Abstract
Introduction:
This is a report of a mechanical failure of an S-ROM revision total knee prosthesis. The prosthesis was used as a revision implant following deep peri-prosthetic infection in a morbidly obese male. The prosthesis failed on both the femoral and tibial sides at the modular metaphyseal stem junctions and required a further revision using the same type of implant after infection was excluded.
Case Presentation:
A 57 year old male had previously undergone a left total knee arthroplasty in 1999 for osteoarthritis. He acquired a late deep peri-prosthetic infection with a multi-resistant Staphylococcus epidermidis. The organism was sensitive to vancomycin and rifampicin. A two stage revision was undertaken after clinical signs of infection had resolved and blood parameters had normalized. Intra-operative gram stain was negative for micro-organisms and frozen section of deep tissue was less than five polymorphs per high power field. A cemented S-ROM prosthesis was implanted using a coronal tibial osteotomy and a lateral release for exposure. After three years of the second stage of revision, the patient again presented to the orthopaedic department after reportedly falling on a wet floor six weeks ago.
Conclusion:
Radiographically, there was a broken tibial wire, osteolysis and pedestal formation around both the femoral and distal tibial stem extensions. The prosthesis was bent at the proximal tibial sleeve and stem junction. The prosthesis was considered loose with mechanical failure. At implant removal, it was noted that the femoral and tibial components at the modular metaphyseal sleeve-stem junction were fractured. Surgeons should be cautious in the use of these implants in morbidly obese patients where the stresses generated maybe above the yield stress of the material and the frictional forces that may overcome the modular taper junction’s locking mechanism.
Keywords: Revision Knee, Mechanical Failure
Introduction
This is a report of a mechanical failure of an S-ROM revision total knee prosthesis. The prosthesis was used as a revision implant following deep peri-prosthetic infection in a morbidly obese male.
The prosthesis failed on both the femoral and tibial sides at the modular metaphyseal stem junctions and required a further revision using the same type of implant after infection was excluded.
Case Presentation
A 57 year old male had previously undergone a left total knee arthroplasty in 1999 for osteoarthritis. He acquired a late deep peri-prosthetic infection with a multi-resistant Staphylococcus epidermidis. The organism was sensitive to vancomycin and rifampicin. A two stage revision was undertaken after clinical signs of infection had resolved and blood parameters had normalized. Intra-operative gram stain was negative for microorganisms and frozen section of deep tissue was less than five polymorphs per high power field [1-5].
A cemented S-ROM prosthesis was implanted using a coronal tibial osteotomy and a lateral release for exposure [6,7].
The primary surgeon followed all the guidelines as described in the instructional booklet for the S-ROM implant. A cemented SROM modular tibial plate plus tibial sleeve and an uncemented 15 x 100 mm press fit tibial stem extension was inserted. The femoral side comprised of a cemented Noiles rotating hinge component, a cemented 46 mm S-ROM femoral sleeve which was matched with an uncemented 17 x 150 mm press fit femoral extension. The implant reconstruction was completed using a 12 mm small SROM Noiles rotating hinge polyethylene and axle inserted from the medial side. The patella was not resurfaced secondary to marked bone deficiency.
Long term antibiotics were prescribed and follow up at regular intervals for the next eight months revealed that all of the patient’s blood parameters; erthrocyte sedimentation rate (ESR), C-reactive protein (CRP) and white cell count (WCC) were within normal limits. Radiographically the knee was unremarkable. The patient carried out normal activities of daily living. The patient presented three years following the second stage of revision after reportedly falling on a wet floor six weeks previously. Prior to the fall, the patient did not require any analgesia and reported normal function with activities of daily living and clinically had a range of motion from zero to one hundred and five degrees. After the fall, the patient’s function became increasingly impaired and required crutches for assisted ambulation, which was limited to less than fifty meters. He was required to climb stairs one at a time with a railing and required assisted transfers. Clinically, his height was 173.5 cm and weight 140 kilograms, exhibited an antalgic gait, a well healed surgical scar, an effusion and tenderness around the pes anserinus. The knee had a range of motion of zero to one hundred degrees and quadriceps power was grade four.
Radiographically, there was a broken tibial wire, osteolysis and pedestal formation around both the femoral and distal tibial stem extensions. The prosthesis was bent at the proximal tibial sleeve and stem junction. The ESR and CRP were 17 and 16.7, respectively. A bone scan showed moderate uptake around the prosthesis, especially the proximal medial tibia and the patella. Labelled white cell scan exhibited stress remodelling and synovitis but was not consistent with infection [8]. There was no catastrophic bone loss around the failed modular junction as it is known that revision modular femoral components can fail if the modular junction is unprotected/unsupported.
