Abstract
Objective
To determine whether increases in adolescent or parental self-efficacy predicted subsequent weight gain in two different therapies for adolescent anorexia nervosa (AN).
Method
Participants were 121 adolescents with AN (M = 14.4 years, SD = 1.6), from a two-site randomized clinical trial for family-based treatment (FBT) and individual adolescent focused therapy (AFT). Both adolescent and parental self-efficacy were assessed at baseline and sessions 2, 4, 6, and 8. Adolescent self-efficacy was assessed using a generic measure of self-efficacy, while parental self-efficacy was assessed using a measure specific to the recovery of an eating disorder. Weight was assessed at baseline, sessions 1 through 8, and end of treatment. Mixed-effects models were used to evaluate the relation between patient and parent self-efficacy and subsequent weight gain, controlling for weight at the previous time point.
Results
For families who received FBT, greater within-treatment increases in parental self-efficacy predicted greater subsequent adolescent weight gain compared to those who received FBT with lesser change in parental self-efficacy and those who received AFT. Interestingly, adolescent self-efficacy did not significantly predict subsequent weight gain.
Discussion
Greater increases in parental self-efficacy predicted significantly greater subsequent weight gain for adolescents who received FBT, but the same was not true for adolescents who received AFT. Neither overall level nor change in adolescent self-efficacy significantly predicted subsequent weight gain in either treatment group. These findings emphasize the importance of increasing parental self-efficacy in FBT in order to impact adolescent weight outcomes.
Keywords: adolescent anorexia nervosa, family-based treatment, adolescent focused therapy, self-efficacy, parental self-efficacy
Anorexia Nervosa (AN) is a serious psychiatric illness, with a mortality rate that is 5.9 times greater than that of the general population.1 Peak onset for AN is during adolescence,2 and successful treatment during this time is critical to ensure long-term recovery.3 Several randomized control trials (RCTs) provide support for the efficacy of family-based treatment (FBT) and to a lesser extend for adolescent-focused therapy (AFT) in adolescent AN.4–7 However, available research contributes relatively little to our understanding for whom, why, and how these therapies work.
Several baseline variables have been identified as non-specific predictors of poorer outcome, including older age,8,9 prior psychiatric or medical hospitalization,8 previous eating disorder treatment,10 and longer duration of illness.11–13 While it is certainly of significance to understand from the start of treatment who may be more successful, these baseline variables are not predictors that can be modified to improve outcome. Identifying predictors that may be modifiable over the course of treatment is of high importance in lending a successful treatment outcome.
One factor that may predict treatment response differentially in both FBT and AFT is self-efficacy—the perceived ability to successfully perform a particular behavior.14 On a theoretical level, FBT is thought to work by increasing parental self-efficacy related to AN—the ability of a parent to take charge of the child’s eating and weight-related behaviors in order to help their child recover from AN. Indeed, FBT squarely places the responsibility for adolescent weight gain on the parents, as this is conceptualized as the first step in helping their child recover from AN.15 There is limited empirical evidence to support the notion that better patient outcomes are the result of improvements in parental efficacy to combat AN.16 In AFT, on the other hand, increased general adolescent self-efficacy is theorized as a potential mechanism of change, since related research suggests that general self-efficacy is important in behavior change for many facets of health related behavior (i.e., smoking cessation, pain experience and management).17 For this reason, self-efficacy has been identified as a target for AFT.
The current study examines whether increased parental or adolescent self-efficacy predicted subsequent weight gain in adolescents with AN who were enrolled in an RCT comparing FBT and AFT, after controlling for prior weight. We hypothesized that greater overall levels of parental self-efficacy would predict greater weight gain in FBT but not AFT, while greater overall levels of adolescent self-efficacy would predict greater weight gain in AFT but not FBT. Additionally, we hypothesized that greater increases in parental self-efficacy would predict greater weight gain in FBT but not AFT, while greater increases in patient self-efficacy would predict greater weight gain in AFT but not FBT.
Methods
Data are from a two-site RCT (The University of Chicago and Stanford University) that compared FBT and AFT.5 Adolescents (n=121) meeting DSM-IV criteria for AN, excluding the criterion requiring the absence of at least three menstrual cycles, were randomly assigned to either treatment and received 24 hours of therapy over 12 months, regardless of treatment modality. Assessments were conducted at baseline and end of treatment (EOT), and additional questionnaires were completed by adolescents and parents after sessions 1, 2, 4, 6, and 8. The Institutional Review Boards at both sites approved this study, and all participants gave informed consent. Details of this design and main outcome findings are reported elsewhere.5 The adolescents were predominantly non-Hispanic White adolescent females with a mean %EBW of 82%, using the Centers for Disease Control and Prevention growth charts.
