Abstract
Background
In spite of the increasing incidence of total knee arthroplasties (TKA), evidence is limited regarding risk factors for revision. The objective of this scoping review was to identify and assess demographic, surgical and health services factors that may increase the risk for revision surgery following TKA.
Methods
A scoping review was undertaken following an electronic search in MEDLINE (1990 to December 2013), CINAHL (to December 2013), EMBASE (1990 to December 2013) and Web of Science (1990 to December 2013).
Results
Of the 4460 articles screened, 42 were included of which 26 articles were based on registry data. Increased risk of revision was associated with demographic factors (younger age, African American), surgical factors related to the primary TKA (uncemented components, implant malalignment, increased surgery duration), and health services (low volume hospitals).
Conclusions
Identifying emerging trends in characteristics of those requiring revision following TKA can help identify those at risk and allocate appropriate resources. Further primary clinical articles on risk factors for revision of TKA are necessary to ensure maximal function and lifespan following TKAs.
Electronic supplementary material
The online version of this article (doi:10.1186/s12891-016-1025-8) contains supplementary material, which is available to authorized users.
Keywords: Total knee arthroplasty, Revision, Failure, Risk factor, Scoping review
Background
The effectiveness of total knee arthroplasty (TKA) in relieving pain and improving function has been well documented [1, 2]. TKA is considered a cost effective and efficacious treatment for patients with end stage knee osteoarthritis who experience severe pain, activity limitations and for whom conservative treatment is unsuccessful [3–5]. With more than 700 000 primary TKAs performed annually in the USA, estimates of TKA are projected to increase to 673 % by 2030 in the USA. The large demand for TKA is primarily related to the aging population, the obesity epidemic and technical advancement of the surgical procedure [6–8]. The longevity of implants is typically greater than 10 years with 32,700 revisions performed annually in the USA. Significant demand for primary TKA will correspond to a growing demand for revisions of TKA which are projected to increase by 601 % from 2005 to 2030 [6].
Revisions for TKA pose unique challenges as revision surgery is a more complex surgery than a primary TKA with increased complication and mortality rates [9–11]. Identifying emerging trends in characteristics of those requiring revision following TKA can help identify those at risk and allocate appropriate resources. Several articles have identified risk factors for revision surgery of TKA yet, to our knowledge, the synthesis of these findings have not been documented. A more comprehensive understanding of the potential risk factors for revision of TKA will provide important knowledge for surgeons and patients. The objective of this scoping review was to identify and assess demographic, surgical and health services factors that lead to increased risk of revision surgery following TKA.
Methods
A scoping review of the literature was undertaken to identify and assess relevant evidence given the limited existing evidence on revisions of TKA. Inclusion criteria consisted of studies that comprised a) adult patients who received primary TKA and received a subsequent revision, b) comparative groups or risk-adjusted analyses, and c) at least 20 or more revision cases. Cohort and case control articles were included while descriptive studies and randomized controlled trials comparing specific interventions were excluded. Articles which included hemiarthroplasty, primary TKA used to stabilize a fracture or management of bone pathology or malignancy, simultaneous bilateral TKAs, and patellofemoral arthroplasty were excluded. Revisions for all reasons were included except revisions occurring in the first three months due to sepsis. Ethics was not obtained for this study as the study was a retrospective scoping review that did not involve any individual data or identifying information. In discussion with our Health Research Ethics Board at the University of Alberta, we do not require ethics for review.
Data sources and search strategies
A search strategy was developed and implemented by a health sciences librarian for 4 databases: Medline (1990-Dec 2013; includes in-process & other non-indexed citations), EMBASE (1990-Dec 2013), CINAHL (1990-Dec 2013), and Web of Science (1990-Nov 2012) (Additional file 1). Date (1990–2013) and language (English) restrictions were applied to the searches. The decision to restrict the search to English articles was based on findings from systematic research evidence that reported no empirical evidence of bias was seen if papers written in languages other than English (LOE) were excluded [12]. The search included an extensive list of subject headings and keyword terms for 3 concepts: 1) hip or knee arthroplasty, 2) revision surgery, and 3) prognosis (see Additional file 1). Total hip arthroplasty articles were included in the search because we did not want to inadvertently exclude articles that reported both total hip and total knee arthroplasties. Case articles or case reports were removed along with conference abstracts. This initial search yielded many non-relevant papers so an additional search string was added to increase the relevancy of the results (by including certain terms in either the title or marked as the most important subject headings). A “relevancy forcing search set” was performed to ensure that all relevant papers were captured. All duplicate citations were removed.
Study selection
To ensure consistency with screening of title and abstract, 20 citations were independently reviewed by both reviewers (LJ & SP) using a standardized form based on broad criteria including population intervention, comparison, outcome and study design. The remaining citations were then independently screened for relevance.
If a citation was selected by either reviewer, the full-text article was obtained for further review. Full-text articles were further screened for selection using a standard study selection form, based upon the predetermined inclusion criteria. The study selection form was initially piloted on a sample of 20 articles to ensure that the selection criteria were applied consistently across reviewers. Relevant full-text articles were then reviewed by one of the two reviewers using standardized inclusion and exclusion criteria. Disagreement of article inclusion was resolved through consensus between reviewers or through third party adjudication if the reviewers did not arrive at consensus. Full-text papers were included only if consensus was achieved by reviewers. For those articles selected for full review, data were extracted by one reviewer (LJ) and verified by a second reviewer (LB or AJ). The first 20 full text articles reviewed by both reviewers had excellent agreement (Kappa value 0.96, p < 0.0001). All selected articles were included in data synthesis regardless of methodological quality. Inconclusive findings and gaps in the literature were identified. A narrative description of the included articles was completed and potential patterns identified in terms of targeted behaviors, study outcomes, and intervention effectiveness.
