Abstract
OBJECTIVES:
This study examined the long-term effects on BMI of a randomized controlled trial of Students for Nutrition and Exercise, a 5-week, middle school–based obesity prevention intervention combining school-wide environmental changes, encouragement to eat healthy school cafeteria foods, and peer-led education and marketing.
METHODS:
We randomly selected schools from the Los Angeles Unified School District and assigned 5 to the intervention group and 5 to a wait-list control group. Of the 4022 seventh-graders across schools, a total of 1368 students had their height and weight assessed at baseline and 2 years’ postintervention.
RESULTS:
A multivariable linear regression was used to predict BMI percentile at ninth grade by using BMI percentile at seventh grade, school indicators, and sociodemographic characteristics (child gender, age, Latino race/ethnicity, US-born status, and National School Lunch Program eligibility [as a proxy for low-income status]). Although the Students for Nutrition and Exercise intervention did not exhibit significant effects on BMI percentile overall, intervention students who were classified as obese at baseline (in seventh grade) showed significant reductions in BMI percentile in ninth grade (b = –2.33 percentiles; SE, 0.83; P = .005) compared with control students. This outcome translated into ∼9 pounds (∼4.1 kg) lower expected body weight after 2 years for an obese student in the intervention school at the mean height and age of the sample at baseline.
CONCLUSIONS:
Multilevel school-based interventions can have long-term effects on BMI among students who are obese. Future research should examine the mechanisms by which school-based obesity interventions can affect BMI over time.
What’s Known on This Subject:
Research indicates that school-based interventions, especially those involving changes to the school food environment, can improve adolescents’ eating behaviors. Few previous school-based obesity prevention interventions have shown long-term effects on BMI in randomized controlled trials, especially for middle school students.
What This Study Adds:
We conducted a randomized controlled trial of a middle school–based obesity prevention intervention combining environmental changes, encouragement of healthy eating and physical activity, and peer-led marketing. Students in the intervention who were obese in seventh grade showed reduced BMI in ninth grade.
More than one-fifth of US adolescents aged 12 to 19 years are obese.1–3 Although obesity rates are high overall, rates for Latino adolescents are higher than for other racial/ethnic groups (eg, 22.5% among Latinos aged 12–19 years vs 19.6% among whites).1 Because adolescent obesity is a predictor of obesity and health issues in adulthood,3 obesity prevention interventions for youth are critical.
School-based obesity prevention programs hold promise for reaching adolescents in a setting with multiple potential intervention points. School-based interventions have improved eating and physical activity behaviors among adolescents.4 For example, immediately postintervention, a 10-school randomized controlled trial (RCT) of Students for Nutrition and Exercise (SNaX), a 5-week, middle school–based intervention, found significant increases in the proportions of students served fruit and lunch in the cafeteria and a significant decrease in the proportion of students buying snacks at school. It also found greater obesity prevention knowledge, more positive attitudes about cafeteria food and tap water, increased intentions to drink water, and greater water consumption.5,6 SNaX combined school-wide environmental changes, encouragement to eat healthy food and engage in physical activity in school and at home, and peer-led education about healthy eating and physical activity. Interventions such as SNaX, which combine strategies to increase healthy nutritional intake and physical activity, have been more successful than those interventions that target only nutritional intake or physical activity.7–9
In school-based interventions, effects for BMI and other obesity-related outcomes have generally been small and short-lived.4,7,10 Although some school-based RCTs have reported effects on BMI among adolescents,11 most empirical support comes from quasi-experimental designs.12 Few RCTs of combined physical activity and nutrition-focused, school-based obesity prevention interventions have shown effects on BMI across the school population. For example, Planet Health, a middle school intervention that integrated material on increasing physical activity and healthy eating and decreasing sedentary behavior in the classroom and physical education, reported a reduction in obesity in girls but not in boys.13
Mixed results for BMI may reflect behavior change failing to transfer from the school environment to the home or neighborhood. Interventions that teach youth skills to change habits across contexts, and that also provide tools and education to parents, may be more effective. Thus, we examined the long-term effects of SNaX on BMI 2 years’ post-intervention. Although SNaX lasted only 5 weeks, a primary goal of the program was to teach students skills that could be transferred to the family and to peers, as well as to instill healthier habits and provide students and parents with strategies for longer term behavior changes.5 We hypothesized that SNaX would set in motion changes in behavior that ultimately would affect BMI.
