Abstract
AIM
To investigate the spectrum and antibiotic susceptibility of bacteria isolated from patients with suspected corneal infections in Zhongshan Ophthalmic Center in South China over the past four years retrospectively.
METHODS
Totally 1943 corneal scrapes from patients with corneal infections from 2010 to 2013 were cultured and processed using standard microbiological procedures to identify bacterial isolates. Simultaneously, the bacterial isolates were tested for antibiotic susceptibility to 8 antibiotics (ceftazidime, cefuroxim, cefazolin, levofloxacin, ofloxacin, neomycin, tobramycin, chloramphenicol) using the Kirby-Bauer disc diffusion technique.
RESULTS
Of the total 1943 scrapes, 397 (20.43%) were culture-positive, of which 294 (74.06%) were gram-positive (GP) and 103 (25.94%) were gram-negative (GN) bacteria. Of the GP organisms, the most prevalent genera were Staphylococcus spp. (56.17%, n=223), Kocuria spp. (5.29%, n=21) and Micrococcus spp. (1.26%, n=5). On the other hand, the most prevalent genera were Pseudomonas spp. (12.85%, n=51), Burkholderia spp. (2.02%, n=8) and Acinetobacter spp. (1.51%, n=6) for the GN organisms. Among five antibiotics that have eye drop products, the resistant to neomycin of GP (7.82%, 95% CI: 4.72%-10.92%) and GN isolates (9.71%, 95% CI: 4.01%-15.41%) was lowest, while the resistant to chloramphenicol was highest (GP: 34.35%, 95% CI: 28.92%-39.78%; GN: 60.19%, 95% CI: 50.74%-69.64%).
CONCLUSION
Staphylococcus spp. was the most common bacterial pathogens isolated from patients with corneal infections in this setting. High percentages of GP and GN bacteria were mostly susceptible to neomycin and highly resistant to chloramphenicol.
Keywords: antibiotic susceptibility, epidemiology, corneal infections, bacterial spectrum
INTRODUCTION
The prevalence of corneal bacterial infections is common among various corneal infections. Bharathi et al[1] and Srinivasan et al[2] reported that the prevalence of corneal bacterial infections among corneal microbial infections was 32.77% and 33.2% respectively. Patients may sometimes develop refractory disease or even vision loss. In clinical practice, medical treatments of corneal bacterial infections are usually initiated prior to pathogen identification and the antibiotic susceptibility test[3]. There have been many reports on the microbial spectrum of corneal infections, and the results vary case by case. A retrospective study revealing the distribution of bacterial keratitis in North China reported that, among 490 mono-bacterial positive cultures (isolated from 2220 cases), gram-positive (GP) cocci were the leading causative organism of bacteria keratitis (S. epidermidis, Micrococcus spp., S. aureus), followed by the gram-negative (GN) bacilli (Pseudomonas spp., Acinetobacter spp., Moraxella spp.)[4]. In Australia, GP bacteria (29% of scrapes) were also the most common group of organisms isolated from keratitis, most of which were GP cocci in the Staphylococcus and Streptococcus genera[5]. In the original reports from India and Brazil, the most common pathogens isolated from bacterial keratitis were various species of Staphylococcus spp. (64.5%, 51.7%, respectively)[6]–[7]. However, in South India, the most prevalent bacteria isolated from bacterial keratitis cases was Streptococcus pneumonia (35.95%)[1]. These different results have been attributed to the region and environment, as well as seasonal changes[5],[8]. In fact, many studies have examined the types of bacteria that can be routinely cultured from swabs of ocular surface even immediately after birth, such as S. epidermidis, S. aureus, Propionibacterium, etc[9]–[10]. Although some of these organisms are normal regional flora in ocular surface, when host defenses are breached, they can be pathogenic.