Quality assessment
The Oxford Level of Evidence was used to evaluate the quality of selected full-text articles [13], and has been recommended to determine a hierarchy of the best evidence [14]. SIGN guidelines were also used to assess study quality through completion of their cohort checklist including items such as subject selection, assessment, confounding and statistical analysis [15].
Results
Of the 4460 articles identified through the search strategies, 266 articles remained after the abstracts were screened for eligibility. After full text review, 42 articles met the inclusion criteria for the review (see Fig. 1). Twenty-six (62 %) articles were based on registry or insurance databases of which 12 were based on Nordic registries and 11 from American databases (see Additional file 2).
Fig. 1.
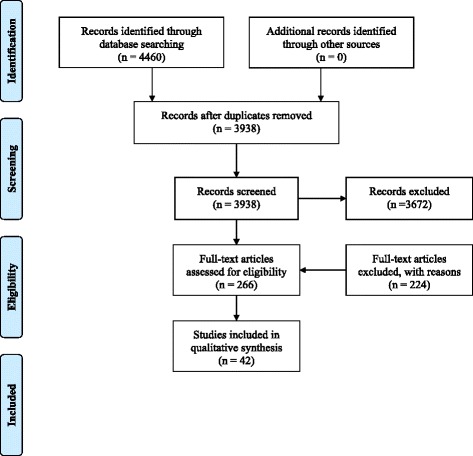
PRISMA flow diagram
All articles were prognostic retrospective articles with level III quality except for one which was a level II prognostic prospective study [13, 16]. Using the SIGN guidelines, 31 articles were regarded of acceptable quality and 11 articles were deemed poor quality often due to incomplete reporting of multivariate analyses (see Additional file 2) [15].
Of the 34 (81 %) articles that reported mean follow-up from the primary TKA, six articles reported 10 year survival rates and two articles reported 20 year survival rates (see Table 1). While survival rates of the primary TKA were consistently high at 10 years ranging from 89.5 to 98.6 % [17–19, 20, 21, 42], 20 year survival rates were expectedly lower at 78–99 % [19, 23].
Table 1.
Survival rates at 10 and 20 Yearsa
| Author(s), year | Duration of follow-up (yrs) | Index procedure (n) | Revision (n) | Survival rate (%, CI) |
|---|---|---|---|---|
| Badawy M. et al., 2013 [42] | 10 | 26,698 | 1169 | Low hospital volumeb: 92.5 %, 95 % CI 91.5 to 93.4 High hospital volume: 95.5 %, 95 % CI 94.1 to 97.0 |
| Gothesen, Ø. et al., 2013 [17] | 10 | 17,782 | NR | 89.5 to 95.3 %, CI- NR |
| Himanen, A. et al., 2007 [20] | 10 | 751 | 37 | Prosthetic moulded component: 94.4 %, 95 % CI 90.4 to 96.7 Prosthetic modular component: 93.6 %, 95 % CI 89.7 to 96.0 |
| Jämsen, E. et al., 2013 [21] | 10 | 53,007 | 1919 | 94.5 %, 95 % CI 94.1 to 94.8 |
| Rand, J. et al., 2003 [19] | 10 | 11,606 | NR | 91 %, 95 % CI 90 to 91 % |
| Vessely, M. et al., 2006 [18] | 10 | 1000 | 45 | 98.6 %, 95 % CI 97.8 to 99.4 |
| Fang, D. et al., 2009 [23] | 20 | 6070 | 51 | 99 %, CI - NR |
| Rand, J. et al., 2003 [19] | 20 | 11,606 | NR | 78 %, 95 % CI 74 to 81 % |
aSee Additional file 2 for further detail. Not reported in publication, NR
bLow hospital volume is 1–24 TKA performed per year; High hospital volume is ≥150 TKA performed per year
Demographic risk factors
Sex
While all articles reported sex, the association of sex and TKA revision was only examined in 10 articles (see Table 2). Inconsistent findings were reported in that males had a higher risk of revision surgery than females in 5 articles (see Table 2), females had a higher risk of revision (HR 1.513, 95 % CI 1.116 to 2.051) in one article, based on American registry data, [24] and four articles, from different countries, did not find a significant association between sex and TKA revision [16, 18, 25–26].
Table 2.
Sex and adjusted risk of revisiona
| Author(s)/year | Control | Hazard ratio (CI) |
|---|---|---|
| Blum, M. et al., 2013 [29] | Female | 0.81, 95 % CI 0.71 - 0.92, p < 0.01 |
| Fehring, T. et al., 2004 [52] | Male | 2.771, 99 % CI 1.662 - 4.620, p < 0.0001 |
| Harrysson, O. et al., 2004 [43] | Male | 1.64, 95 % CI 1.23 - 2.18, p = 0.0007 |
| Rand, J. et al., 2003 [19] | Male | 1.6, 95 % CI 1.4 - 2.0, p < 0.0001 |
| Schrama, J. et al., 2010 [30] | Female | 0.67, 95 % C I 0.47 - 0.88 |
| Stiehl, J. et al., 2006 [24] | Female | 1.513, 95 % CI 1.116 - 2.051 |
aSee Additional file 2 for further detail
Age
Among the 15 articles that examined age as a risk factor, 13 articles reported that revision rates decreased with older age (see Table 3).
