Introduction
Men who have sex with men (MSM) are disproportionately affected by HIV/AIDS. Although MSM represent only about 2% of the population, nearly two thirds (63%) of new HIV infections in the U.S. are attributable to male-to-male sexual contact (1). This is primarily due to the efficiency of unprotected anal intercourse (UAI) as a HIV transmission vector (2). Condom-protected anal intercourse (CPAI) is much lower risk than UAI; when used properly and consistently, condoms decrease the risk of HIV transmission by approximately 70% (3). Unfortunately, rates of UAI with risky partners (i.e., partners who are HIV-positive or serostatus-unknown) remain high among some groups of MSM (4). Reducing UAI by increasing condom use would dramatically reduce HIV incidence among MSM, and is thus a public health priority.
A considerable amount of scientific effort has been devoted to developing interventions to reduce UAI among MSM. Many of these interventions have focused on increasing risk reduction knowledge or behavioral skills (e.g., 5, 6). Although these types of interventions have demonstrated efficacy, the clinical significance of the reductions in UAI they produce is usually modest (7). The observation that some MSM continue to engage in UAI with risky partners despite gaining the knowledge or skills to avoid these risks has prompted studies examining other factors that may underlie HIV risk behavior. Data suggest known relations between risky UAI and other risk behaviors (e.g. substance abuse) may be mediated by common underlying impulsive personality traits or decision-making processes (e.g., 8, 9), providing rationale to further examine relations between decision-making and UAI among MSM.
Assessment of delay discounting has been one particularly useful framework for examining relations between decision-making and risk behavior. Delay discounting is defined as the decrease in a reward or punishment’s ability to control behavior due to a delay until its occurrence. Delay discounting describes how individuals sometimes choose less valuable, immediate rewards (e.g. UAI with a risky partner now) over more valuable, delayed ones (e.g., greater odds of a future life free from HIV infection). Not all individuals discount delayed rewards at the same rate. Steeper discounting of delayed rewards has been associated with many factors that are also related to increased HIV risk among MSM, including young age, socioeconomic disadvantage, substance abuse, sexual risk taking during alcohol intoxication, and depression (10–23). These parallels suggest a plausible link between delay discounting and HIV risk among MSM.
Most studies examining delay discounting among humans have measured preferences between receiving smaller amounts of money immediately vs. receiving a larger amount after various delays (Bickel and colleagues. (2014) provided a recent general review of delay discounting research (24)). While this approach has proven utility, real-world choices between immediate and delayed outcomes involve a variety of reinforcers other than money. The Sexual Discounting Task (SDT) was developed to systematically assess the influence of delay on choices directly related to condom use in order to examine relations between discounting and HIV risk behavior (25). Studies using the SDT (25–27) have reported three important findings. First, participants reliably indicated that they would be less likely to use condoms with hypothetical sexual partners if they had to wait for condoms to become available vs. if they were available immediately. Moreover, condom-protected sex was discounted in a hyperbolic manner, that is, the largest decreases in likelihood of waiting for condoms were observed at delays of one day or less, with relatively less decrease at longer delays. This observation is theoretically important because it may account for preference reversals related to condom use. For example, individuals may assume they would delay sex to acquire a condom in certain situations when considering or planning future sexual behavior days in advance, but when the potential for sex is immediate they may choose to have unprotected sex right away instead of waiting until they acquire a condom. The hyperbolic form of the discounting function mathematically accounts for such preference reversals (28). Second, discounting of condom-protected sex was sensitive to factors that influence real-world decisions to use condoms. For example, participants discounted condom-protected sex less with partners they perceived as being most likely to have a sexually transmitted infection (STI) vs. with those they perceived as being least likely to have a STI (25–27). Finally, steeper discounting of delayed condom-protected sex was associated with higher scores on the Barrett Impulsiveness Scale-11 (27), higher rates of real-world sexual HIV risk behavior (25), and substance dependence (27). The SDT has also shown good test-retest reliability at a 1-week interval (26).
The growing literature summarized above indicates that the SDT is a promising measure of decision-making related to sexual HIV risk behavior, with internal and external validity. However, the vast majority of participants in previous studies selected only opposite gender partners on the SDT, making it unclear whether the aforementioned findings generalize to choices MSM make about condom use with male partners. Indeed, there are no published reports that examine discounting of condom-protected sex or any other HIV-related outcomes among MSM, and to our knowledge, only two studies have examined discounting of any commodity (money) among MSM (13, 23). Taken together, these studies demonstrated associations between steeper discounting of delayed monetary rewards and substance dependence (13) and higher rates of UAI (23) among MSM, and acknowledge that future studies that examine relations between discounting and HIV risk among MSM would benefit from using delay discounting tasks specific to sexual risk taking (23), as no such studies exist in the literature, indicating an important opportunity to extend this area of research.
MSM are a special population associated with unique methodological challenges with regard to research. For example, MSM who do not identify as gay or bisexual, or who are geographically isolated, may be unwilling or unable to participate in laboratory studies recruiting MSM (29, 30). Difficulties with traditional recruitment strategies have inspired the development and adoption of alternative methodologies that better reach representative samples of MSM. Many reports have demonstrated the feasibility of Internet-based data collection for studies examining sexual HIV risk behavior among MSMs (e.g., 16, 23 31–34). Crowdsourcing websites, like Amazon Mechanical Turk (MTurk), provide a new and promising venue for conducting internet-based research with MSM. MTurk allows individuals (e.g. researchers) interested in having Human Intelligence Tasks (HITs; e.g., surveys, decision-making tasks) completed to create Requester accounts. Requesters can advertise HITs on MTurk and offer monetary compensation for completion through the website’s automated payment program. Individuals who are interested in completing HITs can create Worker accounts, allowing them to browse and complete these tasks while remaining anonymous. MTurk provides access to a large (>1 million), diverse sample of Workers capable of providing high-quality data (35, 36). A substantial number of Mturk Workers are likely MSM (46% of Workers are male, 9% of Workers self-identify as gay or bisexual)(37), and Workers report characteristics associated with HIV risk (e.g., substance abuse, depression, history of trauma) at rates that meet or exceed those among the general population (37). These observations suggest that MTurk provides a viable framework for collecting delay discounting and HIV risk behavior data from MSM who are at risk for HIV infection, including MSM who may be difficult to reach for laboratory-based studies.
