Abstract
Care of burn-injured patients requires knowledge of the pathophysiologic changes affecting virtually all organs from the onset of injury until wounds are healed. Massive airway and/or lung edema can occur rapidly and unpredictably after burn and/or inhalation injury. Hemodynamics in the early phase of severe burn injury are characterized by a reduction in cardiac output, increased systemic and pulmonary vascular resistance. Approximately 2–5 days after major burn injury, a hyperdynamic and hypermetabolic state develops. Electrical burns result in morbidity much higher than expected based on burn size alone. Formulae for fluid resuscitation should serve only as guideline; fluids should be titrated to physiologic end points. Burn injury is associated basal and procedural pain requiring higher than normal opioid and sedative doses. Operating room concerns for the burn-injured patient include airway abnormalities, impaired lung function, vascular access, deceptively large and rapid blood loss, hypothermia and altered pharmacology.
INTRODUCTION
In the United States approximately 450,000 people seek treatment for burn injury each year, of whom 40,000 are hospitalized and 3,400 die.* The majority of these patients present in emergency rooms of hospitals without a burn center. Initial care of patients with serious burn injury presents challenges in airway management, vascular access and hemodynamic and pulmonary support. Anesthesiologists are specialists in each of these areas. As a result, anesthesiologists staffing these hospitals with emergency rooms must be familiar with the pathophysiology of major burn injuries and resuscitation. In burn care facilities, anesthesiologists should be familiar with the unique features of perioperative management of burn injured patients. This review will focus on early evaluation and perioperative management of burned patients in the acute (nonreconstructive) phase only.
BURN INJURY PATHOPHYSIOLOGY
Major burns cause massive tissue destruction and result in activation of a cytokine-mediated inflammatory response that leads to dramatic pathophysiologic effects at sites local and distant from the burn. The systemic effects occur in two distinct phases, a burn shock (ebb) phase followed by a hypermetabolic (flow) phase, first described by Cuthbertson in 1942.1 Understanding the pathophysiologic alterations and time course is essential for the clinician providing early resuscitation and perioperative care for these patients.
Generalized edema even in noninjured tissues occurs when the injury exceeds 25–30% total body surface area (TBSA). After major burn injury continued loss of plasma into burned tissue can occur up to the first 48 h or even longer. Loss of intravascular fluid into burned areas and edema formation (in nonburned sites) can quickly result in burn shock with impaired tissue and organ perfusion. In contrast to nonburn trauma, burn-induced fluid loss occurs in the absence of marked red cell volume loss resulting in hemoconcentration rather than anemia. Thus, the initial therapeutic goal is the repletion of intravascular volume with clear fluids to preserve tissue perfusion and minimize the ischemia and inflammatory responses. Burn shock occurs not only because of depletion of intravascular volume but also due to elevated systemic vascular resistance (due to release of catecholamines, antidiuretic hormone, and hemoconcentration) and depressed cardiac output (fig. 1). Depression of cardiac output occurs even before any detectable reduction in plasma volume. The depressed cardiac output continues for 24–36 h.2 The hypermetabolic and hyperdynamic phase which develops over 48 to 72 h after injury is characterized by increased oxygen consumption, carbon dioxide production and protein wasting.3,4 Pari Passu with the hypermetabolism is the hyperdynamic phase evidenced by supranormal cardiac output (often >2–3 times normal), tachycardia and decreased systemic vascular resistance (fig. 2). The onset of sepsis further increases the cardiac output and decreases systemic vascular resistance.3,4 Elderly patients may not exhibit signs of the hyperdynamic state but protein catabolism is ubiquitous.
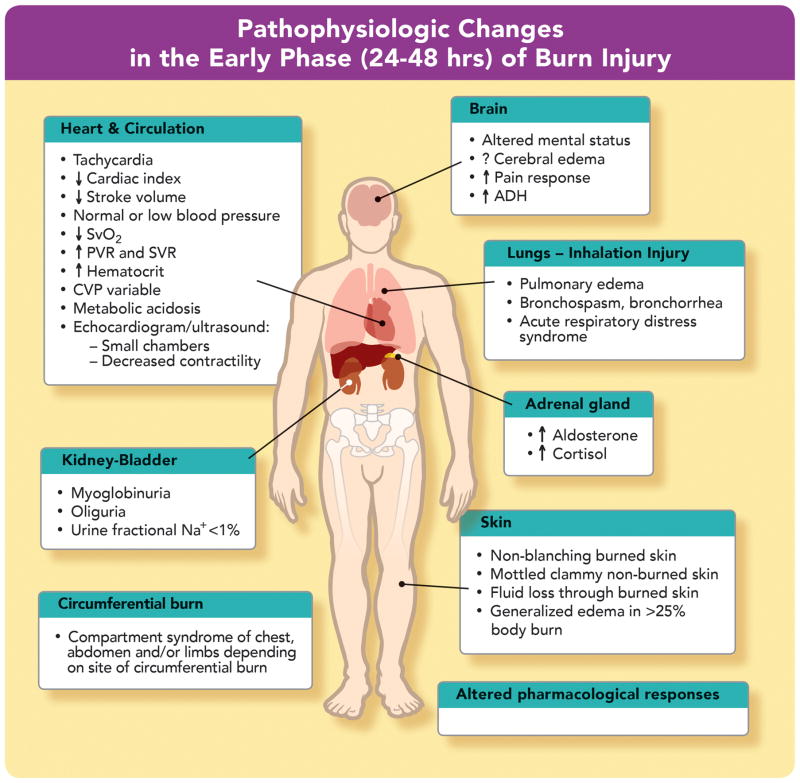
FIGURE 1. Pathophysiologic changes in the early phase (24–48 h) of burn injury.
The early (ebb) phase of burn injury is characterized by decreased cardiac output, and decreased blood flow to all organs. The decreased cardiac output is due to loss of intravascular volume, direct myocardial depression, increased pulmonary and systemic vascular resistance (PVR and SVR, respectively) and hemoconcentration, and can lead to metabolic acidosis, and venous desaturation (↓SVO2). Decreased urine flow results from decreased glomerular filtration, and elevated aldosterone and antidiuretic hormone levels (ADH) levels. Oxygenation and ventilation problems can occur due to inhalation injury and/or distant effects of burn on airways and lung. Compartment syndrome ensues if there is circumferential burn with no escharotomy performed to release the constriction. Compartment Syndrome can also occur in abdomen, extremities or orbits without local or circumferential burns. Mental status can be altered because of hypoxia, inhaled toxins and/or drugs. The reasons why heart rate, blood pressure, and central venous pressure (CVP) can be poor indicators of volume status are explained in table 3.
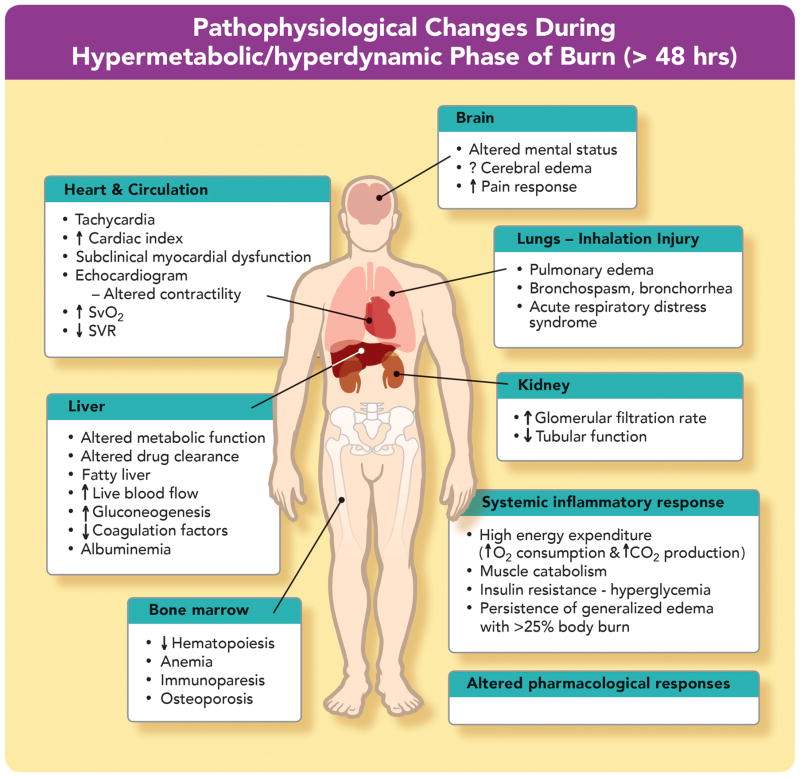
FIGURE 2. Pathophysiological changes during hypermetabolic/hyperdynamic phase of burn.
At 48–72 h after burn, the hypermetabolic-hyperdynamic (flow) phase starts, characterized by increased oxygen consumption, carbon dioxide production, and cardiac output, with enhanced blood flow to all organs including skin, kidney (glomerular filtration rate [GFR]) and liver, and decreased systemic vascular resistance (SVR). Increased venous oxygen saturation (↑SVO2) is related to peripheral arteriovenous shunting. The markedly decreased SVR mimics sepsis. Lungs and airways may continue to be affected because of inhalation injury and/or acute respiratory distress syndrome. Pulmonary edema can occur due to distant effects of major burn and to reabsorption of edema fluid (hypervolemia). The altered mental status may be related to burn itself and/or concomitant drug therapy. Release of catabolic hormones and insulin resistance leads to muscle protein catabolism and hyperglycemia.
INHALATION INJURY
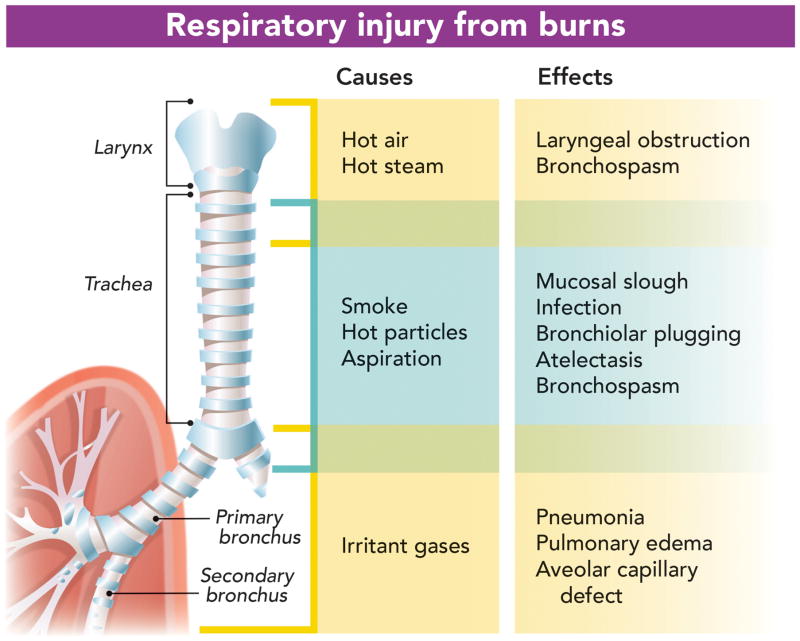
The presence of an inhalation injury significantly increases the morbidity and mortality associated with burn injuries. Resuscitation fluid requirements are increased by up to 50%.5–7 Chest radiographs are usually normal until secondary complications of inflammation, infection or atelectasis develop. The mechanisms of inhalation injury (fig. 3) consist of a combination of (a) direct injury to face and upper airway from inhalation of steam and/or hot gases, (b) chemical injury to the trachea and bronchi, and alveolar and endothelial lining due to inhalation of the toxic products from the fire (c) impairment of oxygen transport processes or oxygen utilization by inhalation of carbon monoxide and cyanide, respectively.5–10
FIGURE 3. Respiratory inadequacy due to direct injury: putative agents and site of injury.
