Abstract
Objective
This study describes gender differences in the level and pattern of physical activity in groups of older adults who were frequent fallers, intermittent fallers, or non-fallers.
Methods
Interviews were conducted with adults aged 50 years and older (N = 1834) at senior centers across Pennsylvania from 2010 to 2011. Self-reported falls and validated measures of physical activity were collected at baseline and at 6- and 12-month follow-up assessments.
Results
Complete follow-up data were available for 1487 participants. Men who fell frequently decreased in recreational/leisure activity and household/yard work compared to the intermittent fallers and non-fallers. This association remained even when controlling for baseline health status. All women—regardless of fall group—engaged in similar levels of recreational/leisure activity and household/yard work over time. For both men and women, frequent fallers also showed a greater decrease in walking activities compared to intermittent fallers and non-fallers.
Discussion
Frequent falling among older adults is associated with declines in common leisure, household, and walking activities. The effect of falling frequency on physical activity appears to affect men and women differently, generating the hypothesis that interventions to promote physical activity among fallers need to be gender specific.
Keywords: Physical activity, Falls, Frequent fallers, Elderly, Gender differences
Falls during late life are prevalent. More than 30% of older adults aged 65 years and older and 50% of older adults aged 80 years and older fall each year (Stevens and Sogolow, 2008; Hammer, 2010; Soriano et al., 2007). Falls have a significant impact on subsequent disability, quality of life, and mortality (Finlayson and Peterson, 2010; Centers for Disease Control and Prevention and National Center for Injury Prevention and Control, 2014; Thiem et al., 2014). Older adults who fall once are two to three times more likely to fall again within the next six months (Stevens and Sogolow, 2008). Older adults who are recurrent fallers experience even further losses of physical function and mobility. A review of the literature on interventions to prevent falls among community-dwelling older adults indicates that exercise interventions are effective in reducing fall prevalence and falls risk factors. However, the most effective exercise component and intensity remain unclear (Michael et al., 2010).
One question that is relevant to exercise interventions is whether older adults who experience recurrent falls develop different behavioral patterns compared to those who fall intermittently or not at all. Frequent falls among older adults are largely due to the same underlying cause (e.g., gait disorder). While activity restriction is a common adverse outcome of falling (Deshpande et al., 2008; LeBouthillier et al., 2013), little is known about longitudinal change in physical activities among older adults who frequently fall. This limits progress in understanding the links between falling frequency and the patterns (maintaining, increasing, or decreasing of activity) of various domains of physical activity. Such knowledge could inform interventions aimed at preventing recurrent falls via behavioral training across multiple physical activity domains (e.g., strength training, balance training, walking).
Gender disparities
There are gender disparities in both falls prevalence and physical activity during late life. Women are more likely than men to report a fall and seek medical care for a fall (Stevens and Sogolow, 2012; Stevens et al., 2012). Non-fatal fall rates are higher among women; however, fatal fall rates are higher among men (CDC, 1999). Women tend to outlive men, which may explain why falls and fall-related injuries disproportionately affect women. Given the aging of the Baby Boom generation, falls among women will become a significant focus of public health intervention. Women's higher fall rate may be explained by gender differences in physical activity. Compared to men, women are less physically active (in terms of aerobic exercise) and have smaller lower body strength (CDC, 2014; Oman et al., 1999). Muscular weakness is a strong predictor of falls in both women and men (Moreland et al., 2004). While research has shown gender differences in falls and physical activity separately, it is not known whether there are differences in the physical activity patterns of older women and men who frequently fall.
Current study
To understand patterns of physical activity among older adults who fall, three waves of data from Falls Free Pennsylvania, a longitudinal community study of falls among older adults, were analyzed (Albert et al., 2014). We grouped physical activity into five domains: recreational/leisure activities, walking activities, household/yard work, aerobic/exercise activities, and non-mobility activities (see Table 1). It was hypothesized that older adults who frequently fall—defined as 3 falls within one year—decrease engagement in aerobic/exercise activities and household chores but maintain engagement in activities that are less physically demanding, or important for self-maintenance (leisure activity, walking), compared to older adults who fall less often or not at all. We also hypothesized that older adults who frequently fall will increase their engagement in non-mobility activities, compared to older adults who fall less often or not at all. We based this hypothesis on the selective optimization with compensation theory which suggests that older adults strive to remain active throughout late life, but compensate for lost functional abilities when faced with an aging-related decline (Baltes and Baltes, 1990; Baltes and Carstensen, 1999). We also examined gender effects on the relationship between falling frequency and physical activity. We hypothesized that falling frequency would have a stronger effect on men's physical activity than it would on women's physical activity. Finally, sustaining an injury as a result of falling was also explored to determine whether injuries moderate the relationship between falling frequency and physical activity.