Table 3.
Age and adjusted risk of revisiona
| Author(s)/Year | Age | Hazard ratio (95 % CI) unless otherwise stated |
|---|---|---|
| Bini, S. et al., 2013 [31] | >55 years | 0.43, 95 % CI 0.27 to 0.67, p < 0.001 |
| Blum, M. et al., 2013 [29] | 18–64 years vs. 65+ yrs | 2.30, 95 % CI 1.96 to 2.69, p < 0.0001 |
| Bordini, B. et al., 2009 [32] | Age at surgery (per year) | 1.05, 95 % CI 1.03 to 1.06, p = 0.0001 |
| Fehring, T. et al., 2004 [52] | Age at surgery (per year) | 0.953, 99 % CI 0.932 to 0.975, p < 0.0001 |
| Gioe, T. et al., 2004 [53] | Age <70 year | 0.46, 95 % CI.0.33 to 0.64, p < 0.001 |
| Harrysson, O. et al., 2004 [43] | Older patients (≥60 year) Revision Attributable to Any Reason Revision Attributable to Loosening of Components |
0.49, 95 % CI 0.38 to 0.62, p < 0.0001 0.41, 95 % CI 0.27 to 0.62, p < 0.0001 |
| Julin, J. et al., 2010 [35] | Age ≤ 55 years: Revision for reasons other than infection Revision for any reason |
2.9, 95 % CI 2.3 to 3.6 2.4, 95 % CI 2.0 to 3.0 Age 56–65 years |
| Age 56–65 years: Revision for reasons other than infection Revision for any reason : |
1.7 95 % CI 1.4 to 2.0 1.5, 95 % CI 1.3 to 1.7 |
|
| Kreder, H. et al., 2003 [25] | Younger age per 10 year: At 1 year after revision At 3 years after revision |
OR 0.77, 95 % CI 0.67 to 0.89 OR 0.70, 95 % CI 0.66 to 0.81 |
| Lygre, S. et al., 2011 [37] | Age >70 year vs. <60 year | 0.4, 95 % CI 0.3–0.4, 0 < 0.001 |
| Namba, R. et al., 2013 [28] | Age (increasing 10 year increments) | 0.62, 95 % CI 0.57 to 0.67, p < 0.001 |
| Namba, R. et al., 2012 [27] | Age (increasing 10 year increments) | 0.64, 95 % CI 0.58 to 0.70, p < 0.001 |
| Rand, J. et al., 2003 [19] | Age 56–70 year vs. ≤55 years Age >70 year vs. ≤55 years |
0.7, 95 % CI 0.5 to 0.9, p < 0.01 0.5, 95 % CI 0.3 to 0.6, p < 0.0001 |
| Stiehl, J. et al., 2006 [24] | Younger patients (for every yr increase) | 0.979, 95 % CI 0.968 to 0.989 |
aSee Additional file 2 for further detail
Race
Race was examined in 3 American articles, of which 2 were based on the same registry [27, 28]. African American patients had a higher risk for revision than Caucasian patients (HR 1.73, 95 % CI 1.33 to 2.25, p < 0.001; HR 1.82, 95 % CI 1.33 to 2.48, p < 0.001; HR 1.39, 95 % CI 1.08 to 1.80, p = 0.01) and represented 5.5 and 8.4 % of the patient population reported in these registries. [27–29].
Medical risk factors
Primary diagnosis
Although the majority of patients undergoing TKA were diagnosed with osteoarthritis, 4 articles specifically examined diagnosis and its potential association with TKA revision with mixed results [19, 24, 25, 30]. Two large registry articles reported differing results with inflammatory arthritis having a greater and lesser risk for revisions than patients with osteoarthritis (HR 1.6, 95 % CI 1.06 to 2.38 and HR 0.5, 95 % CI 0.3 to 0.7, p < 0.001) [19, 30]. A clinical study of 4743 patients found that OA or post-traumatic arthritis had a greater risk of revision than RA (HR 1.51, 95 % CI 1.116 to 2.051) [24]. Further, in a clinical sample of 14352 patients, Kreder et al. reported no significant association between the diagnosis of OA and risk for revision [25].
Comorbidities
Eleven articles specifically looked at the effect of comorbidities examining both total number of conditions and specific conditions (see Additional file 2). Jamsen et al. found that risks increased if there were one or more of the comorbidities identified (HR 1.23, 95 % CI 1.16 to 1.30) [21]. Alternately, Kreder et al. did not find a significant association between the presence of comorbidities and revision following TKA [25].
When looking at comorbidities associated with OA, obesity, cardiac disease and diabetes were at high risk of revision. Two American TKA registries reported increased risk of revision for patients with a higher BMI (BMI 30–35 kg vs <30 kg HR 1.48, 95 % CI 1.00 to 2.19 and BMI ≥35 kg/m2 vs. <30 kg/m2 h 0.78, 95 % CI 0.63 to 0.96, p = 0.020) [28, 31]. However, 3 other articles did not find a significant relationship between BMI and risk for TKA revision [18, 20, 32].
The presence of cardiac conditions at time of the primary TKA increased the risk of revision including hypertension with early revision (0 – 5 years) (HR 1.14, 95 % CI 1.01 to 1.29), coronary disease (HR 1.27 95 % CI 1.07 to 1.50) and cardiovascular disease (HR 1.29, 95 % CI 1.14 to 1.45) [21, 33].