The noxious agents released from the burning material can affect different parts of the airway. The cartoon indicates which part of the respiratory system is affected by each gas, toxin or chemical (“Cause”). The pathophysiological effects of each of these noxious agents is also indicated (“Effects”). Thermal or chemical injury can lead to edema of face, pharynx, glottis and larynx. Injury to trachea and bronchi leads to bronchospasm and bronchorrhea. Chemical and toxin injury can lead to alveolar damage and pulmonary edema.
Direct heat and steam injury to the upper airway can lead to marked swelling of the face, tongue, epiglottis, and glottic opening resulting in airway obstruction. Because airway swelling may not occur immediately but may develop over a period of hours (especially with concurrent fluid resuscitation), a high index of suspicion and frequent re-evaluations of the respiratory status are essential. Upper airway edema will have more immediate consequences in smaller children. A scald injury of the epiglottis mimics symptoms of epiglottitis (see video, Supplemental Digital Content 1). Upper airway edema usually resolves in 3–6 days and is facilitated by elevation of the head of the bed and avoidance of excessive fluid administration. Positive pressure ventilation may increase resuscitation fluid requirements.6
Tracheobronchial injury is caused by inhalation of chemicals in smoke. Smoke from a house fire contains combustion products that are toxic and damaging to the airways and alveoli (fig. 3, see video, Supplemental Digital Content 2). Decreased mucociliary transport impairs clearance of bacteria and mucosal debris.8 Alveolar collapse and atelectasis can occur because of loss of surfactant production or from plugging of small airways by mucosal debris. Over a period of time, these changes result in obstruction of airways, bronchospasm, and atelectasis which cause ventilation perfusion mismatch, shunt, impaired gas exchange and decreased pulmonary compliance. Injury to the airways and lung can also occur with severe cutaneous burns in the absence of inhalational injury. Mechanisms include inflammatory mediators from the burn-injured area, effects of fluid resuscitation, and infection. For example, acute lung injury can occur in patients with scald injury without smoke exposure. Two to three days after scald injury the bronchoscopic features resemble airway injury5,8,9 due to smoke exposure (see video, Supplemental Digital Content 3).
Systemic toxicity can also occur from smoke inhalation. Exposure to carbon monoxide decreases oxygen carrying capacity of hemoglobin leading to tissue hypoxia. Carbon monoxide has a 200 fold higher affinity than oxygen to the same binding sites on hemoglobin.10 Binding of carbon monoxide to hemoglobin also shifts the oxyhemoglobin dissociation curve to the left and alters its shape. Carboxyhemoglobin levels >15% are toxic; those exceeding 50% are lethal. The half-life of carboxyhemoglobin is 4 h for a person breathing room air. This is reduced to 40–60 min when breathing 100% oxygen. Hyperbaric oxygen therapy has been suggested as a therapy to reduce the neurologic sequelae from carbon monoxide toxicity. Hyperbaric oxygen therapy may play a beneficial role in reducing the inflammation and harmful effects of ischemia reperfusion injury caused by carbon monoxide exposure. However a recent Cochrane review failed to demonstrate convincing benefit from hyperbaric oxygen therapy.11 The limited availability of hyperbaric chambers even in academic institutions makes its usefulness limited.
Cyanide is a toxic gas produced in fires by the burning of nitrogenous materials. Cyanide poisoning should be suspected in any patient with a history of smoke inhalation injury with an anion gap metabolic acidosis in the presence of apparently adequate oxygen delivery. Cyanide binds to mitochondrial cytochrome oxidase blocking the last step in the oxidative phosphorylation preventing the use of oxygen for conversion of pyruvate to adenosine triphosphate. Thus, cells can only generate adenosine triphosphate via anaerobic metabolism, which results in a metabolic acidosis from lactic acid production. Concentrations of cyanide greater than 20 ppm are considered dangerous. Concentrations of 100 ppm can lead to seizures, coma, respiratory failure, and death.12 The mixed venous oxygen saturation in cyanide poisoning is often elevated, suggesting inability to use the delivered oxygen.13,14
The treatment of inhalation injury, other than carbon monoxide and cyanide, is supportive respiratory care with airway management, lung protective mechanical ventilation and aggressive pulmonary toilet. Clinical manifestations of an inhalation injury may be delayed up to several days postexposure. Nebulization of anticoagulants, antioxidants and antiinflammatory agents are under investigation but are not part of routine management at this time.15–17 Prophylactic administration of antibiotics and steroids are not routinely recommended.
Mortality persists at a rate of approximately 4% for patients admitted to burn centers.* A large analysis revealed three risk factors as predictive of death after burns: age older than 60 yr, burn size greater than 40% body surface area, and inhalation injury. Mortality is a function of the number of risk factors present.18 The mortality was 0.3, 3, 33, or 90% depending on whether 0, 1, 2, or 3 risk factors were present, respectively. Morality related to burn injury has improved over the last several decades.19 Causes include increased awareness and improved methods of resuscitation, early excision and grafting of burn wounds, better methods of wound coverage, improved anesthesia and intensive care techniques, early diagnosis and aggressive treatment of infections, and enhanced nutritional support methods, particularly early and continuous enteral feeding. Data exist linking improved outcomes from major burns with early referral to a burn center. It is recognized that burn care requires specialized expertise, personnel, and equipment that are not cost-effectively maintained in low-volume centers.
INITIAL EVALUATION AND MANAGEMENT
Successful management of the patient with burn injury begins at the scene of injury and continues in the emergency department with a thorough trauma assessment based on the Advanced Trauma Life Support guidelines. This requires a combined strategy of airway assessment and protection, initiation of resuscitation and evaluation for coexisting injuries. Between 5% and 7% of patients admitted to burn centers suffer from nonthermal traumatic injuries.20 Therefore, all burned patients should be approached initially as multiple-trauma patients. Assessing the airway is the first priority during the initial evaluation. The presence of airway injury, signs of airway obstruction and presence of preexisting airway abnormality should be assessed as soon as the patient arrives at the hospital. Airway injuries may not be evident initially, but with massive fluid resuscitation airway edema can result (see video, Supplemental Digital Content 1). As a general rule, when indicated, it is safer to intubate the patient early than risk a difficult intubation after airway swelling has occurred.
Laryngeal injuries are common in burn injured patients and can be associated with long term morbidity. Early recognition of laryngeal injury and consultation with a laryngologist can influence treatment choices (e.g., tracheostomy) and limit morbidity.21 Since anesthesiologists are most likely to view the larynx of patients with acute burns, it is important to make laryngeal examination part of the initial intubation whether during resuscitation or induction of general anesthesia. Decreased pulmonary compliance because of a circumferential eschar on the chest or abdomen can interfere with respiration. Chest wall escharotomy may be needed when this occurs.
It is important to recognize inhalation injury as soon as possible. A diagnosis of inhalation injury is usually based on a history of exposure to fire and smoke (especially in combination with impaired avoidance behavior such as loss of consciousness or entrapment in an enclosed space) along with the physical examination (burns over face, singed nasal or facial hair, carbonaceous sputum, hypoxia, hoarse voice, and bronchorrhea and/or bronchospasm). Fiberoptic bronchoscopy may be used to support the diagnosis, and may reveal carbonaceous debris, erythema, or ulceration. (see video, Supplemental Digital Content 2) It has been difficult to identify reliable indicators of progressive respiratory failure in patients with smoke inhalation.22 Diagnostic criteria for inhalation injury are complicated by heterogeneous presentation.
Intubation of burn-injured patients, especially combined with interhospital transport is not a benign intervention. In response to the death of a burn injured patient from complications of intubation subsequently judged to not to be indicated, the Parkland Hospital burn staff performed a retrospective review of the hospital course of burn patients intubated prior to transport to their emergency department.23 A large number of these patients were extubated the same or the next day suggesting that intubation was not indicated in these patients. Thus, they were exposed to risk without commensurate benefit. Out of concern for exacerbation of a thermal laryngeal injury, otolaryngologists at the Baltimore Regional Trauma Center performed a prospective study of patients presenting to their emergency department with risk factors for inhalation injury.24 If patients at risk were not in respiratory distress and did not have other indications for immediate intubation such as large full thickness burns, inability to protect their airway, or signs of obstruction, then they were evaluated by flexible fiberoptic laryngoscopy. All the patients with an adequate glottis by endoscopy were managed safely without intubation despite the fact that many met the institution’s traditional criteria for intubation. Although adult patients with facial burns may appear to be at significant risk, the airway may not be compromised and intubation may expose them to unnecessary risk. In contrast, we have seen pediatric patients with oral scald who did not appear in distress and who, on superficial exam did not seem to have significant injury but actually had serious thermal injury resembling epiglottitis (see video, Supplemental Digital Content 1). All patients with significant risk for inhalation injury should have a thorough airway exam and intubation should be performed early when the airway is compromised. Preemptive intubation of patients with inhalation injury can be lifesaving but should be performed for clear indications. Facial burns or glottic edema may make it difficult to secure an endotracheal tube after edema develops. Therefore, extra effort and vigilance is required in these patients.
Standard pulse oximeters cannot distinguish between oxyhemoglobin and carboxyhemoglobin. The PaO2 can be normal or high in patients receiving oxygen therapy even with high levels of carboxyhemoglobin. The diagnosis of carbon monoxide poisoning is made by measuring the carboxyhemoglobin level in arterial blood, or measuring oxygen carrying capacity of hemoglobin by cooximeter. Some pulse oximeters can differentiate between oxyhemoglobin and carboxyhemoglobin.
As with carbon monoxide poisoning, cyanide toxicity can be difficult to diagnose. Cyanide toxicity, just like carbon monoxide poisoning, does not cause cyanosis and direct detection of cyanide poisoning in blood is difficult. The deleterious effects of cyanide are normally neutralized by the conversion of cyanide to thiocyanate, which is excreted in the urine. This can be enhanced by the administration of exogenous thiosulfate. Exogenous thiosulfate has a slow onset of action and therefore coadministration of hydroxycobalamin (Vitamin B12) has been recommended which forms cyanocobalamin.