Although effective antibiotics reduce the incidence of corneal bacterial infections and improve its prognosis, the unreasonable use of various antibiotics leads to the emergence of drug-resistant strains and even induce opportunistic infections caused by bacteria that are usually harmless or of low virulence[11]. Recently, a WHO report emphasized that “resistance to common bacteria has reached alarming levels in many parts of the world indicating that many of the available treatment options for common infections in some settings are becoming ineffective” (www.who.int). Antimicrobial resistance (AMR) is an issue not only for systemic diseases but also ocular infections. To date, various drug resistances in ocular infections were reported by different scholars. Shimizu et al[12] investigated the trend in the emergence of levofloxacin-resistant (LVFX-resistant) strains from patients with ocular infections from 2006 to 2009 in Japan, the result indicated that LVFX-resistant strains accounted for 40 out of a total of 122 strains (32.8%). Fortunately, a report from the US, Miller et al[13] revealed that besifloxacin may offer extended coverage for some ocular pathogens those are resistant to current fluoroquinolones. In Brazil, a study about the shifting trends in vitro antibiotic susceptibilities for corneal scrapes during a period of 15y demonstrated that the susceptibility to amikacin and neomycin was improved (88%-95% and 50%-85%, respectively)[14]. Based on the results above, the diversity of pathogens in ocular infections or even a change in the environment may contribute to differences in drug resistance[15]. On the other hand, multidrug resistant (MDR) bacteria has been recently re-defined as that organisms are resistant to at least one agent in each of three or more antimicrobial categories[16]. Under this new standard, the MDR bacteria profile of cornea infection has not yet been reported.
The bacterial spectra and their antibiotic susceptibility pattern of the cornea infections vary in different geographical areas, which will influence the selection of appropriate empirical treatment before laboratory microbiological reports are available in clinical practice. In order to understand the pathogenic bacterial spectrum of corneal infections and their antibiotic resistance in South China, this study retrospectively investigated and analyzed the ocular isolates obtained from clinical patients and assessed the in vitro susceptibility of the most common bacterial isolates to several antibiotics in an attempt to provide guidance for clinical management.
SUBJECTS AND METHODS
A retrospective review was carried out on all patients with suspected corneal bacterial infections presenting at Zhongshan Ophthalmic Center, Guangzhou, Guangdong Province, China, between January 2010 and December 2013. This study was conducted in compliance with the principles of the Declaration of Helsinki and was approved by the Institutional Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University.
Bacterial Isolation and Identification
Patients with suspected corneal bacterial infections with epithelial damage or ulcers were recruited by ophthalmologists to perform a corneal scrape for smear and culture. Specimens were collected under topical anesthesia (0.5%, proparacaine hydrochloride), complying with the principle of aseptic technique, by using standard corneal scraping kits made of plates and slides that were all directly inoculated. For each patient, a portion of the corneal scraping material was used for gram-staining immediately, while the remaining sample was inoculated in nutrient broth and incubated overnight at 35̊C. Subsequently, the broth was inoculated onto potato dextrose agar for fungal culture or sheep blood agar for bacterial culture. The cultures were considered positive if colonies grew at the sites of inoculation on one or more agar plates and were identified using an automated microbiology system (Vitek2 compact, BioMerieux, Inc.100 Rodolphe Street, Durham, USA). Cultures that grew fungus only were excluded.
Antibiotic Susceptibility Test
Antibiotic susceptibility testing of isolated bacteria was performed in vitro on ceftazidime (30 µg), cefuroxim (30 µg), cefazolin (30 µg), levofloxacin (5 µg), ofloxacin (5 µg), neomycin (30 µg), tobramycin (10 µg), and chloramphenicol (30 µg) using the Kirby-Bauer disc diffusion method. Bacterial susceptibilities were recorded as “resistant”, “intermediate” and “sensitive”, for the purpose of the study, “intermediate” and “sensitive” were both considered “sensitive”. The antibiotic susceptibility was determined in accordance with the methods of the Clinical and Laboratory Standards Institute (CLSI).
Statistical Analysis
The statistical analysis was performed using SPSS 17.0 (Chicago, IL, USA). The Chi-square test was employed for the comparison of categorical variables. Differences were considered significant at P<0.05.
RESULTS
A total of 1943 scrapes from the suspected corneal bacterial infections were cultured at our institution during the study period. Of the 1943 samples collected, bacteria were cultured from 397 samples. Of these, the most prevalent organisms were GP organisms (74.06%, n=294), wherein the most prevalent bacterial genera were Staphylococcus spp. (56.17%, n=223), Kocuria spp. (5.29%, n=21) and Micrococcus spp. (1.26%, n=5). The GN organisms accounted for approximately 25.94% (n=103) of all isolates. Of these, the most prevalent bacterial genera were Pseudomonas spp. (12.85%, n=51), Burkholderia spp. (2.02%, n=8) and Acinetobacter spp. (1.51%, n=6). The bacterial spectrum is described in Table 1 in detail.
