Abstract
Purpose:
To evaluate the postoperative visual outcomes and complications of posterior iris fixated intraocular lens (IFIOL) implantation for pediatric traumatic cataract.
Methods:
A retrospective clinical audit was performed of all the pediatric traumatic cataract patients who underwent lens removal and iris fixated lens implantation due to inadequate capsular support with or without corneal tear repair between January 2009 and December 2013. Data were collected and analyzed on the preoperative and postoperative visual outcomes and complications.
Results:
Twenty-five children (25 eyes; 21 males and 4 females) were enrolled with the mean age of 11 ± 4.0 years. There were 72% of eyes that underwent primary cataract removal with IFIOL implantation. Twenty-eight percent of eyes underwent corneal tear repair prior to intraocular lens (IOL) implantation. Preoperative best corrected visual acuity (BCVA) was hand motion in 32% eyes, counting fingers in 24%, and perception of light in 44%. Postoperative BCVA of 0-0.2 logarithm of minimum angle of resolution was reported in the 64% of eyes. One eye developed secondary glaucoma, one eye underwent re-enclavation, and none developed retinal complications.
Conclusion:
Posterior IFIOL implantation resulted in an improved visual outcome, low incidence of postoperative complications, and is a good alternative to other IOL, in the cases of pediatric traumatic cataract without adequate capsular support.
Keywords: Inadequate Capsular Support, Intraocular Lens, Posterior Iris Fixated, Trauma, Traumatic Cataract
INTRODUCTION
Traumatic cataract may occur in association with an open globe or contusion to the eye. Management remains complex due to difficulties in obtaining accurate keratometry and axial length measurements, timing of surgery, and intraocular lens (IOL) placement in cases with inadequate capsular support. Iris fixated IOL (IFIOL),1 anterior chamber IOL (ACIOL),2 and trans-scleral fixated IOL (SFIOL)3 are the three options for these cases. Posterior IFIOL is considered to be better than SFIOL and ACIOLs in terms of its anatomical position, improved design, easy implantation, better safety, and efficacy with low complications rates.4 This study evaluated the postoperative vision and complications of posterior IFIOL implantation for pediatric traumatic cataract.
MATERIALS AND METHODS
This was a retrospective, observational, clinical audit of the traumatic cases of 25 eyes of the 25 pediatric patients between January 2009 and December 2013 attending the outpatient department who underwent lens removal and IFIOL implantation (due to inadequate capsular support) either as primary or secondary procedure, with or without corneal/corneoscleral tear repair through an anterior approach. All the surgeries were performed by a single surgeon. Informed written consent was obtained from the parents of all the children. The patients were excluded if they had retinal pathologies and cases where a posterior approach with IFIOL implantation would affect the final visual outcome. The study adhered to all the principles of the Declaration of Helsinki 2000.
Data were collected on the nature and duration of the injury, uncorrected visual acuity, and best corrected visual acuity (BCVA) using logarithm of the minimum angle of resolution (LogMAR) charts, intraocular pressure (IOP), and anterior and posterior segment assessment, including B-scan in hazy media. Fellow eye keratometry and axial length readings were used for IOL power calculation in the eyes with corneal tear/status of post tear repair. The iris fixated (claw) was IOL implanted in all cases (Excel optics, Chennai, India, Model No: PIC 5590 or Model No: PIC 5580). This IOL is a modified version of Dr. Worst and Dr. Daljit Singh Model. It can be implanted in either ways as it has no angulations [Figure 1].
Figure 1.