Three articles reported an increased risk of revision for the patients with diabetes. Jamsen et al. and Namba both found an association with diabetes and revision (HR 1.27, 95 % CI 1.08 to 1.50 and HR 1.21, 95 % CI 1.04 to 1.41, p = 0.014) although Jamsen et al. was examining early revisions [28, 21]. Similarly, King et al. also found the 46 to 55 years and 66 years + diabetic cohorts had increased risk of revision as compared to the non-diabetic cohort (HR 2.9 95 % CI 1.5 to 5.8, p = 0.004 and HR 1.5, p = 0.0037 respectively) although there was not a significant difference in the 56 to 65 years cohort [34].
Joint implant factors
Fixation
Two articles consisting of 9337 patients from the US found cemented primary TKAs had a protective effect on receiving revision as compared to cementless/hybrid TKAs [16, 19]. Hybrid fixation, in which the proximal component was cementless and the distal component was cemented, also demonstrated a higher risk for revision than cemented TKAs in both US and Norwegian studies [16, 35].
Cruciate retaining implants
Cruciate ligament status was reported in several articles with inconsistent findings (see Table 4) [16]. Two large American registry studies reported that posterior stabilized implants had increased risk of revision when compared to posterior cruciate-retaining implants (HR 2.6, 95 % CI 2.1 to 3.5, p < 0.0001 and HR = 2.0, 95 % CI 1.67 to 2.5, p < 0.001) [19, 36]. Conversely, an American registry study of 1047 patients found ligament status was not significant [16]. Further, Stiehl et al. found both posterior cruciate retaining arthroplasties and bicruciate retaining arthroplasties had increased risk of revision compared to rotating platform (HR 1.552, 95 % CI 1.157 to 2.081 and HR 2.188, 95 % CI 1.454 to 3.294) [24].
Table 4.
Implant type/technique and adjusted risk of revisiona
| Author(s)/year | Implant type/technique | Reference | Hazard ratio (95 % CI) unless otherwise stated |
|---|---|---|---|
| Abdel, M. et al., 2011 [36] | Cruciate Status: | ||
| Posterior cruciate-retaining | Posterior cruciate-stabilizing | 0.5, 95 % CI 0.4 - 0.6, p < 0.001 | |
| Rand, J. et al., 2003 [19] | Cruciate Status: | ||
| Posterior Stabilized | Posterior cruciate-retaining | 2.6, 95 % CI 2.1 - 3.5, p < 0.0001 | |
| Constrained condylar | Posterior cruciate-retaining | 2.1, 95 % CI 0.9 - 4.9, p = 0.08 | |
| Stiehl J. et al., 2006 [24] | Cruciate Status | ||
| PCRs | Rotating platform | 1.552, 95 % CI 1.157 - 2.081 | |
| BCRs | 2.188, 95 % CI 1.454 - 3.294 | ||
| Gøthesen, O. et al., 2013 [17] | Implant Type: | ||
| Duracon | Profix | 2.6, 95 % CI 1.9 - 3.4, p < 0.001 | |
| LCS Classic HR | 1.3, 95 % CI 1.0 - 1.6, p = 0.017 | ||
| LCS Complete | 1.5, 95 % CI 1.1 - 1.9, p = 0.002 | ||
| AGC Universal | 1.6, 95 % CI 1.3 - 2.0, p < 0.001 | ||
| Lygre, S. et al., 2010 [37] | Implant Type: | Relative Risk = | |
| NR Tricon | NR AGC Universal | 1.67, 95 % CI 1.24–2.24, p = 0.001, | |
| NR Genesis 1 | 1.43, 95 % CI 1.14–1.79, p = 0.002, | ||
| NR Duracon | 1.45, 95 % CI 1.05–1.99, p = 002. | ||
| NR Profix | 0.66, 95 % CI 0.52–0.82, p < 0.001, | ||
| NR e.motion | 0.09, 95 % CI 0.02–0.37, p = 0.001, | ||
| NR AGC anatomic | 0.66, 95 % CI 0.45–0.99, p = 0.04, | ||
| PR AGC universal | 0.48, 95 % CI 0.27–0.83, p = 0.009, | ||
| PR NexGen | 0.40, 95 % CI 0.22–0.74, p = 0.004. | ||
| Namba R. et al., 2013 [28] | Implant Type: | ||
| Rotate LCS | Fixed PS | 2.07, 95 % CI 1.53 - 2.80, p < 0.001 | |
| High flexion | Yes versus No | 1.76, 95 % CI 1.29 - 2.41, p < 0.001 | |
| Namba R. et al., 2012 [27] | Implant Type: | ||
| LCS | Fixed | 2.01, 95 % CI 1.41 - 2.86, p < 0.001 | |
| Inacio M. et al., 2013 [54] | Bearing or inserts: | ||
| CoCr-HXLPE | CoCr-CPE | NS 1.2, 95 % CI 0.9 - 1.5, p > 0.05 | |
| OZ-CPE | C0Cr-CPE | NS 1.4, 95 % CI 0.3 - 5.9, p > 0.05 |
Abbreviations: RR relative risk, NS not significant, BCR bicruciate preservation, PCR posterior cruciate retention, (PR) patella resurfaced, (NR) patella non resurfaced, LCS low contact stress, OZ oxidized zirconium, CoCR cobalt chromium, CPE conventional polyethylene, HXLPE highly crosslinked polyethylene;
aSee Additional file 2 for further detail
Patellar resurfacing
The articles that specifically examined patellar resurfacing had inconsistent findings. Three articles found that the risk of revision increased when the patella was resurfaced (patella not resurfaced HR 1.4, 95 % CI 1.2 to 1.7, patella resurfaced HR 0.84, 95 % CI: 0.071–1.0, p = 0.052, and patellar resurfaced HR 1.814, 95 % CI 1.320 to 2.558 respectively) [24, 35, 37]. Alternately, two articles found that the patellae not resurfaced patellae had higher risks of revision than resurfaced patellae (HR 2.09, 95 % CI 1.07 to 4.06, p = 0.03, HR 1.4, 95 % CI 1.2 to 1.7) [27, 35]. Two studies did not find an association between patellar resurfacing and revision significant [20, 38]. One study reported that metal-backed patella were more likely to be revised than all polyethylene patellar components (HR 2.4, 95 % CI 1.9 to 3.1, p < 0.0001) [19].
