Abstract
Surgeons are under enormous pressure to continually improve and learn new surgical skills. Novel uses of surgical video in the preoperative, intraoperative, and postoperative setting are emerging to accelerate the learning curve of surgical skill and minimize harm to patients. In the preoperative setting, social media outlets provide a valuable platform for surgeons to collaborate and plan for difficult operative cases. Live streaming of video has allowed for intraoperative telementoring. Finally, postoperative use of video has provided structure for peer coaching to evaluate and improve surgical skill. Applying these approaches into practice is becoming easier as most of our surgical platforms (e.g., laparoscopic, and endoscopy) now have video recording technology built in and video editing software has become more user friendly. Future applications of video technology are being developed, including possible integration into accreditation and board certification.
Dear Editor:
Surgeons are under enormous pressure to continually improve and learn new surgical skills. Residents, now under constrained work hours, have less time in their training to master surgical techniques. Newly minted surgeons, enabled by rapidly improving technology (e.g., laparoscopic and robotic platforms), are innovating at unprecedented levels. Even seasoned surgeons, now more than ever, are faced with learning operations that were not described when they were in training. In short, surgeons at every level are continually confronted with new learning curves to maintain and improve their surgical skills.
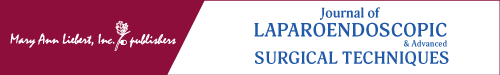
Performing new procedures while minimizing harm to patients has remained a challenge for surgeons.1 Nearly every surgical operation has a learning curve, although some are steeper than others. By definition, learning curves translate into higher patient morbidity during earlier cases.2 The increased risk to patients during early adoption of a new surgical technique and technology has received increased attention secondary to reports in mainstream media and high-profile law suits.3 Although it is clear that new technology and procedures are essential to make progress in surgery, innovation is also needed to reduce the morbidity associated with the surgeon learning curve.
Use of surgical video is emerging as a powerful tool to facilitate acquiring new surgical skills and accelerate learning new techniques. Herein we describe three novel applications with the potential to accelerate the surgical learning curve and reduce harm to patients (Fig. 1).
FIG. 1.
Reducing patient harm learning new procedures.
Preoperative, Intraoperative, and Postoperative Use of Surgical Video
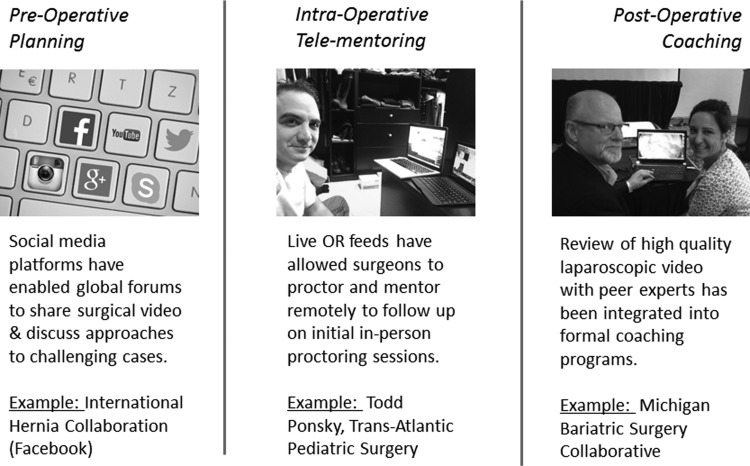
Surgical video can be used by surgeons in the preoperative, intraoperative, and postoperative phases of care to improve quality of care delivered to patients (Fig. 2).
FIG. 2.
Novel use of video to improve surgical safety.
Preoperative use of video
Social media outlets provide a valuable platform for surgeons to collaborate and plan for difficult operative cases. Probably the best example is the International Hernia Collaboration hosted on Facebook.4 More than 1900 members from around the world are in this closed group and contribute to a robust forum on hernia repair. Usually one member presents a deidentified challenging case and asks for peer input. Responses include clarifying questions, description of possible techniques, and often a narrated video of how they handled a similar operation.
Numerous advantages are present with this preoperative use of video. First, the online format allows for rapid feedback (often within minutes to hours) among surgeons who otherwise would never meet or exchange expertise. Second, surgeons often present cases that they struggled through allowing peers to identify pitfalls that led to patient morbidity as well as techniques that were effective. This, importantly, maximizes the educational benefit of the initial surgeon's first case to the benefit of future patients by other surgeons. At present, this type of forum exists for focused operations within hernia repair, but the platform exists to be extended to other specialties. A potential barrier moving forward will be maintaining patient privacy in how information is presented (i.e., nonidentifiable and nontrackable) as the shared content can be widely accessed.
Intraoperative use of video
Use of live streaming video has allowed surgeons to continue mentoring and proctoring peers in new operations during their learning curve. This can be particularly helpful in fields like pediatric surgery where operative volume is low and expertise is often centralized. To maximize the benefit of the initial in-person proctoring, pediatric surgeons have used live intraoperative video for longitudinal telementoring when the learning surgeon returns to his or her home institution.5 Similarly, the same format has been applied to experienced surgeons who want guidance on modifying and improving their technique.6
Important mentorship gaps are filled by surgical telementoring. Current training models in new procedures often involve observerships or double scrubbing a few operations before performing a procedure independently. Rather than this abrupt transition from trainee to practitioner, telementoring allows for a gradual tapering off of mentor expertise for a safer transition to independent practice. Maintaining operative mentorship as a surgeon develops and refines a new technique should help reduce patient risk during this early portion of the learning curve. Although telementoring has been well described in pediatric surgery, it is also being applied in other specialties, including global, urological, and colorectal surgery.7–9 Before telementoring can be widely adopted, surgeons will need guidelines to help decide when and how this type of surgical education should be used.
