Abstract
Objective
There are complications in stand-alone cage assisted anterior cervical discectomy and fusion (ACDF), such as cage subsidence and kyphosis. Here we report our clinical result on ACDF, comparing with stand-alone cages and with cervical plate system for degenerative cervical spine diseases.
Methods
Patients with degenerative cervical disease who were diagnosed and treated in Konyang University Hospital between January 2004 and December 2014 were included in this study. Patients who had operation in single level ACDF were selected. Patients scored the degree of pain using visual analog scale before and after the surgery. Subsidence was defined as ≥3-mm decrease of the segmental height, and cervical kyphosis was defined as progression of ≥5° at 12 months after postoperative follow-up compared to that measured at the immediate postoperative period.
Results
A total of 81 patients were enrolled for this study. Forty-five patients were included in a cervical plate group and the others were in stand-alone cage group. There was no statistical difference in pain score between the 2 groups. Segmental subsidence was observed in 7 patients (15.6%) in plate-assisted cervical fusion group, and 13 patients (36.1%) in stand-alone cage group. Segmental kyphosis was observed in 4 patients (8.9%) in plate-assisted cervical fusion group, and 10 patients (27.8%) in stand-alone cage group. There was statistical difference between the 2 groups.
Conclusion
There was no difference in pain between 2 groups. But stand-alone case group showed higher incidence rate than plate-assisted cervical fusion group in segmental subsidence and cervical kyphosis. When designing cervical fusion, more attention should be given selecting the surgical technique.
Keywords: Stand-alone cervical fusion, Segmental subsidence, Cervical kyphosis, Plate-assisted cervical fusion
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is the most frequently performed surgical treatment for several cervical spinal diseases, including herniated disc, compressive myelopathy, trauma and degenerative disease8,15). This procedure is used to decompress the spinal cord and nerve root, and to stabilize the affected segments7,25).
Smith and Robinson36)'s technique had been the "gold standard" for the surgical treatment of cervical disc disease. However, anterior cervical plates with iliac bone grafts lead to chronic iliac pain16,35) and higher rates of dysphagia11,12,22,31,37). For those reasons, several technical modifications of this procedure have been developed such as stand-alone cages, anterior cervical plates, zero-profile devices etc. But there is currently no consensus regarding the optimal technique18).
Among these procedures, cervical intervertebral disc replacement by a stand-alone cage provides immediate load bearing support to the anterior column and may facilitate arthrodesis. On the other hand, there is evidence documenting relatively frequent complications in stand-alone cage assisted ACDF, such as cage subsidence and cervical kyphosis9).
In this situation, plate-assisted cervical fusion is good alternations to stand-alone cervical fusion. But, there are only a few direct comparative researches in clinical and radiological outcomes between the 2 groups.
Here we report our clinical result of ACDF over 10 years, comparing interbody fusion with stand-alone cage and plateassisted cervical fusion for degenerative cervical spine diseases.
MATERIALS AND METHODS
This study was retrospective study on patients with degenerative cervical disease diagnosed and treated in Konyang University Hospital between January 2004 and December 2014. We evaluated total 81 patients treated with a single level ACDF. The surgery was performed by 3 neurosurgeons in a Konyang University Hospital. But, most of surgery was performed by 1 surgeon(surgeon A, 75 cases; surgeon B, 4 cases; surgeon C, 2 cases). Patients were kept in a soft collar for 8-12 weeks after surgery. And they were treated similar postoperative care such as antibiotics and pain killers etc.
They were divided into 2 groups; plate-assisted cervical fusion in group A (n=45) and stand-alone cages in group B (n=36). And follow-up duration for both groups was 12 months. The patients were randomly selected for each surgical methods.
Inclusion criteria were; (1) signs and symptoms of cervical radiculopathy or cervical spondylotic myelopathy which was unresponsive to the medical treatment, (2) single level disease confirmed by clinical symptom and imaging (plain X-ray and magnetic resonance imaging [MRI]), and (3) continuous clinical follow-up and imaging data over 1 year.
The exclusion criteria were; (1) history of previous cervical spine surgery, (2) others cervical disease, including infection, tumor, deformity etc., and (3) requirement for multilevel fusion or simultaneous anterior and posterior surgery.
1. Demographic Data
Patients' demographic data were collected on chart and plain X-ray, MRI. The preoperative study included plain radiographs and MRI of cervical spine. Patients' demographic data included age, sex, affected cervical level, and types of symptom etc.
2. Pain Results
Patients' pains were evaluated using visual analog scale (VAS) for neck pain and radicular pain before and after the surgery. Preoperative pain was checked in admission time. And regular follow-up was done immediately after surgery, 3 months, 6 months, and 12 months.