Table 1.
Classification of activities.
| Domain | CHAMPS questionnaire items | MET value M (SD, range) |
|---|---|---|
| Recreational/leisure activities | Dance, play golf walking, play golf riding a cart, singles tennis, doubles tennis, skate, ride a bicycle | 4.0 (1.2, 2–6) |
| Household/yard work | Heavy work around the house (washing windows), light work around the house (sweeping), heavy gardening (raking), light gardening (watering plants), work on car, truck, or other machinery | 3.0 (0.6, 2.3–4.0) |
| Walking activities | Walk or hike uphill, walk fast or briskly for exercise, walk to do errands, walk leisurely for pleasure | 3.6 (1.4, 2.5–6.0) |
| Aerobic/exercise activities | Jog/run, aerobic machines, water exercises, swim moderately fast, swim gently, stretching/flexibility exercises, yoga or Tai Chi, aerobics or aerobic dancing, heavy strength training, light strength training, calisthenics, play basketball, soccer, or racquetball | 3.8 (1.4, 2.0–7.0) |
| Non-mobility activities | Visit friends/family, go to senior center, volunteer work, attend church, attend clubs/group meetings, use a computer, arts/crafts, attend concerts/movies/lectures, play card games/bingo, shoot billiards, play a musical instrument, read | N/A |
Note. CHAMPS = Community Healthy Activities Model Program for Seniors.
MET = Metabolic equivalent of task, or the rate of energy consumption during a specific task.
Methods
Study sample and procedure
Participants for this study came from the Pennsylvania (PA) Department of Aging's Healthy Steps for Older Adults, a primary prevention program aimed to prevent falls among older adults in senior centers. Briefly, Healthy Steps included physical performance assessments of balance and mobility; referrals for physician care; and a 2-hour falls prevention class involving recognition of falls risk situations as well as demonstration of exercises designed to improve balance and mobility. To date, 40 of 67 PA counties have hosted Healthy Steps, and more than 32,000 older adults have completed the program. Between 2010 and 2011 Falls Free PA was developed at the University of Pittsburgh to test the effectiveness of Healthy Steps in reducing falls incidence. Falls Free PA enrolled 814 older adults who completed Healthy Steps and 1020 controls (n = 1834) aged 50 years and older from 19 PA counties. Informed consent was obtained at baseline according to protocols approved by the University of Pittsburgh Institutional Review Board. Participants were interviewed via in-person telephone at baseline and were followed up at 6 and 12 months via automated or in-person telephone interviews. Details of the trial including recruitment, assessments, and research design are described elsewhere (Albert et al., 2014).
For this analysis, three interview assessments were used to establish longitudinal trends: baseline, 6, and 12 months. Of the 1834 participants at baseline, complete follow-up data were available for 1487 participants. A comparison of the attrition group (n = 349) with the final study sample indicated a number of differences in sociodemographic characteristics and baseline health status. The attrition group was less physically active and reported more problems with mobility, self-care, and usual activities; but no differences in age, gender, medical conditions, pain, and the rating of their health state were apparent. The attrition group reported significantly more falls in the past year, but not within the last 30 days. For the purpose of identifying longitudinal trajectories in physical activity, the attrition group was not included in the main analysis.
Because the intent was to identify participants who fell over follow-up, all participants who reported a fall at any of the 3 interview assessments were identified (n = 795). To test the hypothesis that participants who fall frequently are different than those who fall intermittently with respect to physical activity, fallers were divided into a frequent faller group (n = 41) and an intermittent faller group (n = 626). Frequent fallers reported a fall at all three interview assessments, while intermittent fallers reported a fall at one or two interview assessments only. The non-faller control group included individuals who did not experience a fall at baseline, 6-, or 12 months (n = 820). In sum, three distinct groups were created: frequent fallers (n = 41), intermittent fallers (626), and non-fallers (n = 820).
