Abstract
Malignant cardiac tumors typically have a grave prognosis; their resection with negative margins is optimal. We present the case of a 21-year-old woman in whom we surgically resected a primary cardiac sarcoma and reconstructed the right atrium with use of a porcine urinary bladder membrane—the MatriStem® Surgical Matrix PSMX. The patient recovered uneventfully. Six months postoperatively, the right atrial wall had retained its integrity. In addition to our patient's case, we discuss the benefits of using the MatriStem membrane in cardiac reconstruction.
Keywords: Biocompatible materials, cardiac surgical procedures, extracellular matrix/transplantation, heart neoplasms/surgery, sarcoma/surgery, tissue scaffolds, treatment outcome, urinary bladder
Optimally, cardiac tumors should be resected with negative margins. For primary cardiac sarcoma, this can entail large resections and subsequent heart reconstruction to restore normal blood-flow dynamics and physiology. We present the case of a young woman who underwent the surgical removal of a primary right cardiac sarcoma. We reconstructed the heart with use of an acellular extracellular-matrix membrane derived from porcine urinary bladder—the MatriStem® Surgical Matrix PSMX membrane (ACell®, Inc.; Columbia, Md)—the potential benefits of which we also discuss.
Case Report
In November 2011, a 21-year-old woman was admitted to a hospital because of chest pain. Investigation for pulmonary emboli was negative; the diagnosis was musculoskeletal pain. A month later, she presented at a different hospital with pericardial and pleural effusions. Pericardiocentesis and thoracentesis yielded no malignant cells. Echocardiograms showed a left ventricular ejection fraction of 0.30. Because of possible viral pericarditis, the patient was started on carvedilol, digoxin, and spironolactone.
Three months later, the patient presented with recurrent pericardial effusion and chest pain. She again underwent pericardiocentesis, and echocardiograms showed an irregular mediastinal mass without tricuspid valve dysfunction. Cardiac magnetic resonance images revealed a large right atrial mass that extended to the atrioventricular groove and was consistent with a malignant tumor (Fig. 1). After she underwent a median sternotomy to evacuate the bloody pericardial effusion, a biopsy specimen was positive for sarcoma.
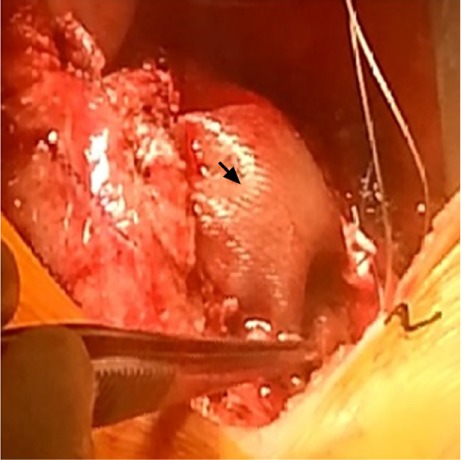
Fig. 1.

Cardiac magnetic resonance image shows a sessile mass (arrow) along the posteromedial aspect of the right atrium, extending anteriorly to the atrioventricular groove.
The patient was referred to MD Anderson Cancer Center, where metastases to her bones and lungs were diagnosed. She completed 12 cycles of adriamycin and ifosfamide chemotherapy, with good response. She was then started on paclitaxel and was referred to our surgical center in September 2013. The metastases to her bones and lungs were completely gone, and her cardiac tumor had shrunk. It was decided to resect the right atrial mass, in accordance with Institutional Review Board-approved protocol and the patient's consent.
Surgical Technique
The patient's previous sternal incision was opened, the sternal wires were removed, and the adhesions were dissected. The venae cavae were directly cannulated, and the displaced aorta was cannulated in standard fashion. After cardiopulmonary bypass (CPB) was started and the caval tapes were snared, the right atrium was opened. The tumor encompassed the entire right atrium from the superior vena cava down to the septum.
The tumor (including the area from the inferior vena cava up to the tricuspid annulus) was removed, along with the right atrial appendage and approximately a 5 × 5-cm section of the lateral right atrial wall. On gross inspection and frozen section, the margins were free of tumor.
To reconstruct the lateral right atrial wall, we sewed a MatriStem Surgical Matrix PSMX patch to the right atrium with a running 4-0 Prolene suture (Fig. 2). The patient was weaned from CPB and the sternum was closed. She recovered uneventfully and was discharged from the hospital after a total stay of 7 days. Six months postoperatively, a computed tomogram showed no patch deterioration, enlargement, or shrinkage; no loss of atrial-wall integrity; and no tumor recurrence (Fig. 3). As of January 2016, the patient continued to undergo monitoring at our hospital and the cancer center.