Measures
Weight
Weight was assessed in pounds by the study therapist at baseline, sessions 1 through 8, and EOT. Gown weights were taken before each major assessment, and the patients were weighed in light indoor clothing, without shoes, and after voiding, prior to each therapy session.
Eating Disorder Examination (EDE)
The EDE (version 12.0) was administered at baseline and EOT as a measure of eating disorder symptomology severity. The global score was used in this study as a measure of overall eating disorder symptom severity, including restraint, eating concern, weight concern, and shape concern. The EDE has demonstrated good reliability and validity and has been utilized in many studies of youth with eating disorders.18,19
Parents Versus Anorexia Scale (PVA)
The PVA is a seven-item scale that measures parents’ level of efficacy to help their child overcome anorexia nervosa (e.g., “I don’t have the knowledge to take a leadership role when it comes to achieving a total victory over the anorexia”; “Parents cannot be seen as the solution in the treatment of anorexia until ways in which they have caused it have been properly explored”).20 Items are rated on a four-point Likert Scale, and total scores range from 5 to 35, with higher scores indicating greater efficacy. The PVA was administered to both parents at baseline assessment, as well as sessions 2, 4, 6, and 8. Given that both parents were not always present at all time points, the score of the parent who completed the measure at any one time point was used, while the mean was calculated when both parents’ completed the measure. There is preliminary evidence of adequate psychometric properties for the PVA,20 and the PVA has been used to measure parental efficacy in several additional studies since its development.16,21
General Self-Efficacy Scale (GSES)
The GSES is a 10-item self-report questionnaire that assesses perceived self-efficacy.22 Items are rated on a four-point scale, and total scores range from 10 to 40, with higher scores indicating greater self-efficacy. Self-efficacy is assessed across a variety of areas, with each item referring to successful coping and an internal-stable attribution of success (e.g., “I can always manage to solve difficult problems if I try hard enough). The GSES was administered to adolescents at the baseline assessment, as well as sessions 2, 4, 6, and 8. The GSES has demonstrated good reliability and validity and has been used cross-culturally for more than two decades to assess general self-efficacy.23
Beck Depression Inventory (BDI)
The BDI is a 21-item multiple choice self-report inventory that was administered to adolescents at baseline to measure depressive symptom severity. Total scores range from 0 to 63, with higher scores indicating more severe depression.24
Rosenberg Self-Esteem Scale (RSES)
The RSES is a 10-item self-report questionnaire that assesses self-esteem. Items are rated on a four-point scale, from strongly agree to strongly disagree. Five of the items have positively worded statements and five have negatively worded ones. The RSES was administered at baseline to adolescents.25
Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS)
The KSADS is a widely used semi-structured interview for detecting psychiatric disorders in children and adolescents (aged 6–18).26 Both parents and adolescents were interviewed at baseline in order to assess for psychiatric comorbidity.
Statistical analyses
All analyses were conducted using SPSS Version 19.0. Mixed-effects models using residual maximum likelihood estimation evaluated the relation between efficacy and weight gain. Two separate models tested whether patient self-efficacy or parental self-efficacy (at baseline, sessions 2, 4, 6, and 8) predicted subsequent weight (at sessions 1, 3, 5, 7, and end of treatment), controlling for weight at the preceding time point (baseline, sessions 2, 4, 6, and 8). Models included a random intercept and fixed effects for time (centered at mid-treatment), treatment, and patient or parental self-efficacy. The main effect for patient or parental self-efficacy and its two- and three-way interactions with time and treatment were entered as both momentary (patient/parental self-efficacywithin-subjects, centered as a time-varying covariate) and between-subjects variables (patient/parental self-efficacybetween-subjects, centered as a time invariant covariate).
