Abstract
Background
Daily low‐dose aspirin is recommended for primary prevention of myocardial infarction and stroke in higher‐risk patients. Population trends in aspirin use for cardiovascular disease (CVD) prevention in an urban population (Minneapolis/St. Paul, 2010 population 2.85 million) from 1980 to 2009 were evaluated.
Methods and Results
Surveys of randomly selected adults aged 25 to 74 years were collected at 5‐year intervals. Self‐reports of regular aspirin use for CVD prevention and history of CVD were obtained. Six cross‐sectional surveys included 12 281 men and 14 258 women. Age‐adjusted aspirin use for primary prevention increased during this period from 1% to 21% among men and 1% to 12% among women. Aspirin use was highest in those aged 65 to 74 years. For secondary prevention, age‐adjusted aspirin use increased from 19% to 74% among men and 11% to 64% among women. While data are based on self‐report, a substudy using a biochemical indicator of aspirin use (serum thromboxane B2) supports the validity of self‐report.
Conclusions
Aspirin for CVD prevention is commonly used by a large and growing portion of the general population. It is not known if this is based on professional advice or self‐prescribed use. It is also likely that many who would benefit do not use aspirin and others use aspirin inappropriately.
Keywords: aspirin, epidemiology, prevention
Subject Categories: Epidemiology, Primary Prevention, Secondary Prevention, Platelets, Intracranial Hemorrhage
Introduction
Cardiovascular disease (CVD), specifically acute myocardial infarction (AMI) and stroke, are the leading causes of disability and death in the United States.1 While significant progress in the prevention, detection, and treatment of these diseases is apparent, much remains to be done to control the epidemic.
The most effective approaches to reducing CVD are strategies shown to prevent first and recurrent events. The reduction of cigarette smoking, control of hypertension, cholesterol lowering, and selective use of revascularization strategies after a CVD event all contribute to observed reductions in morbidity and mortality.2
One well‐studied prevention approach is the use of low‐dose aspirin. Aspirin is widely accepted for secondary prevention after a myocardial infarction or stroke.3 After review of data from multiple prospective randomized clinical trials,4, 5, 6 the United States Preventive Services Task Force (USPSTF) in 2009 published a strong 1A recommendation in favor of use of low‐dose aspirin for primary prevention in men aged 45 to 79 years and women aged 55 to 79 years in whom benefit would be anticipated to exceed risk.7 The recommendation in favor of aspirin use was also included in an American Heart Association prevention guidelines,8, 9, 10, 11 the recent Healthy People 2020 plan,12 and the “Million Hearts Initiative” of the Centers for Medicare and Medicaid Services and Centers for Disease Control and Prevention.13
These recommendations remain controversial, despite the paucity of new evidence to define the relative benefit and risk of such aspirin use. Further, while prescription of aspirin for primary prevention, defined by population‐based aspirin use surveys, resulted in increases in use over relatively short periods in selected populations, newer studies have not provided the associated cardiovascular ischemic event rates or rates of hemorrhagic adverse events.14, 15, 16, 17, 18
The present study evaluates long‐term trends in regular aspirin use in the population of a large metropolitan area from 1980 to 2009. These data describe population trends in the regular use of aspirin for both primary and secondary prevention.
Methods
The Minnesota Heart Survey (MHS) performs cross‐sectional risk factor and health behavior surveys of noninstitutionalized resident adults aged 25 to 74 years in the 7‐county Minneapolis/St. Paul metropolitan area (2010 census 2.85 million). Surveys were conducted in 1980–1982, 1985–1987, 1990–1992, 1995–1997, 2000–2002, and 2007–2009. The metropolitan population is predominantly white and has higher education and employment levels than the overall US population. The MHS obtains a random sample of the metropolitan area population by using methods described in detail elsewhere.19, 20 In brief, a 2‐stage cluster design was created from census maps with the 7‐county metropolitan area divided into 704 clusters of ≈1000 households each. Forty clusters were selected randomly and used for each survey, with a sample of households randomly selected from within each cluster. The sampling fraction (5% to 10%) varied between surveys based on resources. There were previously described small differences in the sampling methodology between surveys.21 An initial home interview solicited information on health status, health behaviors, and medication use. A visit to a survey center in a nearby clinic, public building, or university clinical center followed. The information on aspirin use was collected in the home interview.
