Highlights
-
•
The physiological reserve of extreme elderly patients is very limited.
-
•
Point-of-Care Ultrasound is very useful in the management of critically-ill elderly patients.
-
•
Point-of-Care Ultrasound shortened the time to surgery.
-
•
Point-of-Care Ultrasound early diagnosed internal bleeding despite what appeared haemodynamic stability.
-
•
Point-of-Care Ultrasound helped in guiding the resuscitation.
Abbreviation: POCUS, Point-of-Care Ultrasound
Key words: Strangulated, Epigastric hernia, Point-of-care, Ultrasound, Elderly, Critical care
Abstract
Introduction
The physiological reserve of extreme elderly patients is very limited and has major impact on clinical decisions on their management. Hereby we report a 90-year-old man who presented with a strangulated epigastric hernia and who developed postoperative intra-abdominal bleeding, and highlight the value of Point-of-Care Ultrasound (POCUS) in critical decisions made during the management of this patient.
Presentation of case
A 90-year-old man presented with a tender irreducible epigastric mass. Surgeon-performed POCUS using colour Doppler showed small bowel in the hernia with no flow in the mesentery. Resection anastomosis of an ischaemic small bowel and suture repair of the hernia was performed. Twenty four hours after surgery, in a routine follow up using POCUS, significant intra-peritoneal fluid was detected although the patient was haemodynamically stable. The fluid was tapped under bedside ultrasound guidance and it was frank blood. During induction of anaesthesia for a laparotomy, the patient became hypotensive. Resuscitation under inferior vena cava sonographic measurement, followed by successful damage control surgery with packing, was performed. 36 h later, the packs were removed, no active bleeding could be seen and the abdomen was closed without tension. The patient was discharged home 50 days after surgery with good general condition.
Conclusion
POCUS has a central role in the management of critically-ill elderly patients for making quick critical decisions.
1. Introduction
Managing a strangulated epigastric hernia in extreme elderly patients is more complex than the surgical technique itself. The physiological reserve of these patients is very limited and has major impact on clinical decisions when taking care of them. Minor complications may have serious effects because of the lack of their physiological reserve. Point-of-Care Ultrasound (POCUS) has become a very useful tool for the diagnosis, resuscitation, and postoperative critical care [1]. It is an extension of the clinical examination and a tool for evaluating the haemodynamic status of patients [2]. Hereby we report a 90-year-old man who presented with a strangulated epigastric hernia and who developed postoperative intra-abdominal bleeding. We will highlight the importance of POCUS in critical decisions made during the management of this patient.
2. Case report
A 90-year-old man was admitted to our hospital complaining of a painful epigastric mass and vomiting of one day duration. He had a reducible epigastric hernia for twenty years. On abdominal examination, the mass was tender and irreducible (Fig. 1A). Surgeon-performed POCUS showed small bowel in the hernia. Colour Doppler showed no flow in the mesentery of the bowel (Fig. 1B). The patient was admitted to the hospital with a diagnosis of strangulated epigastric hernia. A decision for surgery was made. Through a transverse skin incision, the hernial sac was opened. The strangulated small bowel was dusky, haemorrhagic and not contracting (Fig. 2A). Ten cm of the small bowel was resected. End-to-end anastomosis using vicryle 3/0 was performed (Fig. 2B). There was a big defect in the abdominal fascia which was difficult to close. A mesh could not be used because of the resection of the small bowel and risk of infection. The fascia was released from the lateral sides. The defect could be directly closed by interrupted prolene sutures 2/0.
Fig. 1.

A 90-year-old man presented with a tender irreducible epigastric mass (Fig. 1A). Surgeon performed Point-of-care Ultrasound (Fig. 2B) showed that it was a hernia containing small bowel (SB) which was strangulated because of the narrow neck of the hernia (yellow arrow heads). Colour Doppler showed no flow in the mesentery of the bowel (black arrow).
Fig. 2.