The present study had two aims. First, to characterize delay discounting of CPAI among MSM using the SDT. Second, to examine relations between choices on the SDT and variables associated with HIV risk among MSM, including young age, socioeconomic disadvantage, substance use, UAI, anal intercourse (AI) under the influence of substances, HIV/STI history, and history of depression or trauma.
Methods
Participants
MTurk Workers were recruited using a HIT request titled “Gay, Bisexual, and Bicurious Individuals Wanted for a Survey on Sex and Decision Making.” This title was chosen to attract the target population without disclosing study inclusion criteria prior to screening. Interested Workers completed a brief screening questionnaire, containing questions about demographics, sexual history, and willingness to answer questions about sensitive personal information. Workers were eligible to participate in the study if they identified as male, reported having AI with a male partner during the previous 6 months, and were willing to provide sensitive personal information. Eligible Workers were provided with a code to access the study survey. Participants who completed the study were compensated $1 for completing the HIT and received a $1 bonus if they provided internally consistent responses on the study questionnaire (described in the Data Analysis section). Participants were informed of the potential to earn bonuses (but not of specific bonus eligibility criteria) in advance to encourage attentive and careful responding to survey questions. The Institutional Review Board at Johns Hopkins University School of Medicine approved this study.
Measures
Questionnaire
The survey contained 65 questions pertaining to demographics, substance use, sexual history (past 6 months), HIV/STI history (lifetime and past 6 months), and psychiatric history. Many of these items were Likert scale questions adapted from the Risk Assessment Battery (38).
Sexual Discounting Task (SDT)
Delay discounting of CPAI was assessed using a version of the SDT modified for use with MSM. Participants began the task by viewing 40 photos of clothed, racially diverse men (in contrast to 30 men and 30 women in the standard version). Participants selected pictures of individuals they would consider having sex with based on appearance, and were asked to imagine that they had just met the person, that they liked his personality, and that they were not currently in a committed relationship. From the photographs selected, participants chose four hypothetical partners: The partner they most wanted to have sex with, the partner they least wanted to have sex with, the partner they thought was least likely to have a STI, and the partner they thought was most likely to have a STI. Participants could choose the same partner for more than one partner condition, but not for both conditions within comparative pairs (e.g., a single partner could be chosen for both the “most want to have sex with” and the “least likely to have a STI” conditions, but could not be chosen for both the “most want to have sex with” and “least want to have sex with” conditions).
These four partner conditions were presented to participants in randomized order. For each partner, and with the photograph of that partner shown on the computer screen, participants were shown the following instructions:
“Imagine that you have just met him. You two are getting along great and are both interested in having sex right away. Imagine that there is a condom readily and immediately available. Please rate how likely you would be to have sex with a condom vs. have sex without a condom.”
Participants used a visual analog scale (VAS; from 0 to 100%) to rate their likelihood of having CPAI immediately vs. UAI immediately (henceforth, “0-delay trial”). Next, with the picture still visible, participants were shown the following instructions:
“Now imagine this same situation, except that you must wait 1 hour for a condom to become available. Please rate how likely you would be to wait for a condom.”
Participants used the VAS again to rate their likelihood of waiting 1 hour to have CPAI vs. having UAI immediately. This process was repeated for six additional delays (3 hours, 6 hours, 1 day, 1 week, 1 month, and 3 months) presented in ascending order for each of the four SDT partner conditions.
Data Analysis
Questionnaire
Responses on related items were examined to verify internal consistency. Participants who provided inconsistent responses (e.g. indicated that he had 3 male sexual partners in his lifetime on one item, but also indicated he had 4 male sexual partners in the past 6 months on a different item) were excluded from further analyses. Variables of interest were coded dichotomously for correlational analysis examining relations between responses on the SDT and factors associated with sexual HIV risk.
Sexual Discounting Task (SDT)
Orderliness of SDT data was assessed using a criteria proposed previously (39): If a participant’s self-reported likelihood of using a condom at a given delay was higher than that of the immediately preceding delay by more than 20%, then discounting data from that partner condition were classified as nonsystematic. Nonsystematic data were excluded from further analyses on a pairwise basis. Likelihood values from delay trials were divided by values from 0-delay trials for each partner condition in order to isolate the effect of delay on choices related to condom use. If 0-delay values were equal to zero (i.e., a participant reported a 0% likelihood of using an immediately available condom), delay values were not standardized and were not included in analyses of standardized delay discounting data (but were included in analyses of 0-delay data). Once the data were standardized in this way, the area under the curve (AUC; 40) was calculated. AUC values range from 0 to 1, with smaller values indicating steeper discounting. Root mean square error (RMSE) was calculated to examine how well standardized discounting data were fit by a hyperbolic discounting equation V = 1/(1 + kD)s. In this function, V is the present perceived value of the future reward (in this case, likelihood of CPAI, expressed as a proportion), D is the length of delay to its receipt, k is a parameter governing the rate of decrease in value, and s is a nonlinear scaling parameter (27). As in previous discounting studies that have compared models (41–43) Akaike information criterion was used to determine whether the hyperbolic discounting equation was more likely to be the correct model compared an exponential discounting model that does not account for preference reversals (28).
