Abstract
Objective
To examine associations among pathological motivations for exercise with eating disorder (ED) specific health-related quality of life (HRQOL).
Method
Survey data assessing ED severity (i.e., Eating Disorder Diagnostic Survey), ED specific HRQOL (i.e., Eating Disorders Quality of Life Instrument), and pathological motivations for exercise (i.e., Exercise Dependence Scale) were collected from female students (N = 387) at seven universities throughout the United States. Regression analyses were conducted to examine the associations among exercise dependence, ED-specific HRQOL and ED severity, and the interaction of exercise dependence and ED severity on HRQOL scores.
Results
The overall model examining the impact of ED severity and exercise dependence (independent variables) on HRQOL (dependent variable) was significant and explained 16.1% of the variance in HRQOL scores. Additionally, the main effects for ED severity and exercise dependence and the interaction among ED severity and exercise dependence were significant, suggesting that the combined effects of ED severity and exercise dependence significantly impacts HRQOL.
Discussion
Our results suggest that pathological motivations for exercise may exacerbate ED’s detrimental impact on HRQOL. Our results offer one possible insight into why exercise may be associated with deleterious effects on ED HRQOL. Future research is needed to elucidate the relationship among psychological aspects of exercise, ED, and HRQOL.
Keywords: Exercise Dependence, Health-Related Quality of Life, Eating Disorders
Disease specific health-related quality of life (HRQOL) represents a disease or condition’s impact on the overall and specific areas of an individual’s health and well-being, yet it is often overlooked as an outcome when examining the impact of psychiatric disorders. Recent research on eating disorders (ED) and HRQOL has shown that both clinical and subclinical ED individuals have lower levels of HRQOL than normal controls. [1] Furthermore, the HRQOL detriments observed in ED are on par with the HRQOL detriments observed in other serious disorders (e.g., somatoform disorders, alcohol abuse, diabetes, cancer, & pulmonary disorders). [1] If the ED is left untreated HRQOL detriments may persist [2]; however, HRQOL improves as a result of ED treatment. [3,4] Thus, identifying behaviors that may contribute to the detrimental impact on HRQOL may elucidate potential pathways that, if intervened upon, could improve HRQOL.
Exercise is one behavior that is associated with earlier ED onset, more ED symptoms, and higher persistence of ED behavior. [5] Specifically, compulsions are one pathological motivation for exercise that has been associated with greater ED symptomatology (e.g., EDE global severity score, vomiting frequency, and depression). [6] Consequently, the distinction between exercise amount and pathological motivations is important in ED. [7,8]. One important limitation in synthesizing knowledge from studies that have examined pathological motivations for exercise is the use of multiple terms to describe problematic patterns of exercise. While compulsive exercise is the preferred term used in the ED literature [26], a recent literature review has concluded that terms such as exercise addiction, compulsion, and dependence all describe the same phenomenon. [27] Conceptualizing problematic exercise as exercise dependence addresses specific compulsive attitudes, motives, beliefs, and behaviors that are common to ED. Thus, recent research has shown that the detrimental effects of exercise on ED may be mediated by exercise dependence. [9,10] Moreover, exercise dependence is associated with detriments in psychological well-being and physical/cognitive well-being domains of ED-specific HRQOL. [11]
A recent review of HRQOL in ED concluded that motivations for exercising (e.g., exercise dependence) appear to predict HRQOL. [1] Previous research has found significant relationships for exercise dependence and psychological aspects of HRQOL on ED symptoms, [11] but has failed to investigate the main effects and interaction effect of ED severity and exercise dependence on total HRQOL scores. Therefore, continued examination of the association between exercise dependence and ED-specific HRQOL is warranted. The purpose of this study was to examine the unique and interactive effects of self-reported ED severity and exercise dependence on ED specific HRQOL. We hypothesized that ED severity will be more strongly associated with reduced HRQOL in individuals with higher levels of exercise dependence. [11]
Method
Procedure
All study procedures were reviewed and approved by the Institutional Review Board. Participants in this report were from a larger sample [11] examining the relationship between exercise, health, and psychological states. Participants were recruited from large lecture style classes from seven colleges and universities in the United States through announcements regarding a study. After completing the informed consent, the students were given a pen and paper survey to complete during class time. The survey took about 15 minutes to complete.