Methods
Design
The present study was an RCT that included 5 intervention schools and 5 wait-list control schools in the Los Angeles Unified School District (LAUSD), a primarily Latino school district in Los Angeles County in which 15% of seventh-graders (∼12–13 years old) and 19% of ninth-graders (∼14–15 years old) were estimated to be obese in the 2012–2013 school year, and 22% of seventh-graders and 25% of ninth-graders were estimated to be overweight.14 The number of schools was based on a pre-RCT power analysis for small-to-medium effects.
The RCT began in January 2009. We used stratified randomization of 5 pairs of intervention-control schools, matched on baseline school similarity, such that each matched-pair was randomized together and participated during the same semester. Study implementation was staggered over 3 semesters, such that 1 matched-pair received SNaX in the 2009 spring semester, and 2 matched-pairs each received SNaX in the 2010 and 2011 spring semesters. The first 2-year post-intervention anthropometric assessment occurred in the spring 2011 semester, and the last 2-year post-intervention anthropometric assessment occurred in the spring 2013 semester. To decrease the possibility of contamination, control schools were not offered the SNaX program until the 2012–2013 school year (∼2 years after the last baseline BMI assessment and 1 year after seventh-graders exposed to SNaX would have graduated from middle school).
Intervention
SNaX was tested as a 5-week, middle school intervention combining school-wide food environmental changes with a seventh-grade peer leader club that incorporated social marketing. The environmental changes included offering a greater variety of sliced/bite-sized food and freely available chilled filtered water at lunch; posters promoting physical activity, cafeteria food, and healthy eating; and nutritional postings about cafeteria food. A main goal of the club was to increase student advocacy. Specifically, using role-plays, seventh-grade student peer leaders were taught skills for approaching other students during lunchtime activities, as well as family members at home, to promote SNaX messages (regarding cafeteria food, water, sugar-sweetened beverages, fruits/vegetables, and physical activity/inactivity) with a motivational interviewing (nonconfrontational and encouraging) style. Each peer leader was asked to recruit a partner (another student) to assist with lunchtime activities, which directly exposed more students to intervention messages. The social marketing aspect also included taste tests of cafeteria foods, delivered by peer leaders, and a short film shown to the entire seventh-grade class that encouraged physical activity (eg, through a dance video) and healthy eating. Students were encouraged to eat in the cafeteria because the district had reformulated its offerings to be healthier. All seventh-graders were given take-home activities to do with their parents during each week of the program (eg, a worksheet to indicate parents’ and adolescents’ likes and dislikes for fruits and vegetables, and the types of fruits and vegetables kept at home). After the 5-week intervention period, the club and provision of water and additional fruits and vegetables ended.
A total of 454 peer leaders and partners participated across intervention schools (23% of all seventh-graders); 1128 students across schools (57%; range, 24%–75%) completed at least 1 parent–student activity. Further descriptions of SNaX (including the setting, design, and results) are available in earlier publications,5,6,15–20 and intervention materials are available at www.snaxinschools.org.
Participants
Parents of all seventh-graders were asked for written informed consent for their child to participate in the in-class surveys before and immediately after the 5-week intervention period; for their child to participate in anthropometric measurement of height and weight; and for the team to obtain the child’s district records at seventh grade to determine National School Lunch Program (NSLP) eligibility (a proxy for lower income) and at ninth grade to obtain height and weight (assessed district-wide on the Fitnessgram, a California-mandated test that includes BMI).21 Parents gave active consent for the anthropometric assessment, NSLP data extraction, and surveys. Children provided assent.
