Abstract
Objective:
The purpose of this study is to evaluate the distribution of end plate oedema in different types of Modic change especially in mixed type and to analyze the presence of end plate sclerosis in various types of Modic change.
Materials and methods:
276 patients with low back pain were scanned with 1.5-T MRI. Three radiologists assessed the MR images by T1 weighted, T2 weighted and fat-saturation T2 weighted sequences and classified them according to the Modic changes. Pure oedematous end plate signal changes were classified as Modic Type I; pure fatty end plate changes were classified as Modic Type II; and pure sclerotic end plate changes as Modic Type III. A mixed feature of both Types I and II with predominant oedematous signal change is classified as Modic I–II, and a mixture of Types I and II with predominant fatty change is classified as Modic II–I. Thus, the mixed types can further be subdivided into seven subtypes: Types I–II, Types II–I, Types I–III, Types III–I, Types II–III, Types III–II and Types I–III. During the same period, 52 of 276 patients who underwent CT and MRI were retrospectively reviewed to determine end plate sclerosis.
Results:
(1) End plate oedema: of the 2760 end plates (276 patients) examined, 302 end plates showed Modic changes, of which 82 end plates showed mixed Modic changes. The mixed Modic changes contain 92.7% of oedematous changes. The mixed types especially Types I–II and Types II–I made up the majority of end plate oedematous changes. (2) End plate sclerosis: 52 of 276 patients were examined by both MRI and CT. Of the 520 end plates, 93 end plates showed Modic changes, of which 34 end plates have shown sclerotic changes in CT images. 11.8% of 34 end plates have shown Modic Type I, 20.6% of 34 end plates have shown Modic Type II, 2.9% of 34 end plates have shown Modic Type III and 64.7% of 34 end plates have shown mixed Modic type.
Conclusion:
End plate oedema makes up the majority of mixed types especially Types I–II and Types II–I. The end plate sclerosis on CT images may not just mean Modic Type III but does exist in all types of Modic changes, especially in mixed Modic types, and may reflect vertebral body mineralization rather than change in the bone marrow.
Advances in knowledge:
End plate oedema and end plate sclerosis are present in a large proportion of mixed types.
INTRODUCTION
The signal intensity changes in the the vertebral body bone marrow adjacent to the end plates are commonly seen on MRI. Initially, it was described by Modic et al1,2 who classified them into: (1) Type I that includes low T1 and high T2 signals, (2) Type II with high T1 signal and isointense or slightly hyperintense T2 signal and (3) Type III characterized by low T1 and T2 signals. Type I is considered to be the earliest and most active stage in the process of evolution of end plate changes. The presence of different types of Modic changes within the end plate was later regarded as mixed Modic changes, such as mixed Types I–II and Types II–III.3
Initially, attempts were made to correlate the MRI appearance with clinical symptoms and histological findings. Although the precise clinical evaluation of Modic change is controversial, many authors have reported a correlation between Modic change and chronic low back pain, especially for Modic Type I.4–6 Recent studies show the satisfactory results of lumbar disc replacement in patients with Modic changes. Total disc arthroplasty provides good results in the management of chronic low back pain, and the best clinical improvements were seen to be present in patients with Type I Modic change.7 Hence, it is very important to provide an accurate assessment of classification and distribution of Modic changes, especially in Type I. The purpose of this study was to evaluate the end plate oedema in different types of mixed Modic changes.
It has been suggested that end plate sclerosis exists only in Modic Type III,1,2,8 whereas Modic Type I and Type II have shown no definite correlation with sclerosis in radiographic images. We suspect that Modic Type III might not be the only type with end plate sclerosis. Therefore, the other purpose of this study is to evaluate the presence of end plate sclerosis in different Modic types.
METHODS AND MATERIALS
Participants
276 patients (104 males, 172 females; age 20–68 years; mean age, 47 years) referred to Jiangsu Province Hospital between November 2013 and March 2014 were reviewed. The lumbar vertebrae L1–S1 were examined using 1.5-T MRI. Altogether 2760 end plates were examined. During the same duration, 52 patients (18 males, 34 females; age 32–65 years; mean age, 49 years) who underwent lumbar 64-row multislice CT and 1.5-T MRI were included. Altogether 520 end plates were examined. All the patients met our inclusional criteria, i.e. people with no specific low-back pathology, no fracture, no neoplasia, no spondylolysis, no infectious or rheumatic spinal diseases or no recent history of spinal operative procedures. This study received an approval from our institutional review board.