Table 1. Bacterial isolates recovered from patients with bacteria keratitis.
| Bacterium | n | % |
| GP organisms | 294 | 74.06 |
| Staphylococcus spp. | 223 | 56.17 |
| Kocuria spp. | 21 | 5.29 |
| Micrococcus spp. | 5 | 1.26 |
| Bacillus spp. | 5 | 1.26 |
| Enterococcus spp. | 4 | 1.01 |
| Corynebacterium spp. | 4 | 1.01 |
| Streptococcus spp. | 3 | 0.76 |
| Aerococcus spp. | 3 | 0.76 |
| Others GP organisms | 26 | 6.55 |
| GN organisms | 103 | 25.94 |
| Pseudomonas spp. | 51 | 12.85 |
| Burkholderia spp. | 8 | 2.02 |
| Acinetobacter spp. | 6 | 1.51 |
| Escherichia spp. | 5 | 1.26 |
| Enterobacter spp. | 5 | 1.26 |
| Serratia spp. | 4 | 1.01 |
| Chryseobacterium spp. | 3 | 0.76 |
| Other GN organisms | 21 | 5.29 |
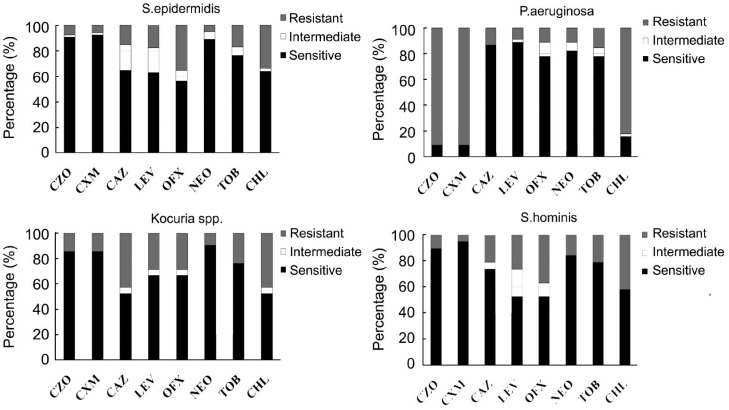
A comparison of the susceptibilities of GP and GN bacteria to eight antibiotics, e.g. ceftazidime, cefuroxim, cefazolin, levofloxacin, ofloxacin, neomycin, tobramycin and chloramphenicol, belonging to four categories, is shown in Table 2. Generally, the total isolates were susceptibility to quinolones, aminoglycosides and third generation of cephalosporins (i.e. ceftazidime). Among the five antibiotics associated with eye drop products (i.e. levofloxacin, ofloxacin, neomycin, tobramycin and chloramphenicol), the resistant to neomycin of GP (7.82%, 95% CI: 4.72-10.92) and GN isolates (9.71%, 95% CI: 4.01-15.41) was lowest, while the resistant to chloramphenicol was highest (GP: 34.35%, 95% CI: 28.92-39.78; GN: 60.19%, 95% CI: 50.74-69.64). Specifically, for five antibiotics that have eye drop products, three predominant GP bacteria (S. epidermidis, S. hominis and Kocuria spp.) showed a high level of susceptibility to neomycin (94.96%, 84.21%, 90.48%, respectively), followed by tobramycin (83.19%, 78.95%, 76.19%, respectively). S. epidermidis was more susceptible to neomycin than tobramycin (P=0.004). The predominant GN bacteria (P. aeruginosa) showed a high level of susceptibility to levofloxacin (91.11%), followed by neomycin (88.89%) and tobramycin (84.45%). The susceptibilities of the four main bacteria to above eight antibiotics are displayed in Figure 1.
Table 2. The percentage of strains resistant to antibacterial agents (95% CI).
| Organism | Cephalosporins |
Quinolones |
Aminoglycosides |
Chloramphenicol | ||||
| Cefazolin | Cefuroxim | Ceftazidime | Levofloxacin | Ofloxacin | Neomycin | Tobramycin | ||
| GP (294) | 10.88 (7.37-14.43) | 9.52 (6.17-12.87) | 22.79 (17.99-27.59) | 18.37 (13.94-22.80) a | 27.9 (22.76-33.04)a | 7.82 (4.72-10.92) | 17.35 (13.07-21.73)a | 34.35 (28.92-39.78)a |
| GN (103) | 75.73 (67.46-84.00) | 70.87 (62.09-79.65) | 15.53 (8.53-22.53) | 15.53 (8.53-22.53) | 16.50 (9.33-23.67) | 9.71 (4.01-15.41) | 25.24 (16.85-33.63)b | 60.19 (50.74-69.64)b |
| Total (397) | 27.71 (23.30-32.12) | 25.44 (21.25-29.83) | 20.91 (16.91-24.91) | 17.63 (13.89-21.37)a | 24.94 (20.69-29.19)a | 8.31 (5.59-11.03) | 19.40 (15.52-23.28)a | 41.06 (36.22-45.90)a |
aP<0.01 vs neomycin (for total bacteria and GP isolates); bP<0.01 vs neomycin (for GN isolates).