Results
Participants were mostly girls (90.9%) with a mean age of 14.4 years (SD = 1.6). Race/ethnicity were represented by non-Hispanic Whites (76%, n=92), Hispanic Whites (7.4%, n=9), Asians (10.7%, n=13), Blacks (0.8%, n=1), and ‘others’ (5.0%, n=6). Mean %Expected Body Weight was 80.4% (1.1) and mean BMI was 16.1 (1.1) using Centers for Disease Control and Prevention growth charts. The average duration of illness was 11.3 months (SD = 8.6), with 44.6% (n=54) of the sample reporting either prior hospitalization for medical problems associated with AN, including bradycardia, electrolyte imbalances, and refeeding syndrome. 17.4% of participants (n=21) had a diagnoses of AN-BP Type, and 24.5% (n=29) met criteria for a comorbid psychiatric disorder. Families were mostly intact (78.9%, n=95), and 16.5% (n=20) were taking psychotropic medications at baseline. At baseline, both adolescent self-efficacy (M = 28.4, SD = 5.6) and parental self-efficacy (M = 19.5, SD = 3.2) scores were within a moderate range.
Missing data
Out of a possible five time points, adolescents reported on self-efficacy 4.54 (SD = 1.03) times on average, and parents reported on self-efficacy at an average of 4.60 (SD = 0.98) times. Comparing adolescents who were missing any data (n = 28, 23.1%) to those with complete self-efficacy data, there were no differences by age, gender, racial/ethnic minority status (yes/no), family intact status (yes/no), income level, AN Type (Restricting v. Binge/Purge), duration of illness, baseline %EBW, baseline eating disorder symptoms (global EDE), prior hospitalization, psychiatric comorbidity (yes/no) (KSADS), depressive symptoms (BDI), baseline self-esteem (RSES), or treatment condition. Comparing parents who were missing any data (n = 24, 19.8%) to those with complete parental self-efficacy data, data were more likely to be missing for parents in AFT v. FBT (28.3% v. 11.5%; χ2(1, 121) = 5.41, p = .020). There were no differences by age, gender, racial/ethnic minority status (yes/no), family intact status (yes/no), income level, AN Type (Restricting v. Binge/Purge), duration of illness, baseline %EBW, baseline eating disorder symptoms (global EDE), prior hospitalization, psychiatric comorbidity (yes/no) (KSADS), depressive symptoms (BDI), baseline self-esteem (RSES).
Does parental self-efficacy predict weight gain?
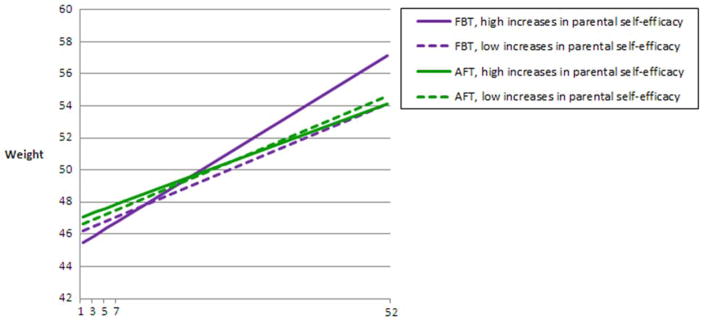
After controlling for weight at a previous time point, several predictors of weight gain at a subsequent time point emerged. There was a significant main effect for time (F1,272.8 = 138.681, p < .001), such that weight increased over time after controlling for weight at a prior time point (F1,272.5 = 77.303, p < .001). There was a significant three-way interaction between treatment, time, and within-subjects parental self-efficacy (F1,273.5 = 10.954, p < .001), such that greater within-treatment increases in parental self-efficacy for families who received FBT predicted greater weight gain for adolescents, compared to those with low change in parental self-efficacy who received FBT and those who received AFT. Treatment (p = .45) and the time by treatment interaction (p = .30) were not associated with weight gain, after controlling for other effects in the model. Similarly, between-subjects parental self-efficacy (p = .78), its two-way interactions with time (p = .32) and treatment (p = .72), and its three-way interaction with time and treatment (p = .40) were not associated with weight gain, indicating that overall level of parental self-efficacy over time (between-subjects) was not predictive of weight gain.
Does patient self-efficacy predict weight gain?
There was a significant main effect for time (F1,272.3 = 124.498, p < .001), such that weight increased over time after controlling for weight at a prior time point (F1,271.6 = 76.974, p < .001). There were no other significant predictors of weight gain (ps > .10).
Discussion
The current study examined both parental and adolescent self-efficacy as theoretical mechanisms of therapeutic change (weight gain) among adolescents with AN in an RCT of FBT and AFT. The results support our hypothesis that greater increases in parental self-efficacy during FBT (but not AFT) predict significantly greater adolescent weight gain, compared to adolescents whose parents had lesser increases in parental self-efficacy. However, contrary to our hypothesis, neither overall level nor increases in patient self-efficacy predicted weight gain in AFT. It also did not predict weight gain in FBT.