Alignment
Malalignment was reported to be a large risk factor for revisions (HR >2.7) in three studies with both varus and valgus malalignment having a greater risk of revision [23, 39, 40]. Two American studies reported an increased risk of revision with varus tibial malalignment (<90°) (HR 10.6, 95 % CI 5.4 to 20.6, p < 0.0001; OR 3.0, p = 0.04 respectively) [23, 39]. Valgus femoral malalignment also showed an increased risk with ≥8° of valgus (HR 5.1, 95 % CI 2.8 to 9.5, p < 0.0001) [40].
Bone quality
As bone stock is a key determinant of the type of implant used and possible peri-prosthetic fracture, bone quality is an important surgical consideration. Only one study examined bisphosphonate use and reported a protective effect for risk for revision (HR 0.40, 95 % CI 0.15 to 1.07, p = 0.068) [41] recommending its use for those patients with the diagnosis of osteoarthritis.
Health services
Of the 3 articles that reported hospital volume in Canada, USA and Norway, low volume hospitals had an increased risk for revision of primary TKAs [25, 42, 22]. The definition of low volume, however, varied from less than 25 to less than 50 procedures annually. Further, Harrysson et al. found that the risk of revision decreased when comparing the year of surgery to the previous year (HR 0.92, 95 % CI 0.89 to 0.96, p < 0.0001) over a 10 year time period [43].
Length of surgery for the primary TKA was also found to have a significant association with revision risk in TKA primary surgery >240 min (OR 1.34, 95 % CI 1.07 to 1.67, p = 0.012) as compared to <240 min, 150 to 180 min (OR 1.31, 95 % CI 1.09 to 1.57, p = 0.004) as compared to 120 to 150 min and <90 min (OR 1.47, 95 % CI 1.10–1.95, p = 0.008) as compared to 120 to 150 min [44].
Discussion
We identified 42 articles that reported risk factors for TKA revision using risk-adjusted analyses. Demographic, medical and implant factors were identified as risk factors for revision of TKA ranging from short-term (<5 years) to long-term follow-up (20+ years). Risk factors were derived largely from registry data, which inherently restricts the type of risk factors examined.
Primary TKA has been consistently identified as a successful surgery with high survival rates even at 10 and 20 years post-surgery. Others have reported rates of 1.26 revisions per 100 observed component years for TKA as compared to 1.29 revisions per 100 observed component years for total hip replacements and 3.29 revisions per 100 component years for total ankle replacements [45]. Given the success of the surgery, it has been suggested the focus of research should perhaps shift to patient selection for these procedures to optimize outcomes and health resources [46].
The trend of increasing revision rates will likely increase [46, 47]. This information was especially relevant given that the 45–64 year old cohort is one of the fastest growing demographics [48, 49]. Further, this age cohort demonstrated an increased use of TKA and will require a longer life expectancy for the TKA, an important consideration when planning for future allocation of resources [46, 49]. The increased risk for revision in the younger population must be further examined to determine if it is indeed age that is the risk factor or if age is a proxy for higher activity levels or increased expectations in this younger patient population.
Comorbidities such as diabetes, cardiovascular disease, hypertension, obesity, cancer and lung disease were found to increase the risk for revision. These findings are particularly meaningful given the increasing prevalence of multi-morbidity and the challenge of surgical management of patients with other chronic diseases [50, 51]. Further investigation of management programs of secondary chronic diseases such as hypertension, obesity and diabetes in patients with primary TKA is warranted.
Often heterogeneity was found among the reported results for other risk factors for TKA revision. For example, mixed results were reported regarding sex, primary diagnosis, BMI, patellar resurfacing and implant components suggesting a need for further investigation. Some consensus existed, however, regarding cemented prostheses which had a lower risk of revision than uncemented or hybrid in spite of an initial goal of uncemented fixation to decrease complications associated with aseptic loosening [16, 19, 35]. Increased surgery length and low hospital volumes were also found to negatively affect revision rates which is important information to consider in health resource allocation and planning.
In spite of a wide body of literature published on various surgical factors, many articles were of low quality and few included risk-adjusted analysis. The majority of included articles (41/42) were retrospective prognostic articles limiting the quality of the articles to an Oxford level III. Because the majority of data (26/42) was taken from registry data, the data were often limited to basic demographic information such as age, gender and BMI and did not evaluate pain and functional measures (see Additional file 2). An inherent limitation of these large, population-based registries is that demographic, surgical and health services data over decades have typically been evaluated and do not provide patient-reported outcomes or patient-reported experience measures which are central to clinical outcomes of TKA. Finally, findings were derived from two geographical populations, 26 in the USA and 11 in Nordic countries. External validity to other populations is uncertain because of different healthcare systems and potentially different prostheses.