Measures
Falls history
Participants were asked several questions on falls including whether they fell in the past 30 days and 6 months, the number of falls they experienced, and whether they sustained injury or received medical care for any fall. Falling was defined to participants as ending up on the floor or ground because they were unable to stop themselves. For this study, we examined whether participants fell during the past year at the baseline assessment and during the past 6 months at each of the follow-up assessments. Previous research has found retrospective reports to be in accord with prospective recording of falls (Mackenzie et al., 2006). We also used the Tinetti Falls Efficacy Scale (Tinetti et al., 1990) to measure participants' confidence in doing activities that post a risk of falling. The scale consists of 10 items that range from 1 (very confident) to 10 (not con-fident at all), for a maximum of 100 points. Higher total scores indicate a lack of confidence in performing activities.
Physical activity
Daily physical activities were measured using the Community Healthy Activities Model Program for Seniors (CHAMPS) physical activity measure (Stewart et al., 1997, 2001). The CHAMPS assesses weekly frequency and duration of 40 different activities and range from light to vigorously intense. The CHAMPS questionnaire was specifically designed for older populations and consistently demonstrates acceptable reliability, validity, and sensitivity to change (Stewart et al., 1997, 2001). We examined the duration (hours/week) of activities in five subgroups: recreational/leisure activities, household/yard work, walking activities, aerobic/exercise activities, and non-mobility activities. These 5 subgroups represent common activities among older populations. The classification of CHAMPS items is presented in Table 1.
Health status variables
Self-rated health was measured using the EuroQuol 5D, a quality of life assessment that measures mobility, self-care, daily activities, frequency of pain, and symptoms of anxiety or depression, as well as ratings of global health (0–100 visual analog scale) (Kind et al., 1998; Shaw et al., 2005). Scores in each domain range from 0 to 2 with higher scores indicating greater difficultly. Medical illnesses were measured using a count of conditions that were diagnosed by a physician, including stroke, diabetes, high blood pressure, heart attack, macular degeneration, arthritis, osteoporosis, glaucoma, inner ear problem, depression, chronic obstructive pulmonary disease, congestive heart failure, peripheral neuropathy, Parkinson's disease, cognitive impairment, fractures, or cancer (range = 0–17).
Statistical analyses
Baseline comparisons of sociodemographic and health status variables among the three groups were performed using analysis of variance for continuous variables or contingency table analysis using the chi-square test for categorical variables. To examine trajectories of physical activity in frequent fallers versus intermittent fallers and non-fallers, repeated-measures multivariate analysis of variance (MANOVA) was performed across the five activity domains, treating group (frequent fallers, intermittent fallers, and non-faller controls) as the between-subject variable and the three interview assessments of physical activity (baseline, 6, and 12 months) as the within-subject variable. Given the gender disparity in falls prevalence (women fall more than men) and physical activity (men engage in more physical activity than women), we explored the main and interaction effects of participant gender on physical activity patterns. In a second model, falls efficacy and health status variables that were significantly different between the three groups were included as covariates in the repeated measures MANOVA. For the analyses mentioned, p values b.05 were considered statistically significant. All analyses were performed using SPSS, version 20.0, statistical software for Windows.
Results
Descriptive statistics
Table 2 compares the three fall groups (frequent fallers, intermittent fallers, and non-fallers) in terms of baseline sociodemographic and health status measures and presents group differences. The groups were similar in age, sex, race, and marital status. The intermittent fallers reported more medical illnesses than non-fallers. Frequent and intermittent fallers reported more confidence in performing activities that pose a risk of falling than non-fallers. Frequent and intermittent fallers also reported more problems with mobility, self-care, usual activities, and anxiety/depression than non-fallers. However, there was no significant group difference in participants' self-reported rating of their health status. Given the significant group difference in falls efficacy, medical illnesses, and in the EQ-5D, we controlled for the number of illness and problems with mobility in our main analyses. We included the mobility scale of the EQ-5D because of the known association between mobility and incident falls.
Table 2.
