Abstract
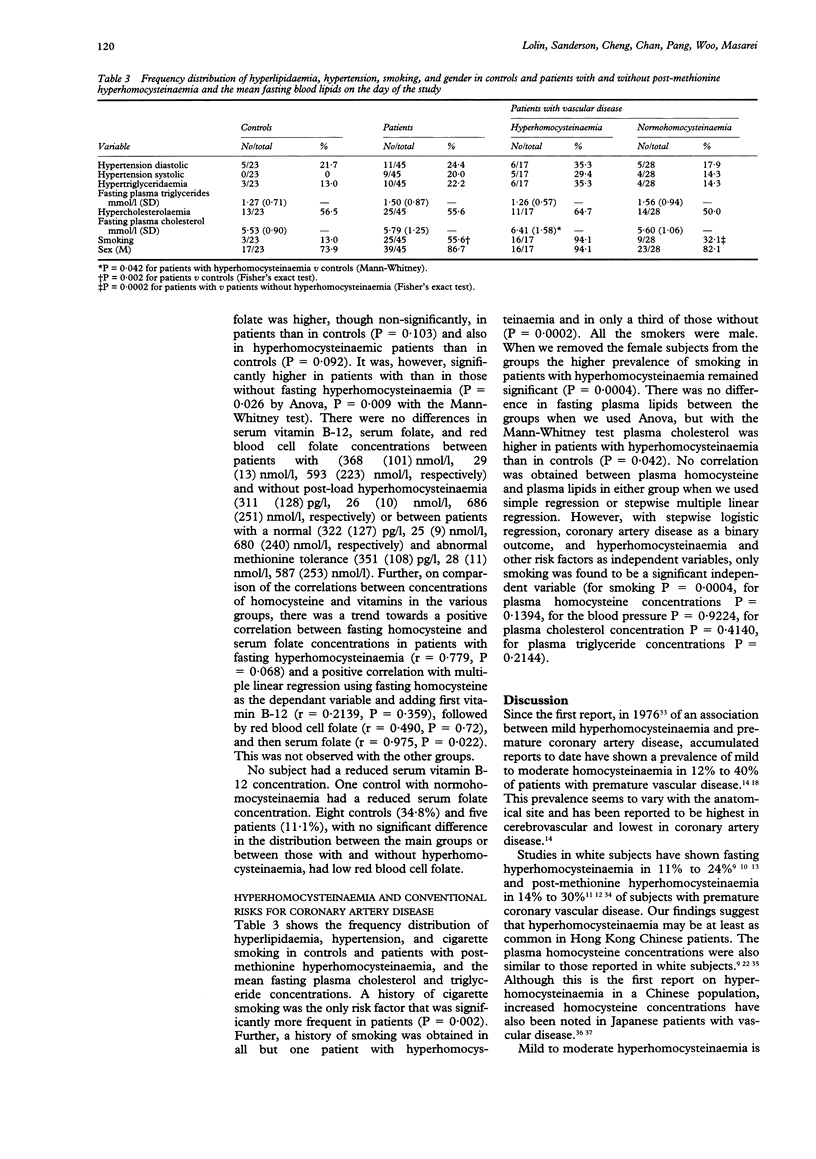
OBJECTIVES: To examine the prevalence of hyperhomocysteinaemia and compare it with the classic risk factors and vitamin status in Hong Kong Chinese patients with premature atherosclerotic coronary artery disease. DESIGN: Case-control study. SETTING: General hospital and community. SUBJECTS: Forty five patients (39 males) with significant coronary artery disease confirmed by angiography (32 post myocardial infarction) and 23 healthy volunteers (17 male), all aged less than 55 years. INTERVENTION: Standardised methionine-loading test. MAIN OUTCOME MEASURES: Coronary artery disease, risk factors. RESULTS: More patients than controls had fasting hyperhomocysteinaemia (10/45 v 2/23, P = 0.122), post-methionine hyperhomocysteinaemia (17/45 v 1/23, P = 0.008), and an abnormal response to methionine (15/45 v 1/23, P = 0.015). A history of smoking was more frequent in patients (3/23 v 25/45, P = 0.002). Sixteen of 17 patients with hyperhomocysteinaemia but only nine of 28 with normohomocysteinaemia were smokers (P = 0.0002). Fasting plasma cholesterol concentrations (mean (SD)) were higher in hyperhomocysteinaemic patients (6.41 (1.58) mmol/l) than in controls (5.53 (0.90) mmol/l) (P = 0.042). Serum vitamin B-12 was not reduced and serum folate was higher in hyperhomocysteinaemic patients (35 (4) nmol/l) than normohomocysteinaemic patients (26 (9) nmol/l) (P = 0.009). CONCLUSIONS: Although the prevalence of hyperhomocysteinaemia in Hong Kong Chinese is similar to that in white subjects, hyperhomocysteinaemia is not an independent risk factor for coronary artery disease and is associated with smoking. This may be of some consequence in view of the change to a more Western diet with more animal protein, and therefore methionine, coupled with a high frequency of cigarette smokers in this region. The causes of the hyperhomocysteinaemia are multifactorial but in this pilot study a deficiency of folate and/or vitamin B-12 did not seem to be one of them.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andersson A., Brattström L., Israelsson B., Isaksson A., Hamfelt A., Hultberg B. Plasma homocysteine before and after methionine loading with regard to age, gender, and menopausal status. Eur J Clin Invest. 1992 Feb;22(2):79–87. doi: 10.1111/j.1365-2362.1992.tb01940.x. [DOI] [PubMed] [Google Scholar]
- Araki A., Sako Y., Fukushima Y., Matsumoto M., Asada T., Kita T. Plasma sulfhydryl-containing amino acids in patients with cerebral infarction and in hypertensive subjects. Atherosclerosis. 1989 Oct;79(2-3):139–146. doi: 10.1016/0021-9150(89)90118-4. [DOI] [PubMed] [Google Scholar]
- Araki A., Sako Y., Ito H. Plasma homocysteine concentrations in Japanese patients with non-insulin-dependent diabetes mellitus: effect of parenteral methylcobalamin treatment. Atherosclerosis. 1993 Nov;103(2):149–157. doi: 10.1016/0021-9150(93)90258-v. [DOI] [PubMed] [Google Scholar]
