Abstract
Purpose:
To compare intraocular pressure (IOP) measurements by rebound tonometry (Icare PRO; Icare Finland Oy, Helsinki, Finland) to measurements by indentation tonometry (Pneumotonometer Model 30 classic and Tono-Pen XL; Reichert, Buffalo, NY, USA) in supine sedated children with glaucoma.
Methods:
Prospective comparative observational study of Saudi Arabian children with glaucoma undergoing chloral hydrate sedation for ophthalmic examination (February 2012 - February 2013). Nonglaucomatous eyes were included as controls. Eyes with corneal scars or prior corneal transplant or lamellar surgery were excluded.
Results:
Fifty-two eyes (26 OD, 26 OS) of 28 children were included. Thirty-six eyes had glaucoma (32 primary congenital glaucoma, two Sturge-Weber related, and two aphakia related). Sixteen eyes did not have glaucoma (six with pediatric cataract, five normal eyes, two strabismic eyes, two eyes with simple megalocornea, and one eye had peripheral corneal laceration repair. In the glaucoma group, the mean IOP was 17.55 ± 5.97 mmHg (range, 8-31.5 mmHg) with the Icare PRO and 20 ± 6.4 mmHg (range, 8-35.5 mmHg) with the Pneumotonometer from 20.47 ± 6.81 mmHg (range, 10-43 mmHg) with the Tono-Pen XL. The Icare PRO readings were significantly lower than each of the indentation tonometers. For the control group, there was no statistically significant difference in IOP measured by the Icare PRO and the indentation tonometers.
Conclusions:
In this population of supine sedated children with glaucoma, IOP measurements with the Icare PRO tend to be lower than readings from the Pneumotonometer and Tono-Pen XL.
Keywords: Chloral hydrate, Indentation tonometry, Pediatric glaucoma, Rebound tonometry
INTRODUCTION
The Icare (Icare Finland Oy, Helsinki, Finland) is a hand-held tonometer with a magnetic solenoid probe that very briefly rebounds off the cornea, does not require topical anesthesia, and is the only commercially available clinical tonometer that uses the impact rebound principle.1 It is often easier to use than other tonometers in children who are awake.2,3,4,5 The Icare has good repeatability and measurements correlates well to other tonometers.2,3,4,5
In some cases, young children require sedation for ophthalmic examination and intraocular pressure (IOP) measurement has to be performed when the patient is supine. Sedation can be used more often for young children with glaucoma. The Icare PRO allows measurement of IOP measurement in either the sitting or supine position. Some studies that compare the Icare PRO to other tonometers in supine children suggest Icare measurements tend to be slightly higher or the same as other tonometers.6,7,8 However, these studies are rare and have typically evaluated data from a Western population.6,7,8 The purpose of this study is to compare IOP measurements with Icare PRO to measurements by two applanation devices (the Tono-Pen XL and Pneumotonometer Model 30 classic; both by Reichert, Buffalo, NY, USA) in supine children with glaucoma.
METHODS
Institutional review board approval was granted for this prospective comparative observational series conducted from February 2012 to February 2013 at the King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia. The study included children aged ≤5 years with or without glaucoma who were already undergoing chloral hydrate sedation for ophthalmic examination purposes.
A single investigator (FTA) evaluated patients presenting to the sedation clinic for potential participation in the study, and parental informed consent was granted for children who entered the study. After conscious sedation (approximately 20 min after a dose of 50 mg/kg of oral chloral hydrate was given), the same investigator instilled a drop of topical anesthetic (oxybuprocaine hydrochloride 0.4%) and measured IOP with the three devices. Chloral hydrate does not appreciably affect IOP and there is no appreciable effect of topical anesthetic on Icare IOP measurements.9,10 The following sequence was used for each sedated supine child: Icare PRO, Pneumotonometer, and Tono-Pen XL, with an interval of 2-3 min between each instrument. For the Pneumotonometer and Tono-Pen XL, a single reading was taken for each instrument unless the standard error was >5%, in which case the measurement was repeated to achieve a standard error of ≤5%.
Data were analyzed using SPSS version 19.0 (IBM Corp., Armonk, NY, USA). Continuous variables were analyzed as mean ± standard deviation and categorical variables as frequency (percentage). The correlations between the Icare PRO and other tonometers were calculated using the Spearman correlation coefficient as the measurements were not normally distributed. Agreement between the measurements by Icare PRO and each applanation tonometer was plotted using the Bland-Altman method using Excel 201011 (Microsoft Corp., Redmond, WA, USA). Icare IOP measurement differences with the second device (Icare versus Pneumotonometer and Icare vs. Tono-Pen) were normally distributed and thus assessed by the paired two-tailed t-test with a level of significance of <5%.
