Abstract
Objective:
Although CT scans provide great medical benefits, concerns have been raised about the magnitude of possible associated cancer risk, particularly in children who are more sensitive to radiation than adults. Unnecessary high doses during CT examinations can also be delivered to children, if the scan parameters are not adjusted for patient age and size. We conducted the first survey to directly assess the trends in CT scan parameters and doses for paediatric CT scans performed in Great Britain between 1978 and 2008.
Methods:
We retrieved 1073 CT film sets from 36 hospitals. The patients were 0–19 years old, and CT scans were conducted between 1978 and 2008. We extracted scan parameters from each film including tube current–time product [milliampere seconds (mAs)], tube potential [peak kilovoltage (kVp)] and manufacturer and model of the CT scanner. We estimated the mean mAs for head and trunk (chest and abdomen/pelvis) scans, according to patient age (0–4, 5–9, 10–14 and 15–19 years) and scan year (<1990, 1990–1994, 1995–1999 and ≥2000), and then derived the volumetric CT dose index and estimated organ doses.
Results:
For head CT scans, mean mAs decreased by about 47% on average from before 1990 to after 2000, with the decrease starting around 1990. The mean mAs for head CTs did not vary with age before 1990, whereas slightly lower mAs values were used for younger patients after 1990. Similar declines in mAs were observed for trunk CTs: a 46% decline on an average from before 1990 to after 2000. Although mean mAs for trunk CTs did not vary with age before 1990, the value varied markedly by age, from 63 mAs for age 0–4 years compared with 315 mAs for those aged >15 years after 2000. No material changes in kVp were found. Estimated brain-absorbed dose from head CT scans decreased from 62 mGy before 1990 to approximately 30 mGy after 2000. For chest CT scans, the lung dose to children aged 0–4 years decreased from 28 mGy before 1990 to 4 mGy after 2000.
Conclusion:
We found that mAs for head and trunk CTs was approximately halved starting around 1990, and age-specific mAs was generally used for paediatric scans after this date. These changes will have substantially reduced the radiation exposure to children from CT scans in Great Britain.
Advances in knowledge:
The study shows that mAs and major organ doses for paediatric CT scans in Great Britain began to decrease around 1990.
INTRODUCTION
The number of CT scans has increased dramatically over the last three decades, resulting in a marked increase in the per capita dose in countries like the UK and USA.1 Even though CT examinations provide great medical benefits, concerns have been raised about the magnitude of possible associated cancer risk, particularly in children who are more sensitive to radiation than adults.2 Recently, retrospective epidemiological studies based on large populations of children exposed to CT radiation reported the first direct evidence of a possible increased risk of cancer solely from CT examinations.3–7 Concerns have also been raised about unnecessary high doses during CT examinations, if CT parameters are not adjusted for patient age and size.8
National surveys of CT protocols in hospitals across the UK were conducted in 1989,9 200310 and 201111 by Public Health England (PHE) (formerly National Radiological Protection Board and Health Protection Agency). The 1989 survey reported the technical scan parameters typically used for the standard scan protocols for adults. The 2003 survey reported technical parameters as well as volumetric CT dose index (CTDIvol) for paediatric and adult protocols. They suggested that technical parameters had been changed to reduce doses but that actual practice may still vary from the protocols because the surveys were based on standard protocols submitted from hospitals. More recently, the 2011 survey collected the CTDIvol and dose–length product for 47,000 individual patients from 182 scanners and found that typical CTDIvol has remained relatively constant relative to the 2003 survey but that typical values of dose–length product have increased by some tens of percent. Although three surveys provided three anchor values for 1989, 2003 and 2011, no information was available between 1989 and 2003 to evaluate when the changes occurred.
We previously conducted a retrospective cohort study in the UK to evaluate the cancer risks after CT scans in 1,80,000 children.4 In that study, we collected CT films (photographic films of tomographic images) from a subset of participating hospitals to estimate organ-specific radiation doses for the study population. In the present study, we used these films to directly assess the trends in CT scan parameters and radiation doses for children in Great Britain between 1978 and 2008.