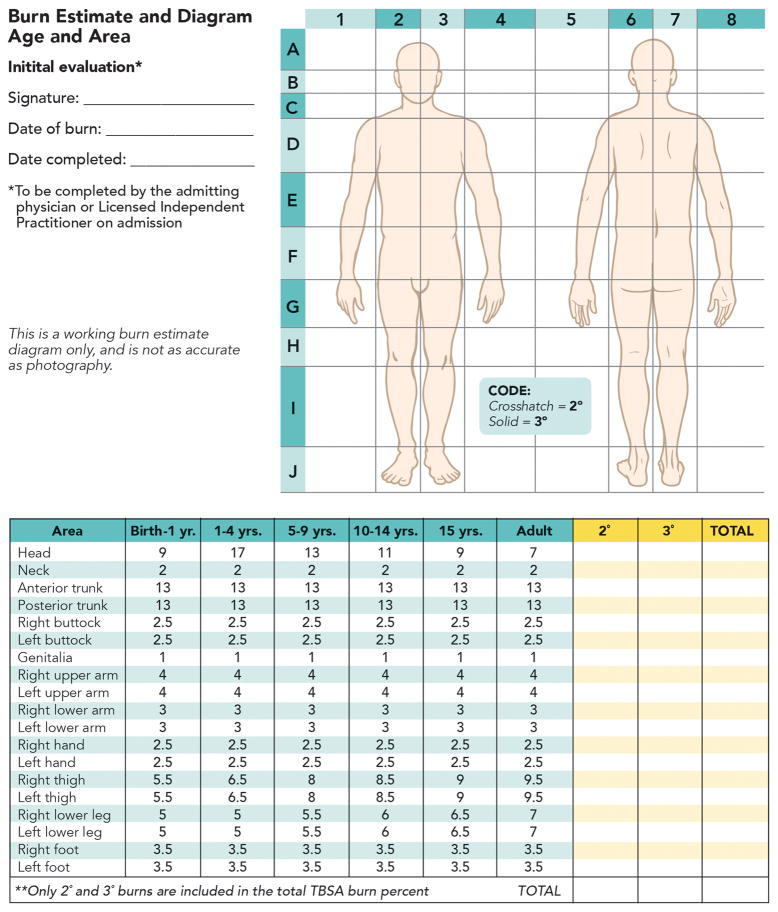
The magnitude of burns is classified according to TBSA involved, depth of the burn, and the presence or absence of inhalational injury. TBSA burned in adults can be estimated using the “rule of nines”. The Lund-Browder chart is an age-specific diagram that more precisely accounts for the changing body surface area relationships with age (fig. 4). The depth of skin destruction is characterized as first-, second-, or third-degree, based on whether there is superficial, partial-thickness, or full-thickness destruction of the skin (table 1). Fourth degree is used to describe burns that have injured deeper structures such as muscle, fascia, and bone. Deep second- and third-degree burns require surgical debridement and grafting, whereas more superficial burns do not.
FIGURE 4. Lund-Browder burn diagram and table.
Lund-Browder burn diagram and table indicate the varying proportions in surface area in persons with different ages. A careful burn diagram should be completed at the time of initial evaluation including wound size, location, and estimated burn depth. Lund-Browder chart should be used in pediatric patients because the body surface area relationships vary with age. LIP = licensed independent practitioner; TBSA = total burn surface area.
Table 1.
Classification of Burn Depth
| Depth | Level of Injury | Clinical Features | Result/Treatment |
|---|---|---|---|
| Superficial (1st degree) | Epidermis | Dry, red; blanches; painful | Healing time 3–6 days, no scarring |
| Superficial partial thickness (Superficial 2nd degree) | Papillary dermis | Blisters; moist, red, weeping; blanches; severe pain to touch | Cleaning; topical agent; sterile dressing; healing time 7–21 days; hypertrophic scar rare; return of full function |
| Deep partial thickness (Deep 2nd degree) | Reticular dermis Most skin appendages destroyed | Blisters; wet or waxy dry; reduced blanching: decreased pain sensation to touch, pain present to deep pressure | Cleaning; topical agent; sterile dressing; possible surgical excision and grafting; scarring common if not surgically excised and grafted; earlier return of function with surgery |
| Full thickness (3rd degree) | Epidermis and dermis; all skin appendages destroyed | Waxy white to leathery dry and inelastic; does not blanch; absent pain sensation; pain present to deep pressure: pain present in surrounding areas of second degree burn | Treatment as for deep partial- thickness burns plus surgical excision and grafting at earliest possible time; scarring and functional limitation more common if not grafted |
| Fourth degree | Involves fascia and muscle and/or bone | Pain to deep pressure, in the area of burn; Increased pain in surrounding areas of second degree burn | Healing requires surgical intervention |
FLUID RESUSCITATION
Rapid and effective intravascular volume replenishment is pivotal for mitigation of burn shock. Delayed or inadequate fluid replacement results in hypovolemia, tissue hypoperfusion, shock and multiple organ failure.25 Inadequate fluid resuscitation can also exacerbate the effects of smoke inhalation injury.26,27 Multiple fluid resuscitation formulae exist for estimating fluid needs. As a general rule, burns of <15% TBSA can be managed with oral or intravenous fluid administered at 1.5 times maintenance rate and careful attention to hydration status. Fluid resuscitation formulae have recently been reviewed by Alvarado et al.28
The Parkland formula is the most common guide used in the United States and recommends isotonic crystalloid initially and use of colloids 24 h after injury (table 2).27 Controversy remains as to ideal time for initiation of colloid therapy in burn resuscitation. There is a general trend now to initiate colloid infusions earlier than the previously recommended time of 24 h. Lactated Ringer solution is often the crystalloid chosen in view of the metabolic acidosis associated with normal (0.9%) saline. In younger children and in patients where hypoglycemia is a potential concern, 5% dextrose solution can be added to the lactated Ringer solution. Side effects of large-volume crystalloid resuscitation include exacerbation of generalized edema, pleural and pericardial effusions and intestinal ileus with abdominal or limb compartment syndrome.28
Table 2.
Formulae for Fluid Resuscitation Following Burn Injury
| Parkland | Lactated Ringer | 4 ml/kg/%TBSA Burn |
| Brooke | Lactated Ringer | 1.5 ml/kg/%TBSA Burn |
| Colloid | 0.5 ml/kg/%TBSA Burn |
LR = lactated ringers; TBSA = total body surface area.
For either formula, half of total volume is administered over the first 8 h. Infusion rates should always be adjusted up or down based on physiological responses.
No matter which formula is used, it should serve only as a guideline and fluid resuscitation is titrated to physiologic end points (table 3). Catheterization of the bladder is important in patients with moderate to severe burns who require intravenous fluid resuscitation. A urinary catheter provides a means of following urine output, to titrate fluid administration and provide samples for urinalysis. Although the best end points of resuscitation following major burn injury have not been conclusively determined, the current recommendation is that urinary output be maintained between 0.5–1 mL/kg/h.29 Actual fluid requirements can vary, depending on size and depth of the burn, interval from injury to start of resuscitation, presence of associated injuries, and presence of inhalational injury. Liberal use of opioids may also increase fluid needs.30 Indicators and criteria used for assessment of adequate fluid volume is specified in table 3.
Table 3.
Indicators of Adequate Circulating Volume and/or Resuscitation
| Urine output | 0.5 – 1.0 ml/kg/hr |
| Blood pressure* | Within normal range for age |
| Heart rate** | Variable |
| Central venous pressure§ | 3 – 8 mm Hg |
| Fractional excretion of Na+ (FeNa)$ | <1% (indicates hypovolemia) |
| BUN/Cr ratio¶ | ≥ 20 (indicates hypovolemia) |
| Echocardiogram/Ultrasound | Normal Stroke volume and ejection fraction |
| Base deficit | <5 (suggests hypoperfusion in the absence of carbon monoxide or cyanide poisoning) |
Blood pressure can be normal even with hypovolemia because of vasoconstriction produced by catecholamines and antidiuretic hormone (vasopressin)
Heart rate can be high despite normovolemia because of catecholamines, anxiety and/or pain, and hypermetabolic state.
Central venous pressures can be artificially altered by airway pressures, pleural or pericardial fluid or abdominal distension.
Blood urea nitrogen (BUN) to creatinine (Cr) ratio
A small percentage of patients fail to respond to conventional fluid resuscitation. Some burn centers administer colloid fluids to patients who, approximately 8 h after injury, are responding inadequately to crystalloid resuscitation.31 Many burn centers including ours administer colloids earlier than 8 h after injury, particularly in children. Consistently, in a recent survey, about 50% of the respondents indicated that they add colloids within the first 24 h.32 A very small percent of patients may require inotropic support during the early resuscitation phase even in the absence of sepsis. No systemic study has evaluated the utility and morbidity associated with the use of inotropes in patients with acute burn injury. After 36–48 h, capillary integrity returns to normal in nonburned areas and reabsorption of edema fluid occurs over the next 1–2 weeks.
ELECTRICAL INJURY
Burns due to electric shock exhibit unique pathology. Soft tissue damage due to electrical burns can dramatically increase fluid needs. Survivors of severe electrical shock frequently experience some form of subsequent arrhythmia (10% to 46%).33,34 Patients without electrocardiographic changes on presentation are unlikely to experience life-threatening arrhythmias.33,35 Damage to the myocardium may occur after exposure to either high- or low-voltage current. The myocardial injury behaves more like a cardiac contusion than a myocardial infarction, with minimal hemodynamic consequences.
Bone experiences the highest heat accumulation during high voltage current flow because it has the highest resistance to flow of electricity. The high heat produced by bone injures muscles surrounding the bone to a greater extent, with more superficial areas of muscle being spared. Subcutaneous tissue and skin also have less damage because they are better conductors than bone. Electrothermal injury of the musculature may manifest as edema formation and tissue necrosis and may lead to compartment syndrome and rhabdomyolysis. For treatment of these complications, patients may come to the operating room within 24 h of injury. Myoglobinuria as a result of muscle damage poses a risk for acute renal failure and requires prompt treatment with crystalloid loading to a target urine output of 2 mL/kg/h. Additional treatment with sodium bicarbonate, mannitol and furosemide facilitate myoglobin excretion and protect against renal tubular injury.
ANESTHETIC MANAGEMENT
PREOPERATIVE EVALUATION
Patients are often brought to the operating room in the early phase of burn injury, when they are undergoing significant fluid shifts with corresponding cardiovascular instability and/or respiratory insufficiency. Early excision of dead/necrotic tissue with temporary or permanent coverage of the open areas decreases the chance of wound colonization and systemic sepsis and has become the standard of care. Along with the standard preoperative evaluation, there are specific features of the history and physical exam which deserve additional focus in the burned patient (table 4). These include the time and extent of burn injury, airway evaluation, presence of inhalation injury, current resuscitation regimen and patient’s response, potential vascular access sites and tolerance to enteral feeding and/or gastric residues (table 4). Communication with the surgeons and critical care team is crucial in order to manage perioperative care in a manner that is compatible with treatment goals of the Intensive Care Unit (ICU). Details of the surgical plan are also essential to estimate blood loss in order to plan appropriate vascular access, invasive monitors, and to order appropriate blood products.
Table 4.
Major Preoperative Concerns for Burn Patients
| Age of patient | Elapsed time from injury |
| Extent of burn injury (total body surface area, depth, and location) | Associated injuries |
| Mechanism of injury | Presence of infection |
| Inhalational injury and/or lung dysfunction | Coexisting diseases |
| Airway patency | Immunedysfunction |
| Hematologic issues | Altered drug responses |
| Adequacy of resuscitation | Magnitude of surgical plan |
| Presence of organ dysfunction | Difficult vascular access |
| Gastric stasis | Altered mental states |
INTRAOPERATIVE MANAGEMENT
Airway Management
Key features of airway assessment include preexisting airway abnormality, current airway injury (i.e., inhalation injury, facial edema), and signs of glottic obstruction. Assessment of mandibular mobility may reveal tightness that will make laryngoscopy challenging. Mouth opening can be limited because of edema or developing contractures (fig. 5). Dressings and nasogastric tubes may make face mask seal difficult. Facial wounds may be painful, and exudate and topical antibiotics may make for a slippery surface and difficulty holding the mask. If the preoperative examination reveals concern for upper airway patency, mobility, or mask ventilation, fiberoptic intubation while maintaining spontaneous ventilation should be considered. In children awake intubation is not a viable option. Ketamine-induced sedation/anesthesia maintains the pharyngeal muscle tone with good conditions for fiberoptic intubation. Gastric emptying may or may not be delayed in burn patients.36 Laryngeal mask airways, with the usual precautions, have been used successfully in burn patients.37 Infection/sepsis, intestinal edema, and opioids may slow gastric emptying, with increased risk of aspiration. The utility of methylnaltrexone, to improve laxation in burned patients on high dose opiate equivalents has been confirmed in a retrospective study.38 Methylnaltrexone antagonizes peripheral but not central opiate effects as it does not cross the blood brain barrier. No prospective studies have examined the utility of methylnaltrexone in the burn injured population.