3. Surgical Technique
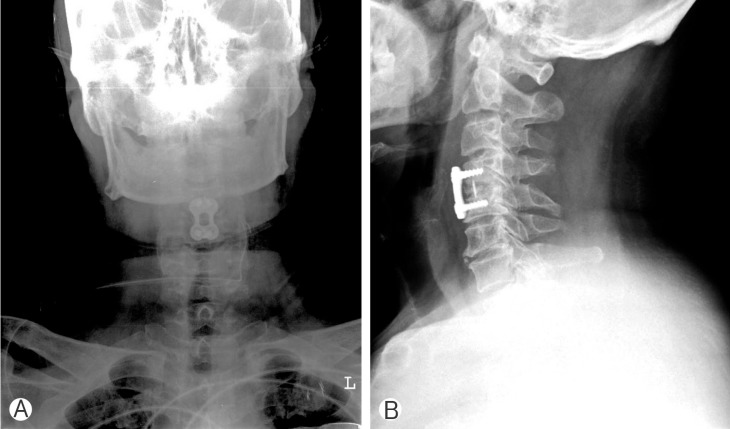
The surgical site was exposed via a standard anterior approach36) and microscopic anterior cervical discectomy was performed. After neural decompression was performed, the interbody fusion was performed using a PEEK cage (Solis, Stryker Spine, Allendale, NJ, USA). And plate-assisted cervical fusion group was accomplished with anterior cervical plates fixed by 4 screws (Figs. 1, 2). Plate was randomly selected, but mainly used Atlantis plate (Medtronic Sofamor-Danek, Memphis, TN, USA). The demineralized bone matrix was filled into the cage for fusion in groups A and B.
Fig. 1. Postoperative radiographs showing the anterior cervical plate with autologous bone graft for a single level cervical disease. (A) Posterior anterior view. (B) Lateral view.
Fig. 2. Postoperative radiographs showing the stand-alone cage for a single level cervical disease. (A) Posterior anterior view. (B) Lateral view.
4. Radiological Evaluation
Anteroposterior and lateral plain radiographs were obtained before and immediately after the surgery and 12 months later. MRI scans were also obtained before surgery.
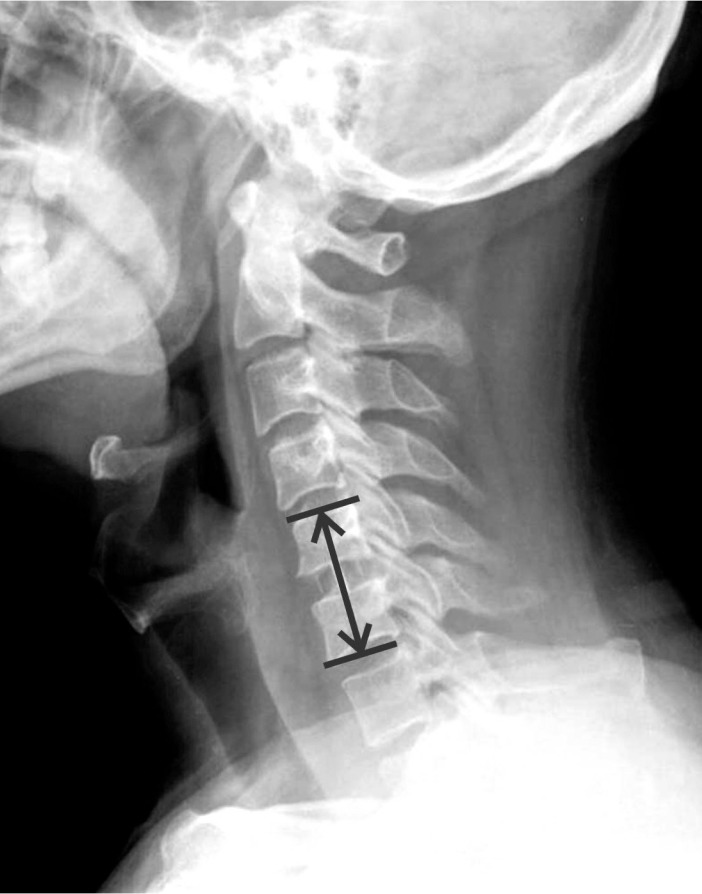
The construct length and spinal curvature were measured to compare stand-alone cage group and plate-assisted cervical fusion group. The construct length was measured as the distance from the midpoint between the anterior and posterior aspects of the superior endplate of the top level of the fusion to the midpoint of the inferior endplate of the bottom level of the fusion on the plain radiographs (Fig. 3).
Fig. 3. The construct length was measured as the distance between the middle margin of the upper end plate of the upper vertebra and the middle margin of the lower end plate of the lower vertebra.
Subsidence was defined as 3mm or more decrease of the segmental height at the postoperation 1 year follow-up compared to that measured at the immediate postoperative period3).
Cervical spinal curvature was measured by the method of Cobb angle. The Cobb angle is defined as the angle formed between a line drawn parallel to the superior endplate of one vertebra above the herniated disc and a line drawn parallel to the inferior endplate of the vertebra one level below herniated disc (Fig. 4).
Fig. 4. Segmental lordosis was measured using Cobb method.
Cervical kyphosis was defined as progression of ≥5° at the postoperative 12-month follow-up compared to that measured at the immediate postoperative period23).
5. Statistical Analysis
The statistical analysis was performed using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). Statistical comparison was made between stand-alone cage group and plate-assisted cervical fusion group based on the pain results and radiologic data. The baseline variables included the age, VAS score, segmental subsidence and cervical kyphosis. These variables were compared using the chi-square test and independent sample t-test. A p-value of 0.05 was considered as significant.