In spite of an extensive search strategy and a strong systematic approach to undertaking this systematic review, identifying risk factors for revision was challenging because of low revision rates in the first 10 years following surgery. Most articles had follow-up periods of <10 years which reflected high survival rates of TKA. Due to these high survival rates, it can be a lengthy and costly process to undertake studies for the appropriate duration to acquire accurate information on revisions. Another consideration is that many early revisions occurring within 10 years are often related to surgical techniques and few articles made the distinction between early and later revisions. Finally, as TKAs are most often performed on an older population, the development of other chronic conditions and mortality poses a challenge to long-term follow-up.
Conclusions
Current literature suggests an increased risk for revision following TKA is associated with younger age, greater number of comorbidities, African American race, uncemented components, increased surgery duration, and lower volume hospitals. This scoping review allowed us to identify areas where consistent results were found but also highlight areas with heterogeneous results or insufficient data where further research is required. The findings also demonstrate the need for large scale and high quality investigations examining factors that increase the risk for revision following TKA including patient-reported outcomes and patient-reported experience measures. Given the increasing numbers of TKA procedures and revisions, information on risk factors for revisions following TKAs is necessary for appropriate interventions to be delivered in a timely manner and for the development of effective health care policy.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article and its additional files.
Acknowledgments
Special gratitude is expressed to Liz Dennett, MLIS for her assistance with the extensive search.
Role of funding source
No funding was received for this work.
Additional files
Search Strategy. (DOCX 14 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors were involved in conception and design, analysis and interpretation of the data, drafting and revisions of the article and had final approval of the article.
Contributor Information
L.L. Jasper, Email: ljasper@ualberta.ca
C. A. Jones, Phone: 780-492-2020, Email: cajones@ualberta.ca
J. Mollins, Email: Juliana.mollins@albertahealthservices.ca
S. L. Pohar, Email: sheri.pohar@yahoo.ca
L. A. Beaupre, Email: lauren.beaupre@ualberta.ca
References
- 1.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963–74. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Jones CA, Pohar S. Health-related quality of life after total joint arthroplasty: a scoping review. Clin Geriatr Med. 2012;28:395–429. doi: 10.1016/j.cger.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–21. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013;95-B:115–21. doi: 10.1302/0301-620X.95B1.29835. [DOI] [PubMed] [Google Scholar]
- 5.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–73. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 7.Martin KR, Kuh D, Harris TB, Guralnik JM, Coggon D, Wills AK. Body mass index, occupational activity, and leisure-time physical activity: an exploration of risk factors and modifiers for knee osteoarthritis in the 1946 British birth cohort. BMC Musculoskelet Disord. 2013;14:219. doi: 10.1186/1471-2474-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Institute of Health Information. Hip and Knee Replacements in Canada: Canadian Joint Replacement Registry 2014 Annual Report. 2014. https://secure.cihi.ca/free_products/CJRR%202014%20Annual%20Report_EN-web.pdf. Accessed 10 May 2015.
- 9.Hamilton DF, Howie CR, Burnett R, Simpson AH, Patton JT. Dealing with the predicted increase in demand for revision total knee arthroplasty: challenges, risks and opportunities. Bone Joint J. 2015;97-B:723–8. doi: 10.1302/0301-620X.97B6.35185. [DOI] [PubMed] [Google Scholar]
- 10.Liodakis E, Bergeron SG, Zukor DJ, Huk OL, Epure LM, Antoniou J. Perioperative complications and length of stay after revision total hip and knee arthroplasties: An analysis of the nsqip database. J Arthroplast. 2015;30:1868–71. doi: 10.1016/j.arth.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 11.Dieterich JD, Fields AC, Moucha CS. Short term outcomes of revision total knee arthroplasty. J Arthroplast. 2014;29:2163–6. doi: 10.1016/j.arth.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Morrison A, Moulton K, Clark M, Polisena J, Fiander M, Mierzwinsjii-Urban. English-Language Restriction When Conducting Systematic Review-Based Meta-Analyses: Systematic Review of Published Studies. Canadian Agency for Drugs and Technologies in Health. 2009. https://www.cadth.ca/media/pdf/H0478_Language_Restriction_Systematic_Review_Pub_Studies_e.pdf. Accessed 11 May 2015.
- 13.OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford. Centre for Evidence-Based Medicine. http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf. Accessed 10 May 2015.
- 14.Howick J, Chalmers I, Greenhalgh T, Heneghan C, Liberati A, Moschetti I et al. The 2011 Oxford CEBM Evidence Levels of Evidence (Introductory Document). Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/2011-oxford-cebm-levels-evidence-introductory-document/. Accessed 10 May 2015.
- 15.Scottish Intercollegiate Guidelines Network. SIGN Methodology Checklist 3: Cohort Studies. http://www.sign.ac.uk/methodology/checklists.html. Accessed 5 Jan 2014.