FIGURE 5. Severe scar contracture developing before complete wound coverage.

In contrast to edema affecting airways in the early phase, burn scar contraction of mouth and neck can complicate airway management during acute recovery phase. Reduced mandibular mobility and contraction around oral commissures can make it difficult or impossible to advance the jaw and open mouth. Furthermore, the airway can become obstructed by collapse of pharyngeal tissues during induction of general anesthesia. In these instances direct laryngoscopy can be difficult or impossible because the larynx also can be tethered to surrounding structures. Awake fiber optic intubation is an option. Ketamine provides analgesia and maintains respiratory drive and pharyngeal tone for pediatric patients and adults who will not tolerate awake intubation.
Securing the endotracheal tube (ETT) is difficult with facial burns. Tape or ties crossing burned areas can irritate the wound or cause graft injury. It is essential to secure the ETT with a carefully secured tie harness to avoid unintentional extubation. Placement of a circumferential tie around the patient’s head, using wire to secure the tube to a tooth, or use of arch bars can provide safe fixation.39,40 Use of cuffed ETT’s in the pediatric population, both in the operating room and in the ICU, is safe and recommended regardless of the child’s age.41–43 Severely burned patients may require tracheostomies because of potential complications from long-term translaryngeal ETT placement for mechanical ventilation and placement of nasogastric feeding tubes (see video, Supplemental Digital Content 4). The proper timing and indications for tracheostomy in burns remain controversial. Tracheostomy-induced dysphagia, dyphonia and other laryngeal pathologies have been described.44 Whether these pathologies were present before the tracheostomy could not be identified.
Vascular Access
Managing vascular access in burn patients is difficult because of technical challenges (edema) and because of the increased risks for bloodstream infection. It may be necessary to place vascular catheters through burn wounds. On occasion, an alternative is to have the surgeons debride the insertion site just before placement of the vascular catheter. In addition to subclavian and internal jugular veins, the femoral veins can be used. If no intravenous access is available, temporary intraosseous cannulation may safely be placed in patients of any age. Localization of vessels using ultrasonographic guidance can be useful in placing peripheral and central catheters in patients when access is difficult.45
Ventilatory Management
In providing perioperative mechanical ventilation, the same considerations used in the ICU must be followed to avoid ventilation-induced morbidity. The findings of the Acute Respiratory Distress Syndrome Network trial have changed ventilatory strategies and have become the standard of care for burn patients with acute lung injury.46 The empiric use of tidal volumes of ≤6 ml/kg ideal body weight and plateau airway pressures below 30 cm H2O in adults are recommended. Although this concept has not been tested in burned patients, a recent report confirms the importance of maintaining low tidal volume ventilation even in the operating room.47 Because of the hypermetabolic state and increased carbon dioxide production, ventilation rates need to be higher than normal. Some patients will require postoperative mechanical ventilation. Assessment of not only pulmonary status but also of the upper airway and glottis is imperative prior to a trial of extubation. The presence of a good air leak after deflation of the endotracheal cuff is an indirect estimate of an adequate glottic opening. In the operating room visualization of the laryngeal structures is often performed by direct laryngoscopy or with flexible fiberoptic bronchoscopy prior to extubation (see video, Supplemental Digital Content 4).
Monitoring
Burn injured areas may involve sites where monitoring equipments have to be placed. Surgical staples can be used to fix adhesive electrocardiogram electrodes. Alternatively, placing the electrodes on the back or dependent sites may hold them in place. Sites for placement of pulse oximetry, if the finger or toe is unavailable, include the ear, nose, or tongue. Reflectance oximetry has been suggested as an alternative if skin sites for monitoring are limited.48 There may be periods when it is not possible to maintain an effective pulse oximeter monitor. When a blood pressure cuff must be placed over grafted wounds great care should be taken to protect the underlying area and the cuff should be sterile. With expected extensive bleeding, an arterial line should be considered for continuous measurement of blood pressure and blood sampling. Respiratory variation in arterial waveforms can be used as a guide to volume and vasoactive therapy. Blood urea nitrogen to creatinine ratio (≥ 20) or fractional sodium (Na+) excretion percent (< 1%) would also indicate hypovolemia.
Temperature monitoring is imperative as burned patients are quite prone to and intolerant to hypothermia. Monitoring of body temperature is also useful for detection of blood transfusion reactions intraoperatively (>2°C rise in temperature). Neuromuscular function monitoring is useful in patients receiving neuromuscular blocking drugs as dose requirements can be significantly altered in burn patients. Multiport central venous catheters are useful for simultaneous monitoring central pressures, and administering of drugs and fluids.
Intrahospital Patient Transport
Intrahospital transport of critically ill patients is associated with an overall adverse event rate of up to 70%.49 Patients requiring mechanical ventilation during transport require at least two anesthesia personnel or an anesthesia personnel and respiratory therapist or nurse to manage ventilation, observe the monitors, and administer medications during transport. A number of professional societies have developed guidelines to improve the safety of transport of critically ill patients by setting rules for pretransport planning and coordination, escort, equipment, and monitoring procedures.50,51 Since patient agitation and extubation during transfer can be disastrous, providing adequate sedation and analgesia and possibly muscle relaxation are essential during intrahospital transport and moving patients to or from the bed to the stretcher or to the operating table.
Pharmacologic Considerations
Large burns result in altered pharmacokinetic and pharmacodynamic responses to many drugs. Plasma protein loss through injured skin and further dilution of plasma proteins by resuscitation fluids decrease the concentration of albumin, an important drug binding protein (Vide infra). There is an increase in volume of distribution of almost every drug studied (propofol, fentanyl, muscle relaxants).52 In addition, pharmacodynamic changes at target organs alter drug-receptor interactions causing variable and at times unpredictable changes in responses to drugs. Consequently changes in the usual dosages of drugs or complete exclusion of other drugs (e.g., succinylcholine) may be necessary to ensure efficacy or avoid toxicity.
During the acute injury phase (0–48 h) and despite adequate volume resuscitation, cardiac output along with renal and hepatic blood flow is decreased (fig. 1). These changes may decrease elimination of some drugs by the kidney and liver. Following the resuscitation phase, the hyperdynamic phase begins, with increased cardiac output and blood flow to the kidneys and liver (fig. 2). Drugs dependent on organ blood flow for elimination will have increased clearances; doses for these drugs may have to be adjusted upwards.
The two major drug-binding proteins, albumin and α1-acid glycoprotein (AAG), are altered in opposite ways following burn injury. The concentration of albumin which binds to mostly acidic and neutral drugs is decreased in burn injury.53 AAG binds cationic drugs such as lidocaine, propranolol, muscle relaxants, and some opioids. AAG is also an acute-phase reactant and its concentration increases two fold or greater in burn injured patients which decreases the free fraction of drugs bound by AAG.53
Hepatic clearance of drugs highly extracted by the liver depends primarily on hepatic blood flow and is relatively insensitive to alterations in protein binding. Clearance of these drugs may decrease during the early postburn phase as a result of decreased liver and renal blood flow. Later on clearance of these drugs may increase during the hyperdynamic phase when hepatic blood flow increases (e.g., propofol, fentanyl).54 During the hypermetabolic state, renal blood flow and glomerular filtration rate also increase. Thus renal clearance of some drugs increases.55,56 Hepatic enzyme activity appears to be altered in patients with burns.57 Phase I reactions, which include oxidation, reduction, hydroxylation, and demethylation, are impaired in burn patients (e.g., diazepam). Phase II reactions involve conjugation, glucuronidation, and sulfation and seem to be relatively unaffected (e.g., lorazepam).58
Muscle Relaxants
Muscle relaxant pharmacology is significantly and consistently altered after burn injury.59 In burn patients, exposure to succinylcholine can result in an exaggerated hyperkalemic response, which can induce cardiac arrest. The current recommendation is to avoid succinylcholine administration in patients 48 h after burn injury.60,61 An increase in the number of extrajunctional acetylcholine receptors which release potassium during depolarization with succinylcholine is the cause for increased hyperkalemia. Martyn and Ritchfield have reviewed the topic of succinylcholine-induced hyperkalemia.62 Almost paralleling the hyperkalemia to succinylcholine, there is concomitantly a decreased sensitivity to the neuromuscular effects of nondepolarizing muscle relaxants (NDMRs). Since succinylcholine is contraindicated, treatment of laryngospasm in burned patients can include high dose NDMRs, positive pressure ventilation, or deepening the anesthetic by intravenous (and inhalational routes, if possible). About 3–7 days after burn injury, the dose of NDMRs required to achieve effective paralysis can be substantially elevated. The etiology of the altered response to NDMRs is multifactorial: (a) upregulation of acetylcholine receptors, including upregulation of fetal and α7 (neuronal type) acetylcholine receptors at the muscle membrane, (b) increased binding to AAG and enhanced renal and hepatic elimination of the NDMRs. The pivotal role of de novo expression of α7AChRs at the neuromuscular junction in the resistance to NDMRs has recently been characterized.63
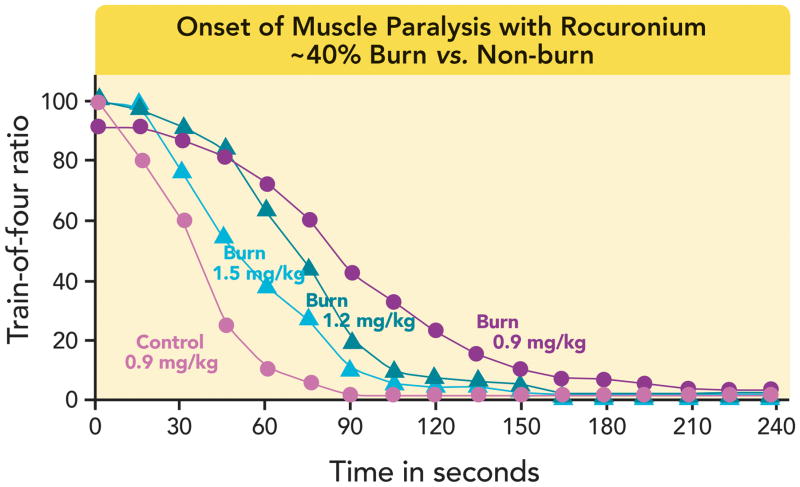
An increased rocuronium dose of 1.2 to 1.5 mg/kg for rapid-sequence induction has been recommended in patients with major burn injury.64 It must be noted, however, that even with a dose of 1.5 mg/kg of rocuronium, the onset time to effective paralysis approximates 90 seconds in burned patients compared with <60 seconds in nonburned patients with a dose 0.9mg/kg (fig. 6).64 Atracurium, broken down by organ-independent pathways (e.g., Hofmann elimination), also exhibits reduced effectiveness following burns. This suggests that the major component to resistance to NDMRs is pharmacodynamic in nature.
FIGURE 6. Dose–response curves and time to maximal effect of rocuronium in adult burned and non-burned patients.