Participation rates for the home interview ranged from 67% to 91% of the selected households, with rates declining over time.
The questions asked of the participants and relevant to this study are shown in Figure 1. Those who were classified as aspirin users were participants who reported they were taking aspirin on a regular basis. They were further categorized to define when such use was for the purpose of preventing heart attack and stroke or other reasons. To determine whether aspirin was taken for primary or secondary prevention, the question was asked, “Have you ever been hospitalized for a heart attack or stroke?” Those subjects who responded positively were classified as secondary prevention aspirin users.
Figure 1.
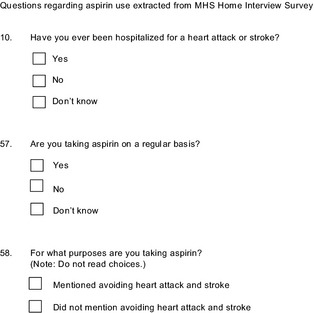
Survey Questionnaire showing only questions related to this study. MHS indicates Minnesota Heart Survey.
Self‐report of any medication use, including aspirin, may be inaccurate because it may be considered a socially desirable behavior subject to overreporting.22 However, in a previous study, self‐reported aspirin use was biochemically validated in a similar population sample.23
Unadjusted frequencies of aspirin use were reported according to sex and 10‐year age group. Age‐adjusted prevalence of aspirin use were estimated using generalized linear mixed models with a logit link and included a random‐effects term to account for the cluster design. Trend analyses were conducted within sex and primary and secondary CVD prevention strata by adding a term for survey year to the regression model. Data on hospitalization for gastrointestinal (GI) bleeding, AMI, and stroke subtype were obtained from the comprehensive Minnesota Hospital Association's administrative claims database (http://www.mnhospitals.org/data-reporting/data-products-services/administrative-claims-database). Only the 7‐county metropolitan area hospitals, the same area covered by the survey, were queried for the relevant diagnostic codes. SAS software version 9.3 was used for all analyses (SAS Institute Inc).
This study was approved by the institutional review board of the University of Minnesota, and all participants signed an informed consent form. The authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Results
The 6 cross‐sectional surveys included a total of 12 281 men and 14 258 women aged 25 to 74. Of these, 547 (4%) of men and 317 (2%) of women reported hospitalization for a myocardial infarction and/or stroke and constitute the secondary prevention group.
Age‐adjusted aspirin use for CVD prevention is shown in Figure 2. For men, prevalence of aspirin use for primary CVD prevention rose steadily from 3.7% in 1980–1982 to 20.8% in 2007–2009. Among women, regular aspirin use for primary CVD prevention in the population rose steadily from 1.0% in 1980–1982 to 12.0% in 2007–2009.
Figure 2.
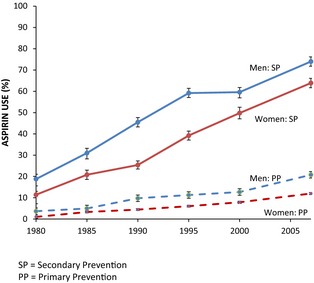
Trends in aspirin use for preventing CVD in PP and SP, by sex. Values are mean±SE and are plotted at the beginning year of each survey. CVD indicates cardiovascular disease; PP, primary prevention; SP, secondary prevention.
The use of aspirin for primary CVD prevention was strongly associated with age, as shown in Tables 1 and 2, and increased markedly over time among those aged 45 years and older. The use of aspirin for secondary CVD prevention increased in all except the youngest age group (ages 25–34) (Tables 3 and 4). Men were consistently more likely to use aspirin than were women at any age.
Table 1.
Aspirin Use for Primary CVD Prevention in Men
| Survey Year | ||||||
|---|---|---|---|---|---|---|
| 1980–1982 | 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | |
| Age, y | ||||||
| 25–34 | 1/332 (0.3) | 9/948 (0.9) | 11/944 (1.2) | 17/781 (2.2) | 8/332 (2.4) | 3/270 (1.1) |
| 35–44 | 0/184 (0.0) | 14/761 (2.9) | 33/767 (4.3) | 45/777 (5.8) | 21/440 (4.8) | 38/379 (10.0) |
| 45–54 | 1/118 (0.8) | 19/426 (4.5) | 32/463 (6.9) | 70/548 (12.8) | 48/348 (13.8) | 76/456 (16.7) |
| 55–64 | 3/89 (3.4) | 22/332 (6.6) | 54/323 (16.7) | 67/327 (20.5) | 57/220 (25.9) | 129/334 (38.6) |
| 65–74 | 1/35 (2.9) | 7/148 (4.7) | 40/170 (23.5) | 64/218 (29.4) | 41/106 (38.7) | 90/158 (57.0) |
Number taking aspirin/total in group (% taking aspirin).