RESULTS
1. Demographic Data
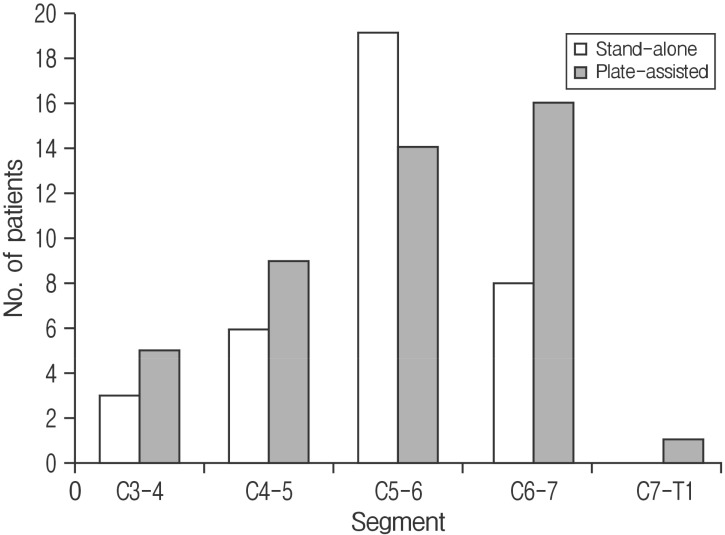
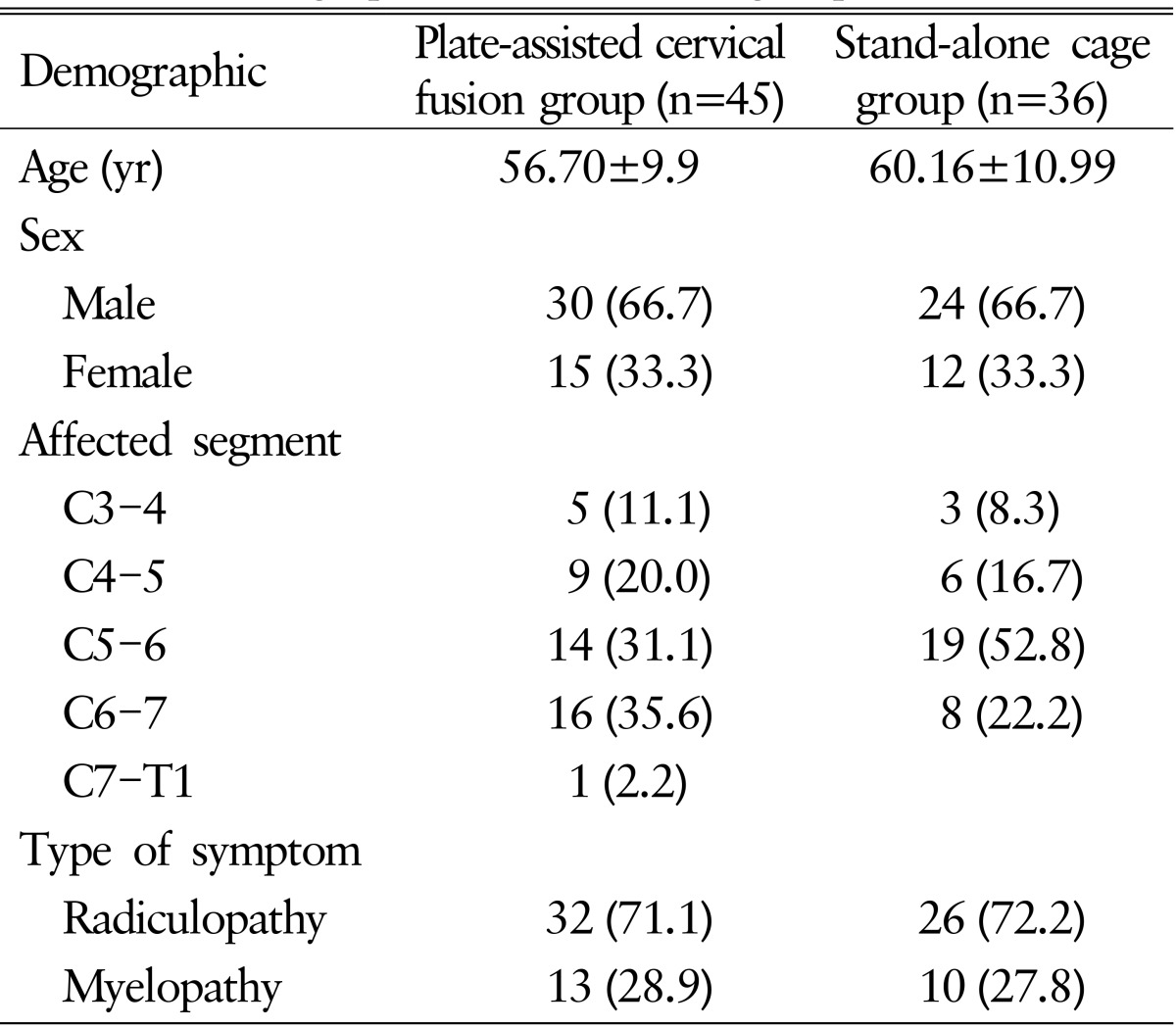
There was no demographic difference between the 2 groups. The mean age of 81 patients was 58.3 years (range, 34-86 years). Fifty-four patients were male, 27 patients were female. Most common operation site was C5-6 (40.7%). C6-7(29.6%) was second common operation site (Fig. 5). Fifty-eight patients (71.6%) had radiculopathy, and 23 patients (28.4%) had myelopathy symptoms (Table 1).
Fig. 5. Operation site for cervical degenerative disease.