Dose versus time to percent twitch suppression for rocuronium in control subjects and burned subjects of mean 40% total body surface area (TBSA) burn and studied at least one week after burn. In normal patients dose of 0.9 mg/kg rocuronium caused 95% twitch suppression in ≤60 s. The same dose has an onset of >120 s following major burn. Increasing doses of rocuronium shifted dose-response curves to the left. However, even with 1.5 mg/kg dose, the onset was still >90 s. TOF Ratio refers to train-of-four ratio recorded in muscle during 2Hz nerve stimulation.64, 104
Anesthetic Drugs
Choice of drug should be based on the patient’s hemodynamic and pulmonary status and potential difficulty in securing the patient’s airway. The choice of volatile anesthetic does not appear to influence outcome in burned patients.
Propofol clearance and volume of distribution are increased in patients with major burns during the hyperdynamic phase of burn injury.65 The pharmacokinetic changes, in combination with pharmacodynamic alterations centrally, could contribute to a decreased hypnotic effect of propofol. Therefore, in comparison with nonburned patients, those with major burn injuries may require larger bolus doses and/or increased infusion rates of propofol to attain or maintain therapeutic plasma drug concentrations.65 The hemodynamic consequences of administering larger doses of propofol should be kept in mind.
Opioids
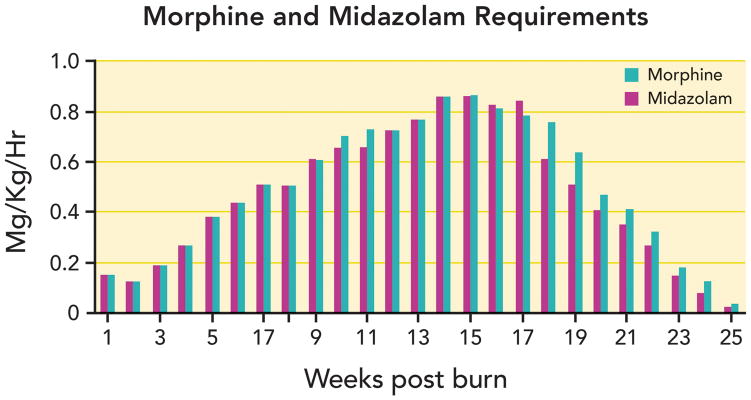
Opioid requirements are increased in burn-injured patients. Opioid tolerance makes pain management challenging throughout all phases of burn care. It is not uncommon for burn-injured patients to manifest opioid tolerance requiring dosing that far exceeds standard textbook recommendations (fig. 7). If patients come to the operating room with infusions of sedatives and narcotics, these infusions should be continued and not stopped; the infusions have been maintained to reach a steady state of effect. Intraoperative analgesia can be achieved by increasing these infusions or turning to other drugs. Table 5 indicates some of the first, second and third line sedative and analgesic regimens used in our institutions during the acute hypermetabolic phase of burn injury. In addition to pharmacokinetic changes documented for morphine, fentanyl and propofol, animal studies of burn injury document changes in the spinal cord receptors. These include down regulation of μ opioid receptors, and upregulation of PKC-γ and N-methyl-D-aspartate (NMDA) receptors.66 In view of the NMDA up regulation following burns, it is not surprising that ketamine requirements to anesthetize patients are increased following burn injury.67 Clonidine, dexmedetomidine, ketamine and methadone have been found to be effective in the treatment of pain for burn injured patients who develop extreme tolerance to morphine (table 5).68,69
FIGURE 7. Burn injury-induced tolerance to narcotics and sedatives.
A 17-yr-old male sustained 90% flame burn injury requiring mechanical ventilation, multiple surgeries and anesthetics. The graph indicates the mg/kg/hr doses of morphine and midazolam administered over time after burn starting from week 1 to week 25. At one stage the intravenous morphine and midazolam doses required exceeded 55mg/hr of each. During procedures (e.g., dressing changes) additional doses of ketamine, dexmedetomidine, fentanyl, and/or propofol were administered pro re nata (PRN). Morerecently, when the doses of morphine and midazolam exceeds 0.5mg/kg/hr, we institute dexmedetomidine or ketamine infusions as sedative and change the opioid from morphine to fentanyl or vice versa (See also table 5)
Table 5.
Sedation and Analgesia Guidelines for Acute Burns
| Stage of Injury | Background Anxiety | Background Pain | Procedural Anxiety | Procedural Pain |
|---|---|---|---|---|
| Acute Burn Ventilated | #1 Midazolam infusion | Morphine infusion | Midazolam boluses | Morphine boluses |
| #2 Dexmedetomidine infusion | Morphine infusion | Dexmedetomidine higher infusion rate | Morphine boluses | |
| #3 Antipsychotics | Morphine infusion | Haloperidol (very slow) boluses | Morphine boluses | |
| #4 Propofol infusion (<48 h) | Morphine infusion | Propofol boluses | Morphine boluses | |
| Acute Burn not ventilated | Dexmedetomidine IV Scheduled Lorazepam IV or PO | Morphine IV or PO | Lorazepam IV/PO | Morphine IV/PO or Ketamine IV |
| Chronic Acute Burn | Scheduled lorazepam or antipsychotics (PO) | Scheduled morphine or methadone | Lorazepam or antipsychotics (PO) | Morphine PO or Oxycodone |
Fentanyl infusions could be substituted for morphine infusions.
In view of the increased incidence of delirium with benzodiazepines, minimal use of them is advocated.
IV = intravenous. PO = per oram (by mouth).
Ketamine
Ketamine has many potential advantages for induction and maintenance of anesthesia in burn patients and is used by some centers as the primary anesthetic. Ketamine in normal patients is associated with hemodynamic stability, preserving airway patency as well as hypoxic and hypercapnic responses, and decreasing airway resistance. Ketamine may exert beneficial anti-inflammatory effects in patients with burns and or sepsis.70–72 Ketamine may be the agent of choice if one wishes to avoid manipulation of the airway (e.g., after placement of fresh facial grafts, for splint or dressing removal, for brief procedures such as dressing or line changes, insertion of Foley catheters in pediatric patients or for patients with toxic epidermal necrolysis syndrome).73 The addition of benzodiazepines is often recommended to reduce the incidence of dysphoria. Because of the increased secretions associated with ketamine, glycopyrrolate is frequently coadministered. Ketamine is now part of the pharmacologic armamentarium to treat burn- and opioid-induced tolerance to narcotics. Bolus doses of ketamine can cause hypotension in patients with burn injury despite ketamine-induced catecholamine release. The persistently high levels of catecholamines in patients with major burns result in desensitization and down regulation of β-adrenoreceptors.74 As a result, direct myocardial depressant effects of ketamine can be manifested.
Regional Anesthesia
Some studies have shown potential benefit of regional anesthesia in patients with burn injury by providing intraoperative anesthesia, improving postoperative analgesia, and facilitating rehabilitation. Patients often have more intense postoperative pain from the split-thickness skin donor site than from the grafted burn wound. Regional anesthesia in its simplest form may be tumescent local anesthesia injected into a donor site prior to harvesting75 or it can take the form of subcutaneous catheter infusions,76 peripheral nerve, or central neuraxial blocks.77
Central neuraxial techniques (spinals, epidurals) have been utilized with good effect as both primary anesthetics and postoperative adjuncts in burn injured patients. There are no reports suggesting epidural abscesses are more common in burn patients, but reports have suggested that intravascular catheters are more likely to become infected if placed in or near burned tissue;78 similarly caution is likely reasonable in selecting appropriate burn patients for central neuraxial techniques.
Truncal blocks (paravertebral and transversus abdominis plane) have been very useful to provide analgesia for donor site harvesting and both block techniques are also amenable to placement of catheters to extend duration of postoperative analgesia. The lateral femoral cutaneous nerve block is particularly well suited to block because it is exclusively a sensory nerve, and innervates an area (the lateral thigh) that is frequently chosen for split-thickness skin grafts. Sometimes there is a need to cover the anterior and medial thigh due to the extent of skin harvest, and therefore a fascia iliaca block can also be performed.76–78
Metabolic and Nutritional Management
The hypermetabolic response following burn injury is more severe and sustained than any other form of trauma.3,4 Continuous enteral or parenteral nutrition partially abates the hypermetabolic response and attenuates muscle protein loss of burns.79 Despite aggressive nutrition, intensive insulin therapy and use of adjuvants (oxandrolone, propranolol, etc.), loss of muscle mass continues even after wound coverage.79 Burn injured patients undergo multiple surgical procedures. Periods of eight hour fasting prior to surgery make it difficult to meet the high caloric requirements of patients with major burn injury and may be poorly tolerated. The feasibility and safety of continuing enteral feeding throughout operative procedures has been studied. Enteral feeding during surgery beyond the pylorus has been successful, provided the airway was secured via a cuffed endotracheal tube or tracheostomy (to prevent aspiration of gastric contents).79 Nonetheless it is prudent to hold enteral feedings when there is potential for increasing abdominal pressure (e.g., prone position during surgery) or when an airway procedure such as tracheostomy is to be performed.
Blood Loss During Burn Wound Excision
It is difficult to estimate blood loss during burn excision because shed blood cannot be efficiently collected in a suction canister, surgical sponges may also contain irrigation fluid, blood can be concealed beneath the patient and substantial bleeding can continue unobserved beneath bulky dressings. Vigilant attention to several physiological variables is necessary to effectively maintain intravascular volume during burn excision. Published estimates of the amount of blood loss during burn excision operations are in the range of 2.6–3.4% of the blood volume for every 1% TBSA excised.80,81 Multiple techniques have been used to minimize intraoperative bleeding, such as application of topical thrombin, staged procedures, and brisk operative pace and topical application or subcutaneous injection of vasoconstrictors (epinephrine, vasopressin analogues, or phenylephrine).82,83 No prospective study has compared the efficiency or superiority of one drug over the other to decrease bleeding.
Intraoperative fluid administration and blood transfusion
If the patient is receiving parenteral nutrition, it is important that its infusion not be stopped because of the danger of hypoglycemia. After the initial massive fluid resuscitation for major burns, much effort is made restricting fluids and administering diuretics to hasten elimination of this edema. In the perioperative period it is important to avoid giving more fluid than is necessary. The use of colloids can help limit the amount of fluid needed to maintain preload. The surgeons may inject large amounts of subcutaneous fluid to facilitate wound debridement and donor harvest. This fluid should also be limited. As with the initial resuscitation there is no single physiological endpoint to rely on for titrating fluid replacement. Constant vigilance and attention to all available information (hemodynamic, metabolic, and urine output) is necessary. The point at which red cell transfusion is beneficial varies greatly between patients. Rather than focusing on hemoglobin or hematocrit it is best to strive to maintain adequate preload and follow metabolic status. Blood component therapy should be reserved for patients with a demonstrated physiologic need but anticipation of continued blood loss may indicate transfusion to prevent significant anemia rather than waiting to treat it when it occurs.
In the past, administration of fresh frozen plasma (FFP) was guided by American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies recommendations that FFP only be given when microvascular bleeding is present and coagulation factor deficiency is demonstrated. Recent experience with civilian and military trauma has demonstrated that mortality is decreased by earlier and more aggressive administration of FFP with massive bleeding.84,85 There are a number of definitions of massive transfusion such as loss of total blood volume in 24 h, requirement of 4 units of packed erythrocytes in an hour, or ongoing loss of more than 150 ml of blood per minute. It is not unusual for patients with large burns to meet these criteria during burn wound excision. The clinical experience with burn patients with massive hemorrhage is not the equivalent of hemorrhagic shock in nonburned trauma patients who present with hypovolemic shock, acidemia, hypothermia and coagulopathy. During burn wound excision, bleeding is simultaneously treated with fluid replacement and measures are taken to support the circulation and prevent hypothermia. Still, it is logical to assume that more aggressive use of FFP to prevent development of coagulopathy can also benefit burn patients who experience massive hemorrhage.