METHODS AND MATERIALS
Data abstraction
We retrieved 1073 CT film sets from 36 hospitals in Great Britain. The patients were 0–19 years old at the time of the CT scans, which were conducted between 1978 and 2008. Patient age, gender, scan type and scan year were available from the radiology information system data from the hospitals. We manually extracted the following parameters from CT films or protocol page (if available): the manufacturer and model of CT scanners, tube current–time product per rotation [in milliampere seconds (mAs)] and tube potential [in peak kilovoltage (kVp)]. If tube current modulation was used (variable mAs for each slice), then we extracted multiple mAs values and calculated the mean. To evaluate the trends in mAs, we plotted mAs against scan years using locally weighted scatter-plot smoothing.12
We also performed more formal tests for departures from log-linear trends in mAs. A linear model was fitted to ln [mAs], so that for record (individual) , the mAs was modelled by:
| (1) |
where is independent and identically distributed . This equation models the log-linear trend in mAs (the terms), allowing for a change in the slope of this trend at calendar year (given by the term). The evaluation of departures of from 0 examines the presence of change in the slope of the calendar year trend at that point. Values of of 1990, 1991, …, 2000 were evaluated. The model was fitted separately to head and trunk scans. Analysis of variance13 was carried out using R (R Project v. 3.1.1, 2014); in particular F tests were used to test for discontinuities in the linear slope in the calendar year trend.
Derivation of volumetric CT dose index
Although mAs is linearly proportional to the organ-absorbed dose received by patients for a given beam spectrum, patient size and scan region, it cannot be directly interpreted as dose. To evaluate a more relevant dosimetric quantity, CTDIvol [in milligray] was derived from scan parameters coupled with the library of normalized CTDIw (nCTDIw; mGy/100 mAs),14 as described in the following equation:
| (2) |
where and are measurements conducted at the centre and periphery of the CT dose index (CTDI) phantom, respectively, by using a 100-mm-long ionization chamber.
| (3) |
where is the CTDIw normalized to 100 mAs for a given scanner's make and model and X-ray spectrum (mGy/100 mAs); is the product of the tube current (I) and the single rotation time (t) (mAs).
The library consists of a matrix of CTDIw normalized to 100 mAs (nCTDIw) for different kVp values (80, 100, 120 and 140 kVp), head and body CTDI phantoms and 162 scanner models from 8 major scanner manufacturers. A normalized CTDIw value was selected from the dose library using the information of the manufacturer and model of scanners and kVp for each CT scan, assuming a standard nominal beam collimation of 10 mm. We excluded the scans using narrow collimation (e.g. high-resolution chest CT) from the analysis because the CTDIw for those collimations would be much greater than the value for the collimation of 10 mm. The selected nCTDIw based on the head CTDI phantom was used for all types of paediatric CT scans in the present study, except the trunk scans of 15–19-year olds for which nCTDIw values of the body CTDI phantom were used. CTDIw (mGy) was then calculated by using the extracted mAs values based on Equation (3).
Pitch also influences radiation dose on scanners that do not change tube current to compensate, but it was not routinely recorded on the films. For CTDIvol and dose estimation, we derived values for pitch from the PHE 1989 survey9 for the time period before 2000 and directly used the values reported from the PHE 2003 surveys10 for the scans after 2000. In head scans, the pitch was assumed to be 1.0. A pitch of 1.5 was assumed for all other trunk scans, except for trunk scans conducted after 2000 (pitch = 1.4). CTDIvol (mGy) was then calculated using Equation (3) for different age groups, scan years and scan types.
Calculation of organ doses
Based on the CTDIvol values described in the previous section, we estimated organ-absorbed doses according to age group, scan year and scan types. We adopted the CTDIvol-to-organ dose conversion coefficients (mGy mGy−1) that we previously published.15 The dose conversion coefficients were calculated using a series of paediatric and adult computational human phantoms16 coupled with a Monte Carlo transport simulation of a reference CT scanner, and then were validated using physical human phantoms.17 The most up-to-date dose–response functions were used to calculate the red bone marrow dose.18
We retrieved age- and scan-type-dependent dose conversion coefficients from the pre-calculated dose library that was then multiplied by the CTDIvol described in the section Derivation of CTDIvol to calculate organ doses. We used general scan ranges for head, chest and abdomen/pelvis scans.19 Since the dose conversion coefficients were calculated for 0-, 1-, 5-, 10- and 15-year-old phantoms, we derived the conversion coefficients for the 0–4-year age group by averaging 0- and 5-year-old data, 5–9-year age group from 5- to 10-year-old data, 10–14-year age group from 10- to 15-year-old data and 15–19-year age group from 15-year-old to adult data. We calculated brain and red bone marrow doses for the head scan, lung and breast doses for the chest scan and stomach and red bone marrow doses for the abdomen/pelvis scan.