Participant characteristics at baseline (n = 1487), Falls Free PA, 2010–2011.
| Variable | Overall (n = 1487) | Fall Group |
p Value | Multiple |
||
|---|---|---|---|---|---|---|
| Frequent fallers (FF, n = 41) | Intermittent fallers (IF, n = 626) | Non-fallers (NF, n = 820) | Comparisons* | |||
| Age, mean ± SD | 75.5 ± 8.3 | 75.7 ± 9.0 | 75.8 8.6 | 75.2 ± 8.0 | 0.39 | – |
| Sex, n (%) | ||||||
| Women | 1184 (79.6) | 31 (75.6) | 487 (77.8) | 666 (81.2) | 0.23 | – |
| Men | 303 (20.4) | 10 (24.4) | 139 (22.2) | 154 (18.8) | ||
| Married, n (%) | 529 (35.6) | 14 (34.1) | 204 (32.6) | 311 (37.9) | 0.22 | – |
| Race, n (%) | 0.09 | – | ||||
| White | 1335 (89.8) | 34 (82.9) | 560 (89.5) | 741 (90.4) | ||
| Black or African American | 109 (7.3) | 4 (9.8) | 48 (7.7) | 57 (7.0) | ||
| Other | 43 (2.8) | 3 (7.2) | 18 (2.8) | 22 (2.6) | ||
| Education | 0.03 | – | ||||
| Elementary | 51 (3.4) | 1 (2.4) | 28 (4.5) | 22 (2.7) | ||
| Some high school education | 138 (9.3) | 3 (7.3) | 53 (8.5) | 82 (10.0) | ||
| High school diploma | 701 (47.2) | 12 (29.3) | 276 (44.1) | 413 (50.6) | ||
| Some college education | 348 (23.5) | 13 (31.7) | 153 (24.4) | 182 (22.3) | ||
| College degree | 246 (16.6) | 12 (29.3) | 116 (18.5) | 118 (14.4) | ||
| Chronic conditions a, mean ± SD | 3.4 ± 1.9 | 3.8 ± 1.7 | 3.8 ± 1.9 | 3.2 ± 1.9 | <.001 | IF > NF |
| Falls efficacy, mean ± SD | 95.6 ± 8.1 | 92.8 ± 8.3 | 94.0 ± 9.6 | 97.0 ± 6.4 | <.001 | FF > NF, IF > NF |
| Health-related QOLb, mean ± SD | ||||||
| Mobility | .37 ± .48 | .59 ± .50 | .46 ± .50 | .28 ± .45 | <.001 | FF > NF, IF > NF |
| Self-care | .05 ± .22 | .12 ± .33 | .07 ± .25 | .03 ± .18 | <.001 | FF > NF, IF > NF |
| Usual activities | .27 ± .46 | .54 ± .51 | .34± .49 | .21 ± .41 | <.001 | FF > NF, IF > NF, FF > IF |
| Pain | .65 ± .55 | .73 ± .59 | .71 ± .56 | .59 ± .53 | <.001 | IF > NF |
| Anxiety or depression | .29 ± .48 | .51 ± .64 | .36 ± .51 | .23 ± .43 | <.001 | FF > NF, IF > NF |
| Rating of health status (1–100) | 81.9 ± 51.0 | 70.5 ± 20.0 | 80.0 ± 55.4 | 84.14 ± 48.4 | 0.11 | – |
Notes. Chi-square and analysis of variance (ANOVA) tested for between group differences.
Multiple comparisons (Bonferroni method) after significant results in ANOVA (p < .05).
Range = 0–11.
QOL = Quality of life; measured with the EQ-5D = EuroQOL five dimensions questionnaire; range = 0–2.
Falling frequency and physical activity patterns
Table 3 shows the repeated measures MANOVA to test the effect of fall group and time (baseline, 6, and 12 months) on physical activity. Results yielded a significant overall effect for fall group. Univariate analyses indicated that there was a significant difference between fall groups in recreational/leisure activities, home/yard work, and walking activities. The interaction between fall group and time was significant for recreational/leisure activities and home/yard work. These findings remained while controlling for baseline falls efficacy, problems with mobility, and medical illnesses. Sustaining an injury as a result of falling did not significantly change trajectories of physical activity.
