Abstract
Perceived risk for disease is included as a predictor of intentions and behavior in many health behavior theories. However, perceived risk is not always a strong predictor of intentions and behaviors. One reason may be suboptimal conceptualization and measurement of risk perceptions; in particular, research may not capture the conviction and certainty with which a risk perception is held. The rich and independent literature on attitudes might be leveraged to explore whether conviction is an important moderator of the effects of risk perceptions on intentions and behavior. Attitudes are more predictive of intentions when they are high in multiple aspects of attitude strength, including attitude certainty and being more accessible and stable over time. Working from the assumption that risk perceptions have a similar structure and function to attitudes, we consider whether factors known to strengthen the attitude-behavior correspondence might also strengthen the risk perception-behavior correspondence. Although by strict definition risk perceptions are not evaluations (a critical component of attitudes), the predictive validity of risk perceptions may be increased by attention to one’s “conviction” or certainty of perceived risk. We also review recent strategies designed to improve risk perception measurement, including affective and experiential assessments of perceived risk and the importance of allowing people to indicate that they “don’t know” their disease risk. The aim of this paper is to connect two disparate literatures—attitudes and persuasion in social psychology with risk perceptions in health psychology and decision science—in an attempt to stimulate more work on characteristics and proper measurement of risk perceptions.
Introduction
Why would someone decide to wear sunscreen? One primary reason is a belief that one is at risk for and could actually get skin cancer. Researchers tend to expect that this perceived risk should predict whether someone engages in a behavior that might decrease that risk. However, people may be unsure of their risk or may consider it impossible to know whether they will develop a disease (Hay, Shuk, Cruz, & Ostroff, 2005; Hay et al., 2014). This uncertainty may be consequential, because when people are uncertain about their disease risk, their responses to questions assessing perceived risk should be less likely to predict performance of important prevention and screening behaviors.
When people are uncertain about their disease risk, their responses on surveys may not represent their true beliefs. Consider a typical risk perception question: “How likely are you to get skin cancer in your lifetime?” People who are uncertain may select a response indicating their best guess, yet one they do not strongly endorse. Alternately, they could skip the question entirely or select “don’t know” if that is an option, probably resulting in exclusion from data analyses (Waters, Hay, Orom, Kiviniemi, & Drake, 2013). They may select 50% if offered a percentage scale, a response that may simply represent belief in an uncertain “50-50” chance (Bruine de Bruin & Carman, 2012; Bruine de Bruin, Fischhoff, Millstein, & Halpern-Felsher, 2000; Fischhoff & Bruine De Bruin, 1999). People also tend to consider hazard risks anywhere between 20% and 80% to be essentially equivalent (Cameron, Sherman, Marteau, & Brown, 2009). To address these issues, there is growing interest in identifying novel ways of measuring disease risk perceptions to improve how well the construct of perceived risk predicts behavior. We present a new approach aimed at assessing “risk perception conviction” (“risk conviction” in short), or the subjective sense that one knows what one’s risk belief is and confidence that this risk belief is accurate. We argue that “conviction” about the degree of one’s risk may matter as much or more than actual risk perceptions. This novel “risk conviction” approach is informed by research on attitude strength and certainty that emerged from the field of social psychology. We discuss two possible ways to use risk conviction assessments: 1) assessing risk conviction as a characteristic of risk perceptions, and 2) assessing risk conviction as an alternative to traditional risk perception items. We review other novel approaches to assessing disease risk perceptions and discuss how the risk conviction approach is both complementary to and distinct from these approaches.
Prior Research on Disease Risk Perceptions
Perceived disease risk, also referred to as perceived likelihood, susceptibility or vulnerability, is a predictor of intentions and behavior in many health behavior theories (Ferrer & Klein, 2015), including the Health Belief Model (Rosenstock, 1990) and the Parallel Processing Model (Witte, 1992). These theories posit that people who believe they are at higher risk for disease will be more likely to engage in health behaviors to mitigate this risk. Consequently, many risk communication strategies are aimed at increasing perceived risk. However, one meta-analysis found that increasing perceived risk experimentally had only a small effect on intentions and health behaviors, although the effect was enhanced when response efficacy and self-efficacy were also increased (Sheeran, Harris, & Epton, 2014). Risk perceptions are often modestly (or not at all) associated with intentions and behavior, as demonstrated by multiple meta-analyses that included observational and descriptive studies (Brewer et al., 2007; Gerrard, Gibbons, & Bushman, 1996; McCaul, Branstetter, Schroeder, & Glasgow, 1996).
There are multiple reasons for the low correspondence between risk perceptions and behavior. Some behaviors – such as sexual behavior and smoking – may result from factors such as appetitive drive rather than cognitive factors such as perceived risk (Gerrard et al., 1996). Additionally, risk perceptions are often deductive judgments that are influenced by self-esteem and global self-evaluations rather than a reasoned consideration of personal risk factors (Klein & Monin, 2009; Klein, Blier, & Janze, 2001). In other words, people may rate their risk for disease as lower when they feel good about themselves, and higher when they feel worse about themselves. A third reason is that correlations between risk perceptions and behavior are difficult to interpret; behavior may alter risk perceptions rather than the reverse (Weinstein, Rothman, & Nicolich, 1998). Although this is less of a problem for experimental studies, it is nevertheless very difficult to change risk perceptions (Weinstein & Klein, 1995), and post-manipulation risk perceptions may simply be a by-product of a priori risk perceptions. Finally, many perceived risk measures do not account for whether individuals plan to engage in risk-reducing behavior, making it difficult to know what assumptions people make when reporting their risk (Ronis, 1992). For example, irrespective of their current smoking behavior, young smokers who plan to quit may believe they are at low risk for lung cancer.
We consider another explanation – namely, that risk perceptions are often not held with conviction or certainty, and do not fully capture the way that people think about risk. When people are uncertain of what their beliefs are and whether these beliefs are accurate, risk perceptions are unlikely to be particularly strong predictors of behavior.
Attitude Strength
Just as risk perceptions often weakly predict behavior, researchers have long recognized that attitudes are often not strong predictors of behavior (see, for example Glasman & Albarracín, 2006; LaPiere, 1934; Wicker, 1969). Importantly, attitudes are more predictive of both intentions and behavior when the attitudes have certain characteristics, including being held with greater certainty and being more accessible and stable over time (Cooke & Sheeran, 2004; Glasman & Albarracín, 2006; Kraus, 1995). The greater attitude-behavior correspondence when attitude certainty is higher is due to increased attitude stability (Glasman & Albarracín, 2006). Researchers have generally not applied insights from this research to the conceptualization or measurement of risk perceptions (but see Fischhoff & Bruine De Bruin, 1999).