RESULTS
Tube current–time product (mAs)
Among the 1073 films collected from hospitals, mAs was available from 84% of the films (n = 899). Of these 71% (n = 637) were head scans and 17% (n = 157) were trunk scans.
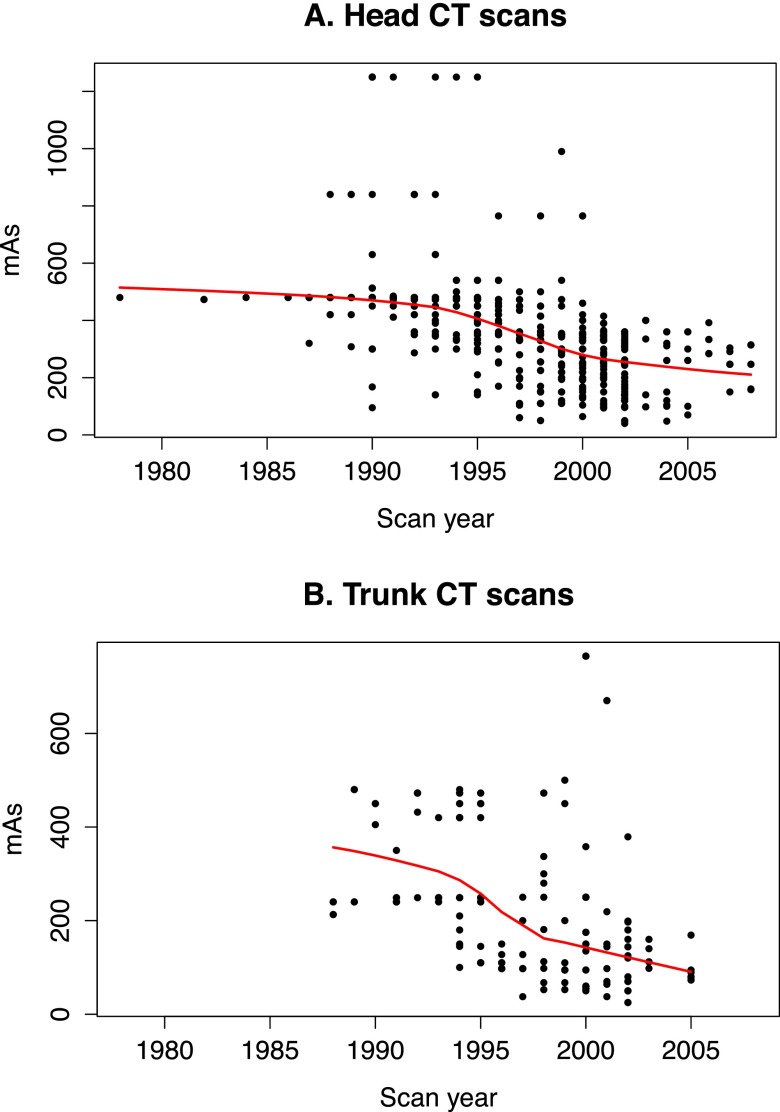
For head CT scans, the mean mAs decreased by about 47% on average from before 1990 to after 2000, with the decrease starting around 1990 (Table 1, Figure 1a). The largest decrease was observed in the youngest age group (0–4 years). The mean mAs for the head CT did not vary with age before 1990, whereas slightly lower mAs values were used for younger patients after 1990: 217 mAs for 0–4 years of age and 261 mAs for >15 years of age after 2000.
Table 1.