Paired-samples t-tests were conducted to compare both 0-delay values and standardized AUC values between paired partner conditions (“most want to have sex with” vs. “least want to have sex with” and “least likely to have a STI” vs. “most likely to have a STI”). Spearman’s rank correlations were used to examine relations between both 0-delay values and standardized AUC values and: Demographic variables (age, education, and income), past 6 month substance use (alcohol, cannabis, and illicit use of substances other than cannabis), past 6 month sexual history (having >1 male partner, having male and female partners, having UAI with male partner(s), having UAI with male partner(s) because a condom was not immediately available, and having AI with male partner(s) while or after binge drinking, using cannabis, or illicitly using substances other than cannabis), HIV/STI history (not worried about getting HIV, not tested for HIV in the past 6 months, ever being diagnosed with HIV or another STI), and psychiatric history (a history of depression, child abuse, or intimate partner violence). Analyses were conducted using GraphPad Prism v.6.0 (GraphPad Software, La Jolla, CA) and SPSS v.21.0. (IBM, Armonk, NY), Significance was determined according to p<0.05.
Results
Participant characteristics
Screening results and data quality
Eighteen percent (432/2,381) of participants who completed the screening questionnaire qualified for the study. Most of those who did not qualify were excluded because they were female or males who had not had AI with a male partner during the past 6 months. Slightly more than half of those who qualified began the survey (223/432), and about three-quarters of those who began the survey completed it (168/223). About two-thirds of completers (109/168) provided internally consistent questionnaire data. One participant provided nonsystematic responses for all four SDT partner conditions and was excluded listwise. The final sample size was n=108 included in analyses.
Demographics
Table 1 shows participant demographics, substance use (past 6 months), sexual history (past 6 months), HIV/STI history (lifetime), and psychiatric history (lifetime). Participants averaged 30 years old, 89% identified as Caucasian, 42% had a 4-year college degree, and 65% made at least $30,000/year before taxes. Almost all participants identified as either gay (49%) or bisexual (47%). Four percent of participants identified as heterosexual.
Table 1.
Participant characteristics. Values are percentage of sample reporting unless otherwise indicated.
| Characteristic | (n=108) |
|---|---|
| Demographics | |
| Age (years) (mean ± SD) | 30.0 ± 9.1 |
| Race | |
| Caucasian | 89 |
| African American | 6 |
| Asian American | 1 |
| More than one race (e.g., Caucasian and African American) | 5 |
| Ethnicity (identify as Hispanic/Latino) | 6 |
| Education (highest level completed) | |
| Less than high school | 1 |
| High school diploma or equivalent | 47 |
| Associate (two-year) degree | 10 |
| Batchelor's (four-year) degree | 27 |
| Graduate or professional degree | 15 |
| Annual income before taxes | |
| Under $30,000 | 35 |
| $30,000–$59,999 | 24 |
| $60,000 or more | 44 |
| Sexual Identity | |
| Gay | 49 |
| Bisexual | 47 |
| Heterosexual | 4 |
| Substance use (past 6 months) | |
| Alcohol | 85 |
| Cannabis | 42 |
| Drugs other than cannabis and alcohol (at least one of the following) | 30 |
| Opioids (e.g., heroin, prescription opioid pain medications) | 11 |
| Stimulants (e.g., cocaine, methamphetamine, prescription stimulants) | 11 |
| Club drugs (e.g., MDMA, ketamine, GHB) | 6 |
| Erectile disfunction drugs drugs (e.g., Viagra®, Cialis®, etc.) not prescribed to them | 5 |
| Alkyl nitrites ("poppers") | 3 |
| Hallucinogens (e.g., LSD, psilocybin) | 2 |
| Other (e.g., synthetic cannabis, "bath salts", Salvia divinorum) | 4 |
| Sexual history (past 6 months) | |
| More than one male AI partner | 44 |
| Both male and female sexual partners | 44 |
| UAI with male partner(s) | 75 |
| UAI with male partner(s) because a condom was not immediately available | 24 |
| Unprotected sex with female partner(s) | 37 |
| AI with male partner(s) while/after binge drinking (! 5 drinks) | 26 |
| AI with male partner(s) while/after using cannabis | 35 |
| AI with male partner(s) while/after illicitly using drugs other than cannabis | 20 |
| HIV/STIs | |
| Worried about getting HIV | 66 |
| Tested for HIV in the past 6 months | 46 |
| Diagnosed HIV positive | 2 |
| Diagnosed with a STI other than HIV | 12 |
| Psychiatric History | |
| Diagnosed with depression | 35 |
| Victim of child abuse | 30 |
| Victim of intimate partner violence | 35 |
Note. SD = standard deviation, MDMA = methylendioxymethylamphetamine, GHB = gamma-hydroxybutyric acid, LSD = lysergic acid diethylamide, AI = anal intercourse, UAI = unprotected anal intercouse, HIV = human immunodeficiency virus, STI = sexually transmitted infection
Income data were only available for n=57.
Substance Use
Regarding substance use in the past 6 months, 85% of participants reported using alcohol, 42% reported using cannabis, and 30% reported illicit use of drugs other than cannabis (e.g. opioids, stimulants, club drugs).
Sexual History
Regarding sexual history in the past 6 months, 44% of participants reported having AI with more than one male partner, 44% reported having sex with both male and female partners. Three quarters of participants reported UAI with a male partner, 24% reported UAI with a male partner because they did not have a condom immediately available, and 37% reported unprotected intercourse with a female partner. Regarding sex under the influence of substances in the past 6 months, 26% reported having AI with male partners while or after binge drinking (≥5 drinks), 35% while or after using cannabis, and 20% while or after illicit use of drugs other than cannabis.