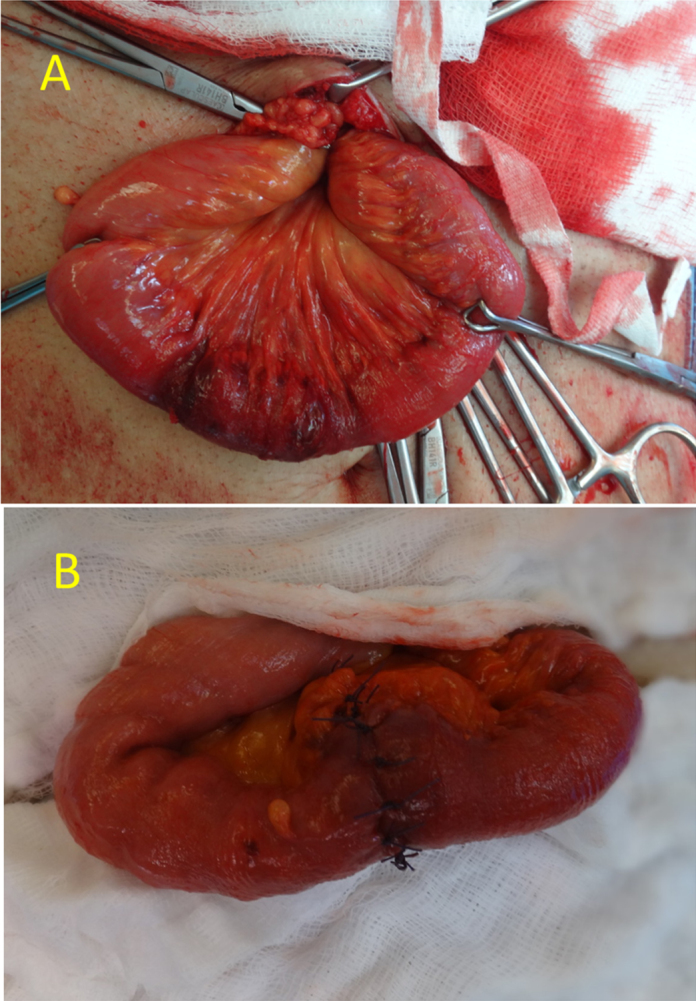
Surgical exploration of the hernial sac showed that the strangulated small bowel was dusky, haemorrhagic and not contracting (Fig. 2A). Ten cm of the small bowel was resected and end-to-end anastomosis was performed (Fig. 2B).
24 h after surgery, in a routine follow up using POCUS, post-operative intra-peritoneal fluid was seen (about 1.5 L) (Fig. 3A). The fluid was tapped to decide its nature. It was frank blood (Fig. 3B). The patient was haemodynamically stable having a blood pressure of 145/65 mmHg, a pulse of 95 bpm but low urine output (20 ml/ h). Despite that, it was decided that it is safer to re-explore the abdomen through a laparotomy because of the old age of the patient. During induction of anaesthesia, the patient became hypotensive (blood pressure of 40/20 mmHg). Damage control resuscitation was performed under inferior vena cava sonographic measurement till blood pressure picked up quickly (Fig. 4A–B). Laparotomy was performed. There was 1.5 L of fresh blood which was removed but no definite major bleeder could be seen. Since the patient was fragile, damage control surgery was decided. The abdominal cavity was packed with abdominal towels and the skin was closed by towel clips. Damage control resuscitation continued on the surgical table. Four pints packed RBC and 4 FFP with a ratio of 1:1 were given on the theatre. The patient was transferred to the ICU when he became haemodynamically stable (BP of 110/70 mm Hg). The hypotensive period was less than 10 min.
Fig. 3.