Postoperative use of video
Surgeons are using postoperative review of video to facilitate peer coaching sessions. For example, the Wisconsin Surgical Coaching Program10,11 has been used by surgeons in the Michigan Bariatric Surgical Collaborative who record a recent “typical” and “challenging” laparoscopic bariatric operation from their own practice. Meeting quarterly, surgeons then review the videos with peer coaches to share best practices and identify where the technique could be improved. Early reports from this group have demonstrated a correlation with surgical skill and patient outcomes,12 suggesting that these coaching interventions may ultimately help improve patient outcomes.
Postoperative video evaluation addresses important cognitive limitations surgeons experience while learning new techniques. Comparing surgical videos to dictated operative reports has demonstrated a sharp contrast between what the surgeons think they did and what actually happened.13 This poses a major barrier for improving a surgical technique. Reviewing a video with a peer mentor allows for an evaluation of what actually happened and proper identification of areas where a technique can be improved. As this model develops among bariatric surgeons, it will likely also disseminate to other surgical fields in which surgeons perform technically challenging procedures. Although potentially a high-yield form of quality improvement, video-based surgical coaching is time intensive and requires a significant amount of social buy-in from participating surgeons to openly share and receive feedback about their technique.
Toward Safer Surgery: Future Applications of Video Technology
Current uses of surgical video are facilitating surgeons learning new procedures and technique. A primary benefit of these advances is accelerating the surgeon learning curve. In addition, the ability of countless surgeons to learn from a single video helps reduce potential patient morbidity that is inevitably associated with the start of any procedural learning curve. Applying these approaches into practice is becoming easier as most of our surgical platforms (e.g., laparoscopic and endoscopy) now have video recording technology built in and video editing software has become more user friendly.
Future applications to maximize the power of video recording in surgery are still to be developed. Given the existing time crunch on residency work hours, video could play a vital role in helping trainee surgeons prepare for and learn from the operating room. Video may also be valuable to morbidity and mortality conferences where surgeons can peer review each other and specifically comment on technical opportunities for improvement. Finally, as our knowledge grows about the correlation of surgical technical skills and patients outcomes, objective assessment of surgical video could readily become a part of accreditation for board certification. Regardless of how surgical video is applied, it is emerging as a valuable tool to accelerate innovation and move our field toward safer surgery.
Disclosure Statement
No competing financial interests exist.
References
- 1.Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J 2007;83:777–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harrysson IJ, Cook J, Sirimanna P, Feldman LS, Darzi A, Aggarwal R. Systematic review of learning curves for minimally invasive abdominal surgery: A review of the methodology of data collection, depiction of outcomes, and statistical analysis. Ann Surg 2014;260:37–45 [DOI] [PubMed] [Google Scholar]
- 3.Pradarelli JC, Campbell DA, Jr, Dimick JB. Hospital credentialing and privileging of surgeons: A potential safety blind spot. JAMA 2015;313:1313–1314 [DOI] [PubMed] [Google Scholar]
- 4.Jacob BP. International Hernia Collaboration. 2016. www.facebook.com/groups/herniacollab/ (accessed February9, 2016)
- 5.Ponsky TA, Schwachter M, Parry J, Rothenberg S, Augestad KM. Telementoring: The surgical tool of the future. Eur J Pediatr Surg 2014;24:287–294 [DOI] [PubMed] [Google Scholar]
- 6.Treter S, Perrier N, Sosa JA, Roman S. Telementoring: A multi-institutional experience with the introduction of a novel surgical approach for adrenalectomy. Ann Surg Oncol 2013;20:2754–2758 [DOI] [PubMed] [Google Scholar]
- 7.Datta N, MacQueen IT, Schroeder AD, et al. . Wearable technology for global surgical teleproctoring. J Surg Educ 2015;72:1290–1295 [DOI] [PubMed] [Google Scholar]
- 8.Raison N, Khan MS, Challacombe B. Telemedicine in surgery: What are the opportunities and hurdles to realising the potential? Curr Urol Rep 2015;16:43. [DOI] [PubMed] [Google Scholar]
- 9.Forgione A, Kislov V, Guraya SY, Kasakevich E, Pugliese R. Safe introduction of laparoscopic colorectal surgery even in remote areas of the world: The value of a comprehensive telementoring training program. J Laparoendosc Adv Surg Tech A 2015;25:37–42 [DOI] [PubMed] [Google Scholar]
- 10.Greenberg CC, Ghousseini HN, Pavuluri Quamme SR, Beasley HL, Wiegmann DA. Surgical coaching for individual performance improvement. Ann Surg 2015;261:32–34 [DOI] [PubMed] [Google Scholar]
- 11.Hu YY, Peyre SE, Arriaga AF, et al. . Postgame analysis: Using video-based coaching for continuous professional development. J Am Coll Surg 2012;214:115–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birkmeyer JD, Finks JF, O'Reilly A, et al. . Surgical skill and complication rates after bariatric surgery. N Engl J Med 2013;369:1434–1442 [DOI] [PubMed] [Google Scholar]
- 13.Wauben LS, van Grevenstein WM, Goossens RH, van der Meulen FH, Lange JF. Operative notes do not reflect reality in laparoscopic cholecystectomy. Br J Surg 2011;98:1431–1436 [DOI] [PubMed] [Google Scholar]