Abstract
Fulminant myocarditis is a rare but potentially life-threatening illness caused by 5-fluorouracil cardiotoxicity. Data supporting the use of extracorporeal membrane oxygenation for the treatment of fulminant myocarditis are limited.
A 49-year-old, previously healthy white man, recently diagnosed with anal squamous cell carcinoma, developed severe chest pain hours after completing his first 96-hour intravenous 5-fluorouracil treatment. Over a period of 3 days from onset of symptoms, the patient developed cardiogenic shock secondary to fulminant myocarditis induced by 5-fluorouracil cardiotoxicity. This required emergency initiation of extracorporeal membrane oxygenation. The patient's systolic function recovered by day 5, and on the 17th day he was discharged in hemodynamically stable condition, without symptoms of heart failure.
This case shows the importance of prompt recognition of cardiogenic shock secondary to 5-fluorouracil–induced myocarditis and how the immediate initiation of extracorporeal membrane oxygenation can restore adequate tissue perfusion, leading to myocardial recovery and ultimately the survival of the patient.
Keywords: Antineoplastic agents/cardiotoxicity, colorectal neoplasms/drug therapy, ECMO, male, fluorouracil/adverse effects/therapeutic use/toxicity, middle aged, myocarditis/chemically induced, treatment outcome
Chemotherapy regimens based on 5-fluorouracil (5-FU) are frequently administered in the treatment of gastrointestinal malignancies—especially colorectal carcinomas.1,2 Fulminant myocarditis is a rare but potentially life-threatening illness caused by 5-FU cardiotoxicity.3,4 Commonly presenting as chest pain, cardiac toxicity has manifestations that can include ischemic changes evident upon electrocardiography (ECG), and arrhythmias, myocardial infarction, heart failure, cardiogenic shock, and sudden death, with higher incidences in patients who have existing cardiac disease.5 Although salvage extracorporeal membrane oxygenation (ECMO) has been used successfully to treat various forms of cardiogenic shock, no data exist for the use of ECMO in the treatment of 5-FU–induced myocarditis. We report a case in which ECMO rescued a patient who was in cardiogenic shock resulting from 5-FU–associated fulminant myocarditis.
Case Report
In May 2014, a 49-year-old white man with newly diagnosed anal squamous cell carcinoma was being treated with combination therapy: radiotherapy, 5-FU, and mitomycin-C. At the start of chemotherapy, he had excellent exercise capacity and no history of cardiac disease to our knowledge. Hours after completing the first cycle of intravenous 5-FU treatment, the patient developed severe chest pain and presented at our emergency room.
Upon arrival, the patient was alert, oriented, and hemodynamically stable, with a heart rate (HR) of 100 beats/min and a blood pressure (BP) of 100/70 mmHg. An ECG revealed diffuse ST-segment elevations (Fig. 1), and laboratory data included an elevated troponin I level (0.79 ng/mL). He was diagnosed with an ST-segment-elevation myocardial infarction and was transferred to the cardiac catheterization laboratory on an emergency basis.
Fig. 1.
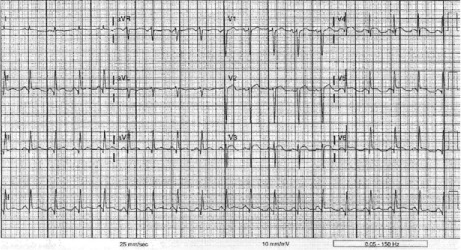
Electrocardiogram at presentation shows diffuse ST-segment elevation.
Coronary angiography revealed occlusion of the right coronary artery, which was well collateralized by the left anterior descending coronary artery (Fig. 2), and the absence of any other obstructive lesions. Left ventriculography revealed global hypokinesis (Fig. 3), with a left ventricular ejection fraction (LVEF) of 0.10 to 0.15 and a left ventricular (LV) end-diastolic pressure of 48 mmHg. An intra-aortic balloon pump (IABP) was inserted on an emergency basis. Subsequently, the patient developed a ventricular tachycardia, which required electrical defibrillation. Spontaneous circulation was restored, but the patient remained in cardiogenic shock, needing endotracheal intubation and multiple vasopressors. Despite aggressive resuscitation, the patient was cold, mottled, acidotic (pH, 7.1), and hemodynamically unstable (BP, 72/46 mmHg).
Fig. 2.