Tube current-time-product (mAs) for different age groups, scan years and scan types
| Age (years) | Scan year | Head CT scan |
Trunk CT scan |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | n | Min | Max | Mean | n | Min | Max | ||
| 0–4 | <1990 | 499 | 44 | 308 | 840 | 213 | 2 | 213 | 213 |
| 1990–1994 | 507 | 85 | 300 | 1250 | 282 | 9 | 145 | 473 | |
| 1995–1999 | 341 | 57 | 104 | 765 | 139 | 16 | 38 | 250 | |
| >=2000 | 217 | 51 | 64 | 765 | 63 | 5 | 25 | 120 | |
| 5–9 | <1990 | 469 | 25 | 320 | 480 | 240 | 4 | 240 | 240 |
| 1990–1994 | 462 | 54 | 95 | 1250 | 288 | 14 | 100 | 480 | |
| 1995–1999 | 372 | 36 | 50 | 1250 | 206 | 13 | 110 | 473 | |
| >=2000 | 271 | 44 | 48 | 765 | 170 | 15 | 38 | 765 | |
| 10–14 | <1990 | 480 | 15 | 480 | 480 | 480 | 2 | 480 | 480 |
| 1990–1994 | 505 | 18 | 350 | 840 | 389 | 7 | 249 | 473 | |
| 1995–1999 | 363 | 34 | 110 | 765 | 352 | 6 | 200 | 473 | |
| >=2000 | 274 | 88 | 40 | 990 | 157 | 33 | 50 | 500 | |
| 15–19 | <1990 | – | – | – | – | – | – | – | – |
| 1990–1994 | 492 | 21 | 300 | 840 | 409 | 13 | 240 | 473 | |
| 1995–1999 | 325 | 17 | 110 | 500 | 277 | 7 | 98 | 473 | |
| >=2000 | 261 | 48 | 50 | 360 | 315 | 11 | 98 | 765 | |
Max, maximum; min, minimum.
Figure 1.
Change in the milliampere seconds (mAs) value over the scan year for (a) head and (b) trunk CT scans for all ages plotted using the locally weighted scatter-plot smoothing method.
Similar declines in mAs were seen over time for trunk CT scans. From before 1990 to after 2000, the mean mAs decreased by about 46%, starting around 1990 (Table 1, Figure 1b). The decline was less for the 15–19-year olds (23%) than for the youngest children (70% for 0–4-year olds). After 2000, the mean mAs for trunk CT scans varied markedly by age from 63 mAs for 0–4 years of age compared with 315 mAs for >15 years of age.
Supporting Figure 1a, the results of Table 2 show that for head scans, there were significant changes in the calendar year trend in the early 1990s, with the trend with calendar time becoming more negative after the chosen break point about then. In the late 1990s, there is a change in the linear calendar year trend in the opposite direction (i.e. with the trend in calendar year becoming less negative), again supporting Figure 1a. Supporting Figure 1b, Table 2 shows that there are discontinuities in the linear trend for trunk CT scans for all years within the interval 1990–2000.
Table 2.
Change in the log-linear trend of milliampere seconds with calendar year, in regression using Equation (1), adjusted for age and sex, separately for head and trunk CT scans
| Year of break in trend with calendar year (yearbreak) | Change in trend (year−1) at calendar year yearbreak, α2 (year−1) (+95% CI) | p-value for heterogeneity in calendar year trend |
|---|---|---|
| Head CT scans | ||
| 1990 | −0.085 (−0.132, −0.039) | 0.0003 |
| 1991 | −0.077 (−0.115, −0.038) | <0.0001 |
| 1992 | −0.064 (−0.096, −0.032) | 0.0001 |
| 1993 | −0.053 (−0.080, −0.025) | 0.0002 |
| 1994 | −0.042 (−0.067, −0.016) | 0.0012 |
| 1995 | −0.029 (−0.053, −0.006) | 0.0151 |
| 1996 | −0.015 (−0.038, 0.008) | 0.2000 |
| 1997 | 0.001 (−0.022, 0.023) | 0.9617 |
| 1998 | 0.018 (−0.004, 0.041) | 0.1142 |
| 1999 | 0.031 (0.008, 0.055) | 0.0095 |
| 2000 | 0.043 (0.018, 0.067) | 0.0007 |
| Trunk CT scans | ||
| 1990 | −0.563 (−0.925, −0.202) | 0.0024 |
| 1991 | −0.320 (−0.529, −0.119) | 0.0028 |
| 1992 | −0.221 (−0.365, −0.078) | 0.0026 |
| 1993 | −0.167 (−0.276, −0.058) | 0.0028 |
| 1994 | −0.132 (−0.220, −0.043) | 0.0038 |
| 1995 | −0.112 (−0.189, −0.036) | 0.0042 |
| 1996 | −0.107 (−0.182, −0.033) | 0.0051 |
| 1997 | −0.103 (−0.176, −0.029) | 0.0068 |
| 1998 | −0.110 (−0.182, −0.037) | 0.0032 |
| 1999 | −0.119 (−0.191, −0.048) | 0.0012 |
| 2000 | −0.130 (−0.203, −0.057) | 0.0005 |
CI, confidence interval.