Figure 1. Bar charts showing the susceptibility of the main germs of our study namely S. epidermidis, P. aeruginosa, Kocuria and S. hominis.
OFX: Ofloxacin; NEO: Neomycin; CHL: Chloramphenicol; LEV: Levofloxacin; TOB: Tobramycin; CZO: Cefazolin; CXM: Cefuroxim; CAZ: Ceftazidime.
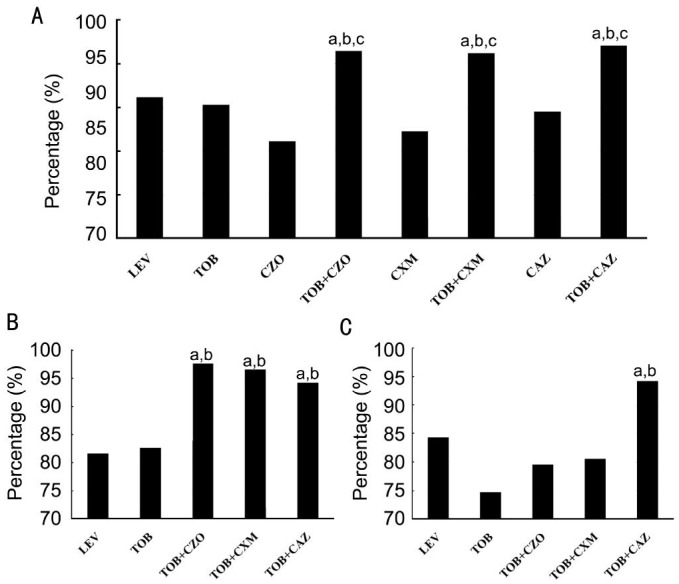
The susceptibility of bacteria to two combined antibiotics were analyzed to explore if they produce a stronger effect in combination than either drug alone, or levofloxacin, which is widely used nowadays (Figure 2). For total bacterial isolates or GP isolates, the susceptibility to combination of tobramycin with cefazolin, cefuroxim or ceftazidime was significant higher than using either one of them or levofloxacin alone (P<0.05, Figure 2A, 2B). However, for GN isolates, the susceptibility to combination of tobramycin and ceftazidime was higher than only one drug was used (Figure 2C).
Figure 2. Comparison of susceptibilities of isolated bacteria to various combinations of antibiotics.
A: The susceptibility of total bacterial isolates to different combinations of antibiotics; B: The susceptibility of GP isolates to different combinations of antibiotics; C: The susceptibility of GN isolates to different combinations of antibiotics. a,b,cP<0.05, a: vs LEV; b: vs TOB; c: vs cephalosporins. LEV: Levofloxacin; TOB: Tobramycin; CZO: Cefazolin; CXM: Cefuroxim; CAZ: Ceftazidime.
Additionally, MDR bacteria species were found in this study. We found sixty-one (15.37%) MDR bacteria those were resistant to at least one agent in each of three or more antimicrobial categories (in our study, cephalosporins, quinolones, aminoglycosides and phenicols) of antibiotics. Of these, the first-two high proportion of resistant bacteria were S. epidermidis (10.92%, 13/119) and P. aeruginosa (20%, 9/45) (Table 3).