Table 1. Demographic data of the 2 groups.
Values are presented as mean±standard deviation or number (%).
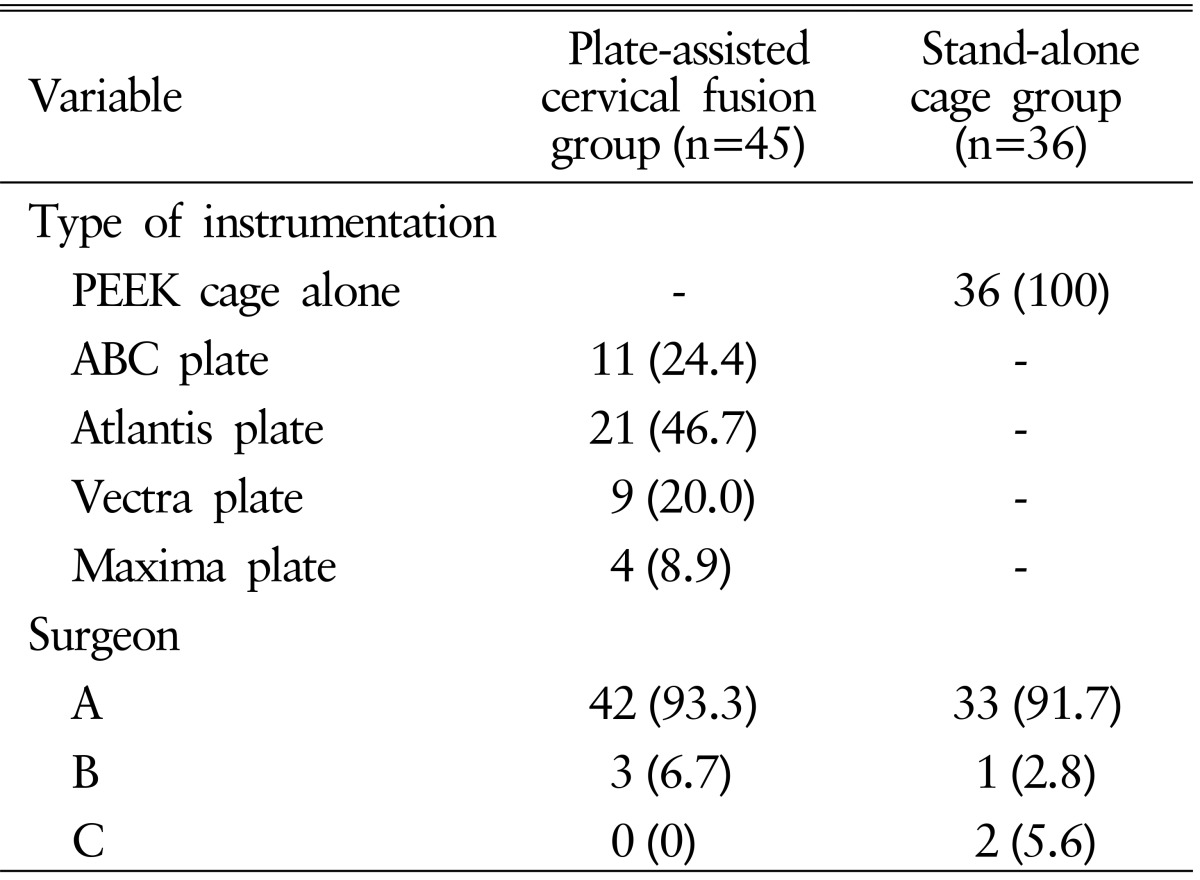
2. Surgical Data
The surgery was predominantly performed by 1 surgeon (surgeon A, 75 cases; surgeon B, 4 cases; surgeon C, 2 cases). The operation methods were randomly selected. Stand-alone cage group inserted a PEEK cage (Solis) in 36 patients (100%). And plate-assisted cervical fusion group also inserted a PEEK cage, but the plate is different. Twenty-one patients (46.7%) used Atlantis plate, 11 patients (24.4%) used ABC plate, 9 patients (20.0%) used Vectra plate, and 4 patients (8.9%) used Maxima plate (Table 2).
Table 2. Surgical data of the 2 groups.
Values are presented as number (%).