Attitudes are preferences or evaluations of an object indicating some degree of favor or disfavor (Banaji & Heiphetz, 2010; Eagly & Chaiken, 1993, 1998). For example, “I hate snakes” is an attitude. Attitude strength is one dimension of attitudes, defined as the “extent to which attitudes manifest the qualities of durability and impactfulness” (Krosnick & Petty, 1995, p. 3). Attitude certainty is one dimension of attitude strength that we believe could be particularly informative with respect to risk perceptions, because as we will argue there are many reasons people may be uncertain of their disease risk. In addition to certainty, stronger attitudes are higher in accessibility, extremity, importance or centrality, and consistency (see definitions in Table 1), and thus measuring these factors as moderators of the association between risk perceptions and behavior might also improve the predictive validity of perceived risk.
Table 1.
Dimensions of attitude strength that may inform measurement of risk perceptions
| Dimension of attitude strength | Definition in attitude literature | Application to risk perception measurement | Hypotheses concerning risk perceptions |
|---|---|---|---|
| Certainty | “The subjective sense of conviction one has about one’s attitude, or the extent to which one is confident or sure of one’s attitude” (Tormala & Rucker, 2007) | Conviction about one’s personal risk for disease could be measured and treated as either a moderator of perceived risk or alternative to perceived risk items. | See Table 3 |
| Accessibility | “The strength of the object-evaluation link” which is manifested as “the ease with which an attitude comes to mind” (Krosnick & Petty, 1995, p. 6) | Accessibility about perceived risk could be assessed by asking people how frequently they have thought about a particular disease or their likelihood of getting it (Windschitl, 2003), or by asking about “preoccupation with thoughts about risk” (Weinstein, 2003). The potential application of attitude accessibility to risk perception measurement has been previously identified (see Windschitl, 2003) but does not seem to have been extensively pursued. | Risk perceptions that are higher in accessibility should be more predictive of behavior. |
| Extremity | “The extent to which the attitude deviates from neutrality” (Krosnick & Petty, 1995, p. 6); in other words, the positivity or negativity of an attitude. | Extremity of risk perceptions could be determined by assessing the extent to which perceived risk deviates from the midpoint of the response scale. At their most extreme (e.g., 0% or 100%), risk perceptions should be held with substantial certainty. However, individuals who believe their risk to be intermediate may feel very confident that this is the case or they may pick an intermediate degree of risk because they are uncertain of their risk. | Risk perceptions that are more extreme may be more predictive of behavior, to the extent that extreme risk perceptions are also held with greater conviction. We expect that risk conviction should be more useful to measure than risk extremity. |
| Importance | “The degree of psychological significance people attach to an attitude” and a “manifestation of the degree of personal relevance of the attitude object” (Krosnick & Petty, 1995, p. 7). | A potentially related construct in the health domain is illness centrality, which has been measured as the extent to which people “define themselves in terms of their illness” (Helgeson & Novak, 2007, p. 260). This construct refers to people who have an illness. Future research on illness centrality may benefit from applying lessons learned from research on attitude importance. | Perceived risk may be more likely to predict behavior when a disease is more central to one’s sense of self, for example when people have a family history of disease. For individuals who do not yet have a disease, risk importance or illness centrality (adapted for individuals without disease) could be measured for multiple diseases, which might indicate whether risk perceptions are likely to predict health behaviors for a particular individual. |
Attitude certainty is “the subjective sense of conviction one has about one’s attitude, or the extent to which one is confident or sure of one’s attitude” (Tormala & Rucker, 2007; see also Abelson, 1988; Gross, Holtz, & Miller, 1995 for earlier conceptualizations). Attitude certainty is a meta-cognitive aspect of attitudes because it is a subjective understanding of one’s attitude, distinct from whether the attitude is objectively correct (Tormala & Rucker, 2007). Attitude certainty consists of two dimensions (Petrocelli, Tormala, & Rucker, 2007; Tormala & Rucker, 2007). Attitude correctness refers to confidence that one’s attitude is “correct, valid, or justified” (Petrocelli et al., 2007, p. 31). Attitude clarity refers to “the subjective sense that one knows what one’s attitude really is” (Petrocelli et al., 2007, p. 30). The dimensions of correctness and clarity can be assessed with items such as “How certain are you that your attitude toward capital punishment is the correct attitude to have?” and “To what extent is your true attitude toward capital punishment clear in your mind?”, respectively (Petrocelli et al., 2007).
What is Risk Perception Conviction?
We propose that measuring “risk perception conviction” could improve conceptualization and measurement of risk perceptions. As previously noted, we define risk perception conviction as the subjective sense that one knows what one’s risk belief is, as well as confidence that this risk belief is accurate. We contend that risk perceptions share many of the same properties as attitudes and could be evaluated on many of the same dimensions, although we note two specific distinctions between these constructs. Risk perceptions are not, by definition, attitudes; rating how likely one is to get a disease is not an evaluation indicating favor or disfavor. Another distinction is that risk perceptions can (in theory) be evaluated for accuracy, whereas attitudes are typically correct only by virtue of agreement with others or strength of evidence supporting an attitude, as indicated by items used to measure attitude correctness (Petrocelli et al., 2007). It is unlikely that these differences would limit the ability to extrapolate research on attitudes to that on risk perceptions.
The consideration of conviction with respect to perceived risk is not entirely new. Over 10 years ago, Weinstein (2003) used the word “conviction” with respect to risk perceptions: “In addition to what people state about their beliefs [about their disease risk], are there degrees of conviction that need to be recognized?” Despite this foreshadowing in language, Weinstein’s conceptualization seems to refer to whether risk judgments are based on experience, and to the distinctions among cognitions versus feelings about vulnerability to disease (an approach utilized in Weinstein et al., 2007 that we discuss later). Additionally, Fischhoff and colleagues (1999) have assessed confidence about risk perceptions, but this approach is infrequently taken.
A note on terminology
Certainty, conviction, and confidence are often used interchangeably in the attitude literature, although attitude certainty is used most commonly (see Gross et al., 1995 for a list of synonyms). We carefully selected the term “risk conviction” because we expect it to be less confusing than the term “risk certainty.” When rating perceived risk, a person is in many respects rating the certainty that an outcome will occur. This is evident, for example, by the response options on some risk perception scales that range from “almost zero” or “impossible” to “almost certain” (see, for example Dillard, Ferrer, Ubel, & Fagerlin, 2012; Windschitl & Wells, 1996). Thus, certainty could be a synonym of perceived risk as well as a characteristic of perceived risk. We chose conviction because it does not have multiple meanings in this context, whereas certainty does.
How do people become certain of their perceived risk for disease?