Table 3. The species and numbers of multidrug resistance bacteria.
| Organisms (total numberb) | Positive numbera | % |
| S.epidermidis (119) | 13 | 10.92 |
| P.aeruginosa (45) | 9 | 20.00 |
| B.cepacia (8) | 6 | 75.00 |
| S.hominis (19) | 4 | 21.05 |
| E.coli (5) | 3 | 60.00 |
| S.aueicularis (14) | 3 | 21.43 |
| K.roesus (11) | 3 | 27.27 |
| S.simulans (17) | 3 | 17.65 |
| S.haemolyticus (15) | 3 | 20.00 |
| S.warneri (14) | 3 | 21.43 |
| E.faecalis (2) | 2 | 100.00 |
| A.junii (2) | 2 | 100.00 |
| A.baumannii (2) | 1 | 50.00 |
| K.varians (3) | 1 | 33.33 |
| P.putida (2) | 1 | 50.00 |
| Methylobacterum spp. (2) | 1 | 50.00 |
| K.kristinas (7) | 1 | 14.29 |
| P.stutzeri (2) | 1 | 50.00 |
| E.cloacae (3) | 1 | 33.33 |
| Total (292) | 61 | 20.89 |
aThe positive number of the multidrug resistance; bThe total number of each bacteria.
DISCUSSION
The objective of this study was to perform a comprehensive investigation of the bacteria causing corneal infections and their antibiotic resistance in a Tertiary Eye Hospital in South China. In our present study, the culture-positive rate in patients with suspected corneal infections was 20.43%, which approached the rate of 22.07% reported by Sun, who retrospectively investigated the distribution and shifting trends of bacterial keratitis in north China over a span of ten years[4]. In contrast, the culture positivity rates reported from Australia[17] and France[18] were 62.8% and 68.0%, respectively. Because our institution is a tertiary ocular hospital, it is likely that most of the patients received antibiotic treatment prior to the culture. Moreover, the use of topical anesthetic drops has been reported to have antibacterial effects with 24h of incubation[19]–[20]. These reasons may lead to our relatively low culture positivity rate.
Our results also demonstrated that the prominent pathogenic bacteria are GP bacteria, wherein Staphylococcus spp. were the most frequently isolated species (56.17%), a figure similar to that reported in Beijing[4], India[6] and Australia[5]. In Brazil, similarly, the most common pathogens (Staphylococcus spp) of bacterial keratitis accounted for 51.7%[7]. However, in the studies from Western Gujarat (India)[21] and Hong Kong[22], P. aeruginosa was the most common organism isolated. Environmental influences, the number of contact lens-related keratitis cases or the severity of cases included in each study may contribute to these differences[6]. Besides, a number of the most prevalent bacterial genera isolated from the corneal scrapings (i.e. Staphylococcus spp.) are opportunistic pathogens, which can cause ocular infections when host defenses are breached.
The emergence of antibiotic-resistant ocular isolates has long been a concern. In our study, 8 antibiotics (of which 5 are associated with commercial eye drops) belonging to four categories (cephalosporins, quinolones, aminoglycosides, and phenicols) were tested for resistance. Apart from cephalosporins (without eye drops), eye drops of quinolones (levofloxacin, ofloxacin) and aminoglycosides (neomycin, tobramycin) are the main products in the market, while chloramphenicol is an outdated product in China[23]–[24]. In the present study, our results revealed that both the GP and GN microorganisms were highly susceptible to neomycin even more than tobramycin (P<0.01) and highly resistant to chloramphenicol. Both neomycin and chloramphenicol were developed in the 1940s. Neomycin, which is not frequently or routinely used systemic, showed high susceptibility during the study period. However, chloramphenicol as an eye drop was widely used in Chinas a broad-spectrum antibacterial agent and was also widely used in aquaculture and animal husbandry[25]. These uses may increase the concentration of chloramphenicol residues and promote the development and abundance of bacterial resistance by spreading chloramphenicol resistance genes in the ecosystem[26]. This was supported by findings from India, Australia and London[6],[27]–[28].
Results of systematic review and Meta-analysis suggested that fluoroquinolones may be the first choice for empirical treatment in most cases of suspected bacterial keratitis[29]. Several eye drops containing fluoroquinolones are commercially available in China. Of them, ofloxacin and levofloxacin are the most widely used[23]. Our current data revealed that the susceptibility of levofloxacin for total bacteria was up to 80%, which is higher than that of ofloxacin, and lower than that of neomycin. Among the eight antibiotics, neomycin has the lowest resistance for total isolates in this study. The ocular products of neomycin, including compound preparation (e.g. with polymyxin B, gramicidin or corticoid), are produced in solution or ointment form and widely used internationally[30]. It is worth noting that neomycin has nephrotoxicity, ototoxicity and causing contact dermatitis[31], which may lead to less use in systemic diseases. However, according to literature and our present data, ocular preparations of fluoroquinolones as well as neomycin are both suitable for the empirical treatment of suspected bacterial keratitis.