Table 2.
Aspirin Use for Primary CVD Prevention in Women
| Survey Year | ||||||
|---|---|---|---|---|---|---|
| 1980–1982 | 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | |
| Age, y | ||||||
| 25–34 | 0/329 (0.0) | 6/1050 (0.6) | 6/1043 (0.6) | 3/915 (0.3) | 3/376 (0.8) | 3/318 (0.9) |
| 35–44 | 0/241 (0.0) | 8/784 (1.0) | 13/902 (1.4) | 14/914 (1.5) | 12/509 (2.4) | 10/470 (2.1) |
| 45–54 | 2/144 (1.4) | 14/503 (2.8) | 24/554 (4.3) | 41/650 (6.3) | 30/455 (6.6) | 51/729 (7.0) |
| 55–64 | 2/138 (1.4) | 12/373 (3.2) | 30/371 (8.1) | 46/364 (12.6) | 39/214 (18.2) | 106/372 (28.5) |
| 65–74 | 0/84 (0.0) | 21/247 (8.5) | 32/306 (10.5) | 54/251 (21.5) | 39/138 (28.3) | 92/197 (46.7) |
Number taking aspirin/total in group (% taking aspirin). CVD indicates cardiovascular disease.
Table 3.
Aspirin Use for Secondary CVD Prevention in Men
| Survey Year | ||||||
|---|---|---|---|---|---|---|
| 1980–1982 | 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | |
| Age, y | ||||||
| 25–34 | 0/2 (0.0) | 1/2 (50.00 | 1/6 (16.7) | 0/0 (0.0) | 0/3 (0.0) | 0/1 (0.0) |
| 35–44 | 0/4 (0.0) | 0/7 (0.0) | 6/13 (46.2) | 5/15 (33.3) | 1/7 (14.3) | 1/3 (33.3) |
| 45–54 | 1/4 (25.0) | 5/17 (29.4) | 12/21 (57.1) | 11/26 (42.3) | 10/19 (52.6) | 8/11 (72.7) |
| 55–64 | 4/16 (25.0) | 11/39 (28.2) | 24/39 (61.5) | 20/38 (52.6) | 13/20 (65.0) | 31/36 (86.1) |
| 65–74 | 1/10 (10.0) | 12/32 (37.5) | 36/57 (63.2) | 22/44 (50.0) | 12/24 (50.0) | 23/31 (74.2) |
Number taking aspirin/total in group (% taking aspirin). CVD indicates cardiovascular disease.
Table 4.
Aspirin Use for Secondary CVD Prevention in Women
| Survey Year | ||||||
|---|---|---|---|---|---|---|
| 1980–1982 | 1985–1987 | 1990–1992 | 1995–1997 | 2000–2002 | 2007–2009 | |
| Age, y | ||||||
| 25–34 | 0/2 (0.0) | 0/4 (0.0) | 0/2 (0.0) | 0/4 (0.0) | 1/2 (50.0) | 0/1 (0.0) |
| 35–44 | 0/5 (0.0) | 0/2 (0.0) | 2/7 (28.6) | 0/0 (0.0) | 1/3 (33.3) | 3/5 (60.0) |
| 45–54 | 1/4 (25.0) | 3/13 (23.1) | 2/7 (28.6) | 4/14 (28.6) | 3/10 (30.0) | 3/9 (33.3) |
| 55–64 | 1/9 (11.1) | 6/25 (25.0) | 10/15 (66.7) | 9/18 (50.0) | 7/11 (63.6) | 10/14 (71.4) |
| 65–74 | 0/12 (0.0) | 9/20 (45.0) | 12/34 (35.3) | 13/27 (48.1) | 11/19 (57.9) | 13/19 (68.4) |
Number taking aspirin/total in group (% taking aspirin). CVD indicates cardiovascular disease.