Tube potential (kVp)
The tube potential (kVp) was available for 90% (n = 962) of the CT films. A tube potential of 120 kVp was used for the majority of head (76%), chest (73%) and abdomen/pelvis (83%) scans. More variation in kVp was observed in the head scans with 80–140 kVp than in the trunk scans with 110–137 kVp. The variation of kVp in abdomen/pelvis scans (120–130 kVp) was less than that in other scan types. No clear trend in kVp was observed either over calendar year or by patient age.
Volumetric CT dose index and organ dose
The scanner manufacturer and model, kVp and mAs that are required to calculate CTDIvol were available from 794 (74%) of the 1073 CT films. Because CTDIvol is linearly proportional to mAs [Equation (3)], similar declines in CTDIvol were noted over calendar time as for mAs for all scan types. For head scans, the CTDIvol values for patients scanned before 1990 were about two times greater than those of more recent years (after 2000) (Table 3). After 2000, the CTDIvol for head CT scans in the 15–19-year age group is slightly greater than that for 0–4-year-old patients (43 vs 33 mGy). For trunk scans, the CTDIvol decreased eightfold from before 1990 to after 2000 for the youngest patients (0–4 years old) from 32 to 4 mGy. Declines were smaller for the older children, but the sample size was very small for some of these estimates (Table 3).
Table 3.
Volumetric CT dose index (CTDIvol) derived from scanner model, milliampere seconds and peak kilovoltage for different age groups, scan years and scan types
| Scan year | Age (years) | Head CT scan |
Trunk CT scan |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | n | Min | Max | Mean | n | Min | Max | ||
| <1990 | All ages | 71 | 59 | 35 | 123 | 32 | 4 | 16 | 47 |
| 1990–1999 | All ages | 57 | 288 | 7 | 123 | 24 | 73 | 4 | 41 |
| ≥2000 | 0–4 | 33 | 48 | 8 | 115 | 4 | 4 | 2 | 6 |
| 5–9 | 39 | 40 | 12 | 115 | 18 | 9 | 4 | 41 | |
| 10–14 | 47 | 86 | 2 | 142 | 17 | 32 | 5 | 39 | |
| 15–19 | 43 | 46 | 10 | 76 | 14 | 11 | 5 | 28 | |
Max, maximum; min, minimum.
In terms of estimated organ doses (Table 4), the largest organ doses were shown in the brain (62 mGy before 1990) for head scans and the lung (28 mGy before 1990) for trunk scans. After 2000, the brain and lung doses decreased by about 50% and 86%, respectively, for 0–4-year olds compared with those before 1990. The bone marrow dose in head scans was about one-third of the brain dose.
Table 4.
Organ-absorbed doses (mGy) calculated for different age groups, scan year and scan types
| Scan year | Age (years) | Head CT scan |
Chest CT scan |
Abdomen/pelvis CT scan |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brain |
Bone marrow |
Lung |
Breast |
Stomach |
Bone marrow |
||||||||||||||
| Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | Mean | Min | Max | ||
| <1990 | All ages | 62 | 31 | 108 | 16 | 8 | 28 | 28 | 15 | 42 | 25 | 13 | 37 | 28 | 14 | 41 | 9 | 5 | 14 |
| 1990–1999 | All ages | 50 | 6 | 108 | 13 | 2 | 28 | 22 | 3 | 36 | 19 | 3 | 32 | 21 | 3 | 36 | 7 | 1 | 12 |
| ≥2000 | 0–4 | 31 | 8 | 109 | 10 | 3 | 36 | 4 | 2 | 6 | 3 | 2 | 5 | 3 | 2 | 5 | 1 | 1 | 2 |
| 5–9 | 33 | 10 | 97 | 9 | 3 | 28 | 16 | 3 | 36 | 13 | 3 | 30 | 16 | 3 | 35 | 5 | 1 | 10 | |
| 10–14 | 38 | 2 | 114 | 7 | 0 | 20 | 13 | 4 | 30 | 11 | 3 | 26 | 13 | 4 | 29 | 5 | 1 | 11 | |
| 15–19 | 33 | 8 | 59 | 5 | 1 | 9 | 10 | 3 | 19 | 9 | 3 | 18 | 9 | 3 | 18 | 4 | 1 | 8 | |
Max, maximum; Min, minimum.