Table 3.
Effects of time and group on duration of physical activity/week, Falls Free PA, 2010–2011.
| Variable | ANOVA |
|||||
|---|---|---|---|---|---|---|
| MANOVA |
Recreational/leisure activities |
Home/yard work |
Walking activities |
Aerobic/exercise activities |
Non-mobility activities |
|
| F (2, 909) | F (2, 909) | F (2, 909) | F (2, 909) | F (2, 909) | ||
| Between | ||||||
| Group | 2.03* | 3.57* | 4.61* | 0.34 | 0.15 | 0.53 |
| Gender | 3.31** | 4.89* | 0.00 | 1.14 | 1.44 | 6.60* |
| Group × gender | 1.12 | 1.13 | 1.54 | 0.03 | 0.14 | 1.62 |
| Within | ||||||
| Time | 0.49 | 0.75 | 0.59 | 0.58 | 0.02 | 0.43 |
| Time × group | 2.27** | 7.84** | 3.09* | 0.40 | 0.07 | 0.18 |
| Time × gender | 3.70** | 12.53** | 3.18* | 1.09 | 0.64 | 1.53 |
| Time × fall group × gender | 2.45** | 7.31** | 2.61* | 1.58 | 0.45 | 0.49 |
Notes. F ratios are Wilk's approximations of Fs. MANOVA = multivariate analysis of variance; ANOVA = univariate analysis of variance. Group = frequent fallers, intermittent fallers, and non-faller controls. Physical activity = baseline, 6-, and 12-month follow-up.
p < .05.
p < .01.
For recreational/leisure activities, frequent fallers decreased engagement from baseline to 6 months and then remained inactive from 6- to 12 months, while intermittent fallers and non-fallers did not change their recreational/leisure activity over time. For home/yard work, frequent fallers engaged in more activity than intermittent fallers and non-faller controls for the entire year. Frequent fallers slightly decreased their home/yard work activities from 6- to 12 months while intermittent fallers and non-faller controls remained relatively stable over time. For walking activities, frequent fallers significantly decreased their walking activity by 12 months, while intermittent fallers and nonfaller controls remained relatively stable over time.
Gender effects