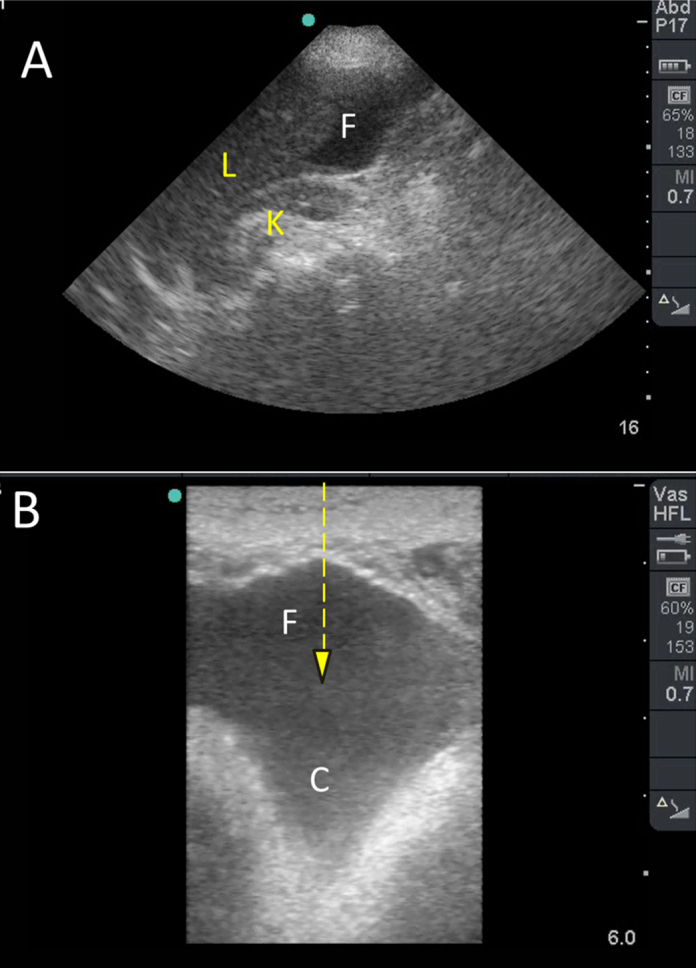
A routine follow Point-of-care Ultrasound by a portable ultrasound machine (Fig. 3A) showed significant intra-peritoneal fluid (F) although the patient was haemodynamically stable. Using a linear probe with a frequency of 10–12 MHz (Fig. 3B), the intra-peritoneal fluid turned out to be heterogeneous. The deep areas of the fluid were more echogenic indicating clotted blood (C). The fluid (F) was tapped under ultrasound guidance (hashed arrow) and it was frank blood.
Fig. 4.

Preoperative IVC measurement (82 mm) showed that the patient was hypovolaemic (Fig. 4A). Aggressive resuscitation using crystalloids, blood and fresh frozen plasma was performed under repeated measurement of IVC diameter. IVC increased to 164 mm (Fig. 4B). The patient blood pressure increased from 40/20 mmHg to 110/70 mmHg.
The patient was admitted to the ICU for damage control resuscitation. On arrival to the ICU, his blood pressure was 118/79 mm Hg, his pulse was 130 bpm, and his temperature was 35 °C. Arterial pH was 7.33 and coagulation profile was normal. Platelets were 118 000 per microliter of blood, and haemoglobin was 11.6 g/dl. Acidosis and hypothermia were successfully corrected over a period of 36 h. The patient was taken for a second look laparotomy as planned. Packs were removed. The abdomen was explored and there was no active bleeding. It was judged that the bleeding occurred from a small bleeder from the abdominal wall possibly from ligamentum teres. The abdominal wall was closed without tension with continuous PDS loops/1. Skin was closed by clips.
The patient was kept in the ICU for further care. During the ICU stay, the patient had bowel motion. His abdominal wound was clean and healed nicely without evidence of a hernia. The patient was ventilated for one week. He developed ventilator associated pneumonia, and mild diarrhoea caused by clostridia diffcile infection. Infectious complications were successfully treated with proper antibiotics. The patient responded well and his level of care was escalated down according to his clinical status with improvement of respiratory and nutritional function. The patient was discharged home 50 days after surgery fully conscious and on normal diet.
3. Discussion
Strangulated epigastric hernias are extremely rare especially true ones having a hernial sac. Epigastric hernias may exist for long time reaching up to 45 years [3] and reach large sizes before getting strangulated [4]. Furthermore, a sudden unexplained strangulation in an elderly patient may indicate sudden increased intra-abdominal pressure possibly caused by more serious conditions like rupture aortic aneurysm [3] or perforated hollow organs associated with ileus [5].