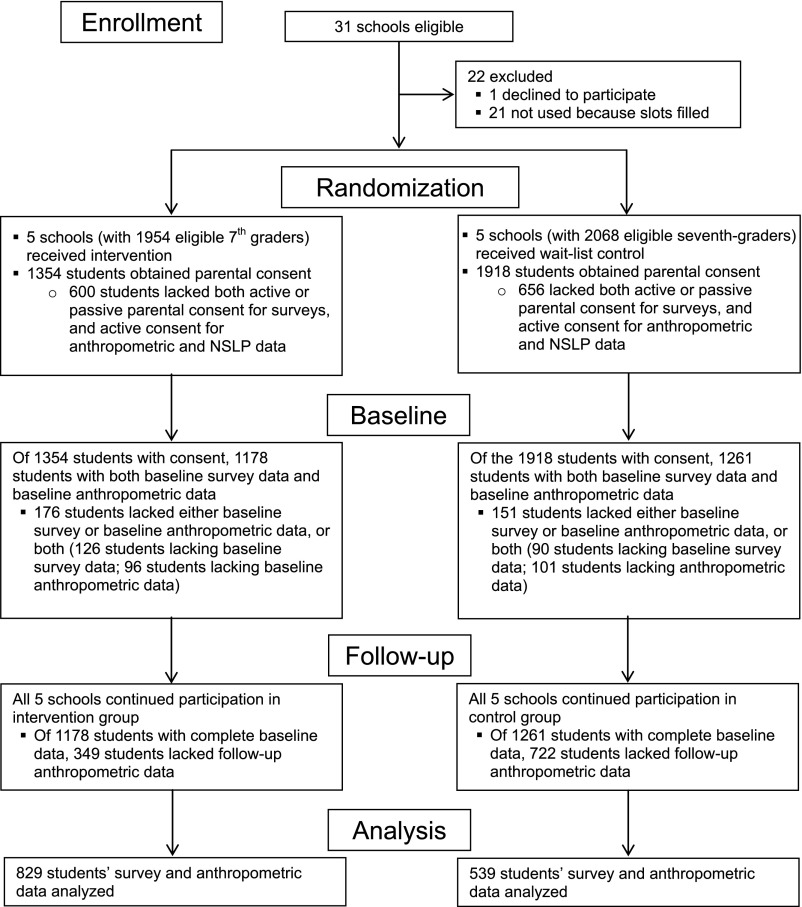
A total of 4022 students were eligible across schools (1954 intervention, 2068 control), of whom 2809 obtained parental consent for both the survey and anthropometric data collection from the child’s school records (1371 intervention, 1438 control). Of those students who had parental consent, 2439 (1178 intervention, 1261 control) had baseline survey and anthropometric data, and 1368 (829 intervention, 539 control) had follow-up anthropometric data (Fig 1). Analyses were performed on the 1368 students (829 intervention, 539 control) for whom we had a completed baseline survey and seventh- and ninth-grade anthropometric data.
FIGURE 1.
Consolidated Standards of Reporting Trials flow diagram for SNaX.
Data Collection
Outcome: Anthropometric Measurement
For all seventh-graders at baseline, study team members used a portable stadiometer (maximum capacity, ≤206 cm) to take 2 height measurements and a third when measurements differed by >0.5 cm. Weight was measured by using an electronic scale (BWB-8005; Tanita Corporation of America, Inc, Arlington Heights, IL) with a maximum capacity of 200 kg (440 pounds). BMI was calculated as (weight in pounds/[height in inches × height in inches]) × 703. Youth were classified according to the categorization by the Centers for Disease Control and Prevention as underweight (BMI <5th percentile), healthy weight (BMI ≤5th but <85th percentile), overweight (BMI ≥85th percentile and <95th percentile), or obese (BMI ≥95th percentile) by using age- and gender-appropriate charts for BMI percentile.22
At follow-up, school staff were required by the district to assess height and weight in ninth grade as part of the Fitnessgram.21 We obtained Fitnessgram height and weight records from LAUSD at ninth grade for students who participated in SNaX in seventh grade, allowing us to compare each student’s seventh- and ninth-grade BMI percentiles.
Covariates
Data on sociodemographic characteristics (eg, child gender, age, race/ethnicity, US-born status) were obtained from baseline seventh-grade surveys. We extracted NSLP eligibility for each participant from the records of the LAUSD.