DISCUSSION
We conducted the first survey to directly assess the trends in CT scan parameters and doses for paediatric CT scans performed between 1978 and 2008, by retrieving 1073 CT film sets from 36 hospitals in Great Britain. We found that mean mAs, CTDIvol and organ doses decreased by about 50% for scans performed before 1990 vs after 2000, with the decrease starting around 1990. This seems to be in line with the finding from the 2003 PHE survey10 that the overall levels of exposure in 2003 were in general lower by about 40% than the previous 1989 UK survey data for adult patients.
We compared our CTDIvol values from the CT films with those derived from the PHE protocol surveys (Table 5). In general, our estimates for CT scans both before 1990 and after 2000 showed broad agreement with the mean CTDIvol from the 19899 and 200310 surveys, except for head CT scans before 1990 (71 vs 56 mGy). The small sample size for trunk CT scans after 2000 in our study means that these differences should be interpreted with caution. We also compared our CTDIvol with the data from the US Food and Drug Administration (FDA) for adults20 and from Germany for paediatric CT scans,21 conducted in 2000 and 2005–2006, respectively. Our CTDIvol (for >15 years of age) for CT scans after 2000 was smaller by 31% and 4% for head and trunk scans, respectively, than that for those from the US FDA (CTDIvol for the head scan = 62 mGy and CTDIvol for the trunk scan = 17 mGy). When compared with the German protocol survey for children (2005–2006), our CTDIvol values for CT scans performed after 2000 for ages 0–4, 5–9, 10–14 and >15 years for head scans were smaller than those in the German data by up to 28%. Our CTDIvol for trunk scans after 2000 for 0–4 and 5–9 years of age were 21% smaller and 66% greater than that in the German data, respectively (5 and 11 mGy). No data for body scans of children >10 years of age are available from the German survey. In general, we found that the CTDIvol from paediatric CT scan practices in the UK was lower than that reported from the US FDA and German surveys.
Table 5.
Comparison of volumetric CT dose index (mGy) between our study and the Public Health England (PHE) survey for before 1990 and after 2000
| Age (year) | Head CT scan |
Trunk CT scan |
||
|---|---|---|---|---|
| CT film < 1990 | PHE 1989 | CT film < 1990 | PHE 1989 | |
| All ages | 71 | 56 | 32 | 27 |
| Age (years) | Head CT scan |
Trunk CT scan |
||
| CT film > 2000 | PHE 2003 | CT film > 2000 | PHE 2003a | |
| 0–4 | 33 | 30 | 4 | 11 |
| 5–9 | 39 | 40 | 18 | 13 |
| 10–14 | 47 | 50 | 17 | 17 |
| >15 | 43 | 56 | 14 | 10 |
The data are for chest scan.
Compared with the existing nationwide surveys9–11 of hospital protocols, the advantage of our study is that we directly assessed the trends in CT scan parameters for paediatric CT scans in Great Britain by extracting CT films from hospitals and covered the whole time period to assess when the practice actually changed. We also estimated CTDIvol and radiation doses to major organs by using age-dependent organ dose conversion coefficients based on realistic computational human models. However, it should be noted that our study has a couple of limitations. Before the early 2000s, the picture archiving and communication system was not available and it was time consuming to abstract data from printed CT films. In addition, many films had been destroyed or were unavailable, which reduced our sample size, particularly for trunk CT scans in some age groups. Also, some parameters that will impact the CTDIvol and organ dose such as pitch were not available from the films, so that we had to use the data reported from the PHE surveys. However, these particular parameters were unlikely to have been routinely changed over time, and these survey estimates should be broadly applicable. It must be noted that the assumption on the collimation of 10 mm may provide uncertainty, even though we removed narrow collimation scans (e.g. high-resolution chest scan) from our study. We used average mAs for the tube current modulation scans (15% of total scans). The actual doses to the lung and breast in chest scans will be smaller (root-mean-square error up to 10%)22 and the red bone marrow dose in abdomen/pelvis scans will be slightly greater than the values in Table 4. Finally, it must be noted that the measurement errors in the normalized CTDIw library14 we used to reconstruct CTDIvol may cause uncertainty in the CTDIvol values that we derived.
Reduction of mAs has been reported as the simplest way to reduce radiation dose to the patient.23,24 Although some hospitals implemented scan protocols in which mAs was varied within scan regions to account for variable patient thickness and density as early as the mid-1980s, we found that such techniques were not in widespread use until the mid-1990s. More recent scanners feature fully automatic tube current modulation,25 with a different mAs being used for each rotation, determined from the planning “scout” image or from the preceding rotation. Scan protocols, in which mAs was adjusted for patient age, were also implemented after the early 1990s. Further innovations include improved detector efficiency, more dose-efficient reconstruction techniques including iterative methods and improved beam-shaping filters. Lowering tube potential (kVp) also has been suggested as another dose-reduction method,23,24 but did not seem to be widely employed in the CT films we collected.