Our patient was 90-year-old who had an ischaemic bowel that needed resection anastomosis. Furthermore, he had a stormy postoperative period due to bleeding. Despite that, he survived without residual complications. We could find only two patients in the literature having an age of more than 85 years who had a strangulated epigastric hernia. Goldman et al. [6] reported a 96-year-old patient who had a strangulated gall bladder which was viable. It was reduced and the hernia was repaired. Angel et al. [7] reported a 95-year-old patient who had a strangulated gastric antrum which was viable. The antrum was reduced and the hernia was repaired. Both patients survived. Improved medical care is associated with increased aged population. More than one-fifth of the world’s population is anticipated to be older than 60 years by 2050 [8]. Age older than 50 years increases the risk of incarceration of non inguinal abdominal wall hernias [9]. The incarcerated epigastric hernia which is located in the upper abdomen may contain an ischaemic bowel as occurred in our patient. Elderly may have decreased physiological reserve and associated comorbidities which poorly impact their clinical outcome [10].
Diagnosis of the contents of strangulated hernias is sometimes difficult. They may present with redness of the skin that mimics an abscess [11]. CT scan is helpful in defining the contents of the strangulated hernia [7], [11]. Nevertheless, it may need oral contrast, have a radiation effect, and may delay surgery. The risk of radiation is not a concern in the elderly. Nevertheless, time to surgery is very important. POCUS proved to be a very useful tool in the diagnosis of the contents of the hernia in our patient. It clearly showed that the mesenteric blood flow was compromised. The combined clinical and sonographic findings helped in making a quick surgical decision.
Using POCUS by non-radiologists to make critical decisions for managing life-threatening conditions is becoming more popular. POCUS is an accurate, quick, and non-invasive, beside diagnostic tool that can be repeated without risk of radiation. Majority of critical care physicians are keen to learn and practice POCUS. We think that ultrasound worked as a saving kit at three points in the management of our patient: the early decision for the first surgery, the early decision for abdominal re-exploration, and the guidance of an on Table resuscitation.
Detecting intra-peritoneal fluid is an easy skill to learn by non radiologists if properly trained [12]. The sensitivity of ultrasound in detecting intra-peritoneal fluid is very high reaching up to 100% [13]. Nevertheless, ultrasound cannot usually differentiate between different types of fluid [13]. Intra-peritoneal fluid in our patient had heterogeneous sonographic echogenity suggesting that it was clotted blood. Fresh blood is usually hypoechoic while clotted blood is echogenic [14]. Intra-peritoneal fluid in a hypotensive patient is most probably blood. Our patient was not hypotensive so we needed to tap the fluid under ultrasound guidance to confirm the diagnosis. We think that the bleeding occurred from the ligamentum teres, an epigastric artery, or tear of the rectus muscle [15].
The measurement of IVC diameter is a very useful tool in evaluating the shock status [2]. It should be correlated with the clinical picture as a whole. We have used the longitudinal B mode to measure the IVC diameter in the present patient. IVC diameter was very useful in guiding resuscitation and in defining fluid requirements during the ICU stay.
In summary, our present case highlights the important role of POCUS in making critical decisions that have serious consequences. POCUS shortened the time to surgery, early diagnosed internal bleeding despite what appeared haemodynamic stability, and helped in guiding the resuscitation in an extreme elderly patient. Although, the results of ultrasound are operator dependable, this case clearly supports the need to train surgeons and critical care physicians so that they can master this important bedside diagnostic tool.
Consent
The caregiver of the patient gave her written consent to report his case.
Conflict of interests
None declared by all authors.
Author contribution
Fikri Abu-Zidan was the treating surgeon, performed the Point-of Care Ultrasound studies, had the idea, read the literature, wrote the first version of the paper, edited it, and approved its final version. Kamal Idris managed the patient in the ICU, participated in the idea, and approved the final version of the paper. Mohammed Khalifa managed the patient in the ward, participated in the idea, drafted the case report and approved the final version of the paper.
Ethical approval
The caregiver of the patient gave her written consent to report his case according to our hospital policy.
Funding
None.
Contributor Information
Fikri M. Abu-Zidan, Email: fabuzidan@uaeu.ac.ae.