- Bergmark C., Mansoor M. A., Swedenborg J., de Faire U., Svardal A. M., Ueland P. M. Hyperhomocysteinemia in patients operated for lower extremity ischaemia below the age of 50--effect of smoking and extent of disease. Eur J Vasc Surg. 1993 Jul;7(4):391–396. doi: 10.1016/s0950-821x(05)80255-5. [DOI] [PubMed] [Google Scholar]
- Boers G. H. Carriership for homocystinuria in juvenile vascular disease. Haemostasis. 1989;19 (Suppl 1):29–34. doi: 10.1159/000216093. [DOI] [PubMed] [Google Scholar]
- Boers G. H., Fowler B., Smals A. G., Trijbels F. J., Leermakers A. I., Kleijer W. J., Kloppenborg P. W. Improved identification of heterozygotes for homocystinuria due to cystathionine synthase deficiency by the combination of methionine loading and enzyme determination in cultured fibroblasts. Hum Genet. 1985;69(2):164–169. doi: 10.1007/BF00293290. [DOI] [PubMed] [Google Scholar]
- Boers G. H., Smals A. G., Trijbels F. J., Fowler B., Bakkeren J. A., Schoonderwaldt H. C., Kleijer W. J., Kloppenborg P. W. Heterozygosity for homocystinuria in premature peripheral and cerebral occlusive arterial disease. N Engl J Med. 1985 Sep 19;313(12):709–715. doi: 10.1056/NEJM198509193131201. [DOI] [PubMed] [Google Scholar]
- Brattstrom L. E., Hardebo J. E., Hultberg B. L. Moderate homocysteinemia--a possible risk factor for arteriosclerotic cerebrovascular disease. Stroke. 1984 Nov-Dec;15(6):1012–1016. doi: 10.1161/01.str.15.6.1012. [DOI] [PubMed] [Google Scholar]
- Brattström L. E., Israelsson B., Jeppsson J. O., Hultberg B. L. Folic acid--an innocuous means to reduce plasma homocysteine. Scand J Clin Lab Invest. 1988 May;48(3):215–221. doi: 10.3109/00365518809167487. [DOI] [PubMed] [Google Scholar]
- Brattström L., Israelsson B., Hultberg B. Plasma homocysteine and methionine tolerance in early-onset vascular disease. Haemostasis. 1989;19 (Suppl 1):35–44. doi: 10.1159/000216094. [DOI] [PubMed] [Google Scholar]
- Brattström L., Israelsson B., Lindgärde F., Hultberg B. Higher total plasma homocysteine in vitamin B12 deficiency than in heterozygosity for homocystinuria due to cystathionine beta-synthase deficiency. Metabolism. 1988 Feb;37(2):175–178. doi: 10.1016/s0026-0495(98)90014-2. [DOI] [PubMed] [Google Scholar]
- Cacciari E., Salardi S. Clinical and laboratory features of homocystinuria. Haemostasis. 1989;19 (Suppl 1):10–13. doi: 10.1159/000216090. [DOI] [PubMed] [Google Scholar]
- Clarke R., Daly L., Robinson K., Naughten E., Cahalane S., Fowler B., Graham I. Hyperhomocysteinemia: an independent risk factor for vascular disease. N Engl J Med. 1991 Apr 25;324(17):1149–1155. doi: 10.1056/NEJM199104253241701. [DOI] [PubMed] [Google Scholar]
- Donnan S. P., Ho S. C., Woo J., Wong S. L., Woo K. S., Tse C. Y., Chan K. K., Kay C. S., Cheung K. O., Mak K. H. Risk factors for acute myocardial infarction in a southern Chinese population. Ann Epidemiol. 1994 Jan;4(1):46–58. doi: 10.1016/1047-2797(94)90042-6. [DOI] [PubMed] [Google Scholar]