HIV/Sexually Transmitted Infection (STI) History
Regarding lifetime HIV/STI history, two thirds of participants were worried about potentially contracting HIV, however, less than half (46%) had been tested for HIV in the prior 6 months. Two percent of participants were HIV positive, and 12% of had been diagnosed with an STI other than HIV.
Psychiatric History
About a third of participants reported lifetime histories of depression (35%), child abuse (30%) and/or intimate partner violence (35%).
Sexual Discounting Task (SDT)
Orderliness of Discounting Data
Eighty-nine percent of SDT data sets (a data set consists of a participant’s responses to one hypothetical partner condition) from the 108 participants included in analyses were systematic. Likelihood of using a condom decreased as the delay to condom availability increased for all four SDT partner conditions in a manner well-fit by hyperbolic discounting functions (mean RMSE values were 0.09 for all four SDT partner conditions). Akaiki information criterion analysis showed that in all four partner conditions the hyperbolic model had a >0.99 probability of being the correct model over the exponential model.
Likelihood of Using Immediately Available Condoms (0-Delay Values)
Participants indicated they would be less likely to use an immediately available condom with the partner they would most want to have sex with (M = 65.8, SEM = 4.5) vs. the partner they would least want to have sex with (M = 79.7, SEM = 2.7), t(84) = −3.43, p=.001, and with the partner they thought was least likely to have a STI (M = 63.9, SEM = 4.4) vs. the partner they thought was most likely to have a STI (M = 88.5, SEM = 2.3), t(86) = −5.66, p< .001.
Discounting of Condom-Protected Anal Intercourse (CPAI)
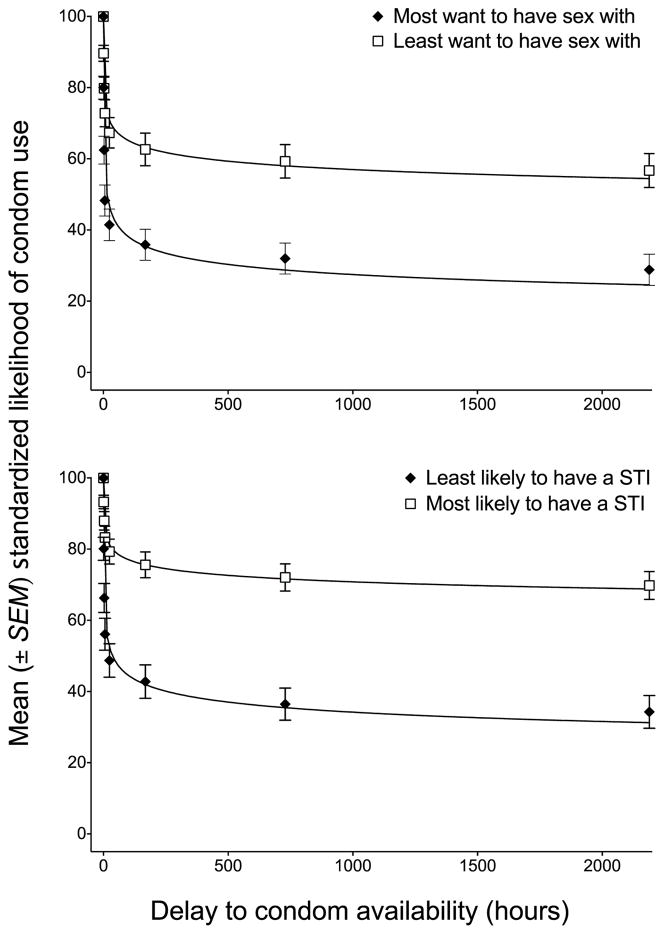
Mean standardized likelihood values from each pair of partner conditions are displayed in Figure 1. Participants discounted the value of CPAI more steeply for the partner that they would most want to have sex with (M = 0.35, SEM = .05) vs. the partner that they would least want to have sex with (M = 0.60, SEM = .05), t(67) = −5.37, p<.001, and for the partner they thought was least likely to have a STI (M = 0.36, SEM = .05) vs. the partner that they thought was most likely to have a STI (M = 0.73, SEM = .04), t(72)= −8.01, p<.001.
Figure 1.
Mean (±SEM) standardized likelihoods of condom use with best-fit hyperbolic discounting functions for “most want to have sex with” and ”least want to have sex with” partner conditions (top graph) and “least likely to have a STI” and “most likely to have a STI” partner conditions (bottom graph) (n=108).
Correlations Between Participant Characteristics and the Sexual Discounting Task (SDT)
Likelihood of Using an Immediately Available Condom
Spearman’s rank correlation coefficients between likelihood of using an immediately available condom (0-delay likelihood) and participant characteristics associated with HIV risk are shown in Table 2. An income of <$30,000/year, illicit use of drugs other than cannabis in the past 6 months, having >1 male partner in the past 6 months, having had both male and female partners in the past 6 months, and having UAI with male partner(s) in the past 6 months were all significantly associated with a lower likelihood of using an immediately available condom with at least one SDT partner.
Table 2.