- 16.Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient. Clin Orthop Rel Res. 2007;464:83–7. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 17.Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J. 2013;95-B:636–42. doi: 10.1302/0301-620X.95B5.30271. [DOI] [PubMed] [Google Scholar]
- 18.Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Rel Res. 2006;452:28–34. doi: 10.1097/01.blo.0000229356.81749.11. [DOI] [PubMed] [Google Scholar]
- 19.Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85A:259–65. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Himanen AK, Belt EA, Lehto MU, Hamalainen MM. A comparison of survival of moulded monoblock and modular tibial components of 751 AGC total knee replacements in the treatment of rheumatoid arthritis. J Bone Joint Surg (Br) 2007;89B:609–14. doi: 10.1302/0301-620X.89B5.17950. [DOI] [PubMed] [Google Scholar]
- 21.Jamsen E, Peltola M, Eskelinen A, Lehto MU. Comorbid diseases as predictors of survival of primary total hip and knee replacements: a nationwide register-based study of 96 754 operations on patients with primary osteoarthritis. Ann Rheum Dis. 2013;72:1975–82. doi: 10.1136/annrheumdis-2012-202064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. J Arthroplasty. 2009;24:1061–7. doi: 10.1016/j.arth.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 23.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24:39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 24.Stiehl JB, Hamelynck KJ, Voorhorst PE. International multi-centre survivorship analysis of mobile bearing total knee arthroplasty. Int Orthop. 2006;30:190–9. doi: 10.1007/s00264-005-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kreder HJ, Grosso P, Williams JI, Jaglal S, Axcell T, Wai EK, et al. Provider volume and other predictors of outcome after total knee arthroplasty: a population study in Ontario. Can J Surg. 2003;46:15–22. [PMC free article] [PubMed] [Google Scholar]
- 26.Himanen AK, Belt E, Nevalainen J, Hamalainen M, Lehto M. Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis. Finnish Arthroplasty Register report on 8,467 operations carried out between 1985 and 1999. Acta Orthop. 2005;76:85–8. doi: 10.1080/00016470510030373. [DOI] [PubMed] [Google Scholar]
- 27.Namba RS, Inacio MC, Paxton EW, Ake CF, Wang C, Gross TP, et al. Risk of revision for fixed versus mobile-bearing primary total knee replacements. J Bone Joint Surgery AM. 2012;94:1929–35. doi: 10.2106/JBJS.K.01363. [DOI] [PubMed] [Google Scholar]
- 28.Namba RS, Cafri G, Khatod M, Inacio MC, Brox TW, Paxton EW. Risk factors for total knee arthroplasty aseptic revision. J Arthroplasty. 2013;28:122–7. doi: 10.1016/j.arth.2013.04.050. [DOI] [PubMed] [Google Scholar]
- 29.Blum MA, Singh JA, Lee GC, Richardson D, Chen W, Ibrahim SA. Patient race and surgical outcomes after total knee arthroplasty: an analysis of a large regional database. Arthrit Care Res. 2013;65:414–20. doi: 10.1002/acr.21834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schrama JC, Espehaug B, Hallan G, Engesaeter LB, Furnes O, Havelin LI, et al. Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplasty Register. Arthrit Care Res. 2010;62:473–9. doi: 10.1002/acr.20036. [DOI] [PubMed] [Google Scholar]
- 31.Bini SA, Chen Y, Khatod M, Paxton EW. Does pre-coating total knee tibial implants affect the risk of aseptic revision? Bone Joint J BR. 2013;95-B:367–70. doi: 10.1302/0301-620X.95B3.27585. [DOI] [PubMed] [Google Scholar]
- 32.Bordini B, Stea S, Cremonini S, Viceconti M, De PR, Toni A. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord. 2009;10:29. doi: 10.1186/1471-2474-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peltola M, Malmivaara A, Paavola M. Introducing a knee endoprosthesis model increases risk of early revision surgery. Clin Orthop Related Res. 2012;470:1711–7. doi: 10.1007/s11999-011-2171-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King KB, Findley TW, Williams AE, Bucknell AL. Veterans with diabetes receive arthroplasty more frequently and at a younger age. Clin Orthop Rel Res. 2013;471:3049–54. doi: 10.1007/s11999-013-3026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Julin J, Jamsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop. 2010;81:413–9. doi: 10.3109/17453674.2010.501747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdel MP, Morrey ME, Jensen MR, Morrey BE. Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am. 2011;93A:2072–8. doi: 10.2106/JBJS.J.01143. [DOI] [PubMed] [Google Scholar]
- 37.Lygre SHL, Espehaug B, Havelin LI, Furnes O, Vollset SE. Pain and function in patients after primary unicompartmental and total knee arthroplasty. J Bone Joint Surg Am. 2010;92A:2890–7. doi: 10.2106/JBJS.I.00917. [DOI] [PubMed] [Google Scholar]
- 38.Robertsson O, Ranstam J. No bias of ignored bilaterality when analysing the revision risk of knee prostheses: analysis of a population based sample of 44,590 patients with 55,298 knee prostheses from the national Swedish Knee Arthroplasty Register. BMC Musculoskelet Disord. 2003;4:1. doi: 10.1186/1471-2474-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am. 2011;93A:1588–96. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- 40.Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, et al. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am. 2013;95A:126–31. doi: 10.2106/JBJS.K.00607. [DOI] [PubMed] [Google Scholar]
- 41.Prieto-Alhambra D, Javaid MK, Judge A, Murray D, Carr A, Cooper C, et al. Association between bisphosphonate use and implant survival after primary total arthroplasty of the knee or hip: population based retrospective cohort study. BMJ. 2011;343:d7222. doi: 10.1136/bmj.d7222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Badawy M, Espehaug B, Indrekvam K, Engesaeter LB, Havelin LI, Furnes O. Influence of hospital volume on revision rate after total knee arthroplasty with cement. J Bone Joint Surg Am. 2013;95 doi: 10.2106/JBJS.L.00943. [DOI] [PubMed] [Google Scholar]
- 43.Harrysson OL, Robertsson O, Nayfeh JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Rel Res. 2004;421:162–168. doi: 10.1097/01.blo.0000127115.05754.ce. [DOI] [PubMed] [Google Scholar]
- 44.Ong KL, Lau E, Manley M, Kurtz SM. Effect of procedure duration on total hip arthroplasty and total knee arthroplasty survivorship in the United States Medicare population. J Arthroplasty. 2008;23:127–32. doi: 10.1016/j.arth.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 45.Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg (Br) 2011;93:293–7. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- 46.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379:1331–40. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 47.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–36. [PMC free article] [PubMed] [Google Scholar]
- 48.Statistics Canada. Population Projections for Canada (2013 to 2063), Provinces and Territories (2013 to 2038). 2014. http://www.statcan.gc.ca/pub/91-520-x/91-520-x2014001-eng.htm. Accessed 8 January 2016.