Statistical Analysis
In unadjusted models, ordinary linear regressions were used to predict ninth-grade BMI percentile from seventh-grade BMI percentile and school indicators, using an intention-to-treat, individual-level analysis that compared each student’s BMI percentile in seventh grade versus his or her BMI percentile in ninth grade. The test for the effect of the intervention was constructed with a linear contrast of the school indicators, subtracting the control school coefficients from the intervention school coefficients. A second covariate-adjusted analysis added sociodemographic characteristics (child gender, age in years, Latino race/ethnicity, and US-born status), and NSLP eligibility. Thus, for both the adjusted and unadjusted models, we had an estimate specific to each school for the extent to which the ninth-grade BMI percentile differed from what would have been expected from the seventh-grade BMI percentile. These estimates were equivalent to what one would obtain with an intervention indicator but with between-school variance removed from the error term. We also examined intervention effects separately according to BMI percentile subgroup (obese, overweight, or healthy weight/underweight), based on research suggesting differential effects of obesity prevention interventions according to baseline weight status or BMI.4,23 Within treatment arms, means and SDs of BMI percentiles were calculated at the individual level, and tests for change were performed with a paired t-test.
A multivariable logistic regression determined that black race, older age, and school were significantly associated with baseline survey nonresponse. A second multivariable logistic regression among baseline survey respondents determined that Latino ethnicity and being born in the United States were associated with the presence of both seventh- and ninth-grade BMI data. Predicted probabilities from these 2 regressions were inverted and multiplied to produce nonresponse/attrition weights used for all analyses. Missing data for covariates were imputed by using weighted school means. All predictors had very few missing values (0 for gender; <0.5% for Latino race/ethnicity, US-born status, and NSLP participation; 4.5% for English spoken at home).
A set of sensitivity analyses was additionally performed to determine the robustness of the results. Separate sensitivity analyses were conducted that: (1) used BMI z-score as the outcome; (2) predicted change scores instead of controlling for baseline and predicting follow-up outcomes; (3) used an overall intervention (versus control) indicator, instead of separate indicators for each school; and (4) used an overall intervention indicator and clustering on school. In addition, based on our school selection criteria (in which we matched pairs of control and intervention schools within the same district area), 1 school served as a control school in 2009 and then again as an intervention school 1 year later in 2010. Because seventh-graders attending the school in 2009 (when their data were used for the control group) may have been exposed to the school-wide elements of the intervention as eighth-graders in 2010 (when the school received SNaX), we conducted the main analysis for all schools, and then in a sensitivity analysis, without the data from this school; of note, any intervention effect on those eighth-graders should have reduced our ability to detect an intervention effect.
Results
Participants
Across schools at baseline, 1.7% of students in the analysis sample were classified as underweight, 18.2% as healthy weight, 50.1% as overweight, and 30.0% as obese. A total of 50.9% were female, 75.4% Latino, and 60.7% US-born; 88.9% were eligible for the NSLP, indicating a primarily low-income sample. The mean ± SD age of the sample was 12.2 ± 0.68 years. Intervention and control samples did not differ significantly at baseline on age, gender, BMI, or NSLP eligibility. However, children born in the United States were less likely to be in the intervention group (odds ratio, 0.50; P < .001), and Latino participants were more likely to be in the intervention group (odds ratio, 1.40; P = .01).
Change in BMI Percentile
As indicated by the multivariable regression analyses (Table 1), obese and overweight students in the intervention and control groups, as well as students overall, exhibited significant decreases in BMI percentile over time. SNaX did not show a significantly different effect on BMI percentile for intervention versus control students overall (unadjusted b, –1.15 [SE, 1.02; P = .26]; adjusted b, –0.98 [SE, 1.01; P = .33]), for students who were of healthy weight or who were underweight (unadjusted b, –1.99 [SE, 2.40; P = .41]; adjusted b, –1.43 [SE, 2.35; P = .54]), or for students who were overweight but not obese (unadjusted b, 0.90 [SE, 1.50; P = .55]; adjusted b, 1.05 [SE, 1.51; P = .49]). However, SNaX did show a significantly different effect on BMI percentile for obese intervention students versus obese control students, such that the change in BMI percentile from seventh to ninth grade was more negative for students in intervention schools than in control schools (unadjusted b, –2.59 [SE, 0.81; P = .002]; adjusted b, –2.33 [SE, 0.83; P = .005]). In all of the sensitivity analyses (ie, predicting BMI z-score, predicting change scores, using an overall intervention indicator, using both an overall intervention indicator and clustering on school), we found similar effects for obese students in terms of significance and magnitude.
