Abstract
Introduction:
Chances of avascular necrosis of acetabulum are rare as it enjoys a rich blood supply. But cases of post - traumatic avascular necrosis of acetabulum following fracture of posterior column have been well documented. Importance of identifying and suspecting the avascular necrosis of acetabulum is essential in cases of failed fixation of fracture acetabulum, previously operated using extensile approach to acetabulum; either extended anterior ilio - femoral or tri - radiate approach. Such patients usually present with repeated deep bone infection or with early failure of fixation with aseptic loosening and migration of its components. We present a similar case.
Case Presentation:
40 years female presented with inadequately managed transverse fracture of left acetabulum done by anterior extended ilio-inguinal approach. The fixation failed. She presented 6 months later with painful hip. Cemented total hip replacement was performed with reconstruction of acetabulum by posterior column plating. Six months postoperatively patient presented with dislodgement of cup, pelvic discontinuity and sinus in the thigh. Two stage revision surgery was planned. First implant, removal; debridement and antibiotic spacer surgery was performed. At second stage of revision total hip replacement, patient had Paprosky grade IIIb defect in acetabulum. Spacer was removed through the posterior approach. Anterior approach was taken for anterior plating. Intra-operatively external iliac pulsations were found to be absent so procedure was abandoned after expert opinion.
Postoperatively digital subtraction angiography demonstrated a chronic block in the external iliac artery and corona mortis was the only patent vascular channel providing vascular to the left lower limb. Thus, peripheral limb was stealing blood supply from the acetabulum to maintain perfusion. Patient was ultimately left with pelvic discontinuity, excision arthroplasty and pseudoarthrosis of the left hip.
Conclusions:
Avascular necrosis of acetabulum is a rare entity & often not recognized. One should be suspicious about diagnosis of avascular necrosis of acetabulum in select cases of failed acetabular fixation, previously operated via extensile anterior ilio - inguinal approach. Angiographic evaluation is essential in revision cases of failed acetabular fixation. Corona mortis (crown or circle of death) can sometimes act as a savior of limb.
Keywords: Avascular Necrosis Acetabulum, Corona Mortis, Pelvic Discontinuity
Introduction
Avascular necrosis of acetabulum is a pathology, which has not been extensively studied. Acetabulum enjoys a rich blood supply from the anastomotic network of its surrounding muscles. Among the major contributors are the ilio - lumbar artery, obturator artery, internal pudendal artery, superior and inferior gluteal arteries and the external iliac artery [1]. So the chances of avascular necrosis of acetabulum are rare.
But the cases of post - traumatic avascular necrosis of acetabulum following fracture of the posterior column have been well documented. Post - traumatic avascular necrosis of acetabulum is usually a result of either high velocity trauma leading to excessive injury to the soft tissues or can be iatrogenically induced. Iatrogenically induced post - traumatic avascular necrosis of acetabulum is usually a result of the extensile approach and excessive soft tissue stripping at time of fracture fixation [2, 3, 4]. Other factors may also contribute to avascular necrosis of acetabulum like, marked fracture comminution or displacement and delay between the time of injury and the surgical procedure. Dana Mears [4] in his article has put light on the importance of identifying and suspecting avascular necrosis of acetabulum in cases of failed fixation of fracture acetabulum, previously operated using extensile approach to acetabulum; either extended anterior ilio - femoral or tri - radiate approach. Such patients usually present with repeated deep bone infection or with early failure of fixation with aseptic loosening and migration of its components.
We are reporting an interesting case of closed transverse fracture of acetabulum, which ended in pelvic discontinuity, excision arthroplasty and pseudoarthrosis of hip.
Case Presentation
40 years old female presented with transverse fracture of left acetabulum (Fig 1). Patient was managed elsewhere with anterior extended ilio-inguinal approach, with inadequate single screw fixation. The fixation failed (Fig 2). She presented 6 months later with painful hip. The patient was managed with reconstruction of acetabulum by posterior column plating, impaction bone grafting; from the morselized bone grafts harvested from the femoral head, fixed with mesh and multiple screws spanning both the columns of acetabulum [5]; and a cemented total hip replacement implant (Fig 3). The mesh acted as internal buttress splint as well as protected the bone grafts. As posterior column is the main weight-bearing pillar during walking, posterior column plating was done to support posterior column union. Autologous bone grafts used for filling up the central defect gave support to the cemented cup. Patient was asked to weight bear with a walker till bone grafts consolidated. Post – operative course of patient was uneventful.
Figure 1.

Initial X – ray of the patient showing transverse fracture of left acetabulum.
Figure 2.

X – ray 6 months post trauma showing failed fixation of the transverse fracture of left acetabulum.
Figure 3.