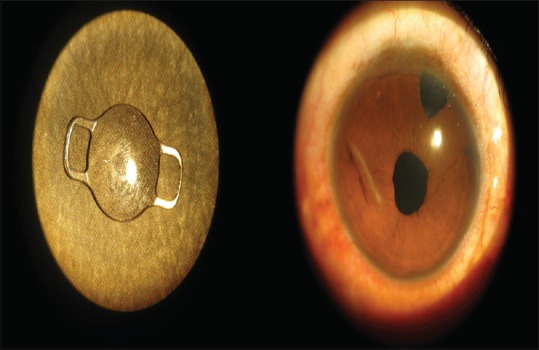
Iris fixated intraocular lens: Overall length of 9 mm or 8 mm, biconvex optic size of 5.5 mm or 5 mm, a constant 117.2: Postoperative round pupil
The IOL power was undercorrected in the anticipation of a myopic shift as the child ages and the eye grows.5 Children <2 years were undercorrected by 20%, between 2 and 5 years by 10%, 5-8 years by 5%, 8-10 years by 2.5%, and children older than 10 years were targeted for emmetropia. All the surgeries were performed under general anesthesia. Corneal/corneoscleral tear was repaired using 10-0 nylon interrupted sutures. Cataract removal and IFIOL implantation were performed as a primary or secondary procedure through a superior 5.5-6 mm scleral tunnel. The anterior capsule was stained with tryphan blue dye. Posterior synechiae, when present, was released. Anterior continuous curvilinear capsulorhexis was performed using a bent 26-gauge needle and Utrata capsule forceps in eyes with intact anterior capsule under sodium hyaluronate (1.4%). In cases with a ruptured anterior capsule, capsulotomy was performed. Lens matter was aspirated using irrigation-aspiration cannula. Closed chamber anterior vitrectomy and superior peripheral iridectomy were performed with automated vitrector in all cases. Two paracentesis at 3 o'clock and 9 o'clock positions were made. IFIOL (claw) was inserted into the anterior chamber with the help of Macpherson forceps. The optic was held with a claw IOL forceps; one haptic (claw) was tilted down (at three o'clock) and gently pushed under the iris. A fine rod (30-gauge) was passed through the paracentesis on the same side, the haptic behind the iris was tilted up to produce an indent on the iris, and the iris tissue was enclaved into the claw with a gentle push of the rod. Similarly, enclavation was performed on the other side (nine o'clock). All patients were treated with steroid antibiotic, homatropine eye drops, and oral steroids for a week. Data were collected on postoperative BCVA, IOP, fundus details, and complications at each follow-up visit.
Statistical analysis
Descriptive and inferential statistical analysis was performed in this study. Results for continuous measurements are presented as mean ± standard deviation (min-max) and results for categorical measurements are presented as a number (%). P <0.05 was considered as statistically significant. Assumptions made during data analysis were: (1) Dependent variables should be normally distributed (2) samples drawn from the population should be random; cases of the samples should be independent. The Student's t-test (two-tailed and dependent) was used to determine the significance of study parameters on a continuous scale within each group.
Statistical analysis was performed with SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment version 2.11. Microsoft Word and Excel (Microsoft Corp., Redmond, WA, USA) were used to generate graphs and tables.
RESULTS
Twenty-five children were enrolled between 4 and 18 years old. The mean age was 11 ± 4.0 years.
Forty-four percent (11/25) of the children were between 6 and 10 years of age, 84% were male and 64% had trauma to the left eye. The most common eye injury was due to trauma from a stick (14 [56%] children). There were 68% of eyes with closed globe injury and the rest had open globe injury. Sixty-eight percent of the children had mature cataract, 20% had absorbed cataract, and 12% children had a subluxated lens. The mean axial length was 22.96 mm ± 0.96 mm and 17 (68%) children had axial length ranging from 22 mm to 24 mm. The mean IOL power was 20.66 D ± 2.61 D; 15 (60%) children had IOL power between 20.5 D and 24 D. Eighteen (72%) children underwent cataract removal with posterior IFIOL implantation (primary procedure) and the remaining seven (28%) children had corneal/corneoscleral tear repair prior to IOL implantation (secondary procedure). One out of seven patients underwent posterior IFIOL implantation as a secondary procedure. Mean postoperative follow-up was 16.44 ± 7.41 months, ranging from 9 months to 36 months. Postoperatively, 20 (80%) children underwent occlusion therapy.
Postoperatively, 21 (84%) children had a normal fundus; one (4%) child had optic atrophy and three (12%) had a myopic fundus. Only one (4%) child had an IOP of 24 mmHg, 1-month postoperatively that was well controlled with timolol maleate 0.5%. Preoperative and postoperative visual acuities are presented in Table 1.
Table 1.