We also explored the effects of gender and its interaction with fall group and time on physical activity. There was a significant overall effect for gender, a significant interaction between gender and time, and a significant three-way interaction between gender, group, and time (see Table 3). Univariate analyses revealed that there was a significant three-way interaction for recreational/leisure activities and home/yard work. No significant interaction effects emerged for walking activities, aerobic/exercise activities, or non-mobility activities.
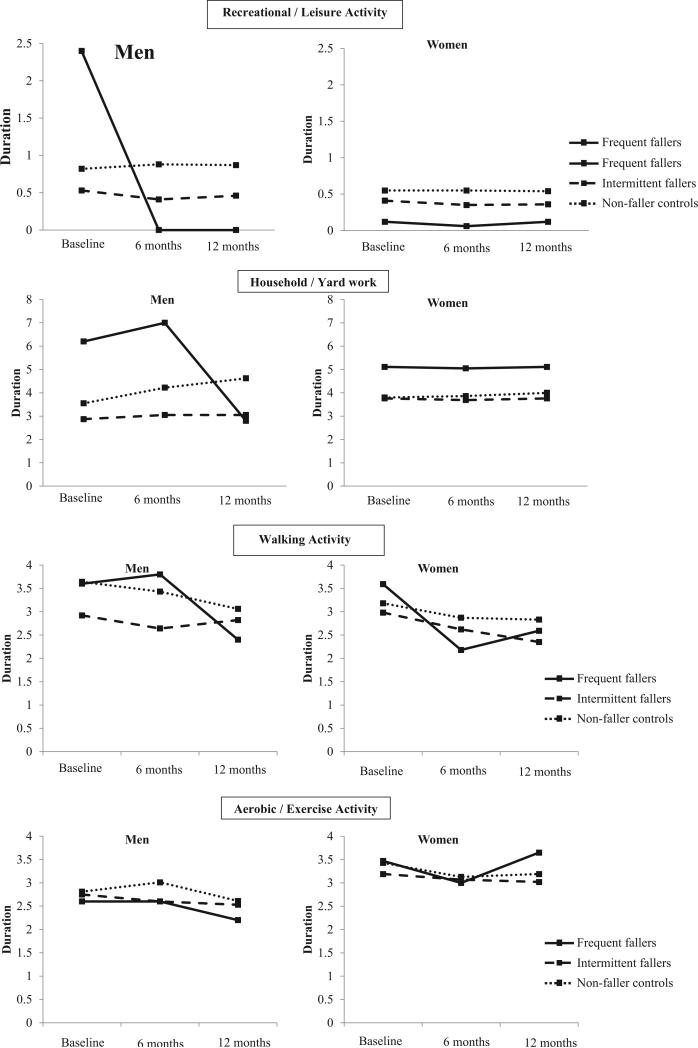
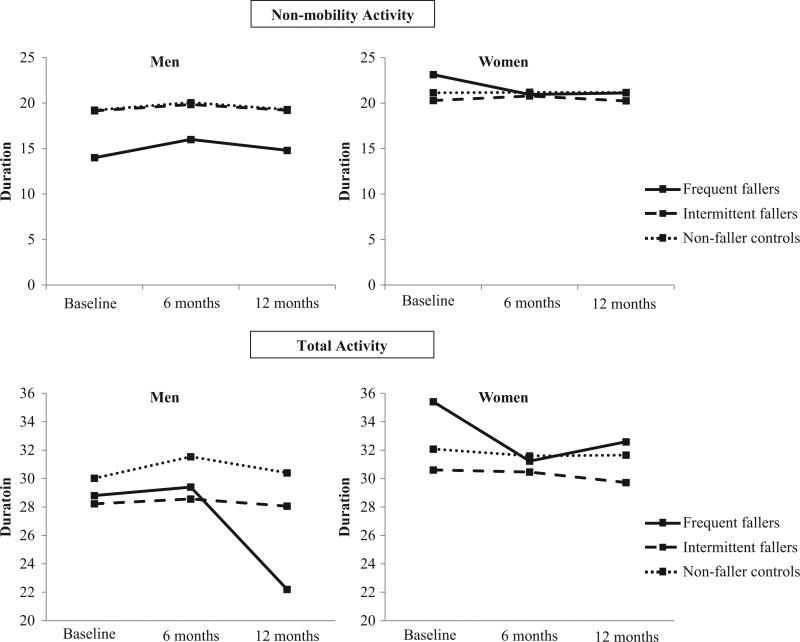
The estimated marginal means are displayed in Fig. 1 to show the difference in trajectory of physical activity in the three fall groups for men and women. For recreational/leisure activity, men who were frequent fallers engaged in the most activity at baseline and then decreased to zero activity at 6- and 12 months. Men who were intermittent fallers and non-fallers engaged in similar levels of recreational/leisure activity over time. All women engaged in similar levels of recreational/leisure activity over time. For home/yard work, men who were frequent fallers engaged in the most activity, but significantly declined by 12 months. Men who were intermittent fallers or non-fallers engaged in similar levels of home/yard work over time. While all women engaged in similar levels of home/yard work over time, frequent fallers engaged in significantly more activity than intermittent fallers and nonfallers at each interview assessment.
Fig. 1.
Trends in physical activity domains for older adult men and women, Falls Free PA, 2010–2011. Duration can be interpreted using the following CHAMPS codes: 1 = less than 1.0 h/week; 2 = 1.0–2.5 h/week; 3 = 3.0–4.5 h/week; 4 = 5.0–6.5 h/week; 5 = 7.0–8.5 h/week; 6 = 9 or more hours/week.
Discussion
In this community sample of older adults, we found that frequent falling was associated with a decline in recreational/leisure activity and household/yard work over one year of follow-up, but among men only. The greater overall decline in activity in the frequent falling group remained significant even after controlling for baseline medical conditions and mobility. By contrast, women—regardless of fall group—showed no decline in recreational/leisure activity and household/ yard work over the one year of follow-up.