RESULTS
Fifty-two eyes (26 OD, 26 OS) of 28 ethnic Saudi Arabian children were included. Thirty-six eyes of 19 children (2-48 months old, mean 26.9; five boys, 14 girls) had glaucoma (glaucoma group; 32 with primary congenital glaucoma, two with Sturge-Weber syndrome related glaucoma, and two with aphakic glaucoma). Sixteen eyes of nine children (10-16 months old, mean 26.2; three boys, six girls) did not have glaucoma (control group; six eyes with pediatric cataract, five normal eyes, two eyes with strabismus, two eyes with simple megalocornea, and one eye which had had peripheral corneal laceration repair).
Glaucoma group
For the 36 eyes in the glaucoma group, the mean IOP was 17.6 ± 6.0 mmHg (range, 8-31.5 mmHg) with the Icare PRO and 20 ± 6.4 mmHg (range, 8-35.5 mmHg) with the Pneumotonometer. The Pneumotonometer measured statistically significantly higher IOP values than the Icare PRO by 2.45 ± 3.9 mmHg (P = 0.0006, 95% confidence interval (CI): 1.13-3.78). The mean IOP with the Tono-Pen XL was 20.5 ± 6.8 mmHg (range, 10-43 mmHg). The Tono-Pen XL measured statistically significantly higher IOP values than the Icare PRO by 2.9 ± 3.6 mmHg (P = 0.00003, 95% CI 1.70-4.15). Bland-Altman plots of the agreement between the Icare PRO and Pneumotonometer and between the Icare PRO and the Tono-Pen XL are presented in Figures 1 and 2. The Icare PRO correlated positively with the Pneumotonometer (Spearman coefficient 0.80, P < 0.001) and the Tono-Pen XL (Spearman coefficient 0.85, P < 0.001). Linear plots of Icare PRO and each applanation tonometer are presented in Figures 3 and 4.
Figure 1.
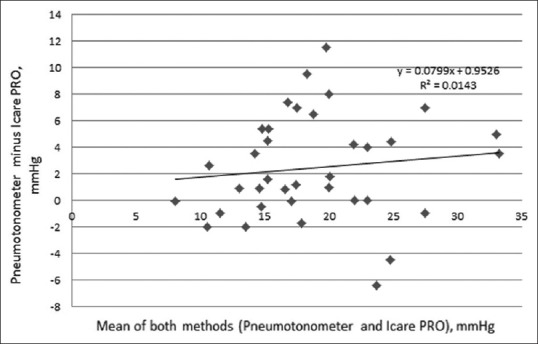
(Bland-Altman plot, Icare PRO and Pneumotonometer): The Bland-Altman plot confirms a tendency for Icare PRO values to measure lower than Pneumotonomer values
Figure 2.
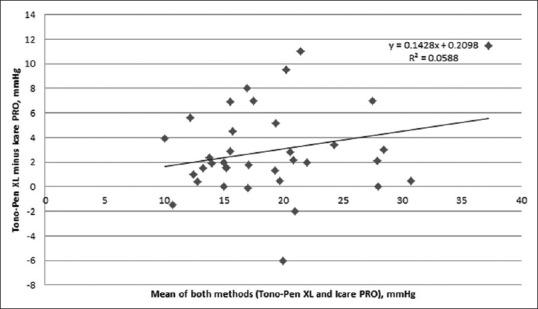
(Bland-Altman plot, Icare PRO and Tono-Pen XL): The Bland-Altman plot confirms a tendency for Icare PRO values to measure lower than Tono-Pen XL values
Figure 3.
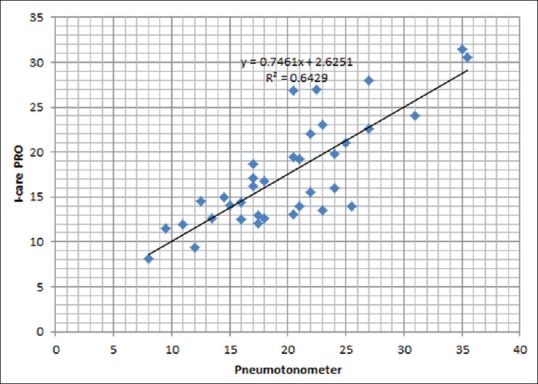
(Linear plot, Icare PRO and Pneumotonometer): The positive linear correlation between Icare PRO and Pneumotonometer values is shown. Spearman coefficient was 0.80, P < 0.001
Figure 4.