- Dudman N. P., Wilcken D. E., Wang J., Lynch J. F., Macey D., Lundberg P. Disordered methionine/homocysteine metabolism in premature vascular disease. Its occurrence, cofactor therapy, and enzymology. Arterioscler Thromb. 1993 Sep;13(9):1253–1260. doi: 10.1161/01.atv.13.9.1253. [DOI] [PubMed] [Google Scholar]
- Franken D. G., Boers G. H., Blom H. J., Trijbels F. J., Kloppenborg P. W. Treatment of mild hyperhomocysteinemia in vascular disease patients. Arterioscler Thromb. 1994 Mar;14(3):465–470. doi: 10.1161/01.atv.14.3.465. [DOI] [PubMed] [Google Scholar]
- Israelsson B., Brattström L. E., Hultberg B. L. Homocysteine and myocardial infarction. Atherosclerosis. 1988 Jun;71(2-3):227–233. doi: 10.1016/0021-9150(88)90147-5. [DOI] [PubMed] [Google Scholar]
- Jacobsen D. W., Gatautis V. J., Green R. Determination of plasma homocysteine by high-performance liquid chromatography with fluorescence detection. Anal Biochem. 1989 Apr;178(1):208–214. doi: 10.1016/0003-2697(89)90381-3. [DOI] [PubMed] [Google Scholar]
- Kang S. S., Passen E. L., Ruggie N., Wong P. W., Sora H. Thermolabile defect of methylenetetrahydrofolate reductase in coronary artery disease. Circulation. 1993 Oct;88(4 Pt 1):1463–1469. doi: 10.1161/01.cir.88.4.1463. [DOI] [PubMed] [Google Scholar]
- Kang S. S., Wong P. W., Susmano A., Sora J., Norusis M., Ruggie N. Thermolabile methylenetetrahydrofolate reductase: an inherited risk factor for coronary artery disease. Am J Hum Genet. 1991 Mar;48(3):536–545. [PMC free article] [PubMed] [Google Scholar]
- Malinow M. R. Homocyst(e)ine and arterial occlusive diseases. J Intern Med. 1994 Dec;236(6):603–617. doi: 10.1111/j.1365-2796.1994.tb00854.x. [DOI] [PubMed] [Google Scholar]
- Malinow M. R. Hyperhomocyst(e)inemia. A common and easily reversible risk factor for occlusive atherosclerosis. Circulation. 1990 Jun;81(6):2004–2006. doi: 10.1161/01.cir.81.6.2004. [DOI] [PubMed] [Google Scholar]
- Malinow M. R., Stampfer M. J. Role of plasma homocyst(e)ine in arterial occlusive diseases. Clin Chem. 1994 Jun;40(6):857–858. [PubMed] [Google Scholar]
- Mansoor M. A., Bergmark C., Svardal A. M., Lønning P. E., Ueland P. M. Redox status and protein binding of plasma homocysteine and other aminothiols in patients with early-onset peripheral vascular disease. Homocysteine and peripheral vascular disease. Arterioscler Thromb Vasc Biol. 1995 Feb;15(2):232–240. doi: 10.1161/01.atv.15.2.232. [DOI] [PubMed] [Google Scholar]
- Murphy-Chutorian D. R., Wexman M. P., Grieco A. J., Heininger J. A., Glassman E., Gaull G. E., Ng S. K., Feit F., Wexman K., Fox A. C. Methionine intolerance: a possible risk factor for coronary artery disease. J Am Coll Cardiol. 1985 Oct;6(4):725–730. doi: 10.1016/s0735-1097(85)80473-3. [DOI] [PubMed] [Google Scholar]
- Murphy-Chutorian D., Alderman E. L. The case that hyperhomocysteinemia is a risk factor for coronary artery disease. Am J Cardiol. 1994 Apr 1;73(9):705–707. doi: 10.1016/0002-9149(94)90940-7. [DOI] [PubMed] [Google Scholar]