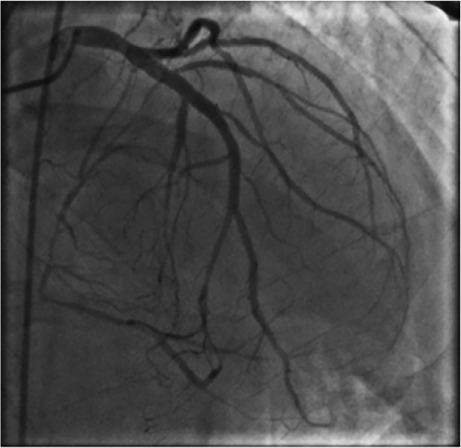
Coronary angiogram shows occlusion of the right coronary artery, which is well collateralized by the left anterior descending coronary artery.
Fig. 3.
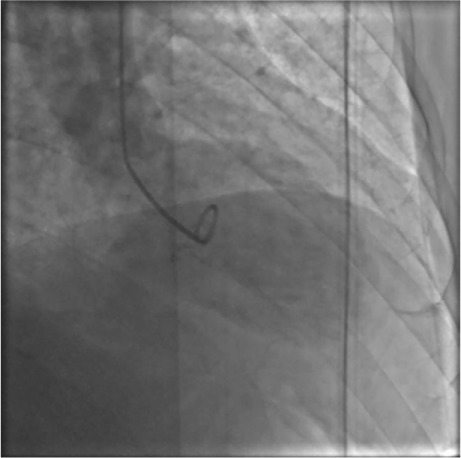
Left ventriculogram shows global hypokinesis at the time of cardiac catheterization, before the initiation of extracorporeal membrane oxygenation.
Supplemental motion image is available for Figure 3 (2.6MB, mp4) .
Extracorporeal Membrane Oxygenation
Percutaneous venoarterial ECMO was quickly initiated for hemodynamic support. The left common femoral artery and vein were cannulated simultaneously with heparin-coated 17F and 21F cannulas, respectively, and support was initiated at a pump flow-rate of 3 L/min. The patient's mottling resolved, his extremities were warm to the touch, and his vital signs stabilized (HR, 70 beats/min; BP, 110/59 mmHg; and pH, 7.3). Standard ECMO protocols for coagulation, monitoring, and sedation were followed. Echocardiograms obtained 12 hours after starting ECMO again indicated severe biventricular hypokinesis (LVEF, <0.10) (Fig. 4).
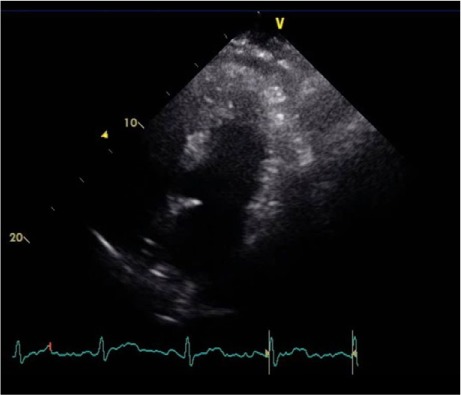
Fig. 4.
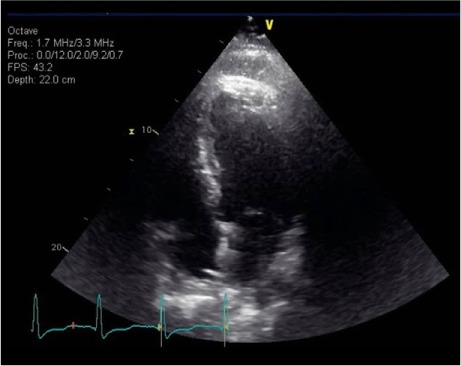
Echocardiogram shows severe biventricular hypokinesis 12 hours after the initiation of extracorporeal membrane oxygenation.
Supplemental motion image is available for Figure 4 (3.3MB, mp4) .
ECMO Day 1. Three hours after cannulation for ECMO, distal malperfusion in the left lower extremity was detected. An antegrade 5F sheath was placed in the left common femoral artery via cutdown, but ischemia persisted.
ECMO Days 2–4. Over the ensuing 48 hours, the patient remained on full ECMO and IABP support, and vasopressors were discontinued as he improved hemodynamically. By hospital day 4, cardiac function, evaluated by means of serial transthoracic echocardiography, showed gradual improvement, and right ventricular (RV) and LV function normalized (LVEF, 0.55–0.60). On day 4, the IABP was removed and an ECMO weaning trial was initiated by gradually reducing ECMO flow under echocardiographic guidance.