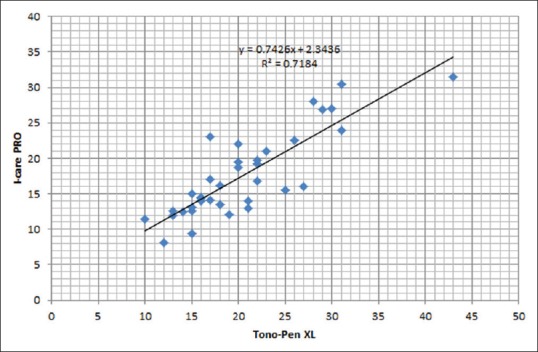
(Linear plot, Icare PRO and Tono-Pen XL): The positive linear correlation between Icare PRO and Tono-Pen XL values is shown. Spearman coefficient was 0.85, P < 0.001
Control group
In the control group, the mean IOP was 13.54 ± 3.07 mmHg (range, 8-19.7 mmHg) with the Icare PRO, 15.25 ± 3.3 mmHg (range, 10-21.5 mmHg) with the Pneumotonometer and 14.6 ± 3.3 mmHg (range, 10-21 mmHg) with the Tono-Pen XL. The Pneumotonometer measured a mean 1.7 ± 3.15 mmHg (median [Q1, Q3] = 0.75 [−0.85, 4.57]) higher than the Icare PRO (P = 0.05, 95% CI: 0.03-3.39). The Tono-Pen XL measured a mean 1.1 ± 2.85 mmHg (median [Q1, Q3] = 1.75 [−2.02, 3.62]) higher than the Icare PRO (P = 0.15, 95% CI: −0.44-2.59). The IOP values from the Icare PRO positively correlated with the Pneumotonometer measurements (Spearman coefficient 0.65, P < 0.05) and the Tono-Pen XL measurements (Spearman coefficient 0.620, P < 0.05).
DISCUSSION
In our cohort of sedated supine children with glaucoma, the Icare PRO IOP measurements tended to be statistically significantly lower than the measurements from the two applanation tonometers and were positively correlated with both devices (P < 0.05, all comparisons). The control group had a smaller sample size and had no statistically significant differences in IOP values between the Icare PRO and either applanation tonometer.
Our finding of lower IOP readings with the Icare PRO contrasts with results from some previous studies in children,6,7,8 which have reported a tendency for similar or higher measurements with the Icare PRO. Higher IOP measurements with the Icare PRO compared to applanation tonometry have also been reported for supine adults.12,13 Li et al.6 reported Icare PRO readings were slightly higher than readings from a hand-held Goldmann tonometer in supine children (chloral hydrate sedation). Borrego Sanz et al.7 also found slightly higher readings with the Icare PRO than with a hand-held Goldmann tonometer in children with primary congenital glaucoma who were supine (general anesthesia). However, a recent study of cooperative supine children, most of whom had glaucoma, Dosunmu et al.8 found no significant difference between the Icare PRO measurement and the Tono-Pen. Both devices showed a slightly higher IOP measurement when the child was supine versus sitting.
There are different potential explanations for our observation of the lower measurements with the Icare PRO than with the applanation tonometers when the patients were supine. Corneal variables such as resistance and hysteresis (related to but not absolutely correlated to pachymetry) influence IOP measurements to different extents with different devices.14 In our cohort of Arabian pediatric glaucoma patients, these values may have been unusual or idiosyncratic, particularly because most were primary congenital glaucoma patients, 92% of whom are expected to harbor recessive mutations in CYP1B1, unlike cohorts from previous studies evaluated with the Icare PRO.15 Unfortunately, we were not able to measure these values and thus cannot confirm this possibility. Another factor that potentially influenced our results is the possibility that there were different measured gradients of change in IOP from a sitting to supine position among the different instruments in our cohort with a lower gradient for the Icare PRO. It is generally accepted that IOP increases in the supine versus the sitting position.16 Hence, if this gradient of change measured lower with the Icare PRO compared to the applanation tonometers, the IOP would be lower with the Icare PRO. A comparison of the measured change in IOP from the sitting to the supine for each patient with the different tonometers could have evaluated this possibility in our cohort. However, the children in this study were undergoing sedated because a necessary ophthalmic examination could not be performed while they were awake; thus, it was not possible to measure their IOPs with the three devices while they were awake.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowlegement
The authors thank Nasira Asghar of the King Khaled Eye Specialist Hospital for her assistance with statistical analysis.