Spearman’s rank correlation coefficients between SDT 0-delay trial values and participant characteristics. Significant correlations (p<.05) are shown in bold. Negative values indicate the variable was associated with a lower likelihood of using an immediately available condom for the partner condition indicated above.
| Characteristic | Most want to have sex with | Least want to have sex with | Least likely to have a STI | Most likely to have a STI |
|---|---|---|---|---|
| Demographics | ||||
| Under 30 years of age | −.06 | .02 | −.05 | .05 |
| No 4-year college degree | −.10 | .14 | .13 | −.03 |
| Income < $30,000/year* | −.08 | −.16 | −.31 | −.22 |
| Substance use (past 6 months) | ||||
| Alcohol | −.13 | .00 | .05 | −.06 |
| Cannabis | −.12 | .03 | .08 | −.20 |
| Illicit use of drugs other than cannabis (e.g., opioids, stimulants, club drugs) | −.21 | −.22 | −.16 | −.16 |
| Sexual history (past 6 months) | ||||
| More than one male AI partner | −.25 | −.10 | −.07 | −.09 |
| Both male and female sexual partners | −.12 | −.20 | −.13 | −.36 |
| UAI with male partner(s) | −.24 | −.22 | −.11 | −.30 |
| UAI with male partner(s) because condom was not immediately available | −.18 | .11 | .07 | .03 |
| AI with male partner(s) during/after binge drinking (! 5 drinks) | −.17 | −.12 | −.07 | .00 |
| AI with male partners while/after using cannabis | −.13 | −.02 | .05 | −.19 |
| AI with male partners while/after illicitly using drugs other than cannabis | −.07 | −.06 | −.12 | −.11 |
| HIV/STIs | ||||
| Not worried about getting HIV | .09 | .11 | −.07 | −.04 |
| Not tested for HIV in past 6 months | .16 | .10 | .10 | .11 |
| Diagnosed with HIV or another STI | .01 | .02 | .03 | .02 |
| Psychiatric History | ||||
| Diagnosed with depression | .12 | .07 | .13 | .07 |
| Victim of child abuse | −.06 | −.11 | .15 | −.03 |
| Victim of intimate partner violence | −.04 | −.02 | .08 | .07 |
Note. AI = anal intercourse, UAI = unprotected anal intercourse HIV = human immunodeficiency virus, STI = sexually transmitted infection
Income data only available for n=57.
Discounting of Condom-Protected Anal Intercourse (CPAI)
Spearman’s rank correlation coefficients between standardized AUC values and participant characteristics are also shown in Table 3. Being < 30 years old, use of cannabis in the past 6 months, illicit use of drugs other than cannabis in the past 6 months, having had both male and female partners in the past 6 months, having UAI with a male partner(s) in the past 6 months, having had UAI with male partner(s) in the past 6 months because a condom was not immediately available, having had AI with male partner(s) while or after binge drinking or illicitly using drugs other than cannabis in the past 6 months, not having been tested for HIV in the past 6 months, and having been diagnosed with depression were all significantly associated with steeper discounting of CPAI with at least one SDT partner.
Table 3.
Spearman’s rank correlation coefficients between SDT AUC values and participant characteristics. Significant correlations (p<.05) are shown in bold. Negative values indicate the variable was associated with steeper discounting of delayed condom-protected sex for the partner condition indicated above.
| Characteristic | Most want to have sex with | Least want to have sex with | Least likely to have a STI | Most likely to have a STI |
|---|---|---|---|---|
| Demographics | ||||
| Under 30 years of age | −.23 | .14 | −.22 | .12 |
| No 4-year college degree | −.13 | −.02 | .02 | −.02 |
| Income < $30,000/year* | −.25 | −.14 | −.15 | −.24 |
| Substance use (past 6 months) | ||||
| Alcohol | −.18 | .14 | −.02 | −.16 |
| Cannabis | −.25 | −.11 | .01 | −.15 |
| Illicit use of drugs other than cannabis (e.g., opioids, stimulants, club drugs) | −.26 | −.13 | −.26 | −.33 |
| Sexual history (past 6 months) | ||||
| More than one male AI partner | .06 | .06 | −.08 | −.14 |
| Both male and female sexual partners | −.08 | −.01 | −.17 | −.26 |
| UAI with male partner(s) | −.29 | −.22 | −.17 | −.19 |
| UAI with male partner(s) because condom was not immediately available | −.18 | −.06 | −.16 | −.23 |
| AI with male partner(s) during/after binge drinking (! 5 drinks) | −.22 | −.10 | −.18 | −.31 |
| AI with male partners while/after using cannabis | −.10 | −.07 | .09 | −.13 |
| AI with male partners while/after illicitly using drugs other than cannabis | −.15 | −.04 | −.15 | −.31 |
| HIV/STIs | ||||
| Not worried about getting HIV | .04 | −.07 | −.07 | .11 |
| Not tested for HIV in past 6 months | −.23 | .07 | −.06 | −.13 |
| Diagnosed with HIV or another STI | −.10 | −.16 | −.14 | −.09 |
| Psychiatric History | ||||
| Diagnosed with depression | −.22 | −.14 | −.14 | −.23 |
| Victim of child abuse | .02 | .06 | .15 | .03 |
| Victim of intimate partner violence | −.09 | −.10 | −.06 | −.19 |
Note. AI = anal intercourse, UAI = unprotected anal intercourse HIV = human immunodeficiency virus, STI = sexually transmitted infection
Income data only available for n=57
Discussion
The present study had three major findings. First, MSM discounted the value of delayed CPAI in a manner that was orderly and well-fit by hyperbolic functions. Second, discounting of CPAI was sensitive to partner characteristics likely to influence decisions to use condoms (e.g., partner desirability, perceived STI risk). Third, participants’ choices on the SDT were significantly associated with several variables associated with sexual HIV risk among MSM.
To our knowledge, ours is the first study to examine delay discounting of condom-protected sex among MSM. MSM in the present study indicated decreased likelihood of using a condom with hypothetical partners as delays to condom availability increased. Furthermore, likelihood of using a condom decreased as a function of delay in a manner well-fit by hyperbolic functions, suggesting that discounting might underlie preference reversals related to condom use. That is, despite previous intentions to practice safer sex, during spontaneous sexual situations where a condom is not immediately available, individuals may defect on previous intentions and opt for immediate UAI, as has been demonstrated for the hyperbolic discounting of monetary consequences (28). This may partly explain discrepancies between condom use intentions and actual condom use (e.g., 44), and relations between UAI and impulsivity (e.g., 9, 23) described in previous reports examining sexual HIV risk among MSM.