Combined use of antibiotics can expand the antibiotic spectrum and is already applied widely in the empirical treatment for suspected infection disease[32]–[33]. Our results suggested that the combined use of cephalosporin with tobramycin showed higher susceptibility for bacterial isolates, than using levofloxacin or tobramycin alone, especially for the GP bacteria. For GN isolates in our study, the P. aeruginosa accounted for the biggest proportion, which may lead to higher susceptibility of the combination of tobramycin with ceftazidime[34]. However, the side-effects of the combination therapy, particularly with tobramycin-cefazolin, were reported to be an increased risk of ocular discomfort and chemical conjunctivitis as well as a retardation effect of the epithelial-healing rate (aminoglycosides)[35]–[36]. Despite these, considering the higher susceptibility, the systemic or intraocular application administration is necessary when suppurative endophthalmitis occurs[37]–[38].
According to the new definition[16], MDR bacteria to eight antibiotics was observed in 15.4% of the isolates from cornea infection in the present study. It was emphasized that MDR of P. aeruginosa and A. baumannii became great burden pathogens, frequently being related to the high use of broad spectrum antibiotics and previous inadequate empirical antimicrobial treatment[39]. The damage of these bacteria to eyes is serious, and the clinical treatment is difficult. Additionally, it should be noted that the resistance found in vitro does not always correlate with resistance in vivo.
In summary, we found that the most prominent pathogens in corneal bacterial infections are Staphylococcus spp., followed by P. aeruginosa. In the comparison of eight antibiotics, neomycin, levofloxacin and tobramycin may be a better choice for empirical treatment; chloramphenicol, which is widely used in ocular medicine, as well as in aquaculture and animal husbandry showed the highest resistance (41.06%) for pathogens isolated from corneal infections, indicating that chloramphenicol should not be routinely used for corneal infection in China. There is no doubt that antibiotic resistance should be taken into account in empirical treatment, and antibiotic susceptibility testing in all cases of ocular infections is essential.
Acknowledgments
Foundation: Supported in part by the Doctoral Program of Higher Education, Ministry of Education and the Ophthalmologic State Key Laboratory, Sun-Yat Sen University, China.
Conflicts of Interest: Wang N, None; Huang Q, None; Tan YW, None; Lin LP, None; Wu KL, None.
REFERENCES
- 1.Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, Srinivasan M. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14(2):61–69. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- 2.Srinivasan M, Gonzales CA, George C, Cevallos V, Mascarenhas JM, Asokan B, Wilkins J, Smolin G, Whitcher JP. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997;81(11):965–971. doi: 10.1136/bjo.81.11.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giardini F, Grandi G, De Sanctis U, Eandi C, Machetta F, Pollino C, Grignolo FM. In vitro susceptibility to different topical ophthalmic antibiotics of bacterial isolates from patients with conjunctivitis. Ocul Immunol Inflamm. 2011;19(6):419–421. doi: 10.3109/09273948.2011.624289. [DOI] [PubMed] [Google Scholar]
- 4.Sun X, Deng S, Li R, Wang Z, Luo S, Jin X, Zhang W. Zhang. Distribution and shifting trends of bacterial keratitis in north China (1989-98) Br J Ophthalmol. 2004;88(2):165–166. doi: 10.1136/bjo.2002.011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green M, Apel A, Stapleton F. A longitudinal study of trends in keratitis in Australia. Cornea. 2008;27(1):33–39. doi: 10.1097/ICO.0b013e318156cb1f. [DOI] [PubMed] [Google Scholar]