- Skovby F. Inborn errors of metabolism causing homocysteinemia and related vascular involvement. Haemostasis. 1989;19 (Suppl 1):4–9. doi: 10.1159/000216088. [DOI] [PubMed] [Google Scholar]
- Stampfer M. J., Malinow M. R. Can lowering homocysteine levels reduce cardiovascular risk? N Engl J Med. 1995 Feb 2;332(5):328–329. doi: 10.1056/NEJM199502023320511. [DOI] [PubMed] [Google Scholar]
- Stampfer M. J., Malinow M. R., Willett W. C., Newcomer L. M., Upson B., Ullmann D., Tishler P. V., Hennekens C. H. A prospective study of plasma homocyst(e)ine and risk of myocardial infarction in US physicians. JAMA. 1992 Aug 19;268(7):877–881. [PubMed] [Google Scholar]
- Ubbink J. B., Hayward Vermaak W. J., Bissbort S. Rapid high-performance liquid chromatographic assay for total homocysteine levels in human serum. J Chromatogr. 1991 Apr 19;565(1-2):441–446. doi: 10.1016/0378-4347(91)80407-4. [DOI] [PubMed] [Google Scholar]
- Ueland P. M., Refsum H., Stabler S. P., Malinow M. R., Andersson A., Allen R. H. Total homocysteine in plasma or serum: methods and clinical applications. Clin Chem. 1993 Sep;39(9):1764–1779. [PubMed] [Google Scholar]
- Visy J. M., Le Coz P., Chadefaux B., Fressinaud C., Woimant F., Marquet J., Zittoun J., Visy J., Vallat J. M., Haguenau M. Homocystinuria due to 5,10-methylenetetrahydrofolate reductase deficiency revealed by stroke in adult siblings. Neurology. 1991 Aug;41(8):1313–1315. doi: 10.1212/wnl.41.8.1313. [DOI] [PubMed] [Google Scholar]
- Wilcken D. E., Dudman N. P. Mechanisms of thrombogenesis and accelerated atherogenesis in homocysteinaemia. Haemostasis. 1989;19 (Suppl 1):14–23. doi: 10.1159/000216091. [DOI] [PubMed] [Google Scholar]
- Wilcken D. E., Reddy S. G., Gupta V. J. Homocysteinemia, ischemic heart disease, and the carrier state for homocystinuria. Metabolism. 1983 Apr;32(4):363–370. doi: 10.1016/0026-0495(83)90045-8. [DOI] [PubMed] [Google Scholar]
- Wilcken D. E., Wilcken B. The pathogenesis of coronary artery disease. A possible role for methionine metabolism. J Clin Invest. 1976 Apr;57(4):1079–1082. doi: 10.1172/JCI108350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Ho S. C., Wong S. L., Woo K. S., Tse C. Y., Chan K. K., Kay C. S., Mak W. P., Cheung K. O., Lam C. W. Lipids, lipoproteins and other coronary risk factors in Chinese male survivors of myocardial infarction. Int J Cardiol. 1993 Jun;39(3):195–202. doi: 10.1016/0167-5273(93)90038-i. [DOI] [PubMed] [Google Scholar]
- Woo K. S., Donnan S. P. Epidemiology of coronary arterial disease in the Chinese. Int J Cardiol. 1989 Jul;24(1):83–93. doi: 10.1016/0167-5273(89)90045-4. [DOI] [PubMed] [Google Scholar]
- Wu L. L., Wu J., Hunt S. C., James B. C., Vincent G. M., Williams R. R., Hopkins P. N. Plasma homocyst(e)ine as a risk factor for early familial coronary artery disease. Clin Chem. 1994 Apr;40(4):552–561. [PubMed] [Google Scholar]