- 49.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–7. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Public Health Agency of Canada. Preventing Chronic Disease Strategic Plan 2013–2016. 2013. http://publications.gc.ca/collections/collection_2014/aspc-phac/HP35-39-2013-eng.pdf. Accessed 13 January 2016.
- 51.Hung WW, Ross JS, Boockvar KS, Siu AL. Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatr. 2011;11:47. doi: 10.1186/1471-2318-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fehring TK, Murphy JA, Hayes TD, Roberts DW, Pomeroy DL, Griffin WL. Factors influencing wear and osteolysis in press-fit condylar modular total knee replacements. Clin Orthop Rel Res. 2004;428:40–50. doi: 10.1097/01.blo.0000148853.37270.67. [DOI] [PubMed] [Google Scholar]
- 53.Gioe TJ, Killeen KK, Grimm K, Mehle S, Scheltema K. Why are total knee replacements revised? analysis of early revision in a community knee implant registry. Clin Orthop Rel Res. 2004;428:100–6. doi: 10.1097/01.blo.0000147136.98303.9d. [DOI] [PubMed] [Google Scholar]
- 54.Inacio MC, Cafri G, Paxton EW, Kurtz SM, Namba RS. Alternative bearings in total knee arthroplasty: risk of early revision compared to traditional bearings: an analysis of 62,177 primary cases. Acta Orthop. 2013;84:145–52. doi: 10.3109/17453674.2013.784660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adams AL, Paxton EW, Wang JQ, Johnson ES, Bayliss EA, Ferrara A, et al. Surgical outcomes of total knee replacement according to diabetes status and glycemic control, 2001 to 2009. J Bone Joint Surg Am. 2013;95:481–7. doi: 10.2106/JBJS.L.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berend ME, Davis PJ, Ritter MA, Keating EM, Faris PM, Meding JB, et al. “Thicker” polyethylene bearings are associated with higher failure rates in primary total knee arthroplasty. J Arthroplasty. 2010;25:17–20. doi: 10.1016/j.arth.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 57.Curtin B, Malkani A, Lau E, Kurtz S, Ong K. Revision after total knee arthroplasty and unicompartmental knee arthroplasty in the Medicare population. J Arthroplasty. 2012;27:1480–6. doi: 10.1016/j.arth.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 58.Dy CJ, Wilkinson JD, Tamariz L, Scully SP. Influence of preoperative cardiovascular risk factor clusters on complications of total joint arthroplasty. Am J Orthop. 2011;40:560–5. [PubMed] [Google Scholar]
- 59.Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI. Early failures among 7,174 primary total knee replacements: a follow-up study from the Norwegian Arthroplasty Register 1994–2000. Acta Orthop Scand. 2002;73:117–29. doi: 10.1080/000164702753671678. [DOI] [PubMed] [Google Scholar]
- 60.Gothesen O, Espehaug B, Havelin L, Petursson G, Furnes O. Short-term outcome of 1,465 computer-navigated primary total knee replacements 2005–2008. Acta Orthop. 2011;82:293–300. doi: 10.3109/17453674.2011.575743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hooper GJ, Rothwell AG, Hooper NM, Frampton C. The relationship between the American Society of Anesthesiologists physical rating and outcome following total hip and knee arthroplasty an analysis of the New Zealand Joint Registry. J Bone Joint Surg Am. 2012;94A:1065–70. doi: 10.2106/JBJS.J.01681. [DOI] [PubMed] [Google Scholar]
- 62.Johnson TC, Tatman PJ, Mehle S, Gioe TJ. Revision surgery for patellofemoral problems: should we always resurface? Clin Orthop Rel Res. 2012;470:211–9. doi: 10.1007/s11999-011-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCleery MA, Leach WJ, Norwood T. Rates of infection and revision in patients with renal disease undergoing total knee replacement in Scotland. J Bone Joint Surg (Br) 2010;92:1535–9. doi: 10.1302/0301-620X.92B11.23870. [DOI] [PubMed] [Google Scholar]
- 64.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92A:2143–9. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 65.Robertsson O, Knutson K, Lewold S, Goodman S, Lidgren L. Knee arthroplasty in rheumatoid arthritis a report from the Swedish Knee Arthroplasty Register on 4,381 primary operations 1985–1995. Acta Orthop Scand. 1997;68:545–53. doi: 10.3109/17453679708999024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article and its additional files.