ECMO Day 5. The patient manifested normal RV and LV systolic function (LVEF, 0.55–0.60) in the absence of hemodynamic support (Fig. 5). His vital signs were stable (HR, 93 beats/min; BP, 136/65 mmHg; and pH, 7.4), and he was decannulated and extubated.
Fig. 5.
Echocardiogram shows normal ventricular function on day 5 after discontinuation of extracorporeal membrane oxygenation.
Supplemental motion image is available for Figure 5 (3.3MB, mp4) .
Continuation of Care. The patient ultimately needed a left above-the-knee amputation on the 12th day of admission. He recovered uneventfully and was discharged on the 17th day to a rehabilitation center in stable cardiac condition, without symptoms of heart failure.
At the 8-month follow-up examination, repeat echocardiograms showed preserved LVEF (0.55–0.60) and normal cardiac function. Although the amputation healed well, the patient was unable to use a prosthesis because of severe pain in the perineal region from the rectal tumor. He underwent a radical excision of the tumor in January 2015 and was expected to recover fully.
Discussion
A pyrimidine analog antimetabolite that interferes with DNA and RNA synthesis to inhibit cellular growth, 5-FU is used in the treatment of various solid tumors, including breast, anal, and colorectal cancer.1,2 We show that prompt recognition of cardiogenic shock from fulminant myocarditis secondary to 5-FU cardiotoxicity—followed by the initiation of ECMO on an emergency basis—can provide adequate tissue perfusion and thereby an opportunity for myocardial recovery after discontinuation of 5-FU.
Cardiovascular abnormalities secondary to 5-FU treatment, such as myocardial ischemia and heart failure, have been reported.2,5 The exact mechanism is currently unclear, but the authors of a systematic review5 have proposed multifactorial underlying causes, including endothelium-dependent and -independent pathways, direct myocardial damage from cytotoxic effects, induction of apoptosis, rheological side effects, and the production, during drug storage, of cardiotoxic metabolite precursors (for example, fluoroacetate).6–12 Animal models of 5-FU cardiotoxicity have manifested apoptosis of myocytes, endothelial cells, or both, which gives rise to clinical presentations similar to that of myocarditis.12
The toxicity of 5-FU is dependent on the duration of treatment, on the rate of administration, or both; continuous infusions have higher incidences than do bolus regimens.13,14 Pre-existing cardiac disorders are risk factors for future 5-FU cardiotoxicity.15 A multicenter prospective study, designed to identify risk factors for the development of 5-FU–related cardiotoxicity among patients receiving continuous infusions of 5-FU, found that 3% of patients who received the first course of 5-FU chemotherapy presented with symptoms of acute decompensated heart failure.16
In the case described here, underlying (and undiagnosed) coronary artery disease and continuous infusion of 5-FU accentuated our patient's risk of cardiotoxicity. Although this current case lacks histopathologic evidence, numerous other factors are consistent with a clinical diagnosis of fulminant myocarditis: acuity of presentation in an otherwise heart-healthy individual; clinical manifestation of chest pain, coupled with diffuse ST-segment elevations on ECG; moderate troponin-level elevations despite hours of sustained chest pain; severe global hypokinesis; rapid progression to cardiogenic shock; and complete recovery of myocardial function after discontinuation of 5-FU.
Further, the patient was treated with a combined regimen of 5-FU and mitomycin-C. The role of mitomycin as a drug capable of cardiotoxicity has been reported; the odds are highest when the drug is used in high doses, or after a median of 3 dose cycles, or when administered to a patient with a history of doxorubicin therapy.15 None of these situations pertained to our patient. A relationship between mitomycin and myocarditis, independent or in combination with 5-FU, has been observed, but rarely.
Fulminant myocarditis is a life-threatening medical emergency, with a mortality rate of 25% to 39%.17,18 However, patients who survive the acute phase of fulminant myocarditis are more likely to recover fully than are those who experience nonfulminant acute myocarditis.19–21
The Need for ECMO. The prominence of circulatory support techniques in successfully treating patients with fulminant myocarditis has been investigated.18,21,22 In a retrospective analysis of 105 patients treated with percutaneous cardiopulmonary support, Shirakabe and colleagues23 noted that early recognition of the indication for ECMO was one of the important predictors of reduced morbidity and mortality rates, especially in patients with fulminant myocarditis. In our patient, prompt recognition of cardiogenic shock secondary to fulminant myocarditis led to the following events: the immediate initiation of ECMO, adequate tissue perfusion, myocardial recovery, and (ultimately) the survival of the patient.