REFERENCES
- 1.Kontiola A. A new electromechanical method for measuring intraocular pressure. Doc Ophthalmol. 1996;93:265–76. doi: 10.1007/BF02569066. [DOI] [PubMed] [Google Scholar]
- 2.Sahin A, Basmak H, Niyaz L, Yildirim N. Reproducibility and tolerability of the ICare rebound tonometer in school children. J Glaucoma. 2007;16:185–8. doi: 10.1097/IJG.0b013e31802fc6bc. [DOI] [PubMed] [Google Scholar]
- 3.Flemmons MS, Hsiao YC, Dzau J, Asrani S, Jones S, Freedman SF. Icare rebound tonometry in children with known and suspected glaucoma. J AAPOS. 2011;15:153–7. doi: 10.1016/j.jaapos.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 4.Gandhi NG, Prakalapakorn SG, El-Dairi MA, Jones SK, Freedman SF. Icare ONE rebound versus Goldmann applanation tonometry in children with known or suspected glaucoma. Am J Ophthalmol. 2012;154:843–9.e1. doi: 10.1016/j.ajo.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Grigorian F, Grigorian AP, Olitsky SE. The use of the iCare tonometer reduced the need for anesthesia to measure intraocular pressure in children. J AAPOS. 2012;16:508–10. doi: 10.1016/j.jaapos.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Tang L, Xiao M, Jia S, Liu P, Zhou Y, et al. Comparison of the Icare tonometer and the hand-held Goldmann applanation tonometer in pediatric aphakia. J Glaucoma. 2013;22:550–4. doi: 10.1097/IJG.0b013e31825afc87. [DOI] [PubMed] [Google Scholar]
- 7.Borrego Sanz L, Morales-Fernandez L, Martínez de-la-Casa JM, Sáenz-Francés F, Fuentes M, García-Feijóo J. The Icare-Pro rebound tonometer versus the hand-held applanation tonometer in congenital glaucoma. J Glaucoma. 2016;25(2):149–54. doi: 10.1097/IJG.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 8.Dosunmu EO, Marcus I, Tung I, Thiamthat W, Freedman SF. Intraocular pressure in children: The effect of body position as assessed by Icare and Tono-Pen tonometers. Am J Ophthalmol. 2014;158:1348–52.e1. doi: 10.1016/j.ajo.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Jaafar MS, Kazi GA. Effect of oral chloral hydrate sedation on the intraocular pressure measurement. J Pediatr Ophthalmol Strabismus. 1993;30:372–6. doi: 10.3928/0191-3913-19931101-07. [DOI] [PubMed] [Google Scholar]
- 10.Dosunmu EO, Marcus I, Tung I, Thiamthat W, Freedman SF. The effect of repeated measurements and the use of topical anesthetic on rebound tonometry values in children. J AAPOS. 2014;18:619–21. doi: 10.1016/j.jaapos.2014.07.167. [DOI] [PubMed] [Google Scholar]
- 11.Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb) 2015;25:141–51. doi: 10.11613/BM.2015.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakakura S, Mori E, Yamamoto M, Tsushima Y, Tabuchi H, Kiuchi Y. Intraocular pressure of supine patients using four portable tonometers. Optom Vis Sci. 2013;90:700–6. doi: 10.1097/OPX.0b013e3182972df4. [DOI] [PubMed] [Google Scholar]
- 13.Lee TE, Yoo C, Hwang JY, Lin S, Kim YY. Comparison of intraocular pressure measurements between Icare Pro Rebound Tonometer and Tono-Pen XL Tonometer in supine and lateral decubitus body positions. Curr Eye Res. 2015;40:923–9. doi: 10.3109/02713683.2014.964416. [DOI] [PubMed] [Google Scholar]
- 14.Chui WS, Lam A, Chen D, Chiu R. The influence of corneal properties on rebound tonometry. Ophthalmology. 2008;115:80–4. doi: 10.1016/j.ophtha.2007.03.061. [DOI] [PubMed] [Google Scholar]
- 15.Khan AO. Genetics of primary glaucoma. Curr Opin Ophthalmol. 2011;22:347–55. doi: 10.1097/ICU.0b013e32834922d2. [DOI] [PubMed] [Google Scholar]
- 16.Lee TE, Yoo C, Kim YY. Effects of different sleeping postures on intraocular pressure and ocular perfusion pressure in healthy young subjects. Ophthalmology. 2013;120:1565–70. doi: 10.1016/j.ophtha.2013.01.011. [DOI] [PubMed] [Google Scholar]