In Figure 2, temporal trends are depicted in aspirin use for primary and secondary prevention by sex. For primary prevention, rates steadily rose over time. For secondary prevention among women who reported a history of myocardial infarction or stroke, a steadily increasing trend was also observed from 11% in 1980–1982 to 64% in 2007–2009. Among men, aspirin use for secondary prevention rose from 19% in 1980–1982 to 74% in 2007–2009. Each of the trends shown in Figure 2 was statistically significant (P<0.0001).
Discussion
The concept that aspirin could prevent heart attacks dates at least back to the 1940s, when a California practitioner, Dr Lawrence Craven, noted the relationship between nose bleeds and aspirin use in children.24, 25 He described these observations in 1950, suggesting that aspirin might prevent AMI.25 The first formal clinical trial to test the benefit of aspirin for secondary prevention was published in 1974, and many other trials followed, establishing the efficacy of aspirin during and after an AMI.3 For primary prevention, large randomized clinical trials were first published in 1989, with the Physician's Health Study showing benefit of low‐dose aspirin in preventing AMI among healthy middle‐aged men.4 A comparable benefit of aspirin to prevent first ischemic stroke was demonstrated in the Women's Health Study.5 In a meta‐analysis, investigators observed a significant 12% relative risk reduction in nonfatal cardiovascular events achieved with aspirin use among previously healthy adults.3 These and other studies led the USPSTF in 2009 to recommend low‐dose aspirin for primary prevention in men aged 45 to 79 years and women aged 55 to 79 years7 with similar recommendations from other authoritative bodies.12, 13 Since then, additional analyses also suggest that aspirin use might be associated with a reduction in CVD mortality26 and that this benefit is likely cost‐effective.27
This study demonstrates a steady increase in aspirin use for the prevention of CVD in the adult population. Use rates for primary CVD prevention in the population increased steadily in both men and women from 1980 to 2009, now reaching 21% of men and 12% of women aged 25 to 74 years. As might be expected, there was little change in aspirin use in the youngest age group (25–34 years) over time. However, there were temporal increases among men aged 35 to 44 years and women aged 45 to 54 years, for whom aspirin is not recommended for primary prevention. The reasons that primary prevention aspirin use might rise within these young age groups could include poor public knowledge regarding the absence of benefit data from this age range, use of self‐prescribed aspirin by young individuals anxious about coronary heart disease, or prescription of aspirin to this young cohort by poorly informed health professionals. The use of aspirin as a secondary prevention tool is widespread but not universal, reaching 74% of men and 64% of women.
These data can be interpreted in the context of other studies describing aspirin use in different population samples. The Atherosclerosis Risk in Communities (ARIC) study in 1995 reported 23% of adults aged 45 to 64 regularly using aspirin, representing a 4% increase from the 1987–1989 survey of this cohort.28 The National Ambulatory Medical Care Survey of adult clinic patients with a coronary artery disease diagnosis found 20% aspirin use in 1990 with this rate rising to 30% in 2000.16 The Behavioral Risk Factor Surveillance System telephone survey in 14 states in 2003 found a self‐reported aspirin use rate of 36% among those aged 40 years or greater, with a rate of 76% among those describing a history of CVD.17 A Harris Internet Poll in 2004 found 45% of men and 37% of women using aspirin regularly with a higher 67% rate among those reporting a CVD history.15 However, in a recent study of individuals presenting with ST‐segment elevation myocardial infarction at a Minneapolis hospital, only 24% were found to be taking aspirin before the event among those with no CVD history.29 Although these data were derived from other studies that used widely different methods and are selected populations, all have aspirin use rates of similar magnitude as MHS. They all suggest a gap between national CVD prevention recommendations and contemporary use of aspirin for this purpose.
It must be noted that the MHS data are available only through 2009 and there has been increasing controversy about aspirin use for primary prevention since that time.30 The controversy focuses on recent trials of at‐risk subgroups and the balance between benefit and risk. One clinical trial, which was conducted in Japan and focused on diabetes, failed to find significant differences, although the study was underpowered.31 The American Heart Association, in recent scientific statements, emphasized stricter criteria for aspirin use in high‐risk individuals balancing benefits and harm.8, 9, 10, 11 These reports could have changed aspirin use patterns since 2009. However, a national survey in 2012 found higher levels of aspirin use for primary prevention than those reported here.32 Similarly, rising rates for secondary prevention were observed in the National Health Interview Survey in 2012.33
Lack of adherence to medications, despite positive self‐report, is a common problem when surveys are used to assess any drug treatment recommendation.34 This is particularly true when adherence is associated with a socially desirable answer. Although aspirin use, in contrast to other pharmacologic interventions, has few social connotations, we wondered if aspirin use is overreported. With a sensitive biochemical marker, aspirin use was tested in a randomly selected adult population after self‐report of aspirin use.23 While it is possible that the testing encouraged compliance, the biochemical measure closely tracked the self‐report data, lending support to the validity of survey results.