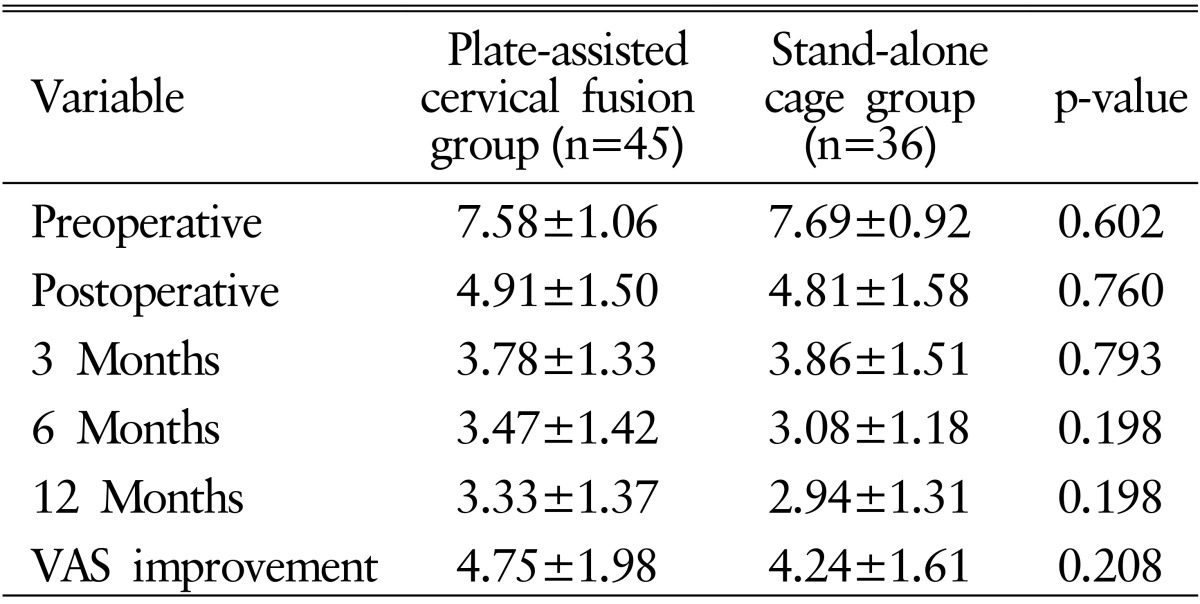
3. Pain Score
The patients clinical symptom, especially pain showed no statistically difference in preoperative, immediate postoperative, 3-month, 6-month, and 12-month follow-up between the 2 groups (Table 3). Pain score during 12 months has improved in both groups. And mean preoperative pain score was 7.58±1.06 vs. 7.69±0.92 and 12-month follow-up pain score was 3.33±1.37 vs. 2.94±1.31. The mean pain improvement was 4.75±1.98 vs. 4.24±1.61. There was no significant difference between 2 groups (p=0.208).
Table 3. Pain results of the 2 groups.
Values are presented as mean±standard deviation.
VAS, visual analog scale.
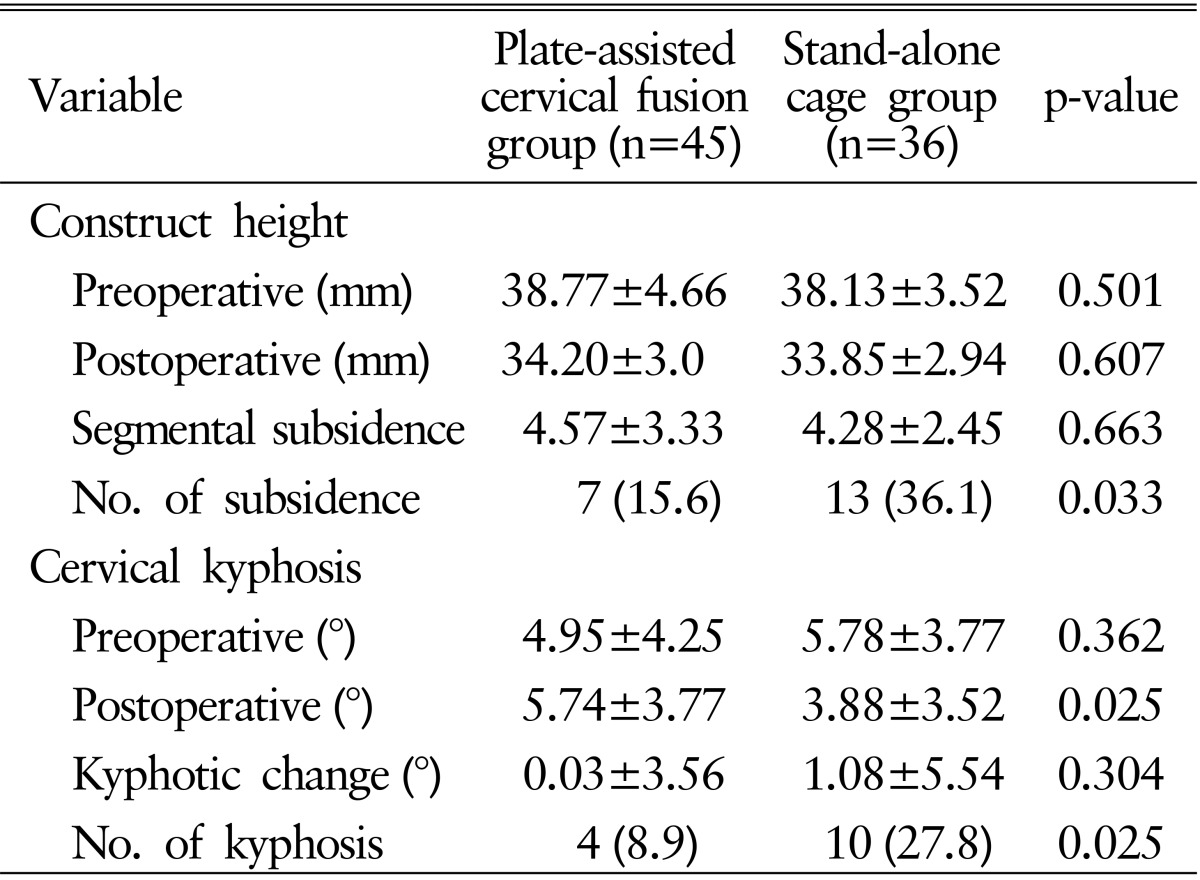
4. Segmental Subsidence
Thirteen out of 36 patients (36.1%) were found the segmental subsidence in stand-alone cage group. Mean segmental subsidence was 4.28±2.45mm during 12-month follow-up. But only 7 out of 45 patients (15.6%) were founded the segmental subsidence in plate-assisted cervical fusion group. Mean segmental subsidence was 4.57±3.33mm. Subsidence occurrence rate was statistically different between the 2 groups (p=0.033) (Table 4).
