicin on thermoregulation were also revealed. Animals given single low systemic doses of capsaicin developed a marked, but transient decrease in body temperature of up to 5–7°C. Interestingly, animals given large systemic doses of capsaicin developed a long-lasting, apparently irreversible impairment of the regulation of their body temperature in a warm environment. Capsaicin-desensitized rats also exhibited an exaggerated febrile response to pyrogens. Although the exact mechanism of this thermoregulatory disturbance is still unclear, besides an altered function of peripheral warm sensors, an impairment of hypothalamic “thermodetectors” was demonstrated. Experiments by N. Jancsó, J. Szolcsányi and K. Thuránszky disclosed that the injection of capsaicin into the hypothalamic preoptic area produced decreases in core body temperature in cats and rats. Further, repeated injections of capsaicin produced desensitization to its own effect and abolished the thermoregulatory responses of hypothalamic warming too. In the 1980s, the thermoregulatory effects of capsaicin and the relationship between thermoregulation and sleep were further studied by Ferenc Obál, Jr. and his colleagues. Inter alia, they observed that central impairments in thermoregulation were much less pronounced in rats treated neonatally with capsaicin; hence, centrally administered capsaicin, serotonin and hypothalamic warming elicited thermoregulatory responses similar to those in the controls. These findings were of particular importance in the light of recent findings that antagonists of the capsaicin/transient receptor potential vanilloid type 1 (TRPV1) receptor, regarded as potential analgesics, produced hyperthermia in both animals and man.
The Legacy of Nicholas Jancsó
The engagement of N. Jancsó in the study of pain mechanism by using capsaicin and related compounds as research tools spanned over more then 2 decades from the early 1940s until his untimely death at the age of 63 in 1966. During his lifetime, almost nothing of these fundamental findings was published in international scientific journals for various reasons. Publication from an Eastern European country in western scientific journals was not easy for political reasons and additionally he had become tired of arguing with journal referees. In the early days of “capsaicin research,” the attitude toward the new ideas of N. Jancsó on the pharmacology of pain receptors can be well illustrated by quoting Lembeck's comment6 on a lecture given by N. Jancsó in Tübingen: “I knew Jancsó's work on the extinction of pain by capsaicin. I invited him to Tübingen for a seminar. Jancsó explained in the seminar his simple, but conclusive experiments, and I was probably the only one in the audience who was convinced that he was right.” This was not a unique experience in the course of “capsaicin research.” Much later, in 1987, one of the present authors (G. J.) received harsh criticism from reviewers of a highly rated scientific journal of the field in connection with a manuscript discussing the possible use of capsaicin-type compounds for pain relief. Nowadays, however, the use of capsaicin and related agents, including the capsaicin receptor antagonists, in pain therapy is commonplace and further possibilities for their use to alleviate pain are continuously sought for.
Most of the results of N. Jancsó's experiments on the effects of capsaicin were published in detail only after his death, by his wife, Aurelia [Aranka] Jancsó-Gábor, who had been working with him from the very beginning of the studies concerned with the pharmacological actions of capsaicin, and by János Szolcsányi, who joined Jancsó only 4 years before Jancsó's death in 1966. N. Jancsó and A. Jancsó-Gábor reported on the first results of the highly selective desensitizing effect of capsaicin at the XVth Meeting of the Hungarian Physiological Society in 1949, and at a meeting of the German Pharmacological Society in 1959, and on the thermoregulatory effects of capsaicin in 1965 at a meeting of the German Pharmacological Society. Together with A. Jancsó-Gábor, Szolcsányi made a valuable contribution by summarizing and publishing the most important data and concepts of Jancsó's work in the next few years before leaving Szeged.
N. Jancsó's groundbreaking observations not only demonstrated the possibility that the function of nociceptive primary sensory neurons can be fundamentally influenced by pharmacological means, but also clarified many aspects of the function of pain receptors, apart from their role in the sensation of pain. His achievements were honored by several national and international awards and by comments from great Hungarian scientists, including János (John) Szentágothai, who remembered him in his introductory remarks to a symposium on “Capsaicin and the sensory system” held in Budapest in 1985, as follows: “Jancsó was undoubtedly the greatest genius of post World War II Hungarian biomedical sciences.”