The major adverse effects of aspirin use are upper GI bleeding and hemorrhagic stroke, as documented in the large clinical trials.4, 5 These bleeding risks are emphasized in the USPSTF report recommending aspirin use for primary prevention. The USPSTF report recommends aspirin use for those with increased Framingham risk scores for CVD.7 Others have recently emphasized these risks.35 However, in the context of large increases in aspirin use observed here, there was no increase in area hospitalizations for upper GI bleeding. GI bleeding actually decreased in the same period (Figure 3). National data for upper GI bleed hospitalizations also observed a 14% decline in rates from 1998 to 2006.36 Similarly, rates of hemorrhagic stroke are decreasing in this population37 (Figure 3). Of course, these ecologic data cannot provide causal inferences as many other factors affect hospitalized bleeding. However, there is no indication of increased prevalence of hemorrhagic stroke or upper GI bleeding in a large metropolitan area associated with substantial increases in daily aspirin use.
Figure 3.
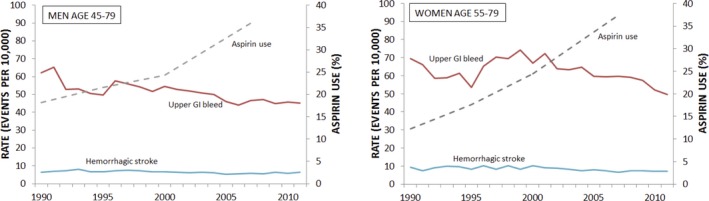
Aspirin use and hospitalization for gastrointestinal bleeding and hemorrhagic stroke.
There are limitations to this study. This study provides no data on the role of the individual's physician in recommending aspirin and cannot confirm the appropriateness of aspirin use. While MHS has some risk factor data on these participants, they are not adequate to enter into the USPSTF algorithm to determine if aspirin use is appropriate. Similarly, self‐report of a CVD event is subject to misclassification. The widespread mass‐media advertising of aspirin for the secondary prevention of heart disease may result in many adults self‐medicating. And while we completed a substudy confirming exposure to aspirin in the previous 2 days, overreporting and underreporting are still possible. Finally, participation rates in the MHS have gradually fallen during the past 30 years, as for most survey‐based research. It is possible that selection bias has occurred. However, analysis of the MHS data suggests participants differ little over time and there is no evidence that aspirin use or nonuse is a factor in participation.
In summary, aspirin use for the prevention of CVD increased significantly for both men and women from 1980 to 2009. Rates of aspirin use increased for both primary and secondary prevention of CVD. Particularly in older age groups, aspirin use for primary CVD prevention is approaching 50% of the population. The impact on CVD ischemic event rates, which were falling during the same time period, is unknown.
Sources of Funding
This work was supported by National Institutes of Health grant 5R01HL023727‐28. This agency played no role in the design, conduct, or writing of this report.
Disclosures
Nicole Zantek has a financial interest in Endo International PLC. This interest has been reviewed and managed by the University of Minnesota in accordance with its conflict of interest policies. Nicole Zantek has also received research funding from AstraZeneca and Bayer HealthCare. The other authors have no conflicts of interest to disclose. Dr Hirsch earns income from serving on a steering committee for an unrelated clinical trial sponsored by Bayer that has no relationship to this research project. This relationship has been reviewed and managed by the University of Minnesota in accordance with its conflict of interest policies.