Table 4. Comparison of the radiologic results between the plate-assisted cervical fusion group and stand-alone cage group.
Values are presented as mean±standard deviation or number (%).
5. Segmental Cervical Kyphosis
Segmental cervical kyphosis was also different between the 2 groups. Ten out of 36 patients (27.8%) were showed cervical kyphosis on stand-alone cage group. On the other hand, 4 out of 45 patients (8.9%) showed cervical kyphosis on plate-assisted cervical fusion group. Mean cervical kyphotic change is 1.08°±5.54° vs. 0.03°±3.56°. Between the 2 groups, segmental cervical kyphosis occurrence rate was statistically different (p=0.025) (Table 4).
DISCUSSION
ACDF is widely accepted surgical procedure for the treatment of cervical spinal degenerative disease6,10,26,29). However, the classic method of Cloward9) and Smith and Robinson36) using an autologous tricortical iliac bone graft has been reported to have problems of donor site morbidity1,35) and subsidence34,40). In order to overcome those problems, ACDF using an intervertebral cage has been recently used with favorable results42).
Stand-alone intervertebral cages can be effective for restoring the intervertebral disc height and lordosis, providing loadbearing support to the anterior column and preventing graft collapse21,23). But nowadays stand-alone cage also reported problems. For example, nonunion and subsidence into the endplates have been reported as the complications of these procedures5,14,23,27,32,39). And some surgeons advocated that plateassisted cervical fusion shows better outcomes than stand-alone cages. So, we designed retrospective study to compare clinical and radiologic outcomes between 2 groups.
Many authors reported that the clinical outcomes between the stand-alone cages and the anterior cervical plates for cervical degenerative disease were similar13,19,20,32). Our study also showed no statistically different between 2 groups on pain score improvement. But, short-term follow-up and short segment surgery can affect this result.
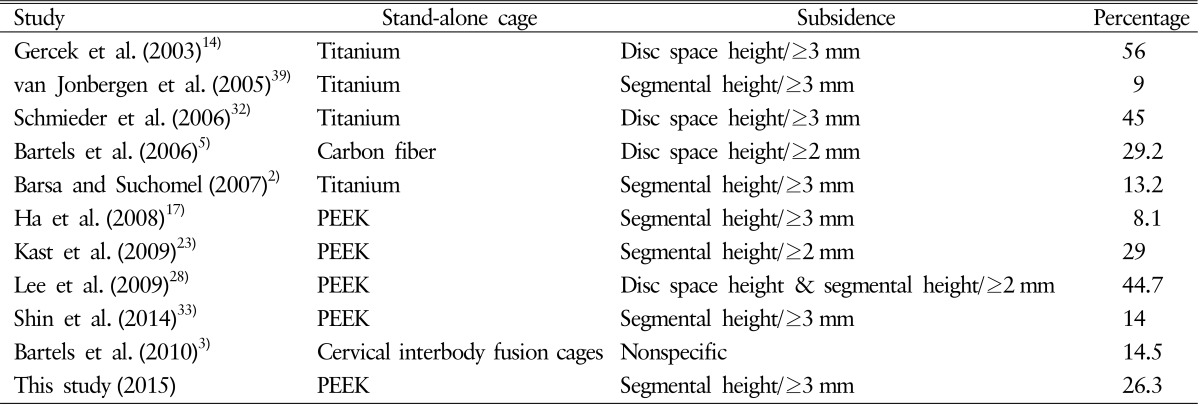
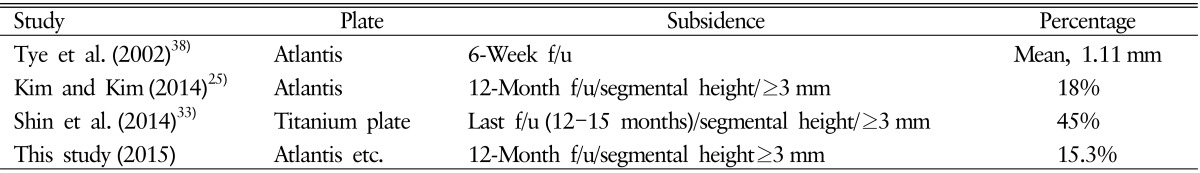
There are some studies compared to stand-alone cages and cervical plating system radiologic outcomes. Bartels et al.5) reported 29.2% subsidence rate in stand-alone cage group for 6-week follow-up. And Yang et al.42) reported over 3-mm cage subsidence have occurred 14.9% rate (n=51). Our stand-alone cage group subsidence rate is 36.1%. This rate is similar to previous studies (Table 5). In addition, Kim et al.25) reported subsidence rate of 18% in plate-assisted cervical fusion at postoperative 1-year follow-up (n=48). Our plate-assisted cervical fusion group subsidence rate is 15.6%(Table 6). These results are also similar to the other studies. As a result, plate-assisted cervical fusion group's segmental subsidence rate is lower than stand-alone cage group.