TABLE 1.
Multivariable Regression Analysis of Effects of SNaX on BMI Percentile on Ninth-Grade Fitnessgram Assessment
| Variable | Unadjusted Means and Tests for Change Within Arma | Estimated Intervention Effectb | ||||
|---|---|---|---|---|---|---|
| Control | Intervention | Unadjusted | Covariate-Adjusted | |||
| Seventh Grade | Ninth Grade | Seventh Grade | Ninth Grade | b ± SE, P | b ± SE, P | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD) | |||
| Overall; N = 1368c | 73.37 ± 27.89 | 71.84 ± 27.00* | 73.37 ± 26.90 | 70.79 ± 26.71** | −1.15 ± 1.02 | −0.98 ± 1.01 |
| Students obese at seventh grade; n = 415c | 97.67 ± 1.30 | 95.16 ± 5.52** | 97.92 ± 1.24 | 93.22 ± 10.85** | −2.59 ± 0.81*** | −2.33 ± 0.83*** |
| Students overweight at seventh grade; n = 275c | 91.22 ± 2.74 | 84.26 ± 13.94** | 90.60 ± 2.94 | 84.76 ± 11.38** | 0.90 ± 1.50 | 1.05 ± 1.51 |
| Students healthy weight/underweight at seventh grade; n = 678c | 50.98 ± 24.12 | 52.19 ± 24.50 | 52.05 ± 22.53 | 52.05 ± 23.98 | −1.99 ± 2.40 | −1.43 ± 2.35 |
Weighted means for all intervention and control students together, regardless of school. Inference tests based on weighted means and SEs of individual-level change in BMI percentile from seventh to ninth grade.
Within each row, weighted linear regression modeled ninth-grade BMI percentile on seventh-grade BMI percentile and indicators for school. Covariate-adjusted results additionally controlled for student sociodemographic characteristics (child gender, age, Latino race/ethnicity, and US-born status) and NSLP eligibility. School-level means were imputed for missing covariates (Latino, home language, US-born status, and NSLP eligibility; missing for <0.5% of the sample).
Among the 1368 students in the analysis, 829 attended intervention schools, and 539 attended control schools. The 415 students who were obese at seventh grade included 244 intervention and 171 control students, whereas the remaining 953 students included 585 intervention and 358 control students. Obesity at seventh grade was defined as being at or above the 95th percentile based on age (in months) and gender; overweight was defined as being between the 85th and 95th percentiles.
P < .05
P < .001
P < .01
To illustrate the magnitude of the adjusted 2.33 percentile intervention effect on obese seventh-graders into pounds, intervention effects were calculated for a hypothetical obese boy and a hypothetical obese girl at the baseline (seventh grade) mean height and age for obese students (5 feet 3 inches and 12.1 years for boys; 5 foot 1 inch and 12.1 years for girls). Although the translation of the intervention effect (in BMI percentiles) into pounds varies according to a student’s age, gender, and height, the effect of the intervention was equivalent to an average student who had been obese in seventh grade weighing ∼9 pounds (4.1 kg) less in ninth grade than he or she would have in the absence of an intervention (ie, 9.0 pounds or 4.1 kg for boys and 9.5 pounds or 4.3 kg for girls at the mean age and height for the sample at baseline). (The Supplemental Appendix presents a more comprehensive description of these calculations.)
The significance and magnitude of the intervention effect for the overall study sample, as well as the student BMI percentile subgroups, were similar in the sensitivity analysis omitting the control school that received the intervention 1 year later. In this analysis, the point estimates for the significant effect among obese seventh-graders were slightly stronger than what was observed in the overall analysis (b [SE], –2.47 [0.87]; P = .005).