Although myocarditis has been reported as an adverse effect of 5-FU toxicity, the topic has not been sufficiently studied to establish the rates of incidence and mortality.3,4,24 The case presented here is perhaps the first to show clinical evidence of an association between 5-FU–induced fulminant myocarditis and successful resolution of that condition with immediate ECMO support.
Conclusion
This case shows that full myocardial recovery is possible in patients who present with cardiogenic shock from fulminant myocarditis induced by 5-FU cardiotoxicity. One must recognize the causal association promptly and maintain adequate tissue perfusion and oxygenation. We propose that ECMO be considered in such patients with life-threatening, but temporary, cardiac dysfunction.
Supplementary Material
Acknowledgments
In the preparation of this case report, we acknowledge the contributions of 2 esteemed colleagues. Christopher J. Carrubba, MD, resident physician of Internal Medicine at the University of Colorado (Aurora, Colorado), contributed to the assembly and evaluation of case data, to the discovery and evaluation of prior reports, to research on the current topic, and to preparation of the manuscript. Mitesh Solanki, MD, Internal Medicine hospitalist at Sound Physician Services (Louisville, Kentucky), contributed to the assembly and evaluation of case data and to critical revision of important intellectual content.
Footnotes
From: Division of Cardiovascular Medicine (Drs. Amraotkar, DeFilippis, and Pachika) and Department of Cardiovascular and Thoracic Surgery (Dr. Grubb), University of Louisville; and Rudd Heart & Lung Center (Drs. DeFilippis and Grubb), KentuckyOne Health Jewish Hospital; Louisville, KY 40202
References
- 1.Longley DB, Harkin DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3(5):330–8. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- 2.Sorrentino MF, Kim J, Foderaro AE, Truesdell AG. 5-fluorouracil induced cardiotoxicity: review of the literature. Cardiol J. 2012;19(5):453–8. doi: 10.5603/cj.2012.0084. [DOI] [PubMed] [Google Scholar]
- 3.Calik AN, Celiker E, Velibey Y, Cagdas M, Guzelburc O. Initial dose effect of 5-fluorouracil: rapidly improving severe, acute toxic myopericarditis. Am J Emerg Med. 2012;30(1):257.e1–3. doi: 10.1016/j.ajem.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 4.Sasson Z, Morgan CD, Wang B, Thomas G, MacKenzie B, Platts ME. 5-Fluorouracil related toxic myocarditis: case reports and pathological confirmation. Can J Cardiol. 1994;10(8):861–4. [PubMed] [Google Scholar]
- 5.Polk A, Vaage-Nilsen M, Vistisen K, Nielsen DL. Cardiotoxicity in cancer patients treated with 5-fluorouracil or capecitabine: a systematic review of incidence, manifestations and predisposing factors. Cancer Treat Rev. 2013;39(8):974–84. doi: 10.1016/j.ctrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Baerlocher GM, Beer JH, Owen GR, Meiselman HJ, Reinhart WH. The anti-neoplastic drug 5-fluorouracil produces echinocytosis and affects blood rheology. Br J Haematol. 1997;99(2):426–32. doi: 10.1046/j.1365-2141.1997.4003212.x. [DOI] [PubMed] [Google Scholar]
- 7.Cwikiel M, Eskilsson J, Wieslander JB, Stjernquist U, Albertsson M. The appearance of endothelium in small arteries after treatment with 5-fluorouracil. An electron microscopic study of late effects in rabbits. Scanning Microsc. 1996;10(3):805–19. [PubMed] [Google Scholar]
- 8.Lamberti M, Porto S, Marra M, Zappavigna S, Grimaldi A, Feola D et al. 5-Fluorouracil induces apoptosis in rat cardiocytes through intracellular oxidative stress. J Exp Clin Cancer Res. 2012;31:60. doi: 10.1186/1756-9966-31-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsubara I, Kamiya J, Imai S. Cardiotoxic effects of 5-fluorouracil in the guinea pig. Jpn J Pharmacol. 1980;30(6):871–9. doi: 10.1254/jjp.30.871. [DOI] [PubMed] [Google Scholar]