Kamal Idris, Email: kidrees@seha.ae.
Mohammed Khalifa, Email: melhassan@seha.ae.
References
- 1.Abu-Zidan F.M. Point-of-care ultrasound in critically ill patients: where do we stand? J. Emerg. Trauma Shock. 2012;5:70–71. doi: 10.4103/0974-2700.93120. (PMID: 22416159) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abu-Zidan F.M. Optimizing the value of measuring inferior vena cava diameter in shocked patients. World J. Crit. Care Med. 2016;5:7–11. doi: 10.5492/wjccm.v5.i1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falgout H.J., Fendley S.M., Walker H., Ferrara J.J. Ruptured abdominal aortic aneurysmapresenting as incarcerated epigastric hernia—a case report. Vasc. Endovascular Surg. 1989;23:59–62. [Google Scholar]
- 4.Scheel M.J., Mateo R.B., Doyle H.R., Atwell R.B. Incarcerated ventral (epigastric) hernia containing a strangulated Meckel’s diverticulum. Hernia. 1999;3:225–227. [Google Scholar]
- 5.Adrid A.S., Ulin A.W. Perforated peptic ulcer presenting as acutely strangulated epigastric hernia. J. Albert Einstein Med. Cent. (Phila) 1961;9:206–209. (PMID: 13681543) [PubMed] [Google Scholar]
- 6.Goldman G., Rafael A.J., Hanoch K. Acute acalculous cholecystitis due to an incarcerated epigastric hernia. Postgrad. Med. J. 1985;61:1017–1018. doi: 10.1136/pgmj.61.721.1017. (PMID: 4070111) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pagnozzi Angel J., Ugalde P., Perez Lopez F., Fernández Fernández J.C. Epigastric hernia with gastric antrum incarceration. Cir. Esp. 2015;93:e9. doi: 10.1016/j.ciresp.2014.09.013. (PMID: 25458548) [DOI] [PubMed] [Google Scholar]
- 8.United Nations Population Division, Department of Economics and Social Affairs, World Population Aging 2009 New York Website:http://www.un.org/esa/population/publications/WPA2009/WPA2009_WorkingPaper.pdf (accessed on 02.02.16).
- 9.Lau B., Kim H., Haigh P.I., Tejirian T. Obesity increases the odds of acquiring and incarcerating noninguinal abdominal wall hernias. Am. Surg. 2012;78:1118–1121. (PMID: 23025954) [PubMed] [Google Scholar]
- 10.Sterling D.A., O'Connor J.A., Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J. Trauma. 2001;50:116–119. doi: 10.1097/00005373-200101000-00021. (PMID: 11231681) [DOI] [PubMed] [Google Scholar]
- 11.Kim R., McCoy M., Bistolarides P., Merchant A.M. Richter's epigastric hernia with transverse colon strangulation. Am. Surg. 2012;78:E301–E303. (PMID: 22691339) [PubMed] [Google Scholar]
- 12.Mohammad A., Hefny A.F., Abu-Zidan F.M. Focused assessment sonography for trauma (FAST) training: a systematic review. World J. Surg. 2014;38:1009–1018. doi: 10.1007/s00268-013-2408-8. (PMID: 24357247) [DOI] [PubMed] [Google Scholar]
- 13.Radwan M.M., Abu-Zidan F.M. Focussed Assessment Sonograph Trauma (FAST) and CT scan in blunt abdominal trauma: surgeon’s perspective. Afr. Health Sci. 2006;6:187–190. doi: 10.5555/afhs.2006.6.3.187. (PMID:17140344) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abu-Zidan F.M., Hefny A.F., Corr P. Clinical ultrasound physics. J. Emerg. Trauma Shock. 2011;4:501–503. doi: 10.4103/0974-2700.86646. (PMID: 22090745) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatjipetrou A., Anyfantakis D., Kastanakis M. Rectus sheath hematoma: a review of the literature. Int. J. Surg. 2015;13:267–271. doi: 10.1016/j.ijsu.2014.12.015. (PMID: 25529279) [DOI] [PubMed] [Google Scholar]