Temperature Management
Maintaining body temperature in burned patients this is especially important and challenging. The inflammatory response to large burns causes an elevation of the hypothalamic core temperature set point. The metabolic rate is increased to maintain this elevated temperature. Hypothermia in these patients is poorly tolerated as it causes an exaggerated increase in oxygen consumption and exacerbates the catabolic response to the injuries.86 Decreased body temperature during burn excisions may also increase blood loss and worsen morbidity and mortality.87 Multiple strategies are used to maintain body temperature in the operating room, including use of warming blankets, radiant warmers, blood/fluid warmers, minimizing skin surface exposure, and wrapping the head and extremities with plastic or thermal insulation. Temperature in the operating room is commonly maintained at 80–100°F (27 – 38°C), depending on the age and severity of the burn.
POSTOPERATIVE CARE
There are several critical postoperative concerns for burn patients: whether to extubate in the operating room, safe transport to the ICU, transfer of care to the ICU staff, and control of postoperative pain. The decision to extubate in the operating room depends on standard criteria with concerns specific to burn patients including an assessment of airway patency, metabolic status, potential for ongoing bleeding and when the patient will return again for surgery.
The same concerns regarding transfer from the ICU to the operating room apply for transfer back to the ICU except that the patient is likely to be less stable physiologically in the postoperative period. Continued bleeding may be concealed by dressings, the patient may be more prone to hypothermia, emergence may be associated with delirium, and analgesic requirements will be greater. Monitors appropriate to the patient’s physiological status, transport oxygen with appropriate respiratory support, a plan to keep the patient warm, adequate transport staff, resuscitation drugs and an easily available intravenous drug administration site are all necessary for safe transport. During this period of exaggerated physiological fragility, it is important to be especially vigilant during transfer of the monitors, respiratory and hemodynamic-support equipment to the ICU staff.
Inadequate control of pain and anxiety can adversely affect wound healing and psychological status. The presence of newly excised tissue and harvested donor sites are very painful. As indicated previously, it is common for burned patients to become quite tolerant of sedatives and analgesics over time and thus doses substantially larger than normal may be required especially in the postoperative period. Other drugs, which act on receptors other than opiates (α2 adrenoceptor agonists, NMDA antagonists, etc.), may have benefits when added to the regimen (Vide infra). The optimal method providing of sedation and analgesia in patients with major burns is still unresolved.
PAIN MANAGEMENT
All aspects of burn injury (e.g., dressing changes, excision and grafting procedures, physical therapy, and line insertion) are associated with pain. There is ongoing background pain and there is procedure related pain. Pain is exacerbated by anxiety if the pain is poorly controlled with sedatives and analgesics. Pain of burns has hyperalgesic (increased response to painful stimuli, e.g., wound debridement) and allodynic components (painful responses to non-painful stimuli, e.g., touch).88 Posttraumatic stress disorder has been reported to occur in up to 30% of patients with severe burn injury, often developing in the setting of inadequate treatment of anxiety and pain.89,90 Patient-controlled analgesia has been shown to be a safe and effective method of opioid delivery for acute or procedure related pain in both children and adults with burn injury.91–93
Sensitivity to analgesics varies with time after burn injury from increased sensitivity and tolerance.94 Continuous administration of analgesics by itself can result in opioid-induced hyperalgesia and accentuate the need for higher opioid doses.95 To provide appropriate, consistent patient comfort, standardized pain and anxiety guidelines are used in many burn centers. The ideal characteristics of such a guideline include (a) safety and efficacy over a broad range of ages and burn injury severities, (b) explicit recommendations for drug selection, dosing, and increases in dosing, (c) a limited formulary to promote staff familiarity with drugs used, and (d) regular assessment of pain and anxiety levels with guidance for intervention through adjusted drug dosing.96,97 Table 5 gives one example of a pain and sedation treatment guideline. Treatment of opioid tolerance includes switching of opioids (morphine-> fentanyl-> methadone) and coadministration of drugs acting on nonopioid receptors (ketamine–NMDA [nonsteroidal antiiflammatory drugs] antagonist, dexmedetomidine– or clonidine-α2-agonist and gabapentin-like drugs).
Acetaminophen and NSAIDS are useful first line analgesic for minor burns. However, oral NSAIDs and acetaminophen exhibit a ceiling effect in their dose-response relationship, rendering them unsuitable for the treatment of severe burn pain.98 NSAIDS can also have deleterious effects on gastric mucosa and renal function. NSAIDs and benzodiazepines are commonly combined with opioids to relieve procedural pain. Pain is exacerbated by anxiety which may be reduced by benzodiazepines. Antidepressants appear to enhance opiate-induced analgesia, especially in patients with chronic (neuropathic) pain. The tolerance to opiates seems to be exaggerated by long-term administration of the benzodiazepine, midazolam.99 Anticonvulsants may be useful following burns but have not been adequately tested. Clonidine, or dexmedetomidine (α2-adenoceptor agonists) can be a useful adjunct in reducing pain without causing pruritus (itching) or respiratory depression. However, it can cause hypotension in higher doses and in the presence of hypovolemia, therefore should not be given to hemodynamically unstable patients.100,101 Dexmedetomidine has been used to provide sedation–analgesia for burned patients and to decrease opioid requirements.101–103
SUMMARY
Burn-injured patients frequently require surgical treatment, yet pose a myriad of pathophysiologic challenges to acute and perioperative care. Optimal care of the burn injured patients requires a comprehensive preoperative assessment and attention to risk factors (e.g., burn shock and resuscitation, difficult airway anatomy, inhalation injury) that predispose these patients to increased morbidity and mortality. Anticipation of these issues, as well as awareness of the alterations in pharmacokinetics and pharmacodynamics in patients with burn injury is essential. Significant losses of blood volume and body temperature are not uncommon sequelae in the intraoperative period. Appropriate precautions should be taken to prevent these. Safe care can be provided by understanding, appreciating, and anticipating the unique preoperative, intraoperative, and postoperative issues and problems of the burn patient.
Supplementary Material
Summary Statement.
Major burn injury affects almost every organ. Understanding the complex and often paradoxical pathophysiological responses in the early and late phases of injury is imperative to provide expert care in the acute and perioperative period.
Acknowledgments
This work was supported in part by grants from the Shriners Hospital Research Philanthropy Tampa Florida, and from the National Institutes of Health Bethesda, Maryland, P50-GM 2500 Project I (to JAJM).
Footnotes
American Burn Association: Burn incidence and treatment in the US: 2007 fact sheet. Available at: http://www.ameriburn.org/resources_factsheet.php. Last accessed May 16, 2014.
The authors declare no competing interests
References
- 1.Cuthbertson DP. Postshock metabolic response. Lancet. 1942;239:433–7. [Google Scholar]
- 2.Martyn JA, Aikawa N, Wilson RS, Szyfelbein SK, Burke JF. Extrapulmonary factors influencing the ration of arterial oxygen tension to inspired oxygen concentration in burn patients. Crit Care Med. 1979;7:492–6. doi: 10.1097/00003246-197911000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Wilmore DW, Goodwin CW, Aulick LH, Powanda MC, Mason AD, Jr, Pruitt BA. Effect of injury and infection on visceral metabolism and circulation. Ann Surg. 1980;192:491–504. doi: 10.1097/00000658-198010000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aulick LH, McManus AT, Mason AD, Jr, Pruitt BA., Jr Effects of infection on oxygen consumption and core temperature in experimental thermal injury. Ann Surg. 1986;204:48–52. doi: 10.1097/00000658-198607000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rehberg S, Maybauer MO, Enkhbaatar P, Maybauer DM, Yamamoto Y, Traber DL. Pathophysiology, management and treatment of smoke inhalation injury. Expert Rev Respir Med. 2009;3:283–97. doi: 10.1586/ERS.09.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackie DP, Spoelder EJ, Paauw RJ, Knape P, Boer C. Mechanical ventilation and fluid retention in burn patients. J Trauma. 2009;67:1233–8. doi: 10.1097/TA.0b013e3181be9c67. [DOI] [PubMed] [Google Scholar]
- 7.McCall J, Cahill T. Respiratory care of the burn patient. J Burn Care Rehab. 2005;26:200–6. [PubMed] [Google Scholar]
- 8.Lykens MG, Haponik EF. Direct and indirect lung injuries in patients with burns. Crit Care Rep. 1990;2:101–14. [Google Scholar]
- 9.Zak AL, Harrington DT, Barillo DJ, Lawlor DF, Shirani KZ, Goodwin CW. Acute respiratory failure that complicated the resuscitation of pediatric patients with scald injuries. J Burn Care Rehabil. 1999;20:391–9. doi: 10.1097/00004630-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Rodkey FL, O’Neal JD, Collison HA, Uddin DE. Relative affinity of hemoglobin S and hemoglobin A for carbon monoxide and oxygen. Clin Chem. 1974;20:83–4. [PubMed] [Google Scholar]
- 11.Buckley NA, Juurlink DN, Isbister G, Bennett MH, Lavonas EJ. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011;4:CD002041. doi: 10.1002/14651858.CD002041.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiss SM, Lakshminarayan S. Acute inhalation injury. Clin Chest Med. 1994;15:103–16. [PubMed] [Google Scholar]