Table 5. Summary of the studies on stand-alone cage grafts subsidence.
PEEK cage (Solis, Stryker Spine, Allendale, NJ, USA).
Table 6. Summary of the studies on plate-assisted allograft subsidence.
f/u, follow-up.
Even though many studies reported subsidence does not always result in poor prognosis or aggravation of symptoms and mostly does not cause symptoms or morbidity32,42,43), intervertebral disc height loss can eventually result in narrowing of the foramen, nerve root compression, pseudoarthrosis due to cervical instability4,17). It means that segmental subsidence arouses significant morbidity on postoperative period.
Similar tendency was also observed on cervical lordosis. It shows also this kind of tendency. Barsa and Suchomel2) have studied stand-alone cage group cervical angulation after 6-month postoperative follow-up. They reported that using Cobb angle resulted about 8.7° loss of segmental lordosis. Also Yang et al.42) have studied average 1.58° cervical angulation change from immediate postoperative to last follow-up stand-alone cage group. And 29.8% of them changed over 3°. Our studies show that cervical kyphosis was resulted 15.8% in stand-alone cage group and 7.6% plate-assisted cervical fusion group. This result indicates not only segmental subsidence but also cervical kyphosis occurrence rate is much higher in stand-alone cage group. Cervical kyphosis can occur disc space narrowing and adjacent segment degeneration24,30).
These results mean that plate-assisted cervical fusion is good alternative of stand-alone cages cervical fusion in degenerative cervical disease. Some studies reported plate-assisted cervical fusion has the drawbacks of high cost, a long operative time, and risk to adjacent structures because of the retraction required for plate insertion41). But the incidence of postoperative complication rate is relatively low and most symptoms were improved as time goes by33).
Plate-assisted cervical fusion group can prevent cage subsidence and cervical kyphosis, even though some author insist radiological results cannot influence clinical outcomes. And there was no statistical difference in pain scores between 2 groups. The results are only limited to short segment and short-term follow-up. We inference long segment fusion resulted more difference than short segment groups. And if time passes, segmental kyphosis affect cervical sagittal imbalance more. Long-term follow-up anticipate pessimistic results.
However, currently we apply only limited plate-assisted cervical fusion because of National Health Insurance does not allow using 2 devices at once. But, this policy can result poor outcome and spend more socioeconomic cost of disease.
Unfortunately, this study has some limitations. This is retrospective study showing somewhat selection bias. And we did not consider implanted cage size and cage migration and surgical technique. Barsa and Suchomel2) reported they are affected cage subsidence and sagittal imbalance. Another weakness of our study did not consider other clinical symptoms (except pain). And short segment fusion (one level), relatively short-term follow-up (12 months) were also limitation of this study. But there are little study direct compare to stand-alone cage group and plate-assisted cervical fusion group. Especially, comparison on subsidence and kyphosis at the same time is strong point of our study.
CONCLUSION
A retrospective review was performed on 81 patients undergoing stand-alone cage group and plate-assisted cervical fusion group. Pain results between 2 groups showed no statistical differences but radiological results showed differences between 2 groups. Stand-alone cage group were much more provoked than plate-assisted cervical fusion group in segmental subsidence and cervical kyphosis. So plate-assisted cervical fusion is good alternative for fusion in patients with cervical degenerative diseases.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity A statistical evaluation. Spine (Phila Pa 1976) 1995;20:1055–1060. doi: 10.1097/00007632-199505000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007;16:1395–1400. doi: 10.1007/s00586-006-0284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartels RH, Beems T, Schutte PJ, Verbeek AL. The rationale of postoperative radiographs after cervical anterior discectomy with stand-alone cage for radicular pain. J Neurosurg Spine. 2010;12:275–279. doi: 10.3171/2009.9.SPINE09263. [DOI] [PubMed] [Google Scholar]
- 4.Bartels RH, Donk R, van Azn RD. Height of cervical foramina after anterior discectomy and implantation of a carbon fiber cage. J Neurosurg. 2001;95(1 Suppl):40–42. doi: 10.3171/spi.2001.95.1.0040. [DOI] [PubMed] [Google Scholar]
- 5.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58:502–508. doi: 10.1227/01.NEU.0000197258.30821.50. [DOI] [PubMed] [Google Scholar]
- 6.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Botelho RV, Dos Santos Buscariolli Y, de Barros Vasconcelos Fernandes Serra MV, Bellini MN, Bernardo WM. The choice of the best surgery after single level anterior cervical spine discectomy: a systematic review. Open Orthop J. 2012;6:121–128. doi: 10.2174/1874325001206010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 9.Cloward RB. The anterior approach for removal of ruptured cervical disks. 1958. J Neurosurg Spine. 2007;6:496–511. doi: 10.3171/spi.2007.6.5.496. [DOI] [PubMed] [Google Scholar]
- 10.Connolly PJ, Esses SI, Kostuik JP. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord. 1996;9:202–206. [PubMed] [Google Scholar]
- 11.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–2317. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 12.Fowler BL, Dall BE, Rowe DE. Complications associated with harvesting autogenous iliac bone graft. Am J Orthop (Belle Mead NJ) 1995;24:895–903. [PubMed] [Google Scholar]