Participants indicated they were less likely to use immediately available condoms and discounted CPAI more steeply for partners they most wanted to have sex with vs. those they least wanted to have sex with, and for those they thought were least likely to have an STI vs. those they thought were most likely to have an STI. This suggests that choices on the SDT are sensitive to factors that influence real-world decisions to use condoms. The robust effects of delay on likelihood of condom use observed in this study warrant discussion. Given the choice between immediate UAI vs. immediate CPAI, participants, on average, indicated that they would most likely use a condom with all four hypothetical sexual partners. Delaying condom access by 6 hours led to a nearly 50% reduction in participants’ perceived likelihood of using a condom with the partner they most wanted to have sex and the partner they thought was least likely to have a STI. Delays of this length could very well be encountered in real-world situations similar to the hypothetical sexual scenarios presented in the SDT, suggesting that discounting may increase UAI among MSM in circumstances where condoms are not immediately available.
Lower likelihood of using an immediately available condom and steeper discounting of CPAI were both significantly associated with self-reported behaviors often responsible for HIV transmission (UAI) and other variables associated with sexual HIV risk (e.g., young age, economic disadvantage, substance use, depression) among MSM. Importantly, steeper discounting was significantly associated with UAI that occurred specifically because a condom was not available (i.e., situations in which participants would use a condom if they had one, but chose to have UAI rather than wait for a condom), a behavior that occurred among approximately one fourth of study participants in the past 6 months. These findings suggest that preferences regarding condom use in general and discounting of delayed CPAI may independently underlie relations between these known risk factors and HIV transmission.
The relations between variables associated with HIV risk and likelihood of using immediately available condoms (Table 2) and delay discounting of condom-protected sex (Table 3) may inform targeted HIV prevention interventions. For example, some variables (e.g., illicit use of drugs other than cannabis) were associated with both decreased likelihood of using immediately available condoms and steeper discounting of condom-protected sex. Individuals such as these would likely benefit from interventions that have multiple components, i.e., interventions that increase condom acceptability and condom carrying, and decrease delay discounting (e. g, working memory training has been show to decrease delay discounting)(45). Other variables (e.g., young age, history of depression) were associated with steeper discounting of condom-protected sex, but had no significant relations to likelihood of using immediately available condoms. For these individuals, increasing condom carrying and/or decreasing delay discounting of condom-protected sex may be a more critical intervention target than improving condom acceptability.
The observed relations between having both male and female partners and decreased likelihood of using immediately available condoms and steeper discounting of condom-protected sex warrant additional discussion. Men who have sex with men and women may be responsible for the transmission of HIV from one socio-sexual network (MSM) to another (heterosexual individuals). Almost half of MSM in the present study reported having sex with both male and female partners in the past 6 months, and these individuals indicated that they were less likely to use immediately available condoms compared to participants who reported having only male partners. Moreover, individuals reporting sex with both males and female partners discounted delayed condom-protected sex with a high-risk male partner (i.e., “Most likely to have an STI“ partner) more steeply than individuals who only reported male partners. For MSM with male and female partners, interventions aimed at increasing condom acceptability and condom carrying and/or decreasing discounting of condom-protected sex with male and female partners would be beneficial, thereby reducing HIV bridging between MSM and heterosexual individuals. Furthermore, interventions aimed at increasing condom use among women who have male partners who also have sex with men would be beneficial, although these women may be challenging to reach since many of them may be unaware that their partners are MSM (46,47).
A notable strength of the present study is that crowdsourcing via MTurk appears to be a viable means of collecting data on delay discounting of condom-protected sex and sexual HIV risk behavior from MSM. The majority of participants who completed the study provided high quality data, and the consistency of our findings with the larger delay discounting literature suggest participants provided truthful responses. It is also evident that we were able to sample from a population of MSM at risk for sexually transmitted HIV. Comparing the characteristics of MSM in the present study to those from clinical trials (e.g., 19), survey studies utilizing in-person recruitment (e.g., 48), and other web-based studies (e.g., 49) suggests that our participants were reasonably representative of MSM who participate in HIV-related behavioral research in the U.S. Furthermore, because of the anonymous, web-based medium in which the study was conducted, we were able to recruit participants who may have been difficult to recruit via in-person sampling (e.g., those who identified as heterosexual, those who had female partners). Together, these results suggest that crowdsourcing appears to be a promising platform for collecting data on sexual HIV risk behavior among special populations, such as MSM.
Our results should be considered in light of three noteworthy limitations. First, data were collected anonymously, making it difficult to verify the accuracy of participant responses. However, our screening procedure, modest compensation rate, and the anonymity of crowdsourcing provided participants no obvious incentive to misrepresent themselves. Second, the racial makeup of the present study sample may not accurately represent the racial makeup of MSM in the U.S. For example, although 8.9% of MSM in the U.S. are African-American (50), only 6% of the present sample was African-American. Although the exact racial characteristics of the MTurk Worker pool are unknown, other studies suggest that African-American individuals are underrepresented on MTurk compared to the U.S. population as a whole (37, 51). Since African-American MSM are disproportionately affected by HIV, future studies using MTurk would benefit from using recruitment and screening methods that provide more representative samples with regard to racial makeup. Furthermore, the screening and recruitment methodology of the present study could be adapted to target high-risk groups of MSM (e.g., young African American MSM) if researchers wish to collect data from these subgroups specifically. Third, the SDT examines choices related to sex and condom use with hypothetical partners. Although we cannot be sure that these choices accurately represent decisions that occur in real-world sexual situations, previous work with the SDT has shown that steeper discounting on the SDT is associated with higher rates of real-world risky sexual behavior (25). Overall, the consistency of our findings with the existing scientific literature on both delay discounting and on sexual HIV risk among MSM suggests data collected using the SDT provide a valid representation of how delay influences choices related to condom use among this population.