In 1992, the PHE published their national guidance, “Protection of the patient in X-ray CT”.26 In the 1990s, the European Commission also began working on European guidelines for better practice in CT scans,27 which followed the Guidelines of the German Federal Chamber of Physicians on Quality Assurance in CT published in 1992.28 It is possible that changes in the CT radiation safety culture might have occurred in the UK during the 1990s, coinciding with our observation of dose reduction in the present study. The Image Gently campaign29 has improved awareness of the radiation hazards of CT. However, it is noteworthy that in the UK, there was a reduction in paediatric CT dose about 15 years before the launch of Image Gently.
CONCLUSION
We evaluated the temporal trends and age dependency in mAs, CTDIvol and selected organ doses based on scan parameters manually extracted from 1073 paediatric and adolescent CT films, taken from hospitals in Great Britain. We found that mean mAs for paediatric CT scans decreased by 50% for scans performed before 1990 vs after 2000, and this decline started around 1990. Mean mAs did not vary with patient age before 1990, whereas lower mAs values began to be used for younger age patients after 1990, particularly for CT scans of the trunk. These changes will substantially reduce the radiation exposure to children from CT scans in Great Britain.
FUNDING
This work was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Division of Cancer Epidemiology and Genetics.
Contributor Information
Choonsik Lee, Email: leechoonsik@mail.nih.gov.
Mark S Pearce, Email: mark.pearce@newcastle.ac.uk.
Jane A Salotti, Email: jane.salotti@newcastle.ac.uk.
Richard W Harbron, Email: richard.hardy@newcastle.ac.uk.
Mark P Little, Email: mark.little@nih.gov.
Kieran McHugh, Email: Kieran.McHugh@gosh.nhs.uk.
Claire-Louise Chapple, Email: claire.chapple@nuth.nhs.uk.
Amy Berrington de Gonzalez, Email: berringtona@mail.nih.gov.
REFERENCES
- 1.Mettler FA, Bhargavan M, Faulkner K, Gilley DB, Gray JE, Ibbott GS, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950–2007. Radiology 2009; 253: 520. doi: 10.1148/radiol.2532082010 [DOI] [PubMed] [Google Scholar]
- 2.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation. Washington, DC: National Academies Press; 2006. pp. 424. [PubMed] [Google Scholar]
- 3.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013; 346: 2360. doi: 10.1136/bmj.f2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505. doi: 10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang WY, Muo CH, Lin CY, Jen YM, Yang MH, Lin JC, et al. Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer 2014; 110: 1–7. doi: 10.1038/bjc.2014.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Journy N, Rehel JL, Ducou Le Pointe H, Lee C, Brisse H, Chateil JF, et al. Are the studies on cancer risk from CT scans biased by indication? elements of answer from a large-scale cohort study in France. Br J Cancer 2015; 112: 185–93. doi: 10.1038/bjc.2014.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krille L, Dreger S, Schindel R, Albrecht T, Asmussen M, Barkhausen J, et al. Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys 2015; 54: 1–12. doi: 10.1007/s00411-014-0580-3 [DOI] [PubMed] [Google Scholar]
- 8.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001; 176: 289–96. doi: 10.2214/ajr.176.2.1760289 [DOI] [PubMed] [Google Scholar]
- 9.Shrimpton PC, Hart D, Hillier MC, Wall BF, Le Heron JC, Faulkner K. Survey of CT practice in the UK. Part 2: dosimetric aspects. Chilton, UK: National Radiological Protection Board; 1991. pp. 165–72. Report number: NRPB-R249. [Google Scholar]
- 10.Shrimpton PC, Hillier MC, Lewis MA, Dunn M. Doses from computed tomography (CT) examinations in the UK: 2003 review. Chilton, UK: National Radiological Protection Board; 2005. pp. 1–93. Report number: NRPB-W67. [Google Scholar]
- 11.Shrimpton PC, Hillier MC, Meeson S, Golding SJ. Doses from computed tomography (CT) examinations in the UK: 2011 review. Chilton, UK: Public Health England; 2014. [Google Scholar]