Imaging method
CT imaging
The CT imaging was performed using a 64-slice CT scanner (Siemens Definition AS) with a detector configuration of 64 × 1.25 mm. A standard lumbar spinal protocol with a tube voltage of 130 kV, tube current with CARE Dose 4D (80–520 mAs) and rotation time of 0.8 s was used. The slice thickness and reconstruction interval were 1.25 and 3 mm, respectively.
MRI
The MRI examination was performed with a 1.5-T scanner (Sigma HDxt Echospeed; GE Healthcare, Milwaukee, WI). Sagittal T2 weighted fast spin echo [repetition time (TR)/echo time (TE), 3000/109), sagittal T1 weighted (T1W) sequences (TR/TE, 640/8.5) and sagittal fat-saturation (FS) T2 weighted (T2W) sequences (TR/TE, 3220/107) were obtained using a matrix of 320 × 224, 320-mm field of view and 4/0.5-mm section thickness/gap. Axial T2 weighted fast spin echo (TR/TE, 2640/118) sequences were obtained using a matrix of 320 × 192, 200-mm field of view and 4/0.5-mm section thickness/gap.
Image analysis
Image evaluation was performed at first by two independent radiologists (one musculoskeletal radiologist with 10 years' of experience and the other musculoskeletal radiologist with 3 years' of experience) who were blinded to clinical data. Each radiologist separately analyzed each set of images. If they had some incompatible results about the classification of Modic changes, a third radiologist (musculoskeletal radiologist with 15 years' of experience) would decide the grade of the classification of Modic changes. The final diagnosis was based on diagnostic concordance by three panelists. The Modic changes were evaluated from MR images. Classification of Modic changes was based on the T1W image (T1WI), T2W image (T2WI) and T2WI-FS MR images. T2WI-FS is much sensitive to identify end plate oedema, thus it is helpful in accurate assessment of Modic Type I. The reviewers assessed the ratio of oedema, assessed fatty and sclerosis signal changes of the end plates on successive slices and graded the end plate signal changes. Pure oedematous end plate signal changes were classified as Modic Type I (Figure 1), pure fatty end plate changes as Modic Type II and pure end plate sclerotic changes as Modic Type III. A mixture of Types I and II but with predominant oedematous signal change (estimated as >50% of oedematous signal changes) is classified as Modic I–II, and a mixture of Types I and II with predominant fatty change (estimated as >50% of fatty signal changes) is classified as Modic II–I (Figure 2). A mixture of Types I and III with predominant oedematous signal change (estimated as >50% of oedematous signal changes) is classified as Modic I–III (Figure 3), and a mixture of Types I and III with predominant sclerotic change (estimated as >50% of sclerotic signal changes) is classified as Modic III–I. A mixture of Types II and III (estimated as >50% of fatty signal changes) with predominant fatty change is classified as Modic II–III; and a mixture of Types II and III with predominant sclerotic change (estimated as >50% of sclerotic signal changes) is classified as Modic III–II. A mixture of end plate oedematous, fatty and sclerotic signal changes were classified as Modic I–II–III.3,9
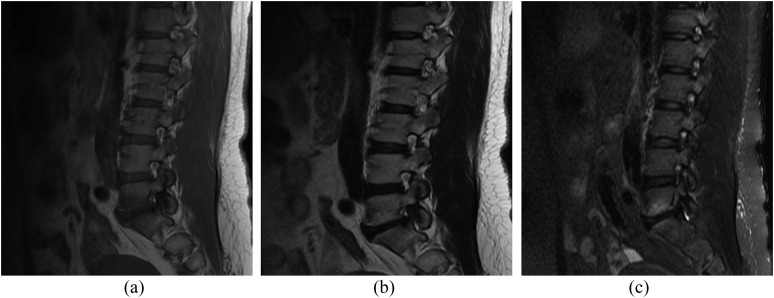
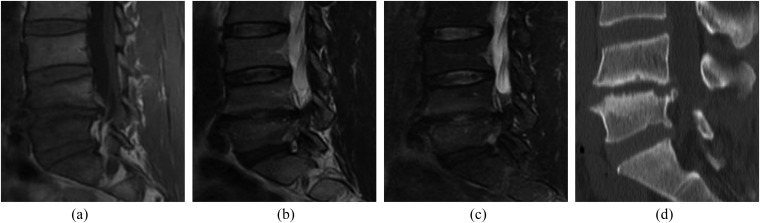
Figure 1.
Pure Modic I signal changes at L5–S1 level. MRI images of Modic change Type I. (a) T1 weighted image, (b) T2 weighted image, (c) T2 weighted image-fat saturation.