- 6.Kaliamurthy J, Kalavathy CM, Parmar P, Nelson Jesudasan CA, Thomas PA. Spectrum of bacterial keratitis at a tertiary eye care centre in India. Biomed Res Int. 2013;2013:181564. doi: 10.1155/2013/181564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marujo FI, Hirai FE, Yu MC, Hofling-Lima AL, Freitas Dd, Sato EH. Distribution of infectious keratitis in a tertiary hospital in Brazil. Arq Bras Oftalmol. 2013;76(6):370–373. doi: 10.1590/s0004-27492013000600011. [DOI] [PubMed] [Google Scholar]
- 8.Chen X, Adelman RA. Microbial spectrum and resistance patterns in endophthalmitis: a 21-year (1988-2008) review in northeast United States. J Ocul Pharmacol Ther. 2012;28(4):329–334. doi: 10.1089/jop.2011.0204. [DOI] [PubMed] [Google Scholar]
- 9.Willcox MD. Characterization of the normal microbiota of the ocular surface. Exp Eye Res. 2013;117:99–105. doi: 10.1016/j.exer.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Dong Q, Brulc JM, Iovieno A, Bates B, Garoutte A, Miller D, Revanna KV, Gao X, Antonopoulos DA, Slepak VZ, Shestopalov VI. Diversity of bacteria at healthy human conjunctiva. Invest Ophthalmol Vis Sci. 2011;52(8):5408–5413. doi: 10.1167/iovs.10-6939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kunimoto DY, Sharma S, Garg P, Rao GN. In vitro susceptibility of bacterial keratitis pathogens to ciprofloxacin. Emerging resistance. Ophthalmology. 1999;106(1):80–85. doi: 10.1016/S0161-6420(99)90008-8. [DOI] [PubMed] [Google Scholar]
- 12.Shimizu Y, Toshida H, Honda R, Matsui A, Ohta T, Asada Y, Murakami A. Prevalence of drug resistance and culture-positive rate among microorganisms isolated from patients with ocular infections over a 4-year period. Clin Ophthalmol. 2013;7:695–702. doi: 10.2147/OPTH.S43323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller D, Chang JS, Flynn HW, Alfonso EC. Comparative in vitro susceptibility of besifloxacin and seven comparators against ciprofloxacin- and methicillin-susceptible/nonsusceptible staphylococci. J Ocul Pharmacol Ther. 2013;29(3):339–344. doi: 10.1089/jop.2012.0081. [DOI] [PubMed] [Google Scholar]
- 14.Chalita MR, Höfling-Lima AL, Paranhos A, Jr, Schor P, Belfort R., Jr Shifting trends in in vitro antibiotic susceptibilities for common ocular isolates during a period of 15 years. Am J Ophthalmol. 2004;137(1):43–51. doi: 10.1016/s0002-9394(03)00905-x. [DOI] [PubMed] [Google Scholar]
- 15.Mohanta T, Goel S. Prevalence of antibiotic-resistant bacteria in three different aquatic environments over three seasons. Environ Monit Assess. 2014;186(8):5089–5100. doi: 10.1007/s10661-014-3762-1. [DOI] [PubMed] [Google Scholar]
- 16.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 17.Butler TK, Spencer NA, Chan CC, Singh Gilhotra J, McClellan K. Infective keratitis in older patients: a 4 year review, 1998-2002. Br J Ophthalmol. 2005;89(5):591–596. doi: 10.1136/bjo.2004.049072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourcier T, Thomas F, Borderie V, Chaumeil C, Laroche L. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003;87(7):834–838. doi: 10.1136/bjo.87.7.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balbaba M, Ulaş F, Toplu SA. Effect of hemodialysis duration on conjunctival bacterial flora and susceptibility of conjunctival bacterial isolates to fluoroquinolones. Ocul Immunol Inflamm. 2013;21(3):197–200. doi: 10.3109/09273948.2012.758747. [DOI] [PubMed] [Google Scholar]
- 20.Yin VT, Weisbrod DJ, Eng KT, Schwartz C, Kohly R, Mandelcorn E, Lam WC, Daneman N, Simor A, Kertes PJ. Antibiotic resistance of ocular surface flora with repeated use of a topical antibiotic after intravitreal injection. JAMA Ophthalmol. 2013;131(4):456–461. doi: 10.1001/jamaophthalmol.2013.2379. [DOI] [PubMed] [Google Scholar]
- 21.Somabhai Katara R, Dhanjibhai Patel N, Sinha M. A clinical microbiological study of corneal ulcer patients at western Gujarat, India. Acta Med Iran. 2013;51(6):399–403. [PubMed] [Google Scholar]
- 22.Houang E, Lam D, Fan D, Seal D. Microbial keratitis in Hong Kong: relationship to climate, environment and contact-lens disinfection. Trans R Soc Trop Med Hyg. 2001;95(4):361–367. doi: 10.1016/s0035-9203(01)90180-4. [DOI] [PubMed] [Google Scholar]