Several findings emerge from our strategy of separating frequent from intermittent fallers. First, we found that frequent fallers at baseline were more active than intermittent fallers and non-fallers. Although frequent fallers may reap the physical and mental health benefits of an active lifestyle, they are more likely to be in situations that pose a risk for falls. This group of older adults may also have the most difficulty adapting to an aging-related decline (e.g., lost functional abilities), especially if they have remained active during most of their lifetime. Second, we found a gender difference in falls, such that women were more likely to be frequent fallers compared to men. This is consistent with previous research on gender differences in falls (Stevens and Sogolow, 2012; Stevens et al., 2012). We also found a notable gender disparity among frequent fallers in physical activities that are common during late-life: leisure activity and household work. Falling frequency does not appear to affect women's engagement in leisure activity and household work. As expected, women—regardless of fall group—engaged in very little leisure activity, may explain why falling did not impact their activity trajectory (Stevens and Sogolow, 2012; CDC, 2014). It is interesting that frequent faller women continue to engage in their household work while frequent faller men decline in household work. This difference may be attributable to older adults’ gender role expectations for household chores. That is, they may be more likely to be obligatorily active, i.e., not have the option to reduce activity in these domains. It is also possible that women are more likely to be engaged in caregiving activities, which also affects their continued engagement in household chores. A third finding is that frequent fallers significantly decreased their walking behavior over one year of follow-up. This finding is troubling from a public health vantage, given the beneficial impact of walking on physical, mental, and cognitive health during late life. At 12 months, frequent fallers were walking at levels similar to controls—approximately 1.0–2.5 h/week—but this level is below the CDC's recommendation of 150 min/week of moderately-intense activity (e.g., brisk walking). All older adults should be encouraged to walk, even if it is in small bouts (e.g., 10 minute segments) throughout the week. Fourth, frequent and intermittent fallers alike appeared to maintain engagement in activities that were less strenuous, like recreational/leisure activity. However, this is not surprising given that older adults are less likely to engage in activities that are vigorously intense (e.g., running and heavy strength training).
Finally, it is important to note that sustaining an injury as a result of falling did not modify the association between falling frequency and physical activity in this cohort. One possibility is that the self-report assessment of falls may have limited our ability to assess the effect of an injury accurately. Some older adults may have interpreted an injury as one that requires medical care, while other older adults may have interpreted it differently. Future studies should use more sensitive assessments of injury-related falls. We would expect that sustaining an injury would severely limit physical activity.
Several study limitations must be acknowledged. First, we used a self-report of physical activity, which is not the equivalent of an objective, accelerometry-based assessment. Although the CHAMPS shows consistent reliability and validity among older populations, participants may have problems with memory and cognition, which may limit their ability to recall their physical activity accurately. Unlike other studies that use the CHAMPS, we did not have data on participants’ weight and therefore were unable to calculate energy expenditure. Future studies should examine the relation between frequent falling and specific activity intensities (light [MET value <3], moderate [MET 3–6], and vigorous [MET >6). Second, participants lost to follow-up had some significant differences from those included in this study. Differences included more problems with mobility, usual activities, and pain in the attrition group; therefore our results may downplay the relationship between falling frequency and patterns of physical activity.
Conclusions
The present study demonstrated that older adults who fall frequently had a steeper decrease in the trajectory of recreational/leisure activity and household/yard work than those who fall intermittently or not at all, but among men only. Studies evaluating the effect of falls on physical activity need to assess physical activity longitudinally rather than at a single time point and need to consider gender effects. Because physical activity is modifiable and reduces the risk of incident falls, future studies need to address the mechanisms (social-cognitive and environmental) by which frequent falling impacts patterns of physical activity.