Discussion
We present here one of the few school-based RCTs to demonstrate long-term effects on BMI percentile. BMI percentile effects were observed for obese students, who comprised nearly one-third of participants in seventh grade. The effect is striking when considered in tandem with research suggesting that obesity status is generally stable from elementary school to high school. One study found that 65% of obese fifth-graders remained obese in 10th grade, and 83% of adolescents who were obese in high school were also obese in fifth grade.24
Although we did not assess long-term mechanisms of the BMI percentile effect, we surmise that SNaX may have triggered changes in physical activity and diet that were sustained from middle school to high school, leading to reductions in BMI. Although SNaX was planned as a 5-week intervention, the main goal of SNaX was to teach adolescents skills that could generalize across contexts (school, home) and that could be sustained. For example, students were given pedometers and provided with instructions about different kinds of exercises that could be done safely at home (eg, dancing; jumping-jacks in front of the television) and at school. Students and parents were given concrete suggestions about new foods to try or keep at home, and told about the risks of sugary drinks and the value of healthy eating. SNaX-related efforts to increase awareness and interest in changes to the cafeteria food could have led to increased awareness about different kinds of fruits and vegetables, the value of drinking water, and the nutritional content of various cafeteria foods; this awareness could have transferred to different contexts over the long term. Although it is unknown why obese students in particular were affected by the intervention, such students may have had greater motivation to make behavioral changes, especially after being exposed to SNaX messages about the health consequences of obesity.
A study limitation was the use of district records for height and weight outcomes 2 years’ post-intervention, rather than follow-up assessments conducted by trained members of the study team. Thus, assessments could have differed according to school, equipment used, and training of the teacher collecting the data, introducing measurement error, although such errors would not be expected to bias change scores or the estimate of the intervention effect. Furthermore, because the study was conducted in a single district, generalizability to other districts should be considered with caution. In addition, we did not conduct a multilevel analysis that accounted for clustering within each of the 10 schools, because statistical research suggests that multilevel corrections are not well estimated and may be inaccurate with <30 higher-level units.25 In addition, SNaX was tested as a 5-week intervention. However, the long-term effects on BMI percentile presented here suggest that SNaX could have even greater impact if it were extended throughout the school year, as it likely would be if conducted in practice, to fit with existing school club and extracurricular activities.
Conclusions
SNaX, a school-based intervention to promote healthy eating and encourage physical activity, showed substantial effects on BMI among obese students 2 years’ post-intervention. Our findings suggest that brief school-based interventions can impart skills for behavior change that have long-term consequences. Results are consistent with previous research suggesting the effectiveness of combination school-based interventions which address both healthy eating and physical activity and that enact environmental changes to support newly learned health behaviors.7
Acknowledgments
The authors are grateful for the contributions of the participants, school staff and administrators, and members of the Healthy Living Advisory Board (ie, the study’s community advisory board).