Preoperative and postoperative BCVA
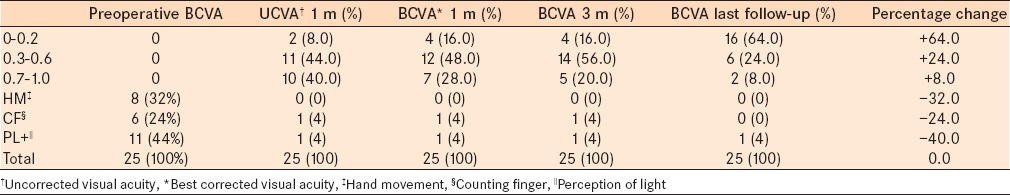
At last postoperative visit, BCVA (0-0.2 logMAR) was better than preoperative in 16 eyes (64%). Postoperatively, no eyes had hand motion or counting fingers vision. One eye (4%) with optic atrophy had perception of light + vision, postoperatively. There was no case of infection/cystoid macular edema (CME)/retinal detachment/dislocation, postoperatively. One eye underwent re-enclavation of one haptic at 1-month for spontaneous disenclavation. One eye had a horizontally oval pupil; the remaining 24 eyes had a round pupil [Figure 1], postoperatively. Pigment dispersion on the lens surface was noted in four eyes (16%) and iris atrophy (at 6 months, postoperatively) at the site of enclavation was noted in one eye (4%) [Figure 2].
Figure 2.
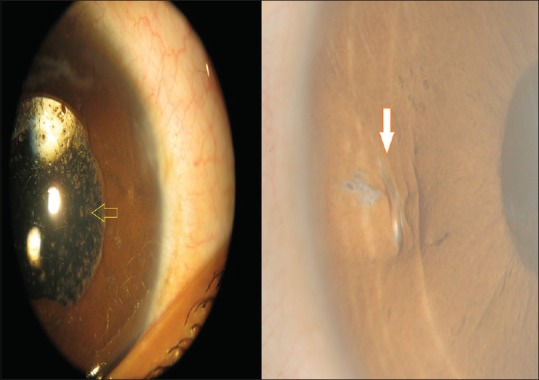
Pigments on the iris fixated intraocular lens; iris atrophy at the enclaved site
DISCUSSION
Trauma is an important cause of monocular blindness. Successful optical rehabilitation in the traumatic cataract cases with no capsular support depends upon the choice of the surgical procedure, experience of the surgeon, and the choice of IOL design.6 Various techniques have been used in the children with ocular trauma, including aphakic spectacles, contact lens, angle-supported ACIOL,7 anterior chamber iris-enclavated IOL,8 posterior-chamber IFIOL,9 posterior-chamber capsule-placed IOL centered with a capsular tension ring,10 or SFIOL.3 IOLs offer the advantages of compliance, minimal aniseikonia, and a predictable refractive result.11 The use of ACIOL is often limited due to complications such as irreversible corneal endothelial loss, corneal decompensation, iris atrophy, iris sphincter erosion, pupil ectopia, and glaucoma. However, SFIOL implantation is a challenging and time-consuming technique. Complications of SFIOL include suture breakage with IOL subluxation, dislocation, endophthalmitis, and retinal detachment.3,12,13 Alternately, IFIOLs, invented by Dr. John Worst and Dr. Daljit Singh, have emerged as safe IOLs, have an improved design, are easy to implant, and offer better safety and efficacy with low dislocation rates compared to other IOLs.4 Posterior IFIOL enclavation is a better option than other IOL implantation techniques due to the decrease in surgical time with minimal complications, greater distance from the endothelium, and the position is similar to the physiological crystalline lens.4,14 We found similar results in our study with minimal complications. Vision improved in all the cases except for one eye that had perception of light + vision. Preoperatively, no eyes had BCVA better than one logMAR. However, at last postoperative visit, 16 of 25 eyes had BCVA between 0 logMAR and 0.2 logMAR, six eyes had 0.3-0.6 logMAR, and two eyes had 0.7-1.0 logMAR. These outcomes suggest a remarkable improvement in the visual acuity, postoperatively, in our study and are similar to Yen et al.'s results.12 Complications of posterior IFIOL implantation in the adults include pupil irregularity, macular edema, transient elevated IOP, and spontaneous IOL dis-enclavation.15 In our study, only one eye had an elevated IOP of 24 mmHg after a month; which may be attributed to preexisting trauma or ocular inflammation. One eye had dis-enclavation at 1-month, iris atrophy and oval pupil, indicating the low incidence of postoperative complications in the current study. None of our patients in our study had CME or retinal detachment. This study is limited by its retrospective, noncomparative nature, lack of endothelial cell analysis, and short term follow-up. Longer term follow-up is required to determine the status of the IOL over time.