The prosthesis was considered loose with mechanical failure. Due to the morbid obesity of the patient, he was referred for laparoscopic gastric banding to facilitate weight loss prior to his revision total knee arthroplasty. Once his weight had decreased to approximately 120 kilograms the revision knee procedure was undertaken. Increasing morbid obesity, and with body mass index (BMI) increasing over the years, bariatric surgery has been well proven in the past few years in treating obesity.
Exposure was through the previous incision and once again a coronal tibial tubercle osteotomy was undertaken. The pseudo capsule sample of frozen section revealed less than five white cells per high power field, excluding active infection. There was marked metallosis with loosening of both the femoral and tibial components at the cement-bone interface. At implant removal it was noted that the femoral and tibial components at the modular metaphyseal sleeve-stem junction were fractured.
Extensive debridement was carried out on both the tibial and femoral sides. The host bone was deficient with Engh type 3 defects in both the distal femur and proximal tibia [9-11-13]. The uncontained defects were reconstructed using anatomic specific structural and morcellised impaction allograft. Another S-ROM modular revision stemmed implant was cemented into position (Fig. 1).
Figure 1.
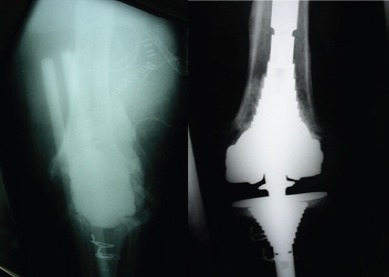
Radiographs showing the preoperative and postoperative revision reconstruction using an S-ROM modular knee revision implant.
Discussion
Macroscopic investigation of the failure mode of the tibial stem presents with a typical fatigue failure, where a crack initiated and propagated until catastrophic failure occurred [12, 13]. Failure has occurred at the tip of the male taper of the tibial tray, outside of the female taper junction. The femoral component has failed at the mouth of the female taper junction. Optical microscopy of the tibial fracture surface presents a smooth region where the fracture has initiated from and a path around the fracture surface where the crack has propagated (Fig. 2a). (Fig. 2b) illustrates that the crack is located at the level of the machining groove in the male taper, which is hollow of the tibial component. There is no evidence of fretting or corrosion occurring at the tibial taper junction (Fig. 3). The femoral taper junction presents with fretting on the male taper (Fig. 4). The female taper junction in the femoral component also presents with fretting and secondary fracture (Fig. 5). A segment of the female taper illustrates a crack initiation site (Fig 6). The fretting of the male femoral component taper is evidence that the taper junction became loose because of cyclic bending of the junction due to the normal daily activities of the patient. This led to the fretting occurring at the junction, followed by loosening and fatigue failure of the taper mouth. Based on the patient’s weight, the stress magnitudes at the failure sites are over the failure magnitudes of the implant material (Table 1). We believe the failure is to be related to the gross obesity of the patient and subsequent loosening components.
Figure 2a.
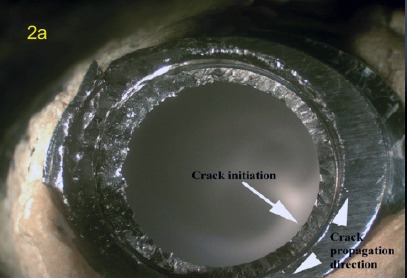
Photograph of the fracture initiation site and direction of propagation around the taper junction.
Figure 2b.
Photograph illustrating the crack location on and close to the machining groove
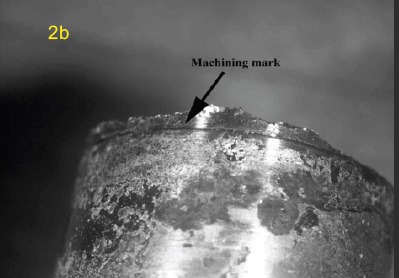
Figure 3.

Photograph showing no fretting corrosion at the outer region of tibial taper junction.
Figure 4.

Photograph presenting mechanical fretting of the male taper junction.
Figure 5.
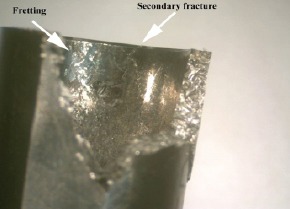
Photograph illustrating the mechanical fretting and secondary cracking of the female taper junction.
Figure 6.
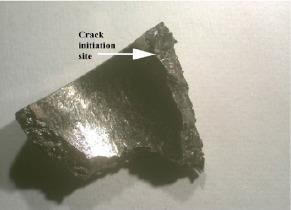
Photograph of a female taper junction fracture fragment showing a crack initiation site.
Table 1.