X – ray showing the revision of the inadequate screw fixation of the trasverse fracture of acetabulum with posterior column plating, impaction bone grafting with mesh and cemented total hip replacement
Six months post - operatively patient presented with dislodgement of cup, pelvic discontinuity (Fig 4), and sinus in thigh (Fig 6). Patient was planned for a two - staged revision surgery. In the first stage implant removal, and antibiotic spacer insertion was done (Fig 7). Infection healed at 3 months following the spacer surgery (Fig 8). Usual protocol of antibiotics followed spacer insertion. Initially intravenous antibiotics were given till C-reactive protein (CRP) came to normal followed by oral antibiotics for a total period of 6 weeks. Drug holiday for a period of 6 weeks was given afterwards. CRP & Erythrocyte sedimentation rate (ESR) returned to normal & clinically infection healed.
Figure 4.

ray taken 6 months after the posterior column plating, impaction bone grafting, mesh fixation and cemented total hip replacement showing failed fixation, dislodgement of the acetabular cup and pelvic discontinuity.
Figure 5.

Clinical photograph 6 months after the posterior column plating, impaction bone grafting, mesh fixation and cemented total hip replacement showing draining sinus along the inferior aspect of the incision of surgery on the lateral aspect of left thigh.
Figure 6.

Clinical photograph 6 months after the posterior column plating, impaction bone grafting, mesh fixation and cemented total hip replacement showing draining sinus along the inferior aspect of the incision of surgery on the lateral aspect of left thigh.
Figure 7.

Clinical photograph of the lateral aspect of left thigh taken 3 months following the antibiotic impregnated cement hip spacer surgery. Shwing healed sinus.
Figure 8.
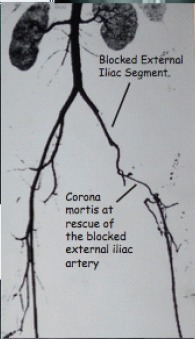
The image is of the Digital Substraction Angiography of the left lower limb showing block in the left external iliac circulation and the patent corona mortis at the rescue of the blocked external iliac circulation providing blood supply to the distal left lower limb.
Patient had Paprosky grade IIIb defect [6] at the time of second stage of revision total hip replacement. Spacer was removed through postero-lateral approach. Anterior approach was taken for anterior plating. On exploring anteriorly, external iliac pulsations were not felt. Vascular surgeons were called in intra - operatively & it was unanimously decided to abandon the procedure.
Postoperatively digital subtraction angiography of affected limb demonstrated chronic block in the external iliac artery and vascularity of the limb was being maintained by corona mortis [7], receiving blood supply from the obturator artery, a branch of internal iliac artery (Fig 8). Retrospectively analyzing, this case at no point of time did have any signs, which could have suggested vascular insufficiency in the lower limb. Patient was ultimately left with pelvic discontinuity, excision arthroplasty and pseudoarthrosis of the left hip (Figs 9 &10).
Figure 9.