- 10.Mosseri M, Fingert HJ, Varticovski L, Chokshi S, Isner JM. In vitro evidence that myocardial ischemia resulting from 5-fluorouracil chemotherapy is due to protein kinase C-mediated vasoconstriction of vascular smooth muscle. Cancer Res. 1993;53(13):3028–33. [PubMed] [Google Scholar]
- 11.Polk A, Vistisen K, Vaage-Nilsen M, Nielsen DL. A systematic review of the pathophysiology of 5-fluorouracil-induced cardiotoxicity. BMC Pharmacol Toxicol. 2014;15:47. doi: 10.1186/2050-6511-15-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsibiribi P, Bui-Xuan C, Bui-Xuan B, Lombard-Bohas C, Duperret S, Belkhiria M et al. Cardiac lesions induced by 5-fluorouracil in the rabbit. Hum Exp Toxicol. 2006;25(6):305–9. doi: 10.1191/0960327106ht628oa. [DOI] [PubMed] [Google Scholar]
- 13.Kosmas C, Kallistratos MS, Kopterides P, Syrios J, Skopelitis H, Mylonakis N et al. Cardiotoxicity of fluoropyrimidines in different schedules of administration: a prospective study. J Cancer Res Clin Oncol. 2008;134(1):75–82. doi: 10.1007/s00432-007-0250-9. [DOI] [PubMed] [Google Scholar]
- 14.National Institutes of Health. Fluorouracil (systemic) drug label information. Available from: http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e0794add-67a7-4308-93e9-f889472716cc [updated 2015 Dec 9]
- 15.Pai VB, Nahata MC. Cardiotoxicity of chemotherapeutic agents: incidence, treatment and prevention. Drug Saf. 2000;22(4):263–302. doi: 10.2165/00002018-200022040-00002. [DOI] [PubMed] [Google Scholar]
- 16.Meyer CC, Calis KA, Burke LB, Walawander CA, Grasela TH. Symptomatic cardiotoxicity associated with 5-fluorouracil. Pharmacotherapy. 1997;17(4):729–36. [PubMed] [Google Scholar]
- 17.Hsu KH, Chi NH, Yu HY, Wang CH, Huang SC, Wang SS et al. Extracorporeal membranous oxygenation support for acute fulminant myocarditis: analysis of a single center's experience. Eur J Cardiothorac Surg. 2011;40(3):682–8. doi: 10.1016/j.ejcts.2010.12.050. [DOI] [PubMed] [Google Scholar]
- 18.Lieberman EB, Hutchins GM, Herskowitz A, Rose NR, Baughman KL. Clinicopathologic description of myocarditis. J Am Coll Cardiol. 1991;18(7):1617–26. doi: 10.1016/0735-1097(91)90493-s. [DOI] [PubMed] [Google Scholar]
- 19.Acker MA. Mechanical circulatory support for patients with acute-fulminant myocarditis. Ann Thorac Surg. 2001;71(3 Suppl):S73–6. doi: 10.1016/s0003-4975(00)02628-x. [DOI] [PubMed] [Google Scholar]
- 20.Gupta S, Markham DW, Drazner MH, Mammen PP. Fulminant myocarditis. Nat Clin Pract Cardiovasc Med. 2008;5(11):693–706. doi: 10.1038/ncpcardio1331. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy RE, 3rd, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Hare JM, Baughman KL. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med. 2000;342(10):690–5. doi: 10.1056/NEJM200003093421003. [DOI] [PubMed] [Google Scholar]
- 22.Yasu T, Murata S, Katsuki T, Fujii M, Kubo N, Ohmura N et al. Acutely severe myocarditis successfully treated by percutaneous cardiopulmonary support applied by a newly developed heparin-binding oxygenator and circuits. Jpn Circ J. 1997;61(12):1037–42. doi: 10.1253/jcj.61.1037. [DOI] [PubMed] [Google Scholar]
- 23.Shirakabe A, Nozaki A, Hata N, Kobayashi N, Shinada T, Tomita K et al. Predictive score for survival after percutaneous cardiopulmonary support in cardiovascular disease patients--evaluation of pre-procedural information. Circ J. 2013;77(8):2064–72. doi: 10.1253/circj.cj-12-1326. [DOI] [PubMed] [Google Scholar]
- 24.Dalzell JR, Samuel LM. The spectrum of 5-fluorouracil cardiotoxicity. Anticancer Drugs. 2009;20(1):79–80. doi: 10.1097/cad.0b013e3283165f27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