(J Am Heart Assoc. 2015;4:e002320 doi: 10.1161/JAHA.115.002320)
References
- 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2013 Update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the U.S. by improvements in use of clinical preventive services. Am J Prev Med. 2010;38:600–609. [DOI] [PubMed] [Google Scholar]
- 3. Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta‐analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Steering Committee of the Physicians’ Health Study Research Group . Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321:129–135. [DOI] [PubMed] [Google Scholar]
- 5. Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE. A randomized trial of low‐dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med. 2005;352:1293–1304. [DOI] [PubMed] [Google Scholar]
- 6. Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL. Aspirin for the primary prevention of cardiovascular events in women and men: a sex‐specific meta‐analysis of randomized controlled trials. JAMA. 2006;295:306–313. [DOI] [PubMed] [Google Scholar]
- 7. U.S. Preventive Services Task Force . Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;150:396–404. [DOI] [PubMed] [Google Scholar]
- 8. Fox CS, Golden SH, Anderson C, Bray GA, Burke LE, de Boer IH, Deedwania P, Eckel RH, Ershow AG, Fradkin J, Inzucchi SE, Kosiborod M, Nelson RG, Patel MJ, Pignone M, Quinn L, Schauer PR, Selvin E, Vafiadis DK; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health, Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, Council on Quality of Care and Outcomes Research, and the American Diabetes Association . Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2015;132:691–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Washam JB, Herzog CA, Beitelshees AL, Cohen MG, Henry TD, Kapur NK, Mega JL, Menon V, Page RL II, Newby LK; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, Council on Functional Genomics and Translational Biology, Council on the Kidney in Cardiovascular Disease, and Council on Quality of Care and Outcomes Research . Pharmacotherapy in chronic kidney disease patients presenting with acute coronary syndrome: a scientific statement from the American Heart Association. Circulation. 2015;131:1123–1149. [DOI] [PubMed] [Google Scholar]
- 10. Kulik A, Ruel M, Jneid H, Ferguson TB, Hiratzka LF, Ikonomidis JS, Lopez‐Jimenez F, McNallan SM, Patel M, Roger VL, Sellke FW, Sica DA, Zimmerman L; American Heart Association Council on Cardiovascular Surgery and Anesthesia . Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation. 2015;131:927–964. [DOI] [PubMed] [Google Scholar]
- 11. Meschia JF, Bushnell C, Boden‐Albala B, Braun LT, Bravata DM, Chaturvedi S, Creager MA, Eckel RH, Elkind MS, Fornage M, Goldstein LB, Greenberg SM, Horvath SE, Iadecola C, Jauch EC, Moore WS, Wilson JA; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; Council on Hypertension . Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3754–3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Healthy People 2020 objectives. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default. Accessed November 7, 2013.
- 13. Frieden TR, Berwick DM. The “Million Hearts” initiative—preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. [DOI] [PubMed] [Google Scholar]
- 14. Kim C, Beckles GL. Cardiovascular disease risk reduction in the Behavioral Risk Factor Surveillance System. Am J Prev Med. 2004;27:1–7. [DOI] [PubMed] [Google Scholar]
- 15. Pignone M, Anderson GK, Binns K, Tilson HH, Weisman SM. Aspirin use among adults aged 40 and older in the United States: results of a national survey. Am J Prev Med. 2007;32:403–407. [DOI] [PubMed] [Google Scholar]
- 16. Stafford RS, Radley DC. The underutilization of cardiac medications of proven benefit, 1990 to 2002. J Am Coll Cardiol. 2003;41:56–61. [DOI] [PubMed] [Google Scholar]
- 17. Ajani UA, Ford ES, Greenland KJ, Giles WH, Mokdad AH. Aspirin use among U.S. adults: Behavioral Risk Factor Surveillance System. Am J Prev Med. 2006;30:74–77. [DOI] [PubMed] [Google Scholar]
- 18. Maddox TM, Ho PM, Roe M, Dai D, Tsai TT, Rumsfeld JS. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catherization: insights from the National Cardiovascular Data Registry Cath‐PCI Registry. Circ Cardiovasc Qual Outcomes. 2010;3:632–641. [DOI] [PubMed] [Google Scholar]