Glossary
- LAUSD
Los Angeles Unified School District
- NSLP
National School Lunch Program
- RCT
randomized controlled trial
- SNaX
Students for Nutrition and Exercise
Footnotes
Dr Bogart conceptualized and designed the study, led the analysis plan and interpretation of the data, and drafted, reviewed, and revised the manuscript; Dr Elliott helped to design the study, led the analysis and interpretation of data, and reviewed and revised the manuscript; Dr Cowgill helped to design the program, helped to interpret data, and reviewed and revised the manuscript; Mr Klein analyzed and interpreted the data and drafted and revised the manuscript; Ms Hawes-Dawson led the data collection and reviewed and revised the manuscript; Dr Uyeda helped to conceptualize and design the study, helped to interpret data, and reviewed and revised the manuscript; Dr Schuster conceptualized and designed the study, analyzed and interpreted the data, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01914471).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute on Minority Health and Health Disparities (R24 MD001648; Dr Schuster, Principal Investigator). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561–566 [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873 [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Wu Y, Wilson RF, et al. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis Review No. 115. Rockville, MD: Agency for Healthcare Research and Quality; 2013 [PubMed] [Google Scholar]
- 5.Bogart LM, Cowgill BO, Elliott MN, et al. A randomized controlled trial of Students for Nutrition and Exercise: a community-based participatory research study. J Adolesc Health. 2014;55(3):415–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Los Angeles Unified School District Guide to Schools. Demographics, 2010-2011. Available at: http://notebook.lausd.net/pls/ptl/ptl_apps.schoolguide.render?p_dist_code=N
- 7.Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity (Silver Spring). 2013;21(12):2422–2428 [DOI] [PubMed] [Google Scholar]
- 8.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;3(3):CD001871. [DOI] [PubMed] [Google Scholar]
- 9.Katz DL, O’Connell M, Njike VY, Yeh MC, Nawaz H. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes. 2008;32(12):1780–1789 [DOI] [PubMed] [Google Scholar]
- 10.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;(12):CD001871. [DOI] [PubMed] [Google Scholar]
- 11.Lubans DR, Morgan PJ, Aguiar EJ, Callister R. Randomized controlled trial of the Physical Activity Leaders (PALs) program for adolescent boys from disadvantaged secondary schools. Prev Med. 2011;52(3-4):239–246 [DOI] [PubMed] [Google Scholar]
- 12.Cadzow RB, Chambers MK, Sandell AM. School-based obesity intervention associated with three year decrease in student weight status in a low-income school district. J Community Health. 2015;40(4):709–713 [DOI] [PubMed] [Google Scholar]
- 13.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–418 [DOI] [PubMed] [Google Scholar]
- 14.Los Angeles Unified School District California Healthy Kids Survey, 2012–13: Main Report. San Francisco, CA: WestEd Health & Human Development Program for the California Department of Education; 2014 [Google Scholar]
- 15.Patel AI, Bogart LM, Elliott MN, et al. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Prev Chronic Dis. 2011;8(3):A60. [PMC free article] [PubMed] [Google Scholar]
- 16.Patel AI, Bogart LM, Uyeda KE, et al. School site visits for community-based participatory research on healthy eating. Am J Prev Med. 2009;37(6 suppl 1):S300–S306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bogart LM, Uyeda K. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol. 2009;28(4):391–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goh YY, Bogart LM, Sipple-Asher BK, et al. Using community-based participatory research to identify potential interventions to overcome barriers to adolescents’ healthy eating and physical activity. J Behav Med. 2009;32(5):491–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel AI, Bogart LM, Uyeda KE, Rabin A, Schuster MA. Perceptions about availability and adequacy of drinking water in a large California school district. Prev Chronic Dis. 2010;7(2):A39. [PMC free article] [PubMed] [Google Scholar]
- 20.Uyeda K, Bogart LM, Hawes-Dawson J, Schuster MA. Development and implementation of a school-based obesity prevention intervention: lessons learned from community-based participatory research. Prog Community Health Partnersh. 2009;3(3):249–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.California Department of Education 2010-2011 California physical fitness report overall—meeting healthy fitness zone summary of results Los Angeles Unified District. Available at: http://data1.cde.ca.gov/dataquest/PhysFitness/PFTDN/MeetingHFZ2011.aspx?r=0&t=2&y=2010-11&c=19647330000000&n=0000. Accessed June 8, 2015
- 22.Centers for Disease Control and Prevention Data table of BMI-for-age charts. 2001. Available at: www.cdc.gov/growthcharts/html_charts/bmiagerev.htm. Accessed June 8, 2015
- 23.Lumeng JC, Kaciroti N, Sturza J, et al. Changes in body mass index associated with head start participation. Pediatrics. 2015;135(2). Available at: www.pediatrics.org/cgi/content/full/135/2/e449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schuster MA, Elliott MN, Bogart LM, et al. Changes in obesity between fifth and tenth grades: a longitudinal study in three metropolitan areas. Pediatrics. 2014;134(6):1051–1058 [DOI] [PubMed] [Google Scholar]
- 25.Kreft I, de Leeuw J. Introducing Multilevel Modeling. Thousand Oaks, CA: SAGE Publications; 1998 [Google Scholar]