The posterior IFIOL implantation was associated with improved visual outcomes with the low incidence of postoperative complications and can be used as an alternative to other IOLs in the children with traumatic cataracts, with inadequate capsular support.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the Management - Sankara Eye Hospital, Staff - Sankara Eye Hospital, Dr. S. Mahesha Bhat, Mr. K. P. Suresh (statistician), Dr. S. P. Somashekhar, and Dr. V. Hariprasad.
REFERENCES
- 1.Lorencová V, Rozsíval P, Urminský J. Clinical results of the aphakia correction by means of secondary implantation of the iris-fixated anterior chamber intraocular lens. Cesk Slov Oftalmol. 2007;63:285–91. [PubMed] [Google Scholar]
- 2.Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31:903–9. doi: 10.1016/j.jcrs.2004.10.061. [DOI] [PubMed] [Google Scholar]
- 3.Asadi R, Kheirkhah A. Long-term results of scleral fixation of posterior chamber intraocular lenses in children. Ophthalmology. 2008;115:67–72. doi: 10.1016/j.ophtha.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 4.Baykara M, Ozcetin H, Yilmaz S, Timuçin OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol. 2007;144:586–91. doi: 10.1016/j.ajo.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 5.Trivedi RH, Wilson ME. IOL power calculation for pediatric cataract. Kerala J Ophthalmol. 2006;18:189–93. [Google Scholar]
- 6.Dakshayani R, Rakesh Analysis of visual prognosis after surgery in traumatic cataract. J Evid Based Med Healthc. 2014;1:1029–46. [Google Scholar]
- 7.Morrison D, Sternberg P, Donahue S. Anterior chamber intraocular lens (ACIOL) placement after pars plana lensectomy in pediatric Marfan syndrome. J AAPOS. 2005;9:240–2. doi: 10.1016/j.jaapos.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Lifshitz T, Levy J, Klemperer I. Artisan aphakic intraocular lens in children with subluxated crystalline lenses. J Cataract Refract Surg. 2004;30:1977–81. doi: 10.1016/j.jcrs.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 9.Kopel AC, Carvounis PE, Hamill MB, Weikert MP, Holz ER. Iris-sutured intraocular lenses for ectopia lentis in children. J Cataract Refract Surg. 2008;34:596–600. doi: 10.1016/j.jcrs.2007.11.044. [DOI] [PubMed] [Google Scholar]
- 10.Konradsen T, Kugelberg M, Zetterström C. Visual outcomes and complications in surgery for ectopia lentis in children. J Cataract Refract Surg. 2007;33:819–24. doi: 10.1016/j.jcrs.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Hsu HY, Edelstein SL, Lind JT. Surgical management of non-traumatic pediatric ectopia lentis: A case series and review of the literature. Saudi J Ophthalmol. 2012;26:315–21. doi: 10.1016/j.sjopt.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yen KG, Reddy AK, Weikert MP, Song Y, Hamill MB. Iris-fixated posterior chamber intraocular lenses in children. Am J Ophthalmol. 2009;147:121–6. doi: 10.1016/j.ajo.2008.07.038. [DOI] [PubMed] [Google Scholar]
- 13.Price MO, Price FW, Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:1320–6. doi: 10.1016/j.jcrs.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 14.Bhandari V, Reddy JK, Karandikar S, Mishra I. Retropupillary iris fixated intraocular lens in pediatric subluxated lens. J Clin Ophthalmol Res. 2013;1:151–4. [Google Scholar]
- 15.Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139–43. doi: 10.1016/j.jcrs.2012.07.035. [DOI] [PubMed] [Google Scholar]