- 13.Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008;15:1017–1022. doi: 10.1016/j.jocn.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of standalone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003;12:513–516. doi: 10.1007/s00586-003-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976) 1984;9:667–671. doi: 10.1097/00007632-198410000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res. 1997;(339):76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Ha SK, Park JY, Kim SH, Lim DJ, Kim SD, Lee SK. Radiologic assessment of subsidence in stand-alone cervical polyetheretherketone (PEEK) cage. J Korean Neurosurg Soc. 2008;44:370–374. doi: 10.3340/jkns.2008.44.6.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hida K, Iwasaki Y, Yano S, Akino M, Seki T. Long-term follow-up results in patients with cervical disk disease treated by cervical anterior fusion using titanium cage implants. Neurol Med Chir (Tokyo) 2008;48:440–446. doi: 10.2176/nmc.48.440. [DOI] [PubMed] [Google Scholar]
- 19.Huh J, Oh JY, Chough CK, Cho CB, Joo WI, Park HK. Polyetheretherketone cage filled with beta-tricalcium phosphate versus autogenous tricortical iliac bone graft in anterior cervical discectomy and fusion. Korean J Spine. 2011;8:165–171. [Google Scholar]
- 20.Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc. 2010;48:342–346. doi: 10.3340/jkns.2010.48.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kandziora F, Pflugmacher R, Schäfer J, Born C, Duda G, Haas NP, et al. Biomechanical comparison of cervical spine interbody fusion cages. Spine (Phila Pa 1976) 2001;26:1850–1857. doi: 10.1097/00007632-200109010-00007. [DOI] [PubMed] [Google Scholar]
- 22.Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E. Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg. 2009;111:18–27. doi: 10.1016/j.clineuro.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 2009;32:207–214. doi: 10.1007/s10143-008-0168-y. [DOI] [PubMed] [Google Scholar]
- 24.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SJ, Kim SD. Anterior cervical discectomy and fusion using a double cylindrical cage versus an anterior cervical plating system with iliac crest autografts for the treatment of cervical degenerative disc disease. J Korean Neurosurg Soc. 2014;55:12–17. doi: 10.3340/jkns.2014.55.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kolstad F, Nygaard ØP, Andresen H, Leivseth G. Anterior cervical arthrodesis using a "stand alone" cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 2010;35:1545–1550. doi: 10.1097/BRS.0b013e3181d259c1. [DOI] [PubMed] [Google Scholar]
- 27.Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007;7:205–209. doi: 10.1016/j.spinee.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Lee SH, Suk KS, Kim KT, Lee JH, Seo EM, Im YS. Outcome analysis of single level anterior cervical fusion using interbody PEEK cage with autologous iliac bone graft. J Korean Orthop Assoc. 2009;44:93–101. [Google Scholar]
- 29.Lind BI, Zoega B, Rosén H. Autograft versus interbody fusion cage without plate fixation in the cervical spine: a randomized clinical study using radiostereometry. Eur Spine J. 2007;16:1251–1256. doi: 10.1007/s00586-007-0337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oda I, Cunningham BW, Buckley RA, Goebel MJ, Haggerty CJ, Orbegoso CM, et al. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine (Phila Pa 1976) 1999;24:2139–2146. doi: 10.1097/00007632-199910150-00014. [DOI] [PubMed] [Google Scholar]
- 31.Riley LH, Jr, Robinson RA, Johnson KA, Walker AE. The results of anterior interbody fusion of the cervical spine. Review of ninety-three consecutive cases. J Neurosurg. 1969;30:127–133. doi: 10.3171/jns.1969.30.2.0127. [DOI] [PubMed] [Google Scholar]
- 32.Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006;4:447–453. doi: 10.3171/spi.2006.4.6.447. [DOI] [PubMed] [Google Scholar]
- 33.Shin JS, Oh SH, Cho PG. Surgical outcome of a zero-profile device comparing with stand-alone cage and anterior cervical plate with iliac bone graft in the anterior cervical discectomy and fusion. Korean J Spine. 2014;11:169–177. doi: 10.14245/kjs.2014.11.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion. A prospective randomised study. J Bone Joint Surg Br. 2003;85:1019–1025. doi: 10.1302/0301-620x.85b7.13398. [DOI] [PubMed] [Google Scholar]
- 35.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2003;28:134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 36.Smith GW, Robinson RA. The treatment of certain cervicalspine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 37.Thorell W, Cooper J, Hellbusch L, Leibrock L. The long-term clinical outcome of patients undergoing anterior cervical discectomy with and without intervertebral bone graft placement. Neurosurgery. 1998;43:268–273. doi: 10.1097/00006123-199808000-00050. [DOI] [PubMed] [Google Scholar]
- 38.Tye GW, Graham RS, Broaddus WC, Young HF. Graft subsidence after instrument-assisted anterior cervical fusion. J Neurosurg. 2002;97(2 Suppl):186–192. doi: 10.3171/spi.2002.97.2.0186. [DOI] [PubMed] [Google Scholar]
- 39.van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW. Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J. 2005;5:645–649. doi: 10.1016/j.spinee.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A. A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine (Phila Pa 1976) 2002;27:1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 41.Whitecloud TS., 3rd Modern alternatives and techniques for one-level discectomy and fusion. Clin Orthop Relat Res. 1999;(359):67–76. doi: 10.1097/00003086-199902000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3:16–23. doi: 10.4055/cios.2011.3.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976) 1991;16:726–729. doi: 10.1097/00007632-199107000-00006. [DOI] [PubMed] [Google Scholar]