The predictive value of within-treatment increases in parental self-efficacy is particularly noteworthy as it suggests a potential mechanism of change for FBT. Regardless of initial or overall level of parental self-efficacy, parents with greater increases in self-efficacy succeeded in helping their adolescent gain more weight. This means that FBT can be an efficacious treatment for adolescents whose parents are initially disempowered, provided they become more empowered (i.e., more self-efficacious) during treatment. These results also suggest that therapists may need to place particular emphasis on ensuring increases in parental self-efficacy in order to improve adolescent outcome, and that failure to increase parental self-efficacy may lead to a weakening of the intervention effect. This is important because adolescents whose parents did not experience increased self-efficacy did not do as well as those who did. On the other hand, this study found that increasing self-efficacy in AFT (a putative target of this treatment approach) did not have a significant impact on weight gain, suggesting that there are other treatment targets that may be of higher importance in AFT. Although general self-efficacy is a proposed mechanism of therapeutic change in AFT, it may be that patient self-efficacy specifically related to AN is the important treatment target. Future research might examine subdomains of self-efficacy (e.g., related to the management of AN specifically), as well as other potential predictors of weight gain in AFT, which could help to clarify how this treatment works.
This study highlights the importance of monitoring parental self-efficacy throughout treatment, and clinicians may need to consider ways to adapt treatment if parental self-efficacy is found to remain significantly unchanged. Future research may benefit from evaluating critical times for increasing parental self-efficacy. For example, FBT involves a “family meal” session in the beginning of treatment, in which the family is asked to bring a meal typical of their family to be eaten in the session.15 Raising parental self-efficacy during the family meal may be particularly important, given that this session asks parents to help their malnourished adolescent eat a calorically-appropriate lunch or dinner. The family meal may provide an early and unique opportunity for efficacy against AN in the context of re-feeding. However, research has not yet examined the importance of the family meal in predicting treatment outcome, and certainly there are many other opportunities throughout treatment to increase parental self-efficacy. In examining more specifically the ways in which parental self-efficacy may be raised, it is possible that treatment moderators and mediators may be identified.
There are several limitations of the current study that should be noted, including the use of average parental self-efficacy scores (rather than using mother and father scores separately), modest sample size, and use of weight gain as an outcome. Certainly weight gain is not equivalent with recovery, but early weight gain has been found to predict positive outcome at end of treatment and follow-up.27,28 Furthermore, increases in weight have been found to predict psychological improvement.29 Finally, the missing data pattern by treatment for parental self-efficacy is problematic, and therefore these results should be replicated in order to strengthen the findings. Despite these limitations, this study is one of the first to examine the role of both patient self-efficacy and parental self-efficacy in adolescent treatment for AN, and therefore likely makes an important contribution in identifying a construct that may be clinically significant in FBT. Additionally, the multi-level statistical analyses established temporal precedence, thereby strengthening the argument that parental self-efficacy may serve as a factor that predicts treatment outcome.
This study highlights the importance of increasing levels of parental self-efficacy throughout the course of FBT, consistent with the theoretical underpinnings of FBT. While this study is not confirmatory, it identifies one potential factor that shows promise in understanding why some adolescents respond well to FBT while others do not. Furthermore, it identifies one key component of how FBT works that is theoretically malleable, and for which adaptations could be designed in order to further increase parental self-efficacy. Future research might examine therapist adaptations that promote greater increases in parental self-efficacy, and whether adolescent outcomes are improved as a result.
Figure 1.
Adolescent weight gain over time by treatment and level of parental self-efficacy growth (high increases = value 1SD above the mean, low increases = 1SD below the mean).
Footnotes
Acknowledgements/Disclosure of Conflicts
This manuscript is original, not previously published, and not under consideration elsewhere, and will not be submitted to any other journal while under consideration at The International Journal of Eating Disorders. None of the listed authors have a conflict of interest in the conduct or reporting of this research. As corresponding author, I will make sure that all authors are informed of editorial decisions and changes made to the manuscript.