Conclusions
This report demonstrates that discounting of CPAI among MSM is orderly, hyperbolic, sensitive to partner characteristics, and is related to factors associated with sexual HIV risk. Considering these findings together with the observation that approximately one fourth of study participants reported having UAI with a male partner in the past 6 months specifically because they did not have a condom immediately available suggests that delay discounting is a critical, but underappreciated facet of HIV risk among MSM. Furthermore, these findings suggest that discounting may underlie the limited efficacy of interventions that aim to reduce sexual HIV risk behavior through increasing knowledge and skills alone if condoms are not always immediately available. Future studies should further examine relations between delay discounting and condom carrying behavior among MSM. If MSM who discount CPAI steeply (e.g. substance users) also have difficulty planning ahead and remembering to carry condoms, they may represent a specific risk group that could benefit from interventions that specifically target increasing condom carrying and/or decreasing delay discounting.
Acknowledgments
This research was supported by R01 DA032363, R21 DA032717 and T32 DA07209 from the National Institute on Drug Abuse.
References
- 1.Centers for Disease Control and Prevention. CDC Fact Sheet: New HIV infections in the United States. 2012 http://www.cdc.gov/nchhstp/newsroom/docs/2012/HIV-Infections-2007-2010.pdf.
- 2.Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. Int J Epidemiol. 2010;39(4):1048–63. doi: 10.1093/ije/dyq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith D, et al. Condom efficacy by consistency of use among MSM: US. 20th Conference on Retroviruses and Opportunistic Infections; Atlanta. 2013. p. abstract 32. [Google Scholar]
- 4.Yang Z, Zhang S, Dong Z, Jin M, Han J. Prevalence of unprotected anal intercourse in men who have sex with men recruited online versus offline: a meta-analysis. BMC public health. 2014;14(1):508. doi: 10.1186/1471-2458-14-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: feasibility, acceptability, and preliminary efficacy. J Behav Med. 2008;31(6):463–477. doi: 10.1007/s10865-008-9171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-positive MSM methamphetamine users: results from the EDGE study. Drug Alcohol Depend. 2007;87(2):249–257. doi: 10.1016/j.drugalcdep.2006.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herbst JH, Sherba RT, Crepaz N, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39(2):228–241. [PubMed] [Google Scholar]
- 8.Patterson TL, Semple SJ, Zians JK, Strathdee SA. Methamphetamine-using HIV-positive men who have sex with men: correlates of polydrug use. J Urban Health. 2005;82:i120–i126. doi: 10.1093/jurban/jti031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Semple SJ, Zians J, Grant I, Patterson TL. Methamphetamine use, impulsivity, and sexual risk behavior among HIV-positive men who have sex with men. J Addict Dis. 2006;25(4):105–114. doi: 10.1300/J069v25n04_10. [DOI] [PubMed] [Google Scholar]
- 10.Boone MR, Cook SH, Wilson P. Substance use and sexual risk behavior in HIV-positive men who have sex with men: An episode-level analysis. AIDS Behav. 2013;17(5):1883–1887. doi: 10.1007/s10461-012-0167-4. [DOI] [PubMed] [Google Scholar]
- 11.Catania JA, Osmond D, Stall RD, et al. The continuing HIV epidemic among men who have sex with men. Am J Public Health. 2001;91(6):907–914. doi: 10.2105/ajph.91.6.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colfax G, Vittinghoff E, Husnik MJ, et al. Substance use and sexual risk: a participant-and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159(10):1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- 13.Dierst-Davies R, Reback CJ, Peck JA, Nuño M, Kamien JB, Amass L. Delay-discounting among homeless, out-of-treatment, substance-dependent men who have sex with men. Am J Drug Alcohol Abuse. 2011;37(2):93–97. doi: 10.3109/00952990.2010.540278. [DOI] [PubMed] [Google Scholar]
- 14.Green L, Fry AF, Myerson J. Discounting of delayed rewards: a life-span comparison. Psych Sci. 1994;5:33–36. [Google Scholar]
- 15.Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addict Behav. 2006;31(7):1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: a national online study in the USA. AIDS care. 2004;16(8):1036–1047. doi: 10.1080/09540120412331292525. [DOI] [PubMed] [Google Scholar]
- 17.Jaroni JL, Wright SM, Lerman C, Epstein LH. Relationship between education and delay discounting in smokers. Addictive behaviors. 2004;29(6):1171–1175. doi: 10.1016/j.addbeh.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 18.MacKillop J, Celio MA, Mastroleo NR, et al. Behavioral Economic Decision Making and Alcohol-related Sexual Risk Behavior. AIDS and Behavior. 2014:1–9. doi: 10.1007/s10461-014-0909-6. Epub Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mimiaga MJ, Noonan E, Donnell D, et al. Childhood sexual abuse is highly associated with HIV risk–taking behavior and infection among MSM in the EXPLORE study. J Acquir Immune Defic Syndr. 2009;51(3):340–348. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Educ Prev. 2003;15(1):81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi T, Oono H, Inoue T, et al. Depressive patients are more impulsive and inconsistent in intertemporal choice behavior for monetary gain and loss than healthy subjects-An analysis based on Tsallis' statistics. Neuro Endocrinol Lett. 2008;29(3):351–358. [PubMed] [Google Scholar]
- 22.Hoffman WF, Moore M, Templin R, McFarland B, Hitzemann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology. 2006;188(2):162–170. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- 23.Jones J, Sullivan PS. Impulsivity as a risk factor for HIV transmission in men who have sex with men: A delay discounting approach. J Homosex. 2015;62(5):588–603. doi: 10.1080/00918369.2014.987568. [DOI] [PubMed] [Google Scholar]