This is the final X – ray of the patient showing pelvic discontinuity, excision arthroplasty and pseudoarthrosis of the left hip.
Figure 10.
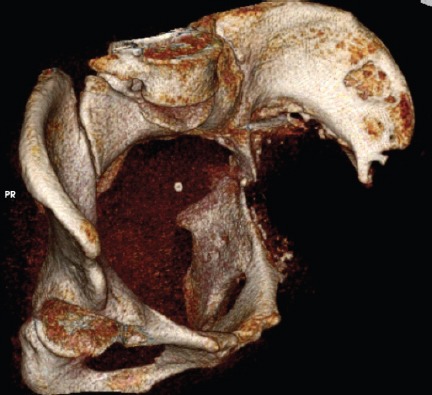
This is the 3D reconstruction CT – Scan image of the patient showing pelvic discontinuity.
At further follow up patient was not only affected physically but also mentally and financially. She felt helpless and depressed all the time. After undergoing four surgeries, patient was financially drained and thus was not willing to undergo any further management for her pathology of hip region. She rather accepted shortening of her limb and always used walker for ambulation. Due to the pathology she had to quit her job, as she could ambulate only within her house. Thus the fracture of the hip region left her physically and mentally handicapped and financially dependent.
Discussion
While discussing this interesting case of transverse fracture of acetabulum, which ended up with pelvic discontinuity, excision arthroplasty, and pseudoarthrosis of the left hip, we wish to put light on the following important facts:
Our patient was similar to the select few Dana Mears’s [4] series of cases, which were earlier, operated with extended approach to acetabulum and presented with resistant deep bone infection and failure of implant components and ultimately the patient landed with Girdlestone type of resection arthroplasty. He proposed that such a presentation could be result of the avascular necrosis of the acetabulum. The findings of our case parallel the propositions of Dana Mears.
In this case corona mortis regarded, as artery of death, was a rescue for the limb, as evidenced by the digital subtraction angiography scans. In our case there was a block in external iliac artery, which is the usual artery supplying lower limb. This could either be post - traumatic or it can be as a result of the earlier surgery done through extended ilio – inguinal approach. Also, it was evident from the scans that vascular supply to limb is only through corona mortis.
Corona mortis, a Latin word literally “means crown or circle of death”. It is an anatomical variation, which is present in around 25% of cases [8]. It is a communication between the internal iliac and external iliac, which is often encountered at the time of exposure in ilio-inguinal approach [9]. If it is injured, can bleed torrentially and can cause death, if not attended to [10]. But instead in our case, it was a savior; as, it was the only communication between the internal iliac and external iliac circulation and thus the only way through which lower limb was being perfused. But in the bargain, the lower limb perfusion was stealing blood supply from acetabulum via corona mortis. This led us to presume that in our case vascular steal type phenomenon occurred which led to decreased blood supply to acetabulum, ultimately causing avascular necrosis of acetabulum. Infection, trauma could have been additional contributory factors to avascular necrosis. Deep bone infection could even be the outcome of avascular bed.
Thus, as a result of vascular steal, leading to avascular necrosis and infection; patient developed repeated failure of implant and non - union of fracture acetabulum, which ultimately culminated into pelvic discontinuity, excision arthroplasty and pseudoarthrosis of left hip. In the absence of sound vascular bed of acetabulum no reconstruction of the acetabulum could ever work, may it be impaction bone grafting with mesh, cage with cemented cup or even perhaps spongy metal augments with cup cage reconstruction.
In our case the diagnosis of avascular necrosis could best be exemplified by retrospective presumption, as, our case had combined findings of nonunion along with avascularity; so, histopathology would not provide conclusive diagnosis. Hence, histopathology was not performed. Also in Dana Mears’s series, he performed trephine biopsies along with the aspirations of hip joint, of all cases undergoing revision arthroplasty, to rule out infection rather than to prove the diagnosis of avascular necrosis. Histopathology, serendipitously confirmed the diagnosis of avascular necrosis. Dana Mears also concluded that, infection could occur due to avascularity of the site, which could be true in our case too.
Conclusion
Avascular necrosis of the acetabulum is a rare entity & often not recognized.
One should be suspicious about the diagnosis of avascular necrosis of acetabulum in select cases of failed acetabular fixation, previously operated via extensile anterior ilio - inguinal approach; as, there are no diagnostic radiological or clinical signs described to detect avascular necrosis of acetabulum, especially in the presence of fracture. There are higher chances of failure of fixation or arthroplasty in such select cases. Resistant deep bone infection, especially in select cases of failed acetabular fixation operated via the extensile anterior ilio - inguinal approach, can be a clinical pointer towards avascularity of the acetabulum. Angiographic evaluation is essential in revision cases of failed acetabular fixation, especially in cases where the previous surgery was performed by the extended anterior ilio – inguinal approach. Corona mortis - “crown or circle of death”, can sometimes act as a savior of limb, as in this case. Select cases of failed acetabular fixation, previously operated via the extensile anterior ilio - inguinal approach, finally tend to culminate in pelvic discontinuity, non – union of acetabulum, excision arthroplasty and pseudoarthrosis of hip.
Clinical Message.
A clinician must keep in mind possibility of avascular necrosis of acetabulum while dealing with cases of fracture acetabulum especially managed earlier with extensile approach to acetabulum and presenting with failed fixation and/or resistant infection. Angiographic evaluation is a must before intervention in such difficult cases and outcome of intervention should be guarded and explained to the patient.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Itokazu M, Takahashi K, Matsunaga T, Hayakawa D, Emura S, Isono H, et al. A study of the arterial supply of the human acetabulum using a corrosion casting method. Clin Anat. 1997;10(2):77–81. doi: 10.1002/(SICI)1098-2353(1997)10:2<77::AID-CA1>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 2.LetourneI E, Judet R, editors. Fractures of the Acetabulum. ed 2. New York, NY: Springer-Verlag; 1993. p. 545. [Google Scholar]
- 3.Judet R. Les fractures du cotyle. ActalOrthopBelge. 1966;32:469–476. [PubMed] [Google Scholar]
- 4.Mears D. Avascular necrosis of the acetabulum. Operative techniques in orthopaedics. 1997 Jul 7;(No. 3) [Google Scholar]
- 5.Paprosky WG, Magrus RE. Principles of bone grafting in revision total hip arthroplasty: Acetabular techniques. ClinOrthop. 1994;298:147–155. [PubMed] [Google Scholar]
- 6.Wayne G, Paprosky, et al. Acetabular defect classification and surgical reconstruction in revision arthroplasty: A 6-year follow-up evaluation. Journal of Arthroplasty. 1994 Feb 9;(1) doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 7.Tornetta Paul., III Corona Mortis: Incidence and Location. Clinical Orthopaedics & Related Research. 1996 Aug;329 [PubMed] [Google Scholar]
- 8.Stavropoulou-Deli A, Anagnostopoulou S. Corona mortis: anatomical data and clinical considerations. Aust N Z J ObstetGynaecol. 2013 Jun;53(3):283–6. doi: 10.1111/ajo.12076. doi: 10.1111/ajo.12076. Epub 2013 Apr 4. [DOI] [PubMed] [Google Scholar]
- 9.Darmanis S, Lewis A, Mansoor A, Bircher M. Corona mortis: an anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat. 2007 May;20(4):433–9. doi: 10.1002/ca.20390. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez L A. Hemorrhage of the “corona mortis”. Its treatment. Prensa Med Argent. 1968 Apr 19;55(8):382–5. [PubMed] [Google Scholar]