- 19. Luepker RV, Jacobs DR Jr, Gillum RF, Folsom AR, Prineas RJ, Blackburn H. Population risk of cardiovascular disease: the Minnesota Heart Survey. J Chronic Dis. 1985;38:671–682. [DOI] [PubMed] [Google Scholar]
- 20. Luepker RV, Jacobs DR Jr, Folsom AR, Gillum RF, Frantz ID Jr, Gomez O, Blackburn H. Cardiovascular risk factor change—1973‐74 to 1980‐82: the Minnesota Heart Survey. J Clin Epidemiol. 1988;41:825–833. [DOI] [PubMed] [Google Scholar]
- 21. Luepker RV, Arnett DK, Jacobs DR Jr, Duval SJ, Folsom AR, Armstrong C, Blackburn H. Trends in blood pressure, hypertension control, and stroke mortality: the Minnesota Heart Survey. Am J Med. 2006;119:42–49. [DOI] [PubMed] [Google Scholar]
- 22. Feldman M, Cryer B, Rushin K, Betancourt J. A comparison of every‐third‐day versus daily low‐dose aspirin therapy on serum thromboxane concentrations in healthy men and women. Clin Appl Thromb Hemost. 2001;7:53–57. [DOI] [PubMed] [Google Scholar]
- 23. Zantek ND, Luepker RV, Duval S, Miller K, Oldenburg N, Hirsch AT. Confirmation of reported aspirin use in community studies: utility of serum thromboxane B2 measurement. Clin Appl Thromb Hemost. 2014;20:385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miner J, Hoffhines A. The discovery of aspirin's antithrombotic effects. Tex Heart Inst J. 2007;34:179–186. [PMC free article] [PubMed] [Google Scholar]
- 25. Craven LL. Acetylsalicylic acid, possible preventive or coronary thrombosis. Ann West Med Surg. 1950;4:95–99. [PubMed] [Google Scholar]
- 26. Raju N, Sobieraj‐Teague M, Hirsh J, O'Donnell M, Eikelboom J. Effect of aspirin on mortality in the primary prevention of cardiovascular disease. Am J Med. 2011;124:621–629. [DOI] [PubMed] [Google Scholar]
- 27. Jacoba P, Greving JP, Buskens E, Koffijberg H, Algra A. Cost‐effectiveness of aspirin treatment in the primary prevention of cardiovascular disease events in subgroups based on age, gender, and varying cardiovascular risk. Circulation. 2008;117:2875–2883. [DOI] [PubMed] [Google Scholar]
- 28. Shahar E, Folsom AR, Romm FJ, Bisgard KM, Metcalf PA, Crum L, McGovern PG, Hutchinson RG, Heiss G; for the ARIC Study Investigators . Patterns of aspirin use in middle‐aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 1996;131:915–922. [DOI] [PubMed] [Google Scholar]
- 29. Miedema MD, Cohn JN, Garberich RF, Knickelbine T, Graham KJ, Henry TD. Underuse of cardiovascular preventive pharmacotherapy in patients presenting with ST‐elevation myocardial infarction. Am Heart J. 2012;164:259–267. [DOI] [PubMed] [Google Scholar]
- 30. Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Ngianga‐Bakwin K, Grove A, Gurung B, Morrow S, Stranges S, Clarke A. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970. doi: 10.1371/journal.pone.0081970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ogawa H, Nakayama M, Morimoto T, Uemura S, Kanauchi M, Doi N, Jinnouchi H, Sugiyama S, Saito Y; Japanese Primary Prevention of Atherosclerosis with Aspirin for Diabetes (JPAD) Trial Investigators . Low‐dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300:2134–2141. [DOI] [PubMed] [Google Scholar]
- 32. Williams CD, Chan AT, Elman MR, Kristensen AH, Miser F, Pignone MP, Stafford RS, McGregor JC. Aspirin use among adults in the U.S.: results of a national survey. Am J Prev Med. 2015;48:501–508. [DOI] [PubMed] [Google Scholar]
- 33. Fang J, George MG, Gindi RM, Hong Y, Yang Q, Ayala C, Ward BW, Loustalot F. Use of low‐dose aspirin as secondary prevention of atherosclerotic cardiovascular disease in US adults (from the National Health Interview Survey, 2012). Am J Cardiol. 2015;115:895–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. [DOI] [PubMed] [Google Scholar]
- 35. Raju NC, Eikelboom JW. The aspirin controversy in primary prevention. Curr Opin Cardiol. 2012;27:499–507. [DOI] [PubMed] [Google Scholar]
- 36. Zhao Y, Encinosa W. Hospitalizations for gastrointestinal bleeding in 1998 and 2006. HCUP Statistical Brief #65. Rockville, MD: Agency for Healthcare Research and Quality; December 2008. [PubMed] [Google Scholar]
- 37. Lakshminarayan K, Anderson DC, Zhou X, Barber CA, Steffen LM, Luepker RV. Trends in stroke subtypes: the Minnesota stroke survey. Stroke. 2005;36:505. [Google Scholar]