The Discovery of the Selective Neurotoxic Effect of Capsaicin and its Significance
Although N. Jancsó's results had clearly revealed that capsaicin acts in a very specific, unique way on pain receptors, the morphological identity, the neurochemical profile and the possibilities to block the function of nociceptive afferents serving specific tissues or organs remained to be clarified. The discovery of the selective neurotoxic/neurodegenerative action of capsaicin contributed significantly to the tackling of these important issues. In 1977, one of the present authors (G. J.) and his colleagues, Elizabeth Király and A. Jancsó-Gábor, published a paper in Nature7 demonstrating that capsaicin administered to newborn rats resulted in the selective degeneration and life-long elimination of C-fiber chemosensitive primary sensory neurons, amounting to about 50% of the total neuronal population in the spinal and cranial sensory ganglia. The effect of this sensory neurotoxin was specific for nociceptive primary afferent neurons which transmit chemogenic pain and mediate the neurogenic inflammatory response. By making use of the selective neurotoxic effect of capsaicin the central nervous system distribution of spinal and cranial nociceptive primary afferents was revealed for the first time through the use of classical light and electron microscopic histological techniques. Since neonatal capsaicin treatment produces selective chemodenervation by eliminating nociceptive primary sensory neurons, comparative immunohistochemical studies on control and capsaicin-treated animals provided an opportunity for the identification of the putative peptide mediator(s) of pain. This was made possible through collaboration with Professor Tomas Hökfelt and his colleagues at the Karolinska Institutet, with whom Ferenc Joó, my (J. G.) first mentor, and Norbert Halász, who at that time was working at the Karolinska Institutet, maintained good personal relationships. These studies supported and extended previous findings by showing that, besides substance P, other peptides, such as somatostatin and cholecystokinin, are also present in nociceptive spinal and cranial sensory ganglion cells. The putative transmitter role of substance P in capsaicin-sensitive primary afferents was suggested in 1978 by Jessel, based, in part, on our earlier findings that capsaicin treatment resulted in the abolition of fluoride-resistant acid phosphatase from the substantia gelatinosa, the principal termination site of nociceptive afferents: “The striking similarity between the distribution of substance P and the fluoride-resistant acid phosphatase in spinal cord led us to investigate the possibility that capsaicin-induced desensitization may be mediated by an action on substance P-containing primary afferent terminals in the substantia gelatinosa.”
The experimental paradigm involving comparative studies on control and neonatally capsaicin-treated animals which lacked C-fiber nociceptive primary afferent neurons was extensively utilized in many laboratories to study the contribution of this special population of afferents to mechanisms of pain, inflammation, immune responses and a variety of visceral functions. In our laboratory, experiments in this respect revealed the role of chemosensitive afferent nerves in the modulation of cutaneous inflammatory reactions, the cardiac function and protection, cardiorespiratory reflexes, headache mechanisms, gastrointestinal circulation and thermoregulation (for reference see Nagy et al.8).
The observations on the neurotoxic effects of capsaicin facilitated further research in many ways. According to Gold and Caterina,9 “One early clue that nociceptive neurons might express signaling proteins distinct from those of other neuronal subtypes was the observation that exposure of neonatal rats to capsaicin, the main pungent ingredient in hot peppers, produces a lifelong depletion of small-diameter sensory neurons, with no such effects on larger diameter neurons. As adults, these animals exhibit diminished responsiveness not only to subsequent capsaicin challenge, but also to other painful stimuli (Jancsó, G. et al., 1977).” The observation that the administration of capsaicin elicited an increase in intracellular free calcium concentration was later utilized for the selection of clones of cultured sensory ganglion cells which expressed the capsaicin/vanilloid receptor type 1. Evidence for the existence of a capsaicin receptor was presented in 1990 by Szallasi and Blumberg in binding studies involving the use of resiniferatoxin. The cloning and identification by Caterina and his colleagues9 of the capsaicin receptor, in 1997, as a non-selective cation channel with a high calcium permeability, now termed the TRPV1 receptor, was of fundamental significance as regards further investigations into the molecular mechanisms of nociception and the evaluation of the role of TRPV1 receptors in a variety of somatic and visceral functions, and in the central nervous system.
Obviously, neonatal treatment with capsaicin affects all capsaicin-sensitive primary afferent neurons in the organism. In further experiments, however, we made the observation that local application of capsaicin onto a peripheral nerve selectively and permanently blocked the function of nociceptive afferents. Hence, by using this approach, it is possible to produce a selective chemodenervation of any tissue or organ by treating the nerves which serve them with capsaicin. This technique has therefore become a widely used approach with which to study the functional significance of these particular somatic and visceral, e.g., vagal nociceptive afferents in different physiological or pathological processes. Since this treatment produces selective regional analgesia, it has been proposed as a possible approach to alleviate pain. The findings additionally pointed to the possibility that axons of nociceptive neurons also express receptors sensitive to capsaicin. One of the authors of this article (G. J.) had the privilege to clarify the neurochemical consequences of perineural capsaicin treatment with Rainer Gamse and Ulrike Petsche in the laboratory of Professor Fred Lembeck, who was impressed by the idea of blocking the function of nociceptive afferents in that way (“again such a simple clever Hungarian idea”). It emerged that perineural capsaicin selectively blocks axonal transport processes in sensory nerves and results in the long-lasting depletion of neuropeptides from sensory ganglion cells.
Other modes of application of capsaicin, such as injection of the drug into the subarachnoid space, have also been introduced, thereby contributing further to the understanding of the functional traits of chemosensitive primary afferent neurons. Hence, the observations that, following an intracisternal injection of capsaicin, the protective wiping reflex observed in controls after the instillation of zingerone or capsaicin into the eye of the rat was completely abolished, but the ability of irritants such as capsaicin or mustard oil to produce neurogenic inflammation in the eyelids or in the skin remained unaffected, provided direct experimental evidence of the dual functional character of these nociceptive primary afferent neurons. Morphological and neurochemical studies revealed that, under these experimental conditions, dissociation of the afferent and the efferent functions of nociceptive neurons could be accounted for by a selective degeneration of the central medullary terminations of these neurons. It was suggested that the sensory ganglion cell perikaryon with its peripheral processes comprises an independent functional entity capable of responding to peripheral (inflammatory) stimuli by the release of vasoactive peptides from its peripheral endings, independently of the central nervous system, i.e., without the contribution of a dorsal root root reflex, for instance.
Novel Mechanisms Involved in Nociceptor Analgesia
Studies on the chemical changes of injured primary sensory neurons led us to examine the possible role of gangliosides, and in particular GM1, in the nociceptor function. Experiments on cultured dorsal root ganglion cells revealed that the inhibition of neural ganglioside synthesis significantly reduced not only the activation of the TRPV1 ion channel by capsaicin in DRG neurons, but also the expression of the TRPV1 receptor protein. We suggested that pharmacological manipulation of the intracellular level of certain ganglioside species may provide a novel approach for modulation of the nociceptor function and possibly for the production of nociceptor analgesia.10
Final Remarks
The ultimate goal of research in the field of pain is undoubtedly the development of novel analgesics and better treatment options. Although our knowledge on pain mechanisms has been greatly advanced through the introduction of capsaicin into the study of sensory functions, the possibility of translating theoretical knowledge into treatment options remains a continuing challenge for pain medicine.
It is the authors' hope that readers of this “History Article” may find it interesting to catch a glimpse of the beginnings and early developments in a research field that has now firmly established itself in the realm of modern neuroscience. A critical evaluation of the work of N. Jancsó and other researchers in Szeged possibly awaits further “History Articles.” However, it is probably appropriate to state that their concepts, methods and experimental approaches to the study of the problems of pain may have left a lasting impact on research in sensory physiology.
Figure 1.
Nicholas Jancsó in the late 1950s. This photograph was taken in the Department of Pharmacology, University of Szeged. (From the family archive of G. Jancsó).
Figure 2.
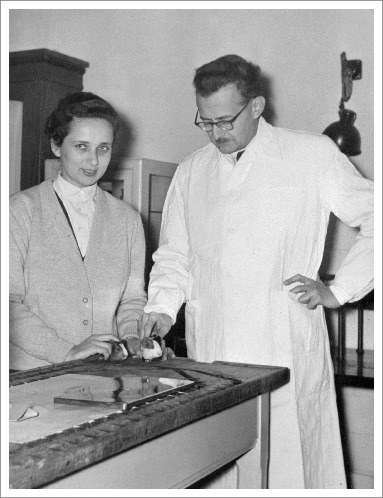
N. Jancsó and A. Jancsó-Gábor in the late 1950s. The note on the back of the photograph indicates that the 2 guinea-pigs have already been desensitized with capsaicin and are no longer sensitive to chemical irritants. This photograph was taken in the Department of Pharmacology, University of Szeged. (From the family archive of G. Jancsó).
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Jancsó N. Nature 1947; 160:227–8; http://dx.doi.org/ 10.1038/160227a0 [DOI] [PubMed] [Google Scholar]
- 2.Jancsó N. Speicherung. Stoffanreichung im Retikuloendothel und in der Niere. Budapest: Akadémiai Kiadó, 1955. [Google Scholar]
- 3.Jancsó N, et al.. Naunyn-Schmiedeberg's Arch exp Path Pharmak 1959; 236:142–3. [Google Scholar]
- 4.Pórszász J, et al.. Acta Phsiol Sci Hung 1959; 16:299–306. [PubMed] [Google Scholar]
- 5.Jancsó G. Neurogenic Inflammation in Health and Disease. Amsterdam: Elsevier, 2009. [Google Scholar]
- 6.Donnerer J, et al.. The Chemical Languages of the Nervous System. Basel: Karger, 2006. [Google Scholar]
- 7.Jancsó G, et al.. Nature 1977; 270:741–3; http://dx.doi.org/ 10.1038/270741a0 [DOI] [PubMed] [Google Scholar]
- 8.Nagy I, et al.. Eur J Pharmacol 2004; 500:351–69; PMID:15464045; http://dx.doi.org/ 10.1016/j.ejphar.2004.07.037 [DOI] [PubMed] [Google Scholar]
- 9.Gold MS, et al. In: Basbaum AI et al. eds. The Senses: A Comprehensive Reference Vol. 5. San Diego, CA: Academic, 2008:43–74. [Google Scholar]
- 10.Sántha P, et al.. Pain 2010; 150:103–12; http://dx.doi.org/ 10.1016/j.pain.2010.04.006 [DOI] [PubMed] [Google Scholar]