Fig. 2.
Intraoperative photograph after reconstruction shows the acellular MatriStem Surgical Matrix PSMX patch (arrow) used to reconstruct the lateral right atrial wall.
Fig. 3.
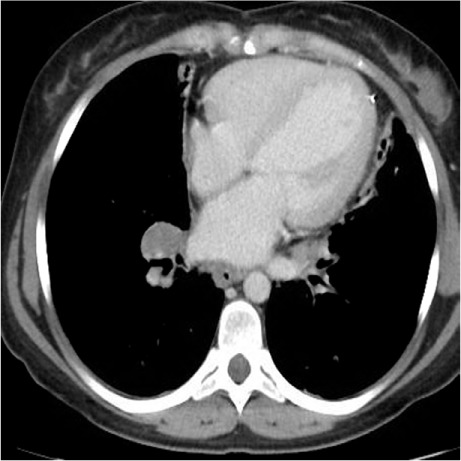
Six months postoperatively, a computed tomogram shows no patch deterioration or lost integrity of the atrial wall.
Discussion
To our knowledge, this is the first reported cardiac sarcoma resection involving extensive right atrial reconstruction with use of the MatriStem acellular porcine urinary bladder membrane. Whereas we have typically reconstructed atrial tissue with the use of bovine pericardial patches,1,2 we have begun using the MatriStem membrane because of its potential benefits in the remodeling of cardiac tissue: porcine urinary bladders and other extracellular-matrix scaffolds have been shown to promote tissue growth while providing strong structural support.3–5 We also have used the MatriStem because its basement membrane might lead to more durable, lasting atrial reconstruction. We encountered no technical difficulty when sewing the patch to our patient's native atrial tissue, and we noted that the patch was hemostatic during protamine administration after CPB.
Our early results have been encouraging. As we continue to use the MatriStem in heart-reconstruction procedures, we intend to perform semiannual imaging studies in this patient for up to 2 years, in order to evaluate the membrane's long-term integrity.
Footnotes
From: Department of Cardiovascular Surgery (Drs. Abu Saleh, Al Jabbari, Ramlawi, and Reardon) and Division of Transplant Surgery and Assist Devices (Drs. Bruckner and Loebe), Houston Methodist De-Bakey Heart & Vascular Center, Houston Methodist Hospital, Houston, Texas 77030
References
- 1.Kim MP, Correa AM, Blackmon S, Quiroga-Garza G, Weilbaecher D, Bruckner B et al. Outcomes after right-side heart sarcoma resection. Ann Thorac Surg. 2011;91(3):770–6. doi: 10.1016/j.athoracsur.2010.09.079. [DOI] [PubMed] [Google Scholar]
- 2.Ramlawi B, Al-Jabbari O, Blau LN, Davies MG, Bruckner BA, Blackmon SH et al. Autotransplantation for the resection of complex left heart tumors. Ann Thorac Surg. 2014;98(3):863–8. doi: 10.1016/j.athoracsur.2014.04.125. [DOI] [PubMed] [Google Scholar]
- 3.Liu L, Deng L, Wang Y, Ge L, Chen Y, Liang Z. Porcine urinary bladder matrix-polypropylene mesh: a novel scaffold material reduces immunorejection in rat pelvic surgery. Int Urogynecol J. 2012;23(9):1271–8. doi: 10.1007/s00192-012-1745-8. [DOI] [PubMed] [Google Scholar]
- 4.Brown BN, Chung WL, Almarza AJ, Pavlick MD, Reppas SN, Ochs MW et al. Inductive, scaffold-based, regenerative medicine approach to reconstruction of the temporomandibular joint disk. J Oral Maxillofac Surg. 2012;70(11):2656–68. doi: 10.1016/j.joms.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brouwer KM, Wijnen RM, Reijnen D, Hafmans TG, Daamen WF, van Kuppevelt TH. Heparinized collagen scaffolds with and without growth factors for the repair of diaphragmatic hernia: construction and in vivo evaluation. Organogenesis. 2013;9(3):161–7. doi: 10.4161/org.25587. [DOI] [PMC free article] [PubMed] [Google Scholar]