References
- 1.Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 2.Favaro A, Caregaro L, Tenconi E, Bosello R, Santonastaso P. Time trends in age at onset of anorexia nervosa and bulimia nervosa. J Clin Psychiatry. 2009;70:1715–21. doi: 10.4088/JCP.09m05176blu. [DOI] [PubMed] [Google Scholar]
- 3.Treasure J, Russell G. The case for early intervention in anorexia nervosa: Theoretical exploration of maintaining factors. Br J Psychiatry. 2011;199:5–7. doi: 10.1192/bjp.bp.110.087585. [DOI] [PubMed] [Google Scholar]
- 4.Couturier J, Isserlin L, Lock J. Family-based treatment for adolescents with anorexia nervosa: A dissemination study. Eat Disord. 2010;18:199–209. doi: 10.1080/10640261003719443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lock J, Le Grange D, Agras S, Moye A, Bryson S, Jo B. Randomized clinical trial comparing family-based treatment to adolescent focused therapy for adolescents with anorexia nervosa. Arch Gen Psychiat. 2010;67:1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell GFM, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry. 1987;44:1047–1056. doi: 10.1001/archpsyc.1987.01800240021004. [DOI] [PubMed] [Google Scholar]
- 7.Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 1999;38:1482. doi: 10.1097/00004583-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Le Grange D, Lock J, Moye A, Bryson S, Jo B, Kraemer H. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther. 2012;50:85–92. doi: 10.1016/j.brat.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinhausen H. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry. 2002;152:1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- 10.Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D. Family therapy for adolescent anorexia nervosa: The results of a controlled comparison of two family interventions. J Child Psychol Psychiat. 2000;41:727–736. [PubMed] [Google Scholar]
- 11.Lock J, Agras WS, Bryson S, Kraemer H. A comparison of short-and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2005;44:632–639. doi: 10.1097/01.chi.0000161647.82775.0a. [DOI] [PubMed] [Google Scholar]
- 12.Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological therapies for adults with anorexia nervosa. Randomised controlled trial of outpatient treatments. Brit J Psychiat. 2001;178:216–221. doi: 10.1192/bjp.178.3.216. [DOI] [PubMed] [Google Scholar]
- 13.Russell GFM, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiat. 1987;44:1047–1056. doi: 10.1001/archpsyc.1987.01800240021004. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 15.Lock J, Le Grange D. Treatment Manual for Anorexia Nervosa, Second Edition: A Family-Based Approach. New York, New York: Guilford Press; 2013. [Google Scholar]
- 16.Robinson AL, Strahan E, Girz L, Wilson A, Boachie A. ‘I know I can help you’: Parental self-efficacy predicts adolescent outcomes in family-based therapy for eating disorders. Eur Eat Disord Rev. 2013;21:108–114. doi: 10.1002/erv.2180. [DOI] [PubMed] [Google Scholar]
- 17.O’Leary A. Self-efficacy and health. Behav Res Ther. 1985;23(4):437–51. doi: 10.1016/0005-7967(85)90172-x. [DOI] [PubMed] [Google Scholar]
- 18.Cooper Z, Cooper PJ, Fairburn CG. The validity of the Eating Disorder Examination and its subscales. Br J Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 19.Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord. 1987;6:1–8. [Google Scholar]
- 20.Rhodes P, Brown J, Baillee A. The Parents Versus Anorexia Scale: A brief measure of parental efficacy in the family-based treatment of anorexia. Eur Eat Disord Rev. 2005;13:399–405. [Google Scholar]
- 21.Rhodes P, Baillee A, Brown J, Madden S. Can parent-to-parent consultation improve the effectiveness of the Maudsley model of family-based treatment for anorexia nervosa? A randomized control trial. J Fam Ther. 2008;30:96–108. [Google Scholar]
- 22.Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Windsor, UK: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- 23.Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: Multicultural validation studies. The Journal of Psychology. 2005;139(5):439–457. doi: 10.3200/JRLP.139.5.439-457. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Ward C, Mendelson M. Beck Depression Inventory (BDI) Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 25.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 26.Biirmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, et al. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children--a preliminary psychometric study. J Psychiatr Res. 2009;43:680–686. doi: 10.1016/j.jpsychires.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doyle PM, Le Grange D, Loeb K, Celio Doyle A, Crosby R. Early response to family-based treatment for adolescent anorexia nervosa. Int J Eat Disord. 2010;43:659–662. doi: 10.1002/eat.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le Grange D, Accurso EC, Lock J, Agras S, Bryson SW. Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. Int J Eat Disord. 2014;47:124–129. doi: 10.1002/eat.22221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Accurso EC, Ciao AC, Fitzsimmons-Craft EE, Lock JD, Le Grange D. Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behav Res Ther. 2014;56:1–6. doi: 10.1016/j.brat.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]