- 12.Cleveland WS. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc 1979; 74: 829–36. doi: 10.1080/01621459.1979.10481038 [DOI] [Google Scholar]
- 13.Rao CR. Linear statistical inference and its applications. 2nd edn. USA: John Wiley & Sons, Inc.; 2002. [Google Scholar]
- 14.Lee E, Lamart S, Little MP, Lee C. Database of normalised computed tomography dose index for retrospective CT dosimetry. J Radiol Prot 2014; 34: 363–88. doi: 10.1088/0952-4746/34/2/363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee C, Kim KP, Long DJ, Bolch WE. Organ doses for reference pediatric and adolescent patients undergoing computed tomography estimated by Monte Carlo simulation. Med Phys 2012; 39: 2129–46. doi: 10.1118/1.3693052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee C, Lodwick D, Hurtado J, Pafundi D, Williams JL, Bolch WE. The UF family of reference hybrid phantoms for computational radiation dosimetry. Phys Med Biol 2010; 55: 339–63. doi: 10.1088/0031-9155/55/2/002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Long DJ, Lee C, Tien C, Fisher R, Hoerner MR, Hintenlang D, et al. Monte Carlo simulations of adult and pediatric computed tomography exams: validation studies of organ doses with physical phantoms. Med Phys 2013; 40: 13901. doi: 10.1118/1.4771934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson PB, Bahadori AA, Eckerman KF, Lee C, Bolch WE. Response functions for computing absorbed dose to skeletal tissues from photon irradiation—an update. Phys Med Biol 2011; 56: 2347–65. doi: 10.1088/0031-9155/56/8/002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee C, Kim KP, Long D, Fisher R, Tien C, Simon SL, et al. Organ doses for reference adult male and female undergoing computed tomography estimated by Monte Carlo simulations. Med Phys 2011; 38: 1196–206. doi: 10.1118/1.3544658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stern SH. National evaluation of X-ray trends (NEXT): tabulation of graphical summary of 2000 survey of computed tomography. Washington, DC: Food and Drug Administration; 2007. [Google Scholar]
- 21.Galanski M, Nagel HD, Stamm G. Paediatric CT exposure practice in the federal Republic of Germany: results of a nation-wide survey in 2005/06. Hannover, Germany: 2005. pp. 56. [Google Scholar]
- 22.Khatonabadi M, Zhang D, Mathieu K, Kim HJ, Lu P, Cody D, et al. A comparison of methods to estimate organ doses in CT when utilizing approximations to the tube current modulation function. Med Phys 2012; 39: 5212–28. doi: 10.1118/1.4736807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kubo T, Ohno Y, Kauczor HU, Hatabu H. Radiation dose reduction in chest CT–review of available options. Eur J Radiol 2014; 83: 1953–61. doi: 10.1016/j.ejrad.2014.06.033 [DOI] [PubMed] [Google Scholar]
- 24.McCollough CH, Bruesewitz MR, Kofler JM, Jr. CT dose reduction and dose management tools: overview of available options. Radiographics 2006; 26: 503–12. doi: 10.1148/rg.262055138 [DOI] [PubMed] [Google Scholar]
- 25.Gies M, Kalender WA, Wolf H, Suess C. Dose reduction in CT by anatomically adapted tube current modulation. I. Simulation studies. Med Phys 1999; 26: 2235–47. doi: 10.1118/1.598779 [DOI] [PubMed] [Google Scholar]
- 26.NRPB. Protection of the patient in X-ray computed tomography. 1992. Report number: Vol. 3, number 4. Chilton, UK. [Google Scholar]
- 27.Menzel H, Schibilla H, Teunen D. European guidelines on quality criteria for computed tomography. Luxembourg: European Commission; 2000. [DOI] [PubMed] [Google Scholar]
- 28.Leitlinien der Bundesärztekammer zur Qualitätssicherung in der Computertomographie (English translation: Guidelines of the federal chamber of physicians on quality assurance in computed tomography. German Medical Association; 1992. Report number: CEC XII/354/92-EN, Dt. Ärztebl. 89: Heft 49. [Google Scholar]
- 29.Goske MJ, Applegate KE, Boylan J, Butler PF, Callahan MJ, Coley BD, et al. The image gently campaign: working together to change practice. AJR Am J Roentgenol 2008; 190: 273–4. doi: 10.2214/AJR.07.3526 [DOI] [PubMed] [Google Scholar]