Participants
Participants were 387 female university students (M age = 20.11, SD = 2.21). For educational level, most of the women were sophomores (51.42%), followed by juniors (21.19%), seniors (16.54%), freshmen (9.30%), and graduate/professional (1.03%). The participants were mostly Caucasian (65.89%) followed by African-American (12.92%), Hispanic (8.53%), Asian (8.53%), and others (4.13%). Full threshold (i.e., met all diagnostic criteria) and subthreshold (i.e., at least one symptom was of sub-diagnostic severity) ED severity assessed by the Eating Disorder Diagnostic Scale [12,13] revealed rates of full threshold anorexia nervosa (1.30%), full threshold bulimia nervosa (3.37%), subthreshold anorexia nervosa (2.59%), and subthreshold bulimia nervosa (3.89%). Individuals with self-reported full and subthreshold anorexia nervosa and bulimia nervosa were collapsed into one ED group (n = 43) and compared with individuals without a self-reported eating disorder (n = 324). Binge eating disorder was excluded from these analyses because physical activity prevalence is low and may be uncorrelated with measures of eating disorders and psychological functioning in individuals with binge eating disorder. [14,25]
Measures
Demographic Questionnaire
The Demographic Questionnaire assessed the participant’s self-reported year in school, age, weight, height, and ethnicity.
Eating Disorder Diagnostic Scale (EDDS)
The EDDS [12,13] was used to determine ED symptoms and tentative diagnosis. The EDDS is a brief (i.e., 22 items) and psychometrically sound measure for assessing symptoms and diagnostic features of: (a) anorexia nervosa; (b) bulimia nervosa; and (c) binge eating disorder. Cronbach's α (alpha) was used to determine the scale’s internal consistency and provide an estimate of reliability. The EDDS reliability in this study was good (α = .85). The EDDs has shown high agreement with clinical interviews for the assessment of anorexia nervosa (κ = .93) and bulimia nervosa (κ = .81) [12]
Exercise Dependence Scale (EDS)
The EDS [15] is a 21-item measure assessing the physiological and psychological aspects of exercise dependence symptoms. Examples of items include: “I am unable to reduce how intense I exercise”; “I exercise to avoid feeling tense”; and “I exercise despite persistent physical problems”. Responses to the items are on a 6-point Likert scale ranging from 1 (never) to 6 (always). A lower score reveals less exercise dependence symptoms. Multiple validation studies and a recent literature review have concluded that the psychometric properties of this scale are good [15,16,27]. The EDS reliability in this study was excellent (α = .97).
The Eating Disorders Quality of Life Instrument (EDQOL)
The EDQOL [17] includes the following subscales: psychological, physical/cognitive, financial, work/school, and a total score. The EDQOL is 25 item scale and it is more sensitive to ED-specific aspects of HRQOL than generic measures of HRQOL. Subscale and total scores may range from 0–4, with a lower score indicating better QOL. The EDQOL reliability in this study was excellent (α = .94).
Leisure-time Exercise Questionnaire (LTEQ)
The LTEQ is a self-report of the frequency and duration that an individual engages in strenuous, moderate, and mild bouts of exercise during a typical week. [21] Each of the intensity scores are converted into metabolic equivalents (METS; [Mild × 3] + [Moderate × 5] + [Strenuous × 9]) and summed to provide an estimate of total METS expenditure from exercise for an average week. The LTEQ is a valid and psychometrically sound measure that is frequently used to assess exercise behavior. The MET values for the LTEQ are based on published reports of its validity [21,22], and this measure is considered the gold standard for self-report exercise assessment. [23] Consistent with previous research protocols, minutes engaged in mild exercise were not used in these analyses, but the category was included in the questionnaire to ensure that participants did not report mild exercise minutes in the moderate intensity category. [24]
Statistical Analysis
“First, we centered the EDS scores and calculated an interaction variable for EDS and ED status. Next, an ordinary least squares regression (OLS) analyses was used to examine the associations among exercise dependence and ED severity on HRQOL. The interaction effect was examined because we were particularly interested in examining the moderating influence of exercise dependence on the relationship between ED severity and HRQOL.”
Results
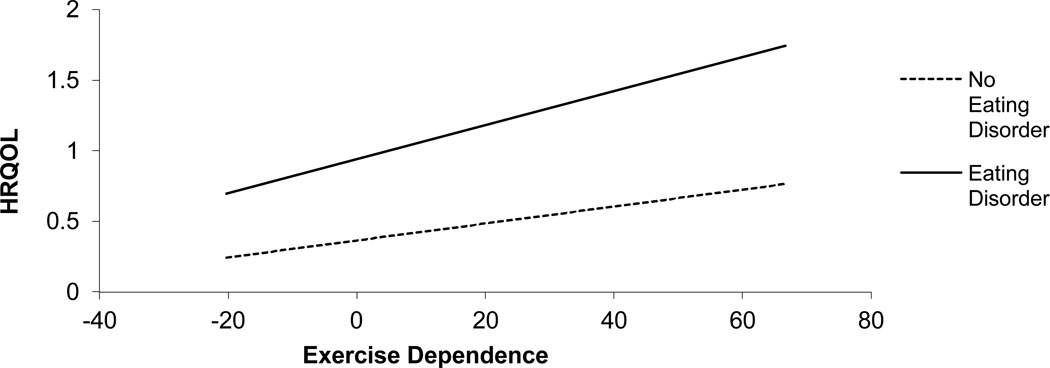
ED severity (ED vs nonED) was determined by scores on the EDDS. That is, the EDDS algorithm [13] was followed to categorize participants into ED or nonED groups based on symptom severity. Therefore, these analyses take into account ED severity. Exercise dependence symptoms were measured by the EDS (M = 41.31, SD = 16.90) and ED-specific HRQOL was measured by the EDQOL total score (M = 0.40, SD = 0.45). The means and standard deviations for the EDS, EDQOL, and LTEQ for the ED and nonED groups are reported in table 1. To our knowledge, EDS assessments of ED individuals have not been previously reported. Our nonED group’s mean of 40.40 (SD = 15.70) is similar to a mean of 40.63 (SD = 13.09) that has been reported in a previous study using the EDS to assess a nonED college sample [9]. With regards to the EDQOL, the ED group (M = 0.77, SD = 0.65) in our study reported scores that are in between scores previously reported by ED individuals with minor symptom severity (M = 0.53, SD = 0.44) and moderate severity symptoms (M = 1.29, SD = 0.54) and the nonED group (M = 0.35, SD = 0.40) in our study reported slightly lower scores than previously reported scores in nonED individuals (M = 0.42, SD = 0.34) [17]. The overall model examining the impact of ED and exercise dependence (independent variables) on HRQOL (dependent variable) was significant [F(3,374) = 24.92, p < .001] and explained 16.1% of the variance in HRQOL scores (R2 = .097). ED severity (β = .396, p = .001) as well as higher exercise dependence scores (β = .231, p = .001) both predicted more HRQOL detriments. (see Figure 1) Additionally, the interaction among ED and exercise dependence was significant (β = .187, p = .040) suggesting that the combined effects of ED and exercise dependence significantly impacts HRQOL. Thus, individuals with ED and higher exercise dependence scores may experience more HRQOL detriments as compared to individuals without an ED and with low exercise dependence scores.
Table 1.
Means (standard deviations) for study measures by group
| Measure | Eating Disorders (n=43) |
No Eating Disorders (n=324) |
Group Comparisons* |
|---|---|---|---|
| Exercise Dependence Scale | 48.56 (23.46) | 40.20 (15.57) | p = .03 |
| Eating Disorders Diagnostic Scale | 25.67 (15.68) | 14.19 (10.38) | p < .01 |
| Eating Disorders Quality of Life Instrument | 0.77 (0.65) | 0.33 (0.39) | p < .01 |
| Leisure-time Exercise Questionnaire | 33.79 (27.30) | 30.59 (23.42) | p = .47 |
Independent samples t tests were used to compare eating disorder and no eating disorder groups.
Figure 1. Association between exercise dependence and health-related quality of life (HRQOL) detriments for eating disorder and no eating disorder groups.
Regression lines depict the association of exercise dependence and health-related quality of life (HRQOL) detriments. Increased HRQOL scores indicate more detriments. Exercise dependence is associated with HRQOL detriments for all groups, but this effect is more pronounced when exercise dependences occurs with an eating disorder. The significant interaction effect of these regressions indicates that motives (i.e., exercise dependence) may detrimentally affect daily functioning/HRQOL, particularly for those who have an ED.
Discussion
The purpose of our study was to examine the association among ED, exercise dependence, and HRQOL. Consistent with our hypothesis, we found that both ED and exercise dependence may impact HRQOL and that ED and exercise dependence also interact to further adversely impact HRQOL. These results suggest that pathological motivations for exercise may exacerbate the detrimental impact of ED on HRQOL. Thus, our results offer insights into why exercise behavior may be associated with deleterious effects on HRQOL in ED. [18]
Our finding of an interaction effect among ED and exercise dependence on HRQOL is important for at least three reasons. First, understanding of the psychological aspects of exercise in ED is limited despite clinical reports and research suggesting that compulsively exercising ED individuals present more severe symptomatology [6] and higher persistence of ED behavior [5]. Thus, the interaction effect observed in our study indicates that motives (i.e., exercise dependence) may detrimentally affect daily functioning/HRQOL particularly for those who have an ED. Our finding that exercise dependence in the absence of ED is also associated with HRQOL detriments suggests that pathological motivations toward exercise, but not exercise amount, may be of interest for further research. [7] Second, our results support previous recommendations to also examine psychological aspects of exercise as these may be markedly more influential than examining only exercise amount or frequency. [7,8, 19] Finally, the use of HRQOL as an outcome variable, rather than the presence of ED or ED symptom severity, further describes the scope of impairment associated with exercise in ED. Thus, our findings of an interaction between ED and exercise dependence suggests that future research examining the impact of psychological aspects of exercise in ED may be fruitful.
Our study highlights several areas for future investigation; however, limitations were present. First, ED was assessed through a self-report measure in a sample of female college students that may not be representative of all variants of ED, allow insights regarding exercise dependence and the severity of ED, provide a clinical diagnosis of ED, or allow examinations of gender differences. Moreover, validation research has concluded that the sensitivity for the EDDS indicates that some individuals with bulimia nervosa may not have been identified. [12] Second, our small sample size did not allow for comparisons between ED variants. This is important because previous research has demonstrated a wide range of compulsive exercise prevalence among ED diagnoses. [5] Finally, our cross-sectional design precludes causal inference into the relationships among exercise dependence, ED, and HRQOL. Thus, our results should be interpreted with caution.
Our study represents an initial attempt to explore the relationships among exercise motives, ED severity, and HRQOL. Our finding of an interaction between ED severity and exercise dependence on HRQOL detriment severity suggest that future research is encouraged to continue to examine psychological aspects of exercise (i.e., exercise dependence; exercise compulsion; obligatory exercise) in ED. [8–10] Moreover, these data were collected as part of a larger study that did not assess other relevant ED-related variables (e.g. affect comorbidities such as depression and anxiety), nor did we address the effect of exercise dependence on HRQOL in relation to previous or current ED treatment. Future research is encouraged to examine the impact of exercise dependence on ED severity, treatment, and possible differences among ED diagnosis. [20] Thus, our results indicate that future research is needed to further elucidate the relationship among psychological aspects of exercise, ED, and HRQOL.
References
- 1.Engel SG, Adair CE, Las Hayas C, Abraham S. Health-related quality of life and eating disorders: A review and update. International Journal of Eating Disorders. 2009;42:179–187. doi: 10.1002/eat.20602. [DOI] [PubMed] [Google Scholar]
- 2.Mitchison D, Hay P, Slewa-Younan S, Mond J. Time trends in population prevalence of eating disorder behaviors and their relationship to quality of life. PlosOne. 2012;7(11):1–7. doi: 10.1371/journal.pone.0048450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munoz P, Quintana JM, Las Hayas C, Padierna A, Aguirre U, González-Torres MA. Quality of life and motivation to change in eating disorders. Perception patient-psychiatrist. Eating behaviors. 2012;13:131–134. doi: 10.1016/j.eatbeh.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 4.Watson HJ, Allen K, Fursland A, Bryne SM, Nathan PR. Does enhanced cognitive behavior therapy for eating disorders improve quality of life? European Eating Disorders Review. 2012;20:393–399. doi: 10.1002/erv.2186. [DOI] [PubMed] [Google Scholar]
- 5.Shroff H, Reba L, Thornton LM, Tozzi F, Klump K, Berrettini WH, Brandt H, Crawford S, Crow S, Fichter MM, Goldman D, Halmi K, Johnson C, Kaplan AS, Keel P, LaVia M, Mitchell J, Rotondo A, Strober M, Treasure J, Woodside DB, Kaye WH, Bulik CM. Features associated with excessive exercise in women with eating disorders. International Journal of Eating Disorders. 2006;39:454–461. doi: 10.1002/eat.20247. [DOI] [PubMed] [Google Scholar]
- 6.Stiles-Shields EC, Goldschmidt AB, Boepple L, Glunz C, LeGrange D. Driven exercise among treatment-seeking youth with eating disorders. Eating Behaviors. 2011;12:328–331. doi: 10.1016/j.eatbeh.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adkins CE, Keel PK. Does “excessive” or “compulsive” best describe exercise as a symptom of bulimia nervosa? International Journal of Eating Disorders. 2005;38:24–29. doi: 10.1002/eat.20140. [DOI] [PubMed] [Google Scholar]
- 8.Meyer C, Taranis L. Exercise in eating disorders: Terms and definitions. European Eating Disorders Review. 2011;19:169–173. doi: 10.1002/erv.1121. [DOI] [PubMed] [Google Scholar]
- 9.Cook BJ, Hausenblas HA. The role of exercise dependence for the relationship between exercise behavior and eating pathology: Mediator or Moderator? Journal of Health Psychology. 2008;13:495–502. doi: 10.1177/1359105308088520. [DOI] [PubMed] [Google Scholar]
- 10.Cook B, Hausenblas H, Crosby RD, Cao L, Wonderlich SA. Exercise dependence as a mediator of the exercise and eating disorders relationship: A pilot study. doi: 10.1016/j.eatbeh.2014.10.012. (under review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook BJ, Hausenblas HA. Eating disorder specific health-related quality of life and exercise in college females. Quality of Life Research. 2011;20:1385–1390. doi: 10.1007/s11136-011-9879-6. [DOI] [PubMed] [Google Scholar]
- 12.Stice E, Telch CF, Rizvi SL. Development and validation of the eating disorder diagnostic scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment. 2000;12:123–131. doi: 10.1037//1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- 13.Stice E, Fisher M, Martinez E. Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- 14.Hrabosky JI, White MA, Masheb RM, Grilo CM. Physical activity and its correlates in treatment-seeking obese patients with Binge Eating Disorder. International Journal of Eating Disorders. 2007;40:72–76. doi: 10.1002/eat.20323. [DOI] [PubMed] [Google Scholar]
- 15.Hausenblas HA, Symons Downs D. How much is too much? The development and validation of the exercise dependence scale. Psychology & Health. 2002;17:387–404. [Google Scholar]
- 16.Symons Downs D, Hausenblas H, Nigg C. Factorial validity and psychometric examination of the exercise dependence scale- revised. Measurement in Physical Education and Exercise Science. 2004;84:183–201. [Google Scholar]
- 17.Engel SG, Wittrock DA, Crosby RD, Wonderlich SA, Mitchell JE, Kolotkin RL. Development and psychometric validation of an eating disorder-specific health-related quality of life instrument. International Journal of Eating Disorders. 2006;39:62–71. doi: 10.1002/eat.20200. [DOI] [PubMed] [Google Scholar]
- 18.Mond J, Myers TC, Crosby R, Hay P, Mitchell J. Excessive exercise’ and eating-disordered behavior in young adult women: Further evidence from a primary care sample. European Eating Disorders Review. 2008;16:215–221. doi: 10.1002/erv.855. [DOI] [PubMed] [Google Scholar]
- 19.Hausenblas HA, Cook BJ, Chittester NI. Can exercise treat eating disorders? Exercise and Sport Sciences Reviews. 2008;36:43–47. doi: 10.1097/jes.0b013e31815e4040. [DOI] [PubMed] [Google Scholar]
- 20.Dalle Grave R, Calugi S, Marchesini G. Compulsive exercise to control shape or weight in eating disorders: Prevalence, associated features, and treatment outcome. Comprehensive Psychiatry. 2008;49:346–352. doi: 10.1016/j.comppsych.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Godin G, Shephard RJ. Godin Leisure-Time Exercise Questionnaire. Medicine and Science in Sports and Exercise. 1997;29:S36–S38. [Google Scholar]
- 22.Jacobs DR, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of ten commonly used physical activity questionnaires. Medicine & Science in Sports & Exercise. 1993;25:81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Courneya KS, Jones LW, Rhodes RE, Blanchard CM. Effect of response scales on self-reported exercise frequency. American Journal of Health Behavior. 2003;27:613–622. doi: 10.5993/ajhb.27.6.4. [DOI] [PubMed] [Google Scholar]
- 24.Haskell WL, Lee I, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health. Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 25.Goldschmidt AB, Le Grange D, Powers P, Crow SJ, Hill LL, Peterson CB, Crosby RD, Mitchell JE. Eating disorder symptomatology in normal-weight vs. obese individuals with binge eating disorder. Obesity. 2011;19(7):1515–1518. doi: 10.1038/oby.2011.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer C, Taranis L. Exercise in the eating disorders: Terms and definitions. European Eating Disorders Review. 2011;19:169–173. doi: 10.1002/erv.1121. [DOI] [PubMed] [Google Scholar]
- 27.Berczik K, Szabó A, Griffiths MD, Kurimay T, Kun B, Urbán R, Demetrovics Z. Exercise addiction: Symptoms, diagnosis, epidemiology, and etiology. Substance use & Misuse. 2012;47:403–417. doi: 10.3109/10826084.2011.639120. [DOI] [PubMed] [Google Scholar]