- 13.Ellenhorn MJ, Schonwald S, Ordog G, Wasserberger J, editors. Diagnosis and Treatment of Human Poisoning. 2. Baltimore: Williams & Wilkins; 1997. Ellenhorn’s Medical Toxicology. [Google Scholar]
- 14.Baud FJ, Barriot P, Toffis V, Riou B, Vicaut E, Lecarpentier Y, Bourdon R, Astier A, Bismuth C. Elevated blood cyanide concentrations in victims of smoke inhalation. N Engl J Med. 1991;325:1761–6. doi: 10.1056/NEJM199112193252502. [DOI] [PubMed] [Google Scholar]
- 15.Toon MH, Maybauer MO, Greenwood JE, Maybauer DM, Fraser JF. Management of acute smoke inhalation injury. Crit Care Resusc. 2010;12:53–61. [PubMed] [Google Scholar]
- 16.Yeung JK, Leung LT, Papp A. A survey of current practices in the diagnosis of and interventions for inhalational injuries in Canadian burn centres. Can J Plast Surg. 2013;21:221–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Miller AC, Elamin EM, Suffredini AF. Inhaled anticoagulation regimens for the treatment of smoke inhalation-associated acute lung injury: A systematic review*. Crit Care Med. 2014;42:413–9. doi: 10.1097/CCM.0b013e3182a645e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 19.Klein MB, Goverman J, Hayden DL, Fagan SP, McDonald-Smith GP, Alexander AK, Gamelli RL, Gibran NS, Finnerty CC, Jeschke MG, Arnoldo B, Wispelwey B, Mindrinos MN, Xiao W, Honari SE, Mason PH, Schoenfeld DA, Herndon DN, Tompkins RG. Inflammation and host response to injury, and large-scale collaborative research program. Benchmarking outcomes in the critically injured burn patient. Ann Surg. 2014;259:833–41. doi: 10.1097/SLA.0000000000000438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenkranz K, Sheridan R. Management of the burned trauma patient: Balancing conflicting priorities. Burns. 2002;28:665–9. doi: 10.1016/s0305-4179(02)00109-2. [DOI] [PubMed] [Google Scholar]
- 21.Valdez TA, Desai U, Ruhl CM, Nigri PT. Early laryngeal inhalation injury and its correlation with late sequelae. Laryngoscope. 2006;116:283–7. doi: 10.1097/01.mlg.0000197932.09386.0e. [DOI] [PubMed] [Google Scholar]
- 22.Woodson LC. Diagnosis and quantification of inhalation injury. J Burn Care Res. 2009;30:143–5. doi: 10.1097/BCR.0b013e3181923b71. [DOI] [PubMed] [Google Scholar]
- 23.Eastman AL, Arnoldo BA, Hunt JL, Purdue GF. Pre-burn center management of the burned airway: Do we know enough? J Burn Care Res. 2010;31:701–5. doi: 10.1097/BCR.0b013e3181eebe4f. [DOI] [PubMed] [Google Scholar]
- 24.Muehlberger T, Kunar D, Munster A, Couch M. Efficacy of fiberoptic laryngoscopy in the diagnosis of inhalation injuries. Arch Otolaryngol Head Neck Surg 2. 1998;124:1003–7. doi: 10.1001/archotol.124.9.1003. [DOI] [PubMed] [Google Scholar]
- 25.Barrow RE, Jeschke MG, Herndon DN. Early fluid resuscitation improves outcomes in severely burned children. Resuscitation. 2000;45:91–6. doi: 10.1016/s0300-9572(00)00175-1. [DOI] [PubMed] [Google Scholar]
- 26.Herndon DN, Traber DL, Traber LD. The effect of resuscitation on inhalation injury. Surgery. 1986;100:248–51. [PubMed] [Google Scholar]
- 27.Alvarado R, Chung KK, Cancio LC, Wolf SE. Burn resuscitation. Burns. 2009;35:4–14. doi: 10.1016/j.burns.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Klein MB, Hayden D, Elson C, Nathens AB, Gamelli RL, Gibran NS, Herndon DN, Arnoldo B, Silver G, Schoenfeld D, Tompkins RG. The association between fluid administration and outcome following major burn; a multicenter study. Ann Surg. 2007;245:622–8. doi: 10.1097/01.sla.0000252572.50684.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pham TN, Cancio LC, Gibran NS. American Burn Association practice guidelines burn schock resuscitation. J Burn Care Res. 2008;29:257–66. doi: 10.1097/BCR.0b013e31815f3876. [DOI] [PubMed] [Google Scholar]
- 30.Sullivan SR, Friedrich JB, Engrav LH, Round KA, Heimbach DM, Heckbert SR, Carrougher GJ, Lezotte DC, Wiechman SA, Honari S, Klein MB, Gibran NS. “Opioid cree” is real and may be the cuase of “fluid creep”. Burns. 2004;30:583–90. doi: 10.1016/j.burns.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Cochran A, Morris SE, Edelman LSA, Saffle JR. Burn patient characteristics and outcomes following resuscitation with albumin. Burns. 2007;33:25–30. doi: 10.1016/j.burns.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Greenhalgh DG. Burn resuscitation: the results of the ISBI/ABA survey. Burns. 2010;36:176–82. doi: 10.1016/j.burns.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Purdue GF, Hunt JL. Electrocardiographic monitoring after electrical injury: Necessity or luxury. J Trauma. 1986;26:166–7. doi: 10.1097/00005373-198602000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Fatovich DM, Lee KY. Household electric shocks: Who should be monitored? Med J Aust. 1991;155:301–3. doi: 10.5694/j.1326-5377.1991.tb142285.x. [DOI] [PubMed] [Google Scholar]
- 35.Arnoldo B, Klein M, Gibran NS. Practice guidelines for the management of electrical injuries. J Burn Care Res. 2006;27:439–47. doi: 10.1097/01.BCR.0000226250.26567.4C. [DOI] [PubMed] [Google Scholar]
- 36.Hu OY, Ho ST, Wang JJ, Ho W, Wang HJ, Lin CY. Evaluation of gastric emptying in severe, burn-injured patients. Crit Care Med. 1993;21:527–31. doi: 10.1097/00003246-199304000-00012. [DOI] [PubMed] [Google Scholar]
- 37.McCall VE, Fischer CG, Schomaker E, Young VM. Laryngeal mask airway use in children with acute burns: Intraoperative airway management. Paediatr Anaesth. 1999;9:515–20. doi: 10.1046/j.1460-9592.1999.00407.x. [DOI] [PubMed] [Google Scholar]
- 38.Hewitt K, Lin H, Faraklas I, Morris S, Cochran A, Saffle J. Use of methylnaltrexone to induce laxation in acutely injured patients with burns and necrotizing soft-tissue infections. J Burn Care Res. 2014;35:e106–11. doi: 10.1097/BCR.0b013e31829b399d. [DOI] [PubMed] [Google Scholar]
- 39.Perrtta VJ, Stern JD, Lo AK, Mitra A. Arch bar stabilization of endotracheal tubes in children with facial burns. J Burn Care Rehabil. 1995;16:437–9. doi: 10.1097/00004630-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 40.Gordon MD. Burn care protocols: Anchoring endotracheal tubes on patients with facial burns. J Burn Care Rehabil. 1987;8:233–7. doi: 10.1097/00004630-198705000-00013. [DOI] [PubMed] [Google Scholar]
- 41.Khine HH, Corddry DH, Kettrick RG, Martyn TM, McCloskey JJ, Rose JB, Theroux MC, Zagnoev M. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology. 1997;86:627–31. doi: 10.1097/00000542-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 42.Deakers T, Reynolds G. Cuffeed endotracheal tubes in pediatric intensive care. J Pediatr. 1994;125:57–62. doi: 10.1016/s0022-3476(94)70121-0. [DOI] [PubMed] [Google Scholar]
- 43.Sheridan RL. Uncuffed endotracheal tubes should not be used in seriously burned children. Pedatr Crit Care Med. 2006;7:258–9. doi: 10.1097/01.PCC.0000216681.71594.04. [DOI] [PubMed] [Google Scholar]
- 44.Clayton N, Kennedy P, Maitz P. The severe burns patient with tracheostomy: Implications for management of dysphagia, dysphonia an dlaryngotracheal pathology. Burns. 2010;36:850–5. doi: 10.1016/j.burns.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 45.Wait M, Hunt J, Purdue G. Duplex scanning of central vascular access sites in burn patients. Ann Srg. 1990;211:499–503. doi: 10.1097/00000658-199004000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peck MD, Koppelman T. Low-tidal-volume ventilation as a strategy to reduce ventilator-associated injury in ALI and ARDS. J Burn Care Res. 2009;30:172–5. doi: 10.1097/BCR.0b013e3181923c32. [DOI] [PubMed] [Google Scholar]
- 47.Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant JY, Allaouchiche B, Verzilli D, Leone M, De Jong A, Bazin JE, Pereira B, Jaber S IMPROVE Study Group. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;269:428–37. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 48.Sheridan RL, Prelack KM, Petras LM, Szyfelbein SK, Tompkins RG. Intraoperative reflectance oximetry in burn patients. J Clin Monit. 1995;11:32–4. doi: 10.1007/BF01627417. [DOI] [PubMed] [Google Scholar]
- 49.Waydhas C. Intrahospital transport of critically ill patients. Crit Care. 1999;3:R83–9. doi: 10.1186/cc362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fanara B, Manzon C, Barbot O, Desmettre T, Capellier G. Recommendations for the intrahospital transport of critically ill patients. Crit Care. 2010;14:R87. doi: 10.1186/cc9018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Warren J, Fromm RE, Jr, Orr RA, Rotello LC, Horst HM American College of Critical Care Medicine. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–262. doi: 10.1097/01.CCM.0000104917.39204.0A. [DOI] [PubMed] [Google Scholar]
- 52.Blancet B, Jullien V, Vinsonneau C, Tod M. Influence of burns on pharmacokinetics and pharmacodynamics of drugs used in the care of burn patients. Clin Pharmacokinet. 2008;47:635–54. doi: 10.2165/00003088-200847100-00002. [DOI] [PubMed] [Google Scholar]
- 53.Martyn JA, Abernethy DR, Greenblatt DJ. Plasma protein binding of drugs after severe burn injury. Clin Pharmacol Ther. 1984;35:535–9. doi: 10.1038/clpt.1984.73. [DOI] [PubMed] [Google Scholar]
- 54.Han T, Harmatz JS, Greenblatt DJ, Martyn JA. Fentanyl clearance and volume of distribution are increased in patients with major burns. J Clin Pharmacol. 2009;47:674–80. doi: 10.1177/0091270007299756. [DOI] [PubMed] [Google Scholar]
- 55.Martyn JA, Greenblatt DJ, Abernethy DR. Increased cimetidine clearance in burn patients. JAMA. 1985;253:1288–91. [PubMed] [Google Scholar]
- 56.Martyn JA, Bishop AL, Oliveri MF. Pharmacokinetics and pharmacodynamics of ranitidine after burn injury. Clin Pharmacol Ther. 1992;51:408–14. doi: 10.1038/clpt.1992.40. [DOI] [PubMed] [Google Scholar]
- 57.Jaehde U, Sorgel F. Clinical pharmacokinetics in patients with burns. Clin Pharmacokinet. 1995;29:15–28. doi: 10.2165/00003088-199529010-00003. [DOI] [PubMed] [Google Scholar]
- 58.Martyn J, Greenblatt DJ. Lorazepam conjugation is unimpaired in burn trauma. Clin Pharmacol Ther. 1988;43:250–5. doi: 10.1038/clpt.1988.29. [DOI] [PubMed] [Google Scholar]
- 59.Martyn JA, Fukushima Y, Chou J, Yang HS. Muscle relaxants in burns, trauma and critical illness. Int Anesth Clin. 2006;44:123–43. doi: 10.1097/00004311-200604420-00008. [DOI] [PubMed] [Google Scholar]
- 60.Martyn JA. Succinylcholine hyperkalemia after burns (letter) Anesthesiology. 1999;91:321–2. doi: 10.1097/00000542-199907000-00048. [DOI] [PubMed] [Google Scholar]