Footnotes
Research supported by Cooperative Agreement DP002657 from the Centers for Disease Control and Prevention, CDC Prevention Research Centers program U48 DP001918, and NIH P30 AG024827. Preparation of this manuscript was also supported in part by grants from NIH P30 MH090333-01A1, MHO19986, NR009573, NR013450, AG026010, AG032370, and NSF 0540865.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Albert SM, Edelstein O, King J, et al. Assessing the quality of a nonrandomized pragmatic trial for primary prevention of falls among older adults. Prev. Sci. 2014 doi: 10.1007/s11121-014-0466-2. (Epub ahead of print) http://www.ncbi.nlm.nih.gov/pubmed/24488533. [DOI] [PMC free article] [PubMed]
- Baltes PB, Baltes MM. Psychological perspectives on successful aging: The model of selective optimization with compensation. In: Baltes PB, Baltes MM, editors. Successful aging: Perspectives from the behavioral sciences. Cambridge University Press; New York: 1990. pp. 1–34. [Google Scholar]
- Baltes MM, Carstensen LL. Social-psychological theories and their applications to aging: from individual to collective. In: Bengtson VL, Schaie KW, editors. Handbook of Theories of Aging. Springer; New York: 1999. pp. 209–226. [Google Scholar]
- CDC Surveillance for injuries and violence among older adults. In: Surveillance for selected public health indicators affecting older adults, United States. Morb. Mortal. Wkly Rep. 1999;48:27–50. [PubMed] [Google Scholar]
- CDC Facts About Physical Activity. 2014 (Retrieved from: http://www.cdc.gov/physicalactivity/data/facts.html)
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control [May 10, 2014];Web-based Injury Statistics Query and Reporting System (WISQARS) 2014 [online] [Google Scholar]
- Deshpande N, Metter EJ, Lauretani F, Bandinelli S, Guralnik J, Ferrucci L. Activity restriction induced by fear of falling and objective and subjective measures of physical function: a prospective cohort study. J. Am. Geriatr. Soc. 2008;56:615–620. doi: 10.1111/j.1532-5415.2007.01639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson ML, Peterson EW. Falls, aging, and disability. Phys. Med. Rehabil. Clin. N. Am. 2010;21:357–373. doi: 10.1016/j.pmr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Hammer J. Increasing number of unintentional falls indicates urgent need for fall prevention programs. J. Am. Geriatr. Soc. 2010;58:603–604. doi: 10.1111/j.1532-5415.2010.02749.x. [DOI] [PubMed] [Google Scholar]
- Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. Brit. Med. J. 1998;316:736–741. doi: 10.1136/bmj.316.7133.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBouthillier DM, Thibodeau MA, Asmundson GJG. Severity of fall-based injuries, fear of falling, and activity restriction: sex differences in a population-based sample of older Canadian adults. J. Aging Health. 2013;25:1378–1387. doi: 10.1177/0898264313507317. [DOI] [PubMed] [Google Scholar]
- Mackenzie L, Byles J, D'Este C. Validation of self-reported fall events in intervention studies. Clin. Rehabil. 2006;20(4):331–339. doi: 10.1191/0269215506cr947oa. [DOI] [PubMed] [Google Scholar]
- Michael YL, Whitlock EP, Lin JS, et al. Primary care relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2010;153:815–824. doi: 10.7326/0003-4819-153-12-201012210-00008. [DOI] [PubMed] [Google Scholar]
- Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J. Am. Geriatr. Soc. 2004;52:1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- Oman D, Reed D, Ferrara A. Do elderly women have more physical disability than men do? Am. J. Epidemiol. 1999;150:834–842. doi: 10.1093/oxfordjournals.aje.a010088. [DOI] [PubMed] [Google Scholar]
- Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med. Care. 2005;43:203–220. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary-care providers. Clin. Interv. Aging. 2007;2:545–553. doi: 10.2147/cia.s1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Sogolow ED. Preventing Falls: What Works. A CDC Compendium of Effective Community-Based Interventions from Around the World. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, GA.: 2008. [Google Scholar]
- Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj. Prev. 2012;11:115–119. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged medicare population. Am. J. Prev. Med. 2012;43:59–62. doi: 10.1016/j.amepre.2012.03.008. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, Sepsis PG, et al. Evaluation of CHAMPS, a physical activity promotion program for older adults. Ann Beh Med. 1997;19:353–361. doi: 10.1007/BF02895154. [DOI] [PubMed] [Google Scholar]
- Stewart A, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS Physical activity questionnaire for older adults: outcomes and interventions. Med. Sci. Sport Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Thiem U, KlaaBen-Mielke R, Trampisch U, Moschny A, Pientka L, Hinrichs T. Falls and EQ-5D rated quality of life in community-dwelling seniors with concurrent chronic diseases: a cross-sectional stud. Health Qaul. Life. Outcomes. 2014;12:2–9. doi: 10.1186/1477-7525-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti M, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990;45(6):239. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]