- 24.Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–77. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson MW, Bruner NR. The Sexual Discounting Task: HIV risk behavior and the discounting of delayed sexual rewards in cocaine dependence. Drug Alcohol Depend. 2012;123(1):15–21. doi: 10.1016/j.drugalcdep.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson MW, Bruner NR. Test–retest reliability and gender differences in the sexual discounting task among cocaine-dependent individuals. Exp Clin Psychopharmacol. 2013;21(4):277–286. doi: 10.1037/a0033071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herrmann ES, Hand DJ, Johnson MW, Badger GJ, Heil SH. Examining delay discounting of condom-protected sex among opioid-dependent women and non-drug-using control women. Drug Alcohol Depend. 2014;144:53–60. doi: 10.1016/j.drugalcdep.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green L, Fristoe N, Myerson J. Temporal discounting and preference reversals in choice between delayed outcomes. Psychon Bull Rev. 1994;1(3):383–389. doi: 10.3758/BF03213979. [DOI] [PubMed] [Google Scholar]
- 29.Chiasson MA, Parsons JT, Tesoriero JM, Carballo-Dieguez A, Hirshfield S, Remien RH. HIV behavioral research online. J Urban Health. 2006;83(1):73–85. doi: 10.1007/s11524-005-9008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams ML, Bowen AM, Horvath K. The social/sexual environment of gay men residing in a rural frontier state: Implications for the development of HIV prevention programs. J Rural Health. 2005;21:48–55. doi: 10.1111/j.1748-0361.2005.tb00061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bull SS, McFarlane M, Rietmeijer C. HIV and sexually transmitted infection risk behaviors among men seeking sex with men on-line. Am J Public Health. 2001;91(6):988–989. doi: 10.2105/ajph.91.6.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khosropour CM, Johnson BA, Ricca AV, Sullivan PS. Enhancing Retention of an Internet-Based Cohort Study of Men Who Have Sex With Men (MSM) via Text Messaging: Randomized Controlled Trial. J Med Internet Res. 2013;2013:15, e194. doi: 10.2196/jmir.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: A mixed-methods study. Arch Sex Behav. 2011;40(2):289–300. doi: 10.1007/s10508-009-9596-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosser BS, Oakes JM, Horvath KJ, Konstan JA, Danilenko GP, Peterson JL. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s INTernet Sex Study-II (MINTS-II) AIDS Behav. 2009;13(3):488–498. doi: 10.1007/s10461-009-9524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk A New Source of Inexpensive, Yet High-Quality, Data? Perspect Psychol Sci. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 36.Paolacci G, Chandler J, Ipierotis P. Running experiments on Amazon Mechanical Turk. Judgm Decis Mak. 2010;5:411–419. [Google Scholar]
- 37.Shapiro DN, Chandler J, Mueller P. Using Mechanical Turk to Study Clinical Populations. Clin Psychol Sci. 2013;1:213–220. [Google Scholar]
- 38.Metzger DS, et al. The Risk Assessment Battery: Validity and Reliability. Paper presented at the 6th Annual Meeting of National Cooperative Vaccine Development Group for AIDS; Nov, 1993. [Google Scholar]
- 39.Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Exp Clin Psychopharm. 2008;16(3):264–274. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Myerson J, Green L, Warusawitharana M. Area under the curve as a measure of discounting. J Exp Anal Behav. 2001;76:235–243. doi: 10.1901/jeab.2001.76-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Odum AL, Baumann AA, Rimington DD. Discounting of delayed hypothetical money and food: Effects of amount. Behav Process. 2006;73(3) doi: 10.1016/j.beproc.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 42.Takahashi T, Ikeda K, Hasegawa T. A hyperbolic decay of subjective probability of obtaining delayed rewards. Behav Brain Funct. 2007;3(1):52. doi: 10.1186/1744-9081-3-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Killeen PR. An additive-utility model of delay discounting. Psychol Rev. 2009;116(3):602–619. doi: 10.1037/a0016414. [DOI] [PubMed] [Google Scholar]
- 44.McFarland W, Chen YH, Nguyen B, et al. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16(1):121–131. doi: 10.1007/s10461-011-9936-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69(3):260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kalichman SC, Roffman RA, Picciano JF, Bolan M. Risk for HIV infection among bisexual men seeking HIV-prevention services and risks posed to their female partners. Health Psychology. 1998;17(4):320. [PubMed] [Google Scholar]
- 47.Agyemang S, Wallace BC, Liebman RE. An exploratory Internet study of Black men on the down low: Potential factors related to non-disclosure to female partners and inconsistent condom use for Black men who have sex with men and women (MSMW) Int J Equity Health. 2008;1(1):79–97. [Google Scholar]
- 48.Eaton LA, Kalichman SC, Cherry C. Sexual partner selection and HIV risk reduction among black and white men who have sex with men. Am J Public Health. 2010;100(3):503–509. doi: 10.2105/AJPH.2008.155903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitchell JW. HIV-negative and HIV-discordant gay male couples’ use of HIV risk-reduction strategies differences by partner type and couples’ HIV-status. AIDS Behav. 2013;17(4):1557–1569. doi: 10.1007/s10461-012-0388-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lieb S, Fallon S, Friedman S, et al. Statewide estimation of racial/ethnic populations of men who have sex with men in the U.S. Public Health Rep. 2011;126(1):60–72. doi: 10.1177/003335491112600110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chandler J, Mueller P, Paolacci G. Nonnaïveté among Amazon Mechanical Turk workers: Consequences and solutions for behavioral researchers. Behav Res. 2014;46(1):112–130. doi: 10.3758/s13428-013-0365-7. [DOI] [PubMed] [Google Scholar]