- 23.Cai DS. The market analysis of Ophthalmic Preparation. Chinese Journal of Pharmacentical Technology Economics & Management. 2008;2(8):7–14. [Google Scholar]
- 24.Xiu CY. Applied Analysis on Eye Drops in Beijing Tongren Hospital. Chinese Pharmaceutical affairs. 2011;25(2):205–209. [Google Scholar]
- 25.Yang H, Yu J, Zhang H. Determination of chloramphenicol residues in milk by gas chromatography-mass spectrometry. Chinese Journal of Health Laboratory Technology. 2006;16(11):1386–1387. [Google Scholar]
- 26.Li J, Shao B, Shen J, Wang S, Wu Y. Occurrence of chloramphenicol-resistance genes as environmental pollutants from swine feedlots. Environ Sci Technol. 2013;47(6):2892–2897. doi: 10.1021/es304616c. [DOI] [PubMed] [Google Scholar]
- 27.Ly CN, Pham JN, Badenoch PR, Bell SM, Hawkins G, Rafferty DL, McClellan KA. Bacteria commonly isolated from keratitis specimens retain antibiotic susceptibility to fluoroquinolones and gentamicin plus cephalothin. Clin Experiment Ophthalmol. 2006;34(1):44–50. doi: 10.1111/j.1442-9071.2006.01143.x. [DOI] [PubMed] [Google Scholar]
- 28.Tuft SJ, Matheson M. In vitro antibiotic resistance in bacterial keratitis in London. Br J Ophthalmol. 2000;84(7):687–691. doi: 10.1136/bjo.84.7.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grasbon T, Miño de Kaspar H, Klauss V. Coagulase-negative staphylococci in normal and chronically inflamed conjunctiva. Ophthalmologe. 1995;92(6):793–801. [PubMed] [Google Scholar]
- 30.Bosscha MI, van Dissel JT, Kuijper EJ, Swart W, Jager MJ. The efficacy and safety of topical polymyxin B, neomycin and gramicidin for treatment of presumed bacterial corneal ulceration. Br J Ophthalmol. 2004;88(1):25–28. doi: 10.1136/bjo.88.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baldo BA, Zhao Z, Pham NH. Antibiotic allergy: immunochemical and clinical considerations. Curr Allergy Asthma Rep. 2008;8(1):49–55. doi: 10.1007/s11882-008-0010-1. [DOI] [PubMed] [Google Scholar]
- 32.Tängdén T. Combination antibiotic therapy for multidrug-resistant Gram-negative bacteria. Ups J Med Sci. 2014;119(2):149–153. doi: 10.3109/03009734.2014.899279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hanet MS, Jamart J, Chaves AP. Fluoroquinolones or fortified antibiotics for treating bacterial keratitis: systematic review and meta-analysis of comparative studies. Can J Ophthalmol. 2012;47(6):493–499. doi: 10.1016/j.jcjo.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Jones RN, Barry AL, Thornsberry C, Gerlach EH, Fuchs PC, Gavan TL, Sommers HM. Ceftazidime, a pseudomonas-active cephalosporin: in-vitro antimicrobial activity evaluation including recommendations for disc diffusion susceptibility tests. J Antimicrob Chemother. 1981;8(Suppl. B):187–211. doi: 10.1093/jac/8.suppl_b.187. [DOI] [PubMed] [Google Scholar]
- 35.Eshraghi B, Masoomian B, Izadi A, Abedinifar Z, Falavarjani KG. Conjunctival bacterial flora in nasolacrimal duct obstruction and its changes after successful dacryocystorhinostomy surgery. Ophthal Plast Reconstr Surg. 2014;30(1):44–46. doi: 10.1097/IOP.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 36.Gündüz A, Gündüz A, Cumurcu T, Doganay V, Seyrek A. The conjunctival flora in vernal conjunctivitis patients. Ann Ophthalmol (Skokie) 2009;41(2):98–101. [PubMed] [Google Scholar]
- 37.Sharma S, Padhi TR, Basu S, Kar S, Roy A, Das T. Endophthalmitis patients seen in a tertiary eye care centre in Odisha: a clinico-microbiological analysis. Indian J Med Res. 2014;139(1):91–98. [PMC free article] [PubMed] [Google Scholar]
- 38.Yang JW, Choi JW, Lee SG, Kim DS. Antibacterial properties of artificial eyes containing nano-sized particle silver. Orbit. 2011;30(2):77–81. doi: 10.3109/01676830.2010.538123. [DOI] [PubMed] [Google Scholar]
- 39.Chaisathaphol T, Chayakulkeeree M. Epidemiology of infections caused by multidrug-resistant gram-negative bacteria in adult hospitalized patients at Siriraj Hospital. J Med Assoc Thai. 2014;97(3):35–45. [PubMed] [Google Scholar]