Calculation of Yield stress magnitudes at the failure sites.
| Implant failure Location | Minimum Yield stress | Calculated Yield Stress |
|---|---|---|
| [MPa](ASTM 1537) | [MPa] based on patient’s weight | |
| Femoral Taper | 827 | 1493.64 |
| Tibial Taper | 827 | 1011.2 |
The development of modular stems has a recognized potential area for fatigue failure in the stem-condyle junction. However, it is difficult to manage interoperatively when customising for bone loss, stability and joint line. Westrich et al. reported cases of failure in other locations of an implant [14]. There have been reports of failures occurring at the stem-condyle junction [15]. All failures were associated with locking screw failure with dissociation of the stem from the condylar portion of the component. The total condylar III component in that series has a flat on flat stemcomponent with no morse taper. They had also noted that the Insall-Burstein design that has a morse taper at its junction has had no reported fractures in the literature.
Conclusion
The S-ROM revision implant in this case does have a Morse type taper yet failure occurred. Its assembly requires in-line impaction for the tapers to lock and the use of a “T” handle hex screw driver for the tightening the locking bolts and no wrenches are required.
Clinical Message.
The authors would favor caution in the use of these implants in morbidly obese patients where the stresses generated may be above the yield stress of the material and the frictional forces that may overcome the modular taper junction’s locking mechanism.
Biography


Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Della Valle CJ, Bogner E, Desai P, Lonner JH, Adler E, Zuckerman JD, Di Cesare PE. Analysis of frozen sections of intraoperative specimens obtained at the time of reoperation after hip or knee resection arthroplasty for the treatment of infection. J Bone Joint Surg Am. 1999;81(5):684–9. doi: 10.2106/00004623-199905000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Lonner JH, Desai P, Dicesare PE, Steiner G, Zuckerman JD. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg. Am. 996;78(10):1553–8. doi: 10.2106/00004623-199610000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Lonner JH, Barrack R, Fitzgerald RH, Jr, Hanssen AD, Windsor ER. Infection in total knee arthroplasty: part I. Classification, prophylaxis, and diagnosis. American Journal of Orthopedics. 1999;28(9):530–5. [PubMed] [Google Scholar]
- 4.Lotke P A, Lonner J H. Lippincroft Williams and Wilkins Chapter 22. In: Thompson R C Jr, editor. Staged Revision of the Infected Total Knee Arthroplasty Knee Arthroplasty. 2nd edition. Philadelphia: 2003. pp. 345–370. [Google Scholar]
- 5.Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and it’s clinical relevance in prosthesis failure. Clinical Orthopaedics & Related Research. 1976;117:221–40. [PubMed] [Google Scholar]
- 6.Bruce WJJ, Rooney JSR, Hutabarat SR, et al. Exposure in difficult total knee arthroplasty using coronal tibial tubercle osteotomy. Journal of Orthopaedic Surgery. 2000;8(1):61–65. doi: 10.1177/230949900000800111. [DOI] [PubMed] [Google Scholar]
- 7.Whiteside LA. Exposure options in the difficult knee. Orthopedics. 2001;24(9):895–6. doi: 10.3928/0147-7447-20010901-33. [DOI] [PubMed] [Google Scholar]
- 8.Chik KK, Magee MA, Bruce WJ, Higgs RJ, Thomas MG, Allman KC, Van der Wall H. Tc-99m stannous colloid-labeled leukocyte scintigraphy in the evaluation of the painful arthroplasty. Clinical Nuclear Medicine. 1996;21(11):838–43. doi: 10.1097/00003072-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Engh GA, Ammeen DJ. Bone loss Revision Total Knee Arthroplasty: Defect Classification and Alternatives for Reconstruction. Instructional Course Lectures. 1999;48:167–175. [PubMed] [Google Scholar]
- 10.Engh G A, Herzwarm P J, Parks N L. Treatment of major defects of bone with bulk allografts and stemmed components during total knee arthroplasty. J Bone Joint Surg. Am. 1997;79(7):1030–1039. doi: 10.2106/00004623-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Hanssen A D. In: Master Techniques in Orthopaedic Surgery Knee Arthroplasty. 2nd Edition. Chapter 21. Thompson R C Jr, editor. Lippincroft Williams and Wilkins; 2003. pp. 321–344. [Google Scholar]
- 12.Ashby M. I.S.o.M.S.a. Technology. Vol. 34. San Diego, CA, USA: Elsevier Science and technology Books; 1980. Engineering Materials 1: An introduction to their properties and applications; p. 278. [Google Scholar]
- 13.Hull D. Fractography Observing, Mearsuring and Interpreting Fracture Surface Topography. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- 14.Westrich G A, Kidaka C, Winsor RE. Disengagement of a locking screw from a modular stem in revision total knee arthroplasty. A report of three cases. J Bone Joint Surg Am. 1997;79(2):254–8. [PubMed] [Google Scholar]
- 15.Lim LA, Trousdale RT, Berry DJ, Hanssen AD. Failure of the Stem- Condyle Junction of a Modular Femoral Stem in Revision Total Knee Arthroplasty: A report of five cases. J Arthroplasty. 2001;16(1):128–132. doi: 10.1054/arth.2001.16496. [DOI] [PubMed] [Google Scholar]