- 61.MacLennan N, Heimbach DM, Cullen BF. Anesthesia for major thermal injury. Anesthesiology. 1998;89:749–70. doi: 10.1097/00000542-199809000-00027. [DOI] [PubMed] [Google Scholar]
- 62.Martyn JA, Richtsfeld M. Succinylcholine-induced hyperkalemia in acquired pathologic states. Anesthesiology. 2006;104:158–69. doi: 10.1097/00000542-200601000-00022. [DOI] [PubMed] [Google Scholar]
- 63.Lee S, Yang HS, Sasakawa T, Khan MA, Khatri A, Kaneki M, Martyn JA. Immobilization with atrophy induces de novo expression of neuronal nicotinic α7 acetylcholine receptors in muscle contributing to neurotransmission. Anesthesiology. 2014;120:76–85. doi: 10.1097/ALN.0000000000000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Han TH, Martyn JA. Onset and effectiveness of rocuronium for rapid onset of paralysis in patients with major burns: Priming or large bolus. Br J Anaesth. 2009;102:55–60. doi: 10.1093/bja/aen332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Han Th, Greenblatt DJ, Martyn JA. Propofol clearance and volume of distribution are increased in patients with major burns. J Clin Pharmacol. 2009;49:768–72. doi: 10.1177/0091270009335767. [DOI] [PubMed] [Google Scholar]
- 66.Wang S, Zhang L, Ma Y, Chen L, Tian Y, Mao J, Martyn JJ. Nociceptive behavior following hindpaw burn injury in young rats: Response to systemic morphine. Pain Med. 2011;12:87–98. doi: 10.1111/j.1526-4637.2010.01021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sheridan RL, Ryan DP, Fuzaylov G, Nimkin K, Martyn JA. Case records of the Massachusetts General Hospital. Case 2-2008. Case 5-2008. An 18-month-old girl with an advanced neck contracture after a burn. N Engl J Med. 2008;358:729–35. doi: 10.1056/NEJMcpc0708792. [DOI] [PubMed] [Google Scholar]
- 68.Kariya N, Shindoh M, Nishi S, Yukioka H, Asada A. Oral clonidine for sedation and analgesia in a burn patient. J Clin Anesth. 1998;10:514–7. doi: 10.1016/s0952-8180(98)00068-3. [DOI] [PubMed] [Google Scholar]
- 69.Williams PI, Sarginson RE, Ratcliffe JM. Use of methadone in the morphine-tolerant burned paediatric patient. Br J Anaesth. 1998;80:92–5. doi: 10.1093/bja/80.1.92. [DOI] [PubMed] [Google Scholar]
- 70.Hofbauer R, Moser D, Hammerschmidt V, Kapiotis S, Frass M. Ketamine significantly reduces the migration of leukocytes through endotelial cell monolayers. Crit Care Med. 1998;26:1545–9. doi: 10.1097/00003246-199809000-00022. [DOI] [PubMed] [Google Scholar]
- 71.Weigand MA, Schmidt H, Zhao Q, Plaschke K, Martin E, Bardenheuer HJ. Ketamine modulates the stimulated adhesion molecule expression on human neutrophils in vitro. Anesth Analg. 2000;90:206–12. doi: 10.1097/00000539-200001000-00041. [DOI] [PubMed] [Google Scholar]
- 72.Gurfinkel R, Czeiger D, Douvedevani A, Shapira Y, Artru AA, Sufaro Y, Mazar J, Shaked G. Ketamine improves survival in burn injury followed by sepsis in rats. Anesth Analg. 2006;103:396–402. doi: 10.1213/01.ane.0000226140.84281.3e. [DOI] [PubMed] [Google Scholar]
- 73.Maldini B. Ketamine anesthesia in children with acute burns and scalds. Acta Anaesthesiol Scand. 1996;40:1108–11. doi: 10.1111/j.1399-6576.1996.tb05572.x. [DOI] [PubMed] [Google Scholar]
- 74.Wang C, Martyn JA. Burn Injury alters beta-adrenergic receptor and second messenger function in rat ventricular muscle. Crit Care Med. 1996;24:118–24. doi: 10.1097/00003246-199601000-00020. [DOI] [PubMed] [Google Scholar]
- 75.Bussolin L, Busoni P, Giorgi L, Crescioli M, Messeri A. Tumescent local anesthesia for the surgical treatment of burns and postburn sequelae in pediatric patients. Anesthesiology. 2003;99:1371–5. doi: 10.1097/00000542-200312000-00020. [DOI] [PubMed] [Google Scholar]
- 76.Hernandez JL, Savetamal A, Crombie RE, Cholewczynski W, Atweh N, Possenti P, Schulz JT., 3rd Use of continuous local anesthetic infusion in the management of postoperative split-thickness skin graft donor site pain. J Burn Care Res. 2013;34:e257–62. doi: 10.1097/BCR.0b013e3182721735. [DOI] [PubMed] [Google Scholar]
- 77.Shank ES, Martyn JA, Donelan M, Perone A, Firth P, Driscoll D. Ultra-sound guided regional anesthesia for pediatric burn reconstructive surgery; a prespective study. J Burn Care Rehab. doi: 10.1097/BCR.0000000000000174. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cuignet O, Pirson J, Boughrouph J, Duville D. The efficacy of continous fascia iliaca compartment block for pain mangaement in burn patients undergoing skin grafting procedures. Anesh Analg. 2004;98:1077–81. doi: 10.1213/01.ANE.0000105863.04140.AE. [DOI] [PubMed] [Google Scholar]
- 79.Abdullahi A, Jeschke M. Nutrition and anabolic pharmacotherapies in the care of burn patients. Nutr Clin Pract. 2014 doi: 10.1177/0884533614533129. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 80.Budny P, Regan P, Roberts A. The estimation of blood loss during burns surgery. Burns. 1993;19:134–7. doi: 10.1016/0305-4179(93)90036-8. [DOI] [PubMed] [Google Scholar]
- 81.Housinger T, Lang D, Warden G. A prospective study of blood loss with excisional therapy in pediatric burn patients. J Trauma. 1993;34:262–3. doi: 10.1097/00005373-199302000-00015. [DOI] [PubMed] [Google Scholar]
- 82.Mitchel RT, Funk D, Spiwak R, Logsetty S. Phenylephrine tumescence in split-thickness skin graft donor sites in surgery for burn injury – a concentration finding study. J Burn Care Res. 2011;32:129–34. doi: 10.1097/BCR.0b013e318204b39b. [DOI] [PubMed] [Google Scholar]
- 83.Sterling JP, Heimbach DM. Hemostasis in burn surgery – a review. Burns. 2011;37:559–65. doi: 10.1016/j.burns.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 84.Teixeira PG, Inaba K, Shulman I, Salim A, Demetriades D, Brown C, Browder T, Green D, Rhee P. Impact of plasma transfusion in massively transfused trauma patients. J Trauma. 2009;66:693–7. doi: 10.1097/TA.0b013e31817e5c77. [DOI] [PubMed] [Google Scholar]
- 85.Pidcoke HF, Aden JK, Mora AG, Borgman MA, Spinella PC, Dubick MA, Blackbourne LH, Cap AP. Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom: Increased plasma and platelet use correlates with improved survival. J Trauma Acute Care Surg. 2012;73:S445–52. doi: 10.1097/TA.0b013e3182754796. [DOI] [PubMed] [Google Scholar]
- 86.Woodson LC, Sherwood ER, Kinsky M, Morvant Elise, Talon M. Total Burn Care. 4. Edinburgh: Elsivier; 2012. Anesthesia for burned patients; pp. 173–98. [Google Scholar]
- 87.Oda J, Kasai K, Noborio M, Ueyama M, Yukioka T. Hypothermia during burn surgery and postoperative acute lung injury in extensively burned patients. J Trauma. 2009;66:1525–9. doi: 10.1097/TA.0b013e3181a51f35. [DOI] [PubMed] [Google Scholar]
- 88.Ueda M, Iwasaki H, Wang S, Murata E, Poon T, Mao J, Martyn JA. Cannabinoid receptor Type 1 antagonist, AM-251, attenuates mechanical allodynia and thermal hyperalgesia after burn injury. Anesthesiology. 2014;121:XXX–XXX. doi: 10.1097/ALN.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Patterson DR, Carrigan K, Questad KA, Robinson R. Posttraumatic stress disorder in hospitalized patients with burn injuries. J Burn Care Rehabil. 1990;11:181–4. doi: 10.1097/00004630-199005000-00002. [DOI] [PubMed] [Google Scholar]
- 90.Saxe GN, Stoddard F, Hall E, Chawla N, Lopez C, Sheridan R, King D, King L, Yehuda R. Pathways to PTSD, part 1: Children with burns. Am J Psychiatry. 2005;162:1299–304. doi: 10.1176/appi.ajp.162.7.1299. [DOI] [PubMed] [Google Scholar]
- 91.Gaukroger PB, Chapman MJ, Davey RB. Pain control in paediatric burns – the use of patient-controlled analgesia. Burns. 1991;17:396–9. doi: 10.1016/s0305-4179(05)80073-7. [DOI] [PubMed] [Google Scholar]
- 92.Kinsella J, Glavin R, Reid WH. Patient-controlled analgesia for burn patients: A preliminary report. Burns. 1988;14:500–3. doi: 10.1016/s0305-4179(88)80011-1. [DOI] [PubMed] [Google Scholar]
- 93.Rovers J, Knighton J, Neligan P, Peters W. Patient-controlled analgesia in burn patients: A critical review of the literature and case report. Hosp Pharm. 1994;29:108–11. [PubMed] [Google Scholar]
- 94.Osgood PF, Szyfelbein SK. Management of burn pain in children. Pediatr Clin North Am. 1989;36:1001–13. doi: 10.1016/s0031-3955(16)36733-5. [DOI] [PubMed] [Google Scholar]
- 95.Angst MS, Clark D. Opioid-induced hyperalgesia: A qualitative systematic review. Anesthesiology. 2006;104:570–87. doi: 10.1097/00000542-200603000-00025. [DOI] [PubMed] [Google Scholar]
- 96.Faucher LD, Furukawa K. Practice guidelines for the management of pain. J Burn Care Rehabil. 2006;27:659–68. doi: 10.1097/01.BCR.0000238117.41490.00. [DOI] [PubMed] [Google Scholar]
- 97.Stoddard FJ, Sheridan RL, Saxe GN, King BS, King BH, Chedekel DS, Schnitzer JJ, Martyn JA. Treatment of pain in acutely burned children. J Burn Care Rehabil. 2002;23:135–56. doi: 10.1097/00004630-200203000-00012. [DOI] [PubMed] [Google Scholar]
- 98.Richardson P, Mustard L. The management of pain in the burns unit. Burns. 2009;35:921–6. doi: 10.1016/j.burns.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 99.Song L, Wang S, Zuo Y, Chen L, Martyn JA, Mao J. Midazolam exacerbates morphine tolerance and morphine-induced hyperactive behaviors in young rats with burn injury. Brain Res. 2014;1565:52–61. doi: 10.1016/j.brainres.2014.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pal SK, Cortiella J, Herndon D. Adjunctive methods of pain control in burns. Burns. 1997;23:404–12. doi: 10.1016/s0305-4179(97)00029-6. [DOI] [PubMed] [Google Scholar]
- 101.Shank ES, Sheridan RL, Ryan CM, Keaney TJ, Martyn JA. Hemodynamic responses to dexmedetomidine in critically ill intubated pediatric patients: A preliminary study. J Burn Care Rehab. 2013;24:311–7. doi: 10.1097/BCR.0b013e318257d94a. [DOI] [PubMed] [Google Scholar]
- 102.Walker J, MacCallum M, Fischer C, Kopcha R, Saylors R, McCall J. Sedation using dexmedetomidine in pediatric burn patients. J Burn Care Res. 2006;27:206–10. doi: 10.1097/01.BCR.0000200910.76019.CF. [DOI] [PubMed] [Google Scholar]
- 103.Lin H, Faraklas I, Sampson C, Saffle JR, Cochran A. Use of dexmedetomidine for sedation in critically ill mechanically ventilated pediatric burn patients. J Burn Care Res. 2001;32:98–103. doi: 10.1097/BCR.0b013e318203332d. [DOI] [PubMed] [Google Scholar]
- 104.Han T, Kim H, Bae J, Kim K, Martyn JA. Neuromuscular pharmacodynamics of rocuronium in patients with major burns. Anesth Analg. 2004;99:386–92. doi: 10.1213/01.ANE.0000129992.07527.4B. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.