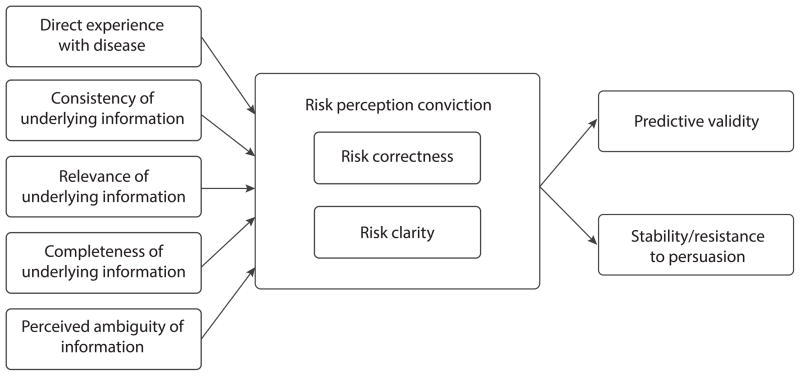
The attitude literature provides insights into when and why people should be more certain about their perceived risk for disease (Gross et al., 1995; Rucker, Tormala, Petty, & Briñol, 2014; Tormala & Rucker, 2007). We highlight several antecedents of attitude certainty that may be particularly relevant to risk perception conviction: direct experience, and greater consistency, relevance, and completeness of the information (e.g., information about risk factors) used to generate the belief (Figure 1).
Figure 1.
Hypothesized antecedents and consequences of risk perception conviction
First, risk perceptions might be held with greater conviction if an individual’s experience with disease is direct (e.g., caring for a family member during a diagnosis) rather than indirect (e.g., hearing about a diagnosis second-hand). More direct and greater experiences have been posited as antecedents of attitude certainty, likely because they result in greater knowledge (Gross et al., 1995; Rucker et al., 2014; Tormala & Rucker, 2007; see for example, Fazio & Zanna, 1978).
Next, risk conviction should be higher when all risk factors consistently confer either increased or decreased risk; a person at elevated genetic risk for melanoma who has a low-risk phenotype (e.g., dark hair, no moles) may have less conviction than a person with elevated genetic risk and a high-risk phenotype. When people have information about an attitude object that is “evaluatively congruent”—this is, all positive or all negative—they have greater attitude certainty (Rucker et al., 2014; see for example, Smith, Fabrigar, MacDougall, & Wiesenthal, 2008).
Risk conviction should also be higher when individuals understand which risk factors are relevant to disease (e.g., knowledge that UV exposure is a risk factor for skin cancer), and thus can evaluate how these risk factors relate to their own risk. If people think their attitudes are based on relevant information, they are posited to have greater attitude certainty (Rucker et al., 2014).
If people are given a risk estimate, risk conviction should be higher when people believe their risk estimate is complete, for example if it encompasses multiple risk factors or if one factor is completely deterministic (such as genetic risk information for Huntington disease). Indeed, people often disbelieve output from risk calculators if factors such as their prior behavior do not appear to have been considered (Scherer et al., 2013). Completeness is posited to be relevant to attitude certainty because it suggests that there are fewer unknown factors that could change one’s attitude (Rucker et al., 2014). In general, by drawing on the previously identified antecedents of attitude certainty, predictions can be made about factors that will be associated with greater risk conviction.
Perceived ambiguity of any information about one’s risk may also influence risk conviction (Gross et al., 1995). Ambiguity refers to uncertainty arising from limitations in the reliability, credibility, or adequacy of information (Ellsberg, 1961; Han, Klein, & Arora, 2011). If people think experts do not have accurate information about their risk, they should have lower risk conviction. For example, if people receive ambiguous information involving a range of probabilities (e.g., “Your risk for bladder cancer is between 10% to 25%”) they should perceive the information to be less legitimate and accurate, and thus have less risk conviction.
Risk conviction as a dimension of perceived risk
Risk conviction might be measured and used in two different ways: as a moderator designed to accompany assessments of perceived risk or as an alternative to existing measures of perceived risk. We discuss each possibility in turn.
One approach is to measure both perceived risk and risk perception conviction and to look at the interactive effects of these constructs. Attitudes held with greater certainty are more stable and persistent, more resistant to persuasive attacks, and show greater correspondence with behavior (Abelson, 1988; Cooke & Sheeran, 2004; Glasman & Albarracín, 2006; Gross et al., 1995; Kraus, 1995; Tormala & Rucker, 2007; Figure 1). These data suggest that risk perceptions will be more predictive of intentions and behaviors for people with greater risk conviction. Because risk perceptions are difficult to change in the long term (Aspinwall, Taber, Kohlmann, Leaf, & Leachman, 2014; Dieng et al., 2014), by measuring risk conviction as a moderator we might also be able to better predict whether and for whom risk perceptions are likely to change following health communications targeting perceived risk. People with less risk conviction should be more responsive to these interventions.
Researchers could also assess risk correctness and clarity, consistent with the approach taken in the attitude literature. However, what would it mean to say that one’s perceived risk (and especially one’s feeling of vulnerability) is correct? In the attitude literature, attitudes are deemed “correct” when other people agree (Petrocelli et al., 2007). In the case of diesease risk, the objective estimate is the number that would be given by a medical professional or risk calculator. However, people may not think these estimates are accurate if they believe disease risk is unknowable or that medical professionals do not have enough information to provide risk estimates. Indeed, people often disagree with objective risk estimates such as those provided through genetic testing (Aspinwall et al., 2014), determined through risk assessment tools (Scherer et al., 2013), or obtained through laboratory tests (Jemmott, Ditto, & Croyle, 1986). This may be due to reasoned, potentially rational responses (i.e., “I plan to quit smoking, so my lung cancer risk is not so high”) or to more defensive processes aimed to minimize risk (McQueen, Vernon, & Swank, 2012; van‘t Riet & Ruiter, 2013). Thus, asking people whether they think their perceived risk aligns with such information may not truly measure perceived risk correctness. With these considerations, an item used to assess risk correctness might be:
Consider your response to [the perceived risk question]. How certain are you that this belief would be similar to what you might learn from a calculator that takes into account every factor that determines how likely you are to get cancer in your lifetime (for example, your past and future behavior, your genetics, your environment, and/or any other factors you might think are important)?
Risk clarity, or the extent to which people believe their perceived risk is clear in their mind, should be more straightforward to assess. One might ask, “Consider your response to [the perceived risk question]. To what extent is this belief clear in your mind?”
Measuring risk conviction as an alternative to perceived risk
Perceived risk estimates are susceptible to contextual factors and often constructed ad-hoc (Windschitl, 2002) based on overall self-evaluations of the self rather than a deliberate consideration of one’s risk factors (Klein et al., 2001). Moreover, perceptions of either low risk or high risk could lead to the identical behavior for different reasons (Lipkus & Klein, 2006). Thus, in addition to measuring conviction as a moderator, another possible approach is to replace conventional risk perception measures with alternative measures of conviction. Hypotheses as to how risk conviction might have main effects on three types of health behaviors (i.e., screening to determine disease risk, screening to determine presence/absence of illness, and prevention behaviors) are outlined in Table 2. If people are certain of their risk, they should be less likely to engage in risk predictive screening tests such as cholesterol tests because they already hold risk beliefs high in certainty and do not require additional information. In the case of screening for the absence/presence of disease, people certain of their low risk may screen for reassurance, whereas people certain of their high risk may screen to identify disease so they can then act appropriately on the information. Indeed, one study showed that people told they were either at low or high risk for colorectal cancer were more likely than controls to intend to get a screening test (Lipkus & Klein, 2006). Conversely, prevention behaviors such as aspirin use to reduce stroke risk may not be predicted better by risk perception than by risk conviction, because what matters more in driving these behaviors may be believing oneself to be at high risk. These hypotheses represent important avenues for future research, as little data exists as to whether and for what behaviors risk conviction may be a stronger predictor of health behaviors than risk perceptions.
Table 2.
Predicted associations of risk conviction with different types of health behaviors, if risk conviction were measured as an alternative to perceived risk
| Type of health behavior | Examples of behavior | Predictions for people with low risk conviction | Predictions for people with high risk conviction | Caveats |
|---|---|---|---|---|
| Screening to determine disease risk | Predictive genetic testing, cholesterol screening, blood pressure screening | Those with low risk conviction will be more likely to obtain screening so they can learn additional risk information because they are uncertain about their degree of risk | Those with high risk conviction will be less likely to obtain screening to learn additional risk information. If they are certain their risk is either high or low, then there is no need to obtain screening to learn whether risk is high or low. | This association may depend on the reason for low risk conviction. If people have low risk conviction because they don’t understand risk factors, they may not have the knowledge to understand what type of screening to seek. |
| Screening to determine presence or absence of disease | Mammography, colonoscopy, clinical or self-skin examination | Those with low risk conviction will be less likely to obtain screening, particularly if fearful of information that might be obtained. | Those with high risk conviction will be more likely to obtain screening. If they are certain their risk is low, then there is no need to be fearful of information that might be obtained. If they are certain their risk is high, then screening will be more likely to be useful. | This association may depend on the extent to which individuals express worry or fear about learning risk information, or they extent to which they typically avoid health information for these reasons. |
| Prevention | Sunscreen use, aspirin use, radon testing | Those with low risk conviction may be less likely to engage in prevention behaviors if the reason for the low risk conviction is lack of prior thought about the relevant disease. | People who are certain their risk is low may not engage in prevention behaviors if they think it is unnecessary, or they may be certain their risk is low precisely because they already engage in prevention behaviors. Conversely, people who are certain their risk is high may engage in more prevention behaviors because they think it is necessary, or they may be certain their risk is high precisely because they do not engage in prevention behaviors. As such, for prevention behaviors we do not think there would be a direct association between risk conviction and behavior, and risk perception itself would be more predictive. | The association of risk conviction with prevention behaviors may depend on whether the research conducted is cross-sectional (in which case risk perceptions may be a result of engagement in prevention behaviors) or prospective/longitudinal (in which risk conviction may predict behavior). |
Complementary but Distinct Approaches to Improving Risk Perception Measurement
For some time now, researchers have recognized various limitations of survey items assessing perceived risk. For example, people’s ratings of their perceived risk using numeric probability scales ranging from 0 to 100% risk are less predictive of intentions than verbal response scales ranging from “certain” to “impossible” (Windschitl & Wells, 1996). These researchers argue that numeric probability scales may evoke deliberative processes, whereas verbal response scales evoke more intuitive processes. Numeric probability scales can also be undesirable because people have difficulty understanding numeric information (Nelson, Reyna, Fagerlin, Lipkus, & Peters, 2008; Reyna, Nelson, Han, & Dieckmann, 2009). Several innovative approaches to risk perception measurement have improved understanding of how people arrive at risk estimates and the degree to which perceived risk predicts intentions and behavior (outlined in Table 3). We review some below, and consider how assessing risk perception conviction is a related but distinct strategy.
Table 3.
Strategies for measuring risk perceptions and dimensions of risk perceptions
| Risk perception assessment | Sample item wording | Sample response scales | Differences from risk conviction |
|---|---|---|---|
| Absolute risk assessments with numeric scales | What do you think are the chances that you will develop cancer in your lifetime? | 0% to 100% | This is a traditional, cognitive assessment of risk that does not account for the conviction with which perceived risk is held. |
| Absolute risk assessments with verbal scales | I think my chances of getting colon cancer sometime in my life are… (Dillard et al., 2012) | “Almost zero” to “Almost certain” | Although verbal scales may allow people to express greater uncertainty (Bruine de Bruin, 2000), this type of risk assessment does not capture the conviction of one’s risk beliefs. |
| How likely are you to get cancer in your lifetime? (Health Information National Trends Survey) | “Very unlikely” to “Very likely” | ||
| Affective risk assessments | How worried are you about getting cancer? (Health Information National Trends Survey) | “Not at all” to “Extremely” | Although affective risk assessments may be systematically held with greater conviction, this is not yet known. |
| Experiential risk assessments | Select one answer that best represents your opinion about the statement: “I feel like I could easily get cancer in my lifetime.” (Health Information National Trends Survey) | “I feel very strongly that this will NOT happen” to “I feel very strongly that this WILL happen.” | Although experiential risk assessments may be systematically held with greater conviction, this is not yet known. It is likely that experiential risk assessments can also be guesses, particularly when people lack underlying knowledge about disease risk factors. |
| I feel that my chances of getting skin cancer at some point in my life are small. (Janssen et al., 2011) | “Completely agree” to “Completely disagree” | ||
| You just indicated your beliefs about how objectively likely it is that you will get skin cancer. However, at a gut-level, you might feel somewhat more or less vulnerable than your response above suggests. Place a mark on the scale below to indicate how you feel about your chances of getting skin cancer. (Windschitl, 2003) | Place a mark on a line that goes from 0 to 100 | ||
| Multi-level intuitive risk assessments | If I think too hard about the possibility of getting cancer, I could get it (Cognitive Causation); I get frightened when I think I could get cancer (Negative affect in risk); Anybody can get cancer, no matter what they do (Unpredictability of cancer) (Hay et al., 2014) | “Strongly disagree” to “Strongly agree” | This approach assesses dimensions of perceived risk. Conviction may be an additional dimension of perceived risk, and intuitive risk perceptions may contribute to whether people are certain of their perceived risk. |
| Don’t know responses | Allowing respondents to select “don’t know” risk versus treating “don’t know” responses as missing data (Waters et al., 2013) | “Very unlikely” to “Very likely” with additional responses of “I don’t know” or “No idea” | This strategy dichotomizes knowing vs. not knowing risk, and does not allow for varying degrees of uncertainty. |
Alternatives to cognitive/deliberative assessments of perceived risk
People make judgments and decisions – including risk judgments—based on cognitive and affective factors (Loewenstein, Weber, Hsee, & Welch, 2001; Slovic, Peters, Finucane, & MacGregor, 2005; Windschitl, 2003). Measures designed to tap into affective factors have had substantial success in predicting behavior. It is important to note that researchers have inconsistently used multiple terms to describe different types of risk beliefs. We use terminology from the tripartite model of Ferrer, Klein, Persoskie, Avishai-Yitshak, and Sheeran (2015) in which perceived risk is composed of deliberative (i.e., rational judgments of likelihood), affective (e.g., worry and fear about the possibility of disease), and experiential (i.e., gut feelings of vulnerability) beliefs about disease risk. We also discuss comparative and multi-level intuitive beliefs about risk.
Affective and experiential perceptions of risk
Researchers have found that affective perceptions of risk – such as worry about a future health risk (as opposed to thinking one is at increased risk) – are reliable predictors of intentions and health behavior. One meta-analysis showed that breast cancer worry was associated with screening; the effect was small (r = .12) but reliable (Hay, McCaul, & Magnan, 2006). Worry about getting heart disease in a sample of people with diabetes was more predictive of their exercise intentions than were perceived absolute, comparative, or conditional risk (Portnoy, Kaufman, Klein, Doyle, & de Groot, 2014).
Experiential perceptions of risk refer to “gut” feelings of vulnerability to a future health risk (e.g., “I feel that my chances of getting cancer at some point in my life are small”). We note that in prior work these “experiential” risk beliefs have been referred to both as “feeling at risk” (e.g., Weinstein et al., 2007) and “affective risk” (e.g., Janssen, van Osch, de Vries, & Lechner, 2011). Windschitl (2003) argued that beliefs about the likelihood of an outcome have two distinct components: beliefs about the objective probability and “gut-level” feelings about vulnerability. Although “gut-level” beliefs about disease risk have been captured by instructions concerning “your initial impressions and your gut-level responses” (Windschitl & Young, 2001), this wording is infrequently used. Some studies have shown that experiential measures are better predictors than conventional risk perception measures such as subjective likelihood (e.g., Dillard et al., 2012; Janssen et al., 2011; Janssen, van Osch, Lechner, Candel, & de Vries, 2012; Janssen, Waters, van Osch, Lechner, & de Vries, 2014; Schmiege, Bryan, & Klein, 2009; Weinstein et al., 2007). For example, Weinstein and colleagues (2007) found that “feeling at risk” for the flu was more predictive of getting vaccinated than were subjective likelihood and comparative risk perceptions.
It is possible that people systematically hold affective and experiential risk judgments with greater conviction than deliberative risk perceptions. This possibility is consistent with the construct of “affective validation” in which people are more certain of attitudes that they “feel” are correct (Rucker et al., 2014). If this were the case for risk perceptions, it can explain why affective and experiential risk assessments are often more predictive of behavior than deliberative risk assessments. We are not aware of any arguments positing that experiential judgments of risk better predict behavior because they are held with greater conviction; relying on affect is said to be “quicker, easier, and more efficient” (Slovic et al., 2005, p. S35). Importantly, risk perceptions held with greater confidence and accessed more quickly and easily might all be indicators of more meaningful risk beliefs, and we expect that these factors would likely co-occur.
A typical experiential risk item asks, “Select one answer that best represents your opinion about the statement: ‘I feel that my chances of getting skin cancer at some point in my life are small’” with response options from “Completely agree” to “Completely disagree” (Janssen et al., 2011; although we note again that Janssen refers to this construct as affective risk beliefs). These response options capture the certainty with which a person thinks an event will happen. Contrast this with a deliberate risk perception item such as “How likely are you to get cancer in your lifetime?” with response options from “Very likely” to “Very unlikely.” These response options capture perceived likelihood but not the certainty with which these beliefs are held. These potentially systematic differences in the way deliberative versus experiential risk questions are phrased raise the possibility that experiential risk assessments are more predictive because they capture risk conviction. Although this confound does not exist for affective beliefs about risk (e.g., worry and fear) we similarly believe that these affective beliefs are held with greater conviction, as it seems likely that people know how much they worry about or fear an event.
Comparative perceptions of risk
So far, we have been referring primarily to conventional subjective likelihood estimates that are assessed on numeric (e.g., 0% to 100%) or verbal scales (e.g., unlikely to likely). Research on social comparison theory (Festinger, 1954) shows that people making self-judgments find comparisons useful because they provide context. Accordingly, comparative risk is another commonly-used measure of perceived risk that measures how one’s risk compares with a reference group such as the “average person” or people of similar age. It is unclear whether comparative judgments are more difficult to make. On one hand, they may require more thought because people must rate their own risk, the referent group’s risk, and compare the two. On the other hand, they may require less thought if people find it easier to judge their risk when they have a comparative referent. Indeed, some social comparisons are virtually automatic (Gilbert, Giesler, & Morris, 1995). At times, comparative risk judgments may be proxies for absolute risk judgments because people focus egocentrically on their own risk (Chambers & Windschitl, 2004).
Comparative risk judgments often (but not always) predict intentions and behavior more reliably than absolute judgments (see, for example Blalock, DeVellis, Afifi, & Sandler, 1990). The risk perceptions of participants given comparative risk information indicating that they were at higher or lower risk than similar peers were more likely to influence behavioral intentions than those of participants given standard risk information (Lipkus & Klein, 2006). In a study in which absolute and comparative risk were experimentally manipulated, only comparative risk influenced intentions to change behavior (Klein, 1997). With these observations in mind, one might expect comparative risk perceptions to be held with more conviction because social comparisons create context, and because comparative risk perceptions are highly resistant to change (Weinstein & Klein, 1995). On the other hand, because both the assessments of own and referent risk could be fraught with error, comparative risk judgments may be held with less conviction. This question is currently unanswered.
Multi-level intuitive risk perceptions
Researchers have also attempted to comprehensively incorporate “gut-level reactions” about risk as well as affect and thoughts about risk into perceived risk assessments (Hay et al., 2005; Hay et al., 2014). This work provides fascinating insights into why people may be unsure of their disease risk and why current risk perception measures lack predictive validity.
A scale consisting of five factors underlying “intuitive risk perceptions” (Hay et al., 2014) was developed based on findings from qualitative work with 15 smokers (Hay et al., 2005). A “cognitive causation” factor consisted of superstitious beliefs in which participants believed they might invoke bad luck or disease just by thinking their disease risk is high or by thinking about their risk at all (this item was endorsed by 6–19% of various samples). In addition, 70–79% of various samples endorsed a “defensive pessimism” belief that being overconfident about avoiding cancer could cause cancer.
Participants also endorsed beliefs that cancer risk is uncertain or unknowable (Hay et al., 2014); approximately 70% of multiple samples agreed that, “There is no way to know whether I might get cancer in the future.” These beliefs may be consequential: some participants who believed that cancer risk is unknowable thought they were less responsible for their behavior (Hay et al., 2005). This suggests that people with less risk conviction may be less likely to engage in preventive behaviors. In general, these studies suggest that there are varied and complex reasons why people’s risk estimates may not reflect their true beliefs, and why people may be uncertain of their risk for disease. This approach is complementary to the risk conviction approach.
Don’t know responses
Researchers are also examining why and how often people respond “don’t know” when asked to report their perceived risk (LeMasters et al., 2014; Orom, O’Quin, Reilly, & Kiviniemi, 2014; Waters et al., 2013). Many people select “don’t know” or “no idea” if it is an option. 69% of respondents in one study indicated that they did not know their risk of developing colorectal cancer (Waters et al., 2013), although the proportion has been smaller in other studies (Orom et al., 2014). People with characteristics often associated with health disparities (e.g., less education) are more likely to select don’t know (Waters et al., 2013), as are those with lower knowledge about cancer prevention and screening (Hay, Orom, Kiviniemi, & Waters, 2015). These data suggest that when researchers exclude people who select “don’t know” from analyses they may be excluding people who most need health interventions. The authors note also that people who don’t know their risk may randomly select an option, leading to error and lower predictive validity of risk perceptions.
Of multiple innovative approaches to improving risk perception measurement, considering don’t know responses seems to be the most similar to our risk conviction approach. Certainly, people who answer “don’t know” should have less conviction. However, we are suggesting a continuous measure of risk conviction to be used as a moderator or an alternative to perceived risk. In contrast, don’t know responses dichotomize presence versus absence of uncertainty. In addition, we expect that people who don’t know their risk are lower in risk clarity than in risk correctness. Clarity refers to whether people have a sense of their own risk beliefs (similar to “don’t know” responding) whereas correctness assesses whether people think their risk beliefs are objectively accurate. Don’t know responses are likely to better capture this former component of risk conviction. Thus, we believe the approaches are complementary and both hold substantial promise for improving risk perception measurement.
Conclusion
By taking a theoretical approach to understanding and promoting engagement in health behaviors, we hope to accelerate knowledge and reduce duplicity. The goal of this paper is to draw connections between the literatures on attitudes and risk perceptions toward the end of promoting our understanding of risk perceptions. Importantly, insights from research on attitude strength might also extend to other health cognitions such as perceived subjective norms and beliefs about how one will feel upon getting a disease (affective forecasting). The specific application to perceived risk has important conceptual, methodological, and applied implications. Conceptually, it is crucial to understand how people think about risk to develop the best models to predict behavior and other outcomes that should be related to risk perceptions. If it conviction is as or even more important than magnitude of risk perception in predicting some types of behaviors, that would cause a notable change in the way researchers conceptualize risk perception.
A substantial literature reveals only modest correlations between risk perceptions and intentions/behavior, indicating that we may not be measuring risk perception in the most effective manner. Alternatives to conventional subjective probability measures (e.g., comparative and experiential risk assessments) have been developed and show promise, but nevertheless still predict a modest amount of variance in behavior. Well-developed measures of risk conviction might address this gap. In addition, applied work often attempts to increase risk perception in order to motivate behavior change; however, these attempts are often ineffective when the people receiving risk estimates cling to their original risk perceptions. Researchers designing interventions may need to pay further heed to the conviction with which people hold their risk perceptions in order to maximize effects on behavior change. We hope the field will consider applying attitude measurement principles to that of risk perception to be a fruitful endeavor.
Acknowledgments
We would like to thank Drs. Rebecca Ferrer and Jerry Suls for helpful comments on an earlier version of this manuscript.
Footnotes
Jennifer M. Taber and William M.P. Klein declare that they have no conflicts of interest.
References
- Abelson RP. Conviction. American Psychologist. 1988;43(4):267–275. doi: 10.1037/0003-066X.43.4.267. [DOI] [Google Scholar]
- Aspinwall LG, Taber JM, Kohlmann W, Leaf SL, Leachman SA. Perceived risk following melanoma genetic testing: a 2-year prospective study distinguishing subjective estimates from recall. Journal of Genetic Counseling. 2014;23(3):421–437. doi: 10.1007/s10897-013-9676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banaji MR, Heiphetz L. Attitudes. In: Fiske ST, Gilbert DT, Lindzey G, Fiske ST, Gilbert DT, Lindzey G, editors. Handbook of social psychology. 5. Vol. 1. Hoboken, NJ, US: John Wiley & Sons Inc; 2010. pp. 353–393. [Google Scholar]
- Blalock SJ, DeVellis BM, Afifi RA, Sandler RS. Risk perceptions and participation in colorectal cancer screening. Health Psychology. 1990;9(6):792–806. doi: 10.1037//0278-6133.9.6.792. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W, Carman KG. Measuring risk perceptions: what does the excessive use of 50% mean? Medical Decision Making. 2012;32(2):232–236. doi: 10.1177/0272989x11404077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W, Fischhoff B, Millstein SG, Halpern-Felsher BL. Verbal and numerical expressions of probability: ‘It’s a fifty-fifty chance.’. Organizational Behavior and Human Decision Processes. 2000;81(1):115–131. doi: 10.1006/obhd.1999.2868. [DOI] [PubMed] [Google Scholar]
- Cameron LD, Sherman KA, Marteau TM, Brown PM. Impact of genetic risk information and type of disease on perceived risk, anticipated affect, and expected consequences of genetic tests. Health Psychology. 2009;28(3):307–316. doi: 10.1037/a0013947. [DOI] [PubMed] [Google Scholar]
- Chambers JR, Windschitl PD. Biases in social comparative judgments: the role of nonmotivated factors in above-average and comparative-optimism effects. Psychological Bulletin. 2004;130(5):813–838. doi: 10.1037/0033-2909.130.5.813. doi: http://dx.doi.org/10.1037/0033-2909.130.5.813. [DOI] [PubMed] [Google Scholar]
- Cooke R, Sheeran P. Moderation of cognition-intention and cognition-behaviour relations: A meta-analysis of properties of variables from the theory of planned behaviour. British Journal of Social Psychology. 2004;43(2):159–186. doi: 10.1348/0144666041501688. [DOI] [PubMed] [Google Scholar]
- Dieng M, Watts CG, Kasparian NA, Morton RL, Mann GJ, Cust AE. Improving subjective perception of personal cancer risk: systematic review and meta-analysis of educational interventions for people with cancer or at high risk of cancer. Psychooncology. 2014;23(6):613–625. doi: 10.1002/pon.3476. [DOI] [PubMed] [Google Scholar]
- Dillard AJ, Ferrer RA, Ubel PA, Fagerlin A. Risk perception measures’ associations with behavior intentions, affect, and cognition following colon cancer screening messages. Health Psychology. 2012;31(1):106–113. doi: 10.1037/a0024787. [DOI] [PubMed] [Google Scholar]
- Eagly AH, Chaiken S. The psychology of attitudes. Orlando, FL, US: Harcourt Brace Jovanovich College Publishers; 1993. [Google Scholar]
- Eagly AH, Chaiken S. Attitude structure and function. In: Gilbert DT, Fiske ST, Lindzey G, Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. 4. 1 and 2. New York, NY, US: McGraw-Hill; 1998. pp. 269–322. [Google Scholar]
- Ellsberg D. Risk, Ambiguity, and the Savage Axioms. The Quarterly Journal of Economics. 1961;75(4):643–669. doi: 10.2307/1884324. [DOI] [Google Scholar]
- Fazio RH, Zanna MP. Attitudinal qualities relating to the strength of the attitude-behavior relationship. Journal of Experimental Social Psychology. 1978;14:398–408. doi: 10.1016/0022-1031(78)90035-5. [DOI] [Google Scholar]
- Ferrer RA, Klein WMP, Persoskie A, Avishai-Yitshak A, Sheeran P. The tripartite model of risk perception (TRIRISK): Evidence that perceived risk has deliberative, affective, and experiential components. 2015 doi: 10.1007/s12160-016-9790-z. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Ferrer R, Klein WMP. Risk perceptions and health behavior. Current Opinion in Psychology. 2015;5:85–89. doi: 10.1016/j.copsyc.2015.03.012. doi: http://dx.doi.org/10.1016/j.copsyc.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human relations. 1954;7(2):117–140. doi: 10.1177/001872675400700202. [DOI] [Google Scholar]
- Fischhoff B, Bruine De Bruin W. Fifty–fifty = 50%? Journal of Behavioral Decision Making. 1999;12(2):149–163. doi: 10.1002/(SICI)1099-0771(199906)12:2<149::AID-BDM314>3.0.CO;2-J. [DOI] [Google Scholar]
- Gerrard M, Gibbons FX, Bushman BJ. Relation between perceived vulnerability to HIV and precautionary sexual behavior. Psychological Bulletin. 1996;119(3):390–409. doi: 10.1037/0033-2909.119.3.390. [DOI] [PubMed] [Google Scholar]
- Gilbert DT, Giesler RB, Morris KA. When comparisons arise. Journal of Personality and Social Psychology. 1995;69(2):227–236. doi: 10.1037//0022-3514.69.2.227. doi: http://dx.doi.org/10.1037/0022-3514.69.2.227. [DOI] [PubMed] [Google Scholar]
- Glasman LR, Albarracín D. Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychological Bulletin. 2006;132(5):778–822. doi: 10.1037/0033-2909.132.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross SR, Holtz R, Miller N. Attitude certainty. In: Petty RE, Krosnick JA, Petty RE, Krosnick JA, editors. Attitude strength: Antecedents and consequences. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1995. pp. 215–245. [Google Scholar]
- Han PKJ, Klein WMP, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Medical Decision Making. 2011;31(6):828–838. doi: 10.1177/0272989X11393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay J, Shuk E, Cruz G, Ostroff J. Thinking through cancer risk: characterizing smokers’ process of risk determination. Qualitative Health Research. 2005;15(8):1074–1085. doi: 10.1177/1049732305276682. [DOI] [PubMed] [Google Scholar]
- Hay JL, Baser R, Weinstein ND, Li Y, Primavera L, Kemeny MM. Examining intuitive risk perceptions for cancer in diverse populations. Health, Risk, & Society. 2014;16(3):227–242. doi: 10.1080/13698575.2014.911822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay JL, McCaul KD, Magnan RE. Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Preventive Medicine. 2006;42(6):401–408. doi: 10.1016/j.ypmed.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Hay JL, Orom H, Kiviniemi MT, Waters EA. “I don’t know” my cancer risk: Exploring deficits in cancer knowledge and information-seeking skills to explain an often-overlooked participant response. Medical Decision Making. 2015;35(4):436–445. doi: 10.1177/0272989x15572827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Information National Trends Survey. 2015 Available at hints.cancer.gov.
- Helgeson VS, Novak SA. Illness centrality and well-being among male and female early adolescents with diabetes. Journal of Pediatric Psychology. 2007;32(3):260–272. doi: 10.1093/jpepsy/jsl018. [DOI] [PubMed] [Google Scholar]
- Janssen E, van Osch L, de Vries H, Lechner L. Measuring risk perceptions of skin cancer: reliability and validity of different operationalizations. British Journal of Health Psychology. 2011;16(Pt 1):92–112. doi: 10.1348/135910710x514120. [DOI] [PubMed] [Google Scholar]
- Janssen E, van Osch L, Lechner L, Candel M, de Vries H. Thinking versus feeling: Differentiating between cognitive and affective components of perceived cancer risk. Psychology & Health. 2012;27(7):767–783. doi: 10.1080/08870446.2011.580846. [DOI] [PubMed] [Google Scholar]
- Janssen E, Waters EA, van Osch L, Lechner L, de Vries H. The importance of affectively-laden beliefs about health risks: The case of tobacco use and sun protection. Journal of Behavioral Medicine. 2014;37(1):11–21. doi: 10.1007/s10865-012-9462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, Ditto PH, Croyle RT. Judging health status: Effects of perceived prevalence and personal relevance. Journal of Personality and Social Psychology. 1986;50(5):899–905. doi: 10.1037/0022-3514.50.5.899. [DOI] [PubMed] [Google Scholar]
- Klein WM. Objective standards are not enough: Affective, self-evaluative, and behavioral responses to social comparison information. Journal of Personality and Social Psychology. 1997;72(4):763–774. doi: 10.1037/0022-3514.72.4.763. [DOI] [PubMed] [Google Scholar]
- Klein WMP, Monin MM. When focusing on negative and positive attributes of the self elicits more inductive self-judgment. Personality and Social Psychology Bulletin. 2009;35(3):376–384. doi: 10.1177/0146167208328065. [DOI] [PubMed] [Google Scholar]
- Klein WMP, Blier H, Janze A. Maintaining Positive Self-Evaluations: Reducing Attention to Diagnostic but Unfavorable Social Comparison Information When General Self-Regard Is Salient. Motivation and Emotion. 2001;25(1):23–40. doi: 10.1023/A:1010607821908. [DOI] [Google Scholar]
- Kraus SJ. Attitudes and the prediction of behavior: A meta-analysis of the empirical literature. Personality and Social Psychology Bulletin. 1995;21(1):58–75. doi: 10.1177/0146167295211007. [DOI] [Google Scholar]
- Krosnick JA, Petty RE. Attitude strength: An overview. In: Petty RE, Krosnick JA, Petty RE, Krosnick JA, editors. Attitude strength: Antecedents and consequences. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1995. pp. 1–24. [Google Scholar]
- LaPiere RT. Attitudes vs. Actions. Social Forces. 1934;13:230–237. doi: 10.2307/2570339. [DOI] [Google Scholar]
- LeMasters T, Madhavan S, Atkins E, Vyas A, Remick S, Vona-Davis L. “Don’t know” and accuracy of breast cancer risk perceptions among Appalachian women attending a mobile mammography program: implications for educational interventions and patient empowerment. Journal of Cancer Education. 2014;29(4):669–679. doi: 10.1007/s13187-014-0621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipkus IM, Klein WMP. Effects of communicating social comparison information on risk perceptions for colorectal cancer. Journal of Health Communication. 2006;11(4):391–407. doi: 10.1080/10810730600671870. [DOI] [PubMed] [Google Scholar]
- Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychological Bulletin. 2001;127(2):267–286. doi: 10.1037/0033-2909.127.2.267. [DOI] [PubMed] [Google Scholar]
- McCaul KD, Branstetter AD, Schroeder DM, Glasgow RE. What is the relationship between breast cancer risk and mammography screening? A meta-analytic review. Health Psychology. 1996;15(6):423–429. doi: 10.1037/0278-6133.15.6.423. [DOI] [PubMed] [Google Scholar]
- McQueen A, Vernon SW, Swank PR. Construct Definition and Scale Development for Defensive Information Processing: An Application to Colorectal Cancer Screening. Health Psychology. 2012;32(20):190–202. doi: 10.1037/a002731110.1037/a0027311.supp. Supplemental. [DOI] [PubMed] [Google Scholar]
- Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: Theory and practice. Annals of Behavioral Medicine. 2008;35(3):261–274. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orom H, O’Quin KE, Reilly S, Kiviniemi MT. Perceived cancer risk and risk attributions among African-American residents of a low-income, predominantly African-American neighborhood. Ethnicity & Health. 2015;20(6):543–556. doi: 10.1080/13557858.2014.950197. [DOI] [PubMed] [Google Scholar]
- Petrocelli JV, Tormala ZL, Rucker DD. Unpacking attitude certainty: Attitude clarity and attitude correctness. Journal of Personality and Social Psychology. 2007;92(1):30–41. doi: 10.1037/0022-3514.92.1.30. [DOI] [PubMed] [Google Scholar]
- Portnoy DB, Kaufman AR, Klein WMP, Doyle TA, de Groot M. Cognitive and Affective Perceptions of Vulnerability as Predictors of Exercise Intentions among People with Type 2 Diabetes. Journal of Risk Research. 2014;17(2):177–193. doi: 10.1080/13669877.2013.794153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychological Bulletin. 2009;135(6):943–973. doi: 10.1037/a0017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronis DL. Conditional health threats: Health beliefs, decisions, and behaviors among adults. Health Psychology. 1992;11(2):127–134. doi: 10.1037//0278-6133.11.2.127. doi: http://dx.doi.org/10.1037/0278-6133.11.2.127. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. The health belief model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. San Francisco, CA US: Jossey-Bass; 1990. pp. 39–62. [Google Scholar]
- Rucker DD, Tormala ZL, Petty RE, Briñol P. Consumer conviction and commitment: An appraisal-based framework for attitude certainty. Journal of Consumer Psychology. 2014;24(1):119–136. doi: 10.1016/j.jcps.2013.07.001. [DOI] [Google Scholar]
- Scherer LD, Ubel PA, McClure J, Greene SM, Alford SH, Holtzman L, …Fagerlin A. Belief in numbers: When and why women disbelieve tailored breast cancer risk statistics. Patient Education and Counseling. 2013;92(2):253–259. doi: 10.1016/j.pec.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiege SJ, Bryan A, Klein WMP. Distinctions between worry and perceived risk in the context of the theory of planned behavior. Journal of Applied Social Psychology. 2009;39(1):95–119. doi: 10.1111/j.1559-1816.2008.00431.x. [DOI] [Google Scholar]
- Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychological Bulletin. 2014;140(2):511–543. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Smith SM, Fabrigar LR, MacDougall BL, Wiesenthal NL. The role of amount, cognitive elaboration, and structural consistency of attitude-relevant knowledge in the formation of attitude certainty. European Journal of Social Psychology. 2008;38(2):280–295. http://dx.doi.org/10.1002/ejsp.447. [Google Scholar]
- Slovic P, Peters E, Finucane ML, MacGregor DG. Affect, risk, and decision making. Health Psychology. 2005;24(4, Suppl):S35–S40. doi: 10.1037/0278-6133.24.4.S35. [DOI] [PubMed] [Google Scholar]
- Tormala ZL, Rucker DD. Attitude certainty: A review of past findings and emerging perspectives. Social and Personality Psychology Compass. 2007;1(1):469–492. doi: 10.1111/j.1751-9004.2007.00025.x. [DOI] [Google Scholar]
- van’t Riet J, Ruiter RAC. Defensive reactions to health-promoting information: An overview and implications for future research. Health Psychology Review. 2013;7(Suppl 1):S104–S136. doi: 10.1080/17437199.2011.606782. [DOI] [Google Scholar]
- Waters EA, Hay JL, Orom H, Kiviniemi MT, Drake BF. “Don’t know” responses to risk perception measures: implications for underserved populations. Medical Decision Making. 2013;33(2):271–281. doi: 10.1177/0272989x12464435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein ND. Conceptualizing and Measuring Risk Perceptions. 2003 http://cancercontrol.cancer.gov/brp/research/theories_project/weinstein.pdf.
- Weinstein ND, Klein WM. Resistance of personal risk perceptions to debiasing interventions. Health Psychology. 1995;14(2):132–140. doi: 10.1037//0278-6133.14.2.132. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychology. 2007;26(2):146–151. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Rothman AJ, Nicolich M. Use of correlational data to examine the effects of risk perceptions on precautionary behavior. Psychology and Health. 1998;13(3):479–501. doi: 10.1080/08870449808407305. [DOI] [Google Scholar]
- Wicker AW. Attitudes versus actions: The relationship of verbal and overt behavioral responses to attitude objects. Journal of Social Issues. 1969;25(4):41–78. doi: 10.1111/j.1540-4560.1969.tb00619.x. [DOI] [Google Scholar]
- Windschitl PD. Judging the accuracy of a likelihood judgment: The case of smoking risk. Journal of Behavioral Decision Making. 2002;15(1):19–35. doi: 10.1002/bdm.401. [DOI] [Google Scholar]
- Windschitl PD. Measuring and conceptualizing perceptions of vulnerability/likelihood. Paper presented at the Paper presented at the Conceptualizing and Measuring Risk Perceptions Workshop; Washington, D.C. 2003. Available at: http://cancercontrol.cancer.gov/brp/research/theories_project/windschitl.pdf. [Google Scholar]
- Windschitl PD, Wells GL. Measuring psychological uncertainty: Verbal versus numeric methods. Journal of Experimental Psychology: Applied. 1996;2(4):343–364. doi: 10.1037/1076-898X.2.4.343. [DOI] [Google Scholar]
- Windschitl PD, Young ME. The influence of alternative outcomes on gut-level perceptions of certainty. Organizational Behavior and Human Decision Processes. 2001;85(1):109–134. doi: 10.1006/obhd.2000.2934. [DOI] [PubMed] [Google Scholar]
- Witte K. Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs. 1992;59(4):329–349. doi: 10.1080/03637759209376276. [DOI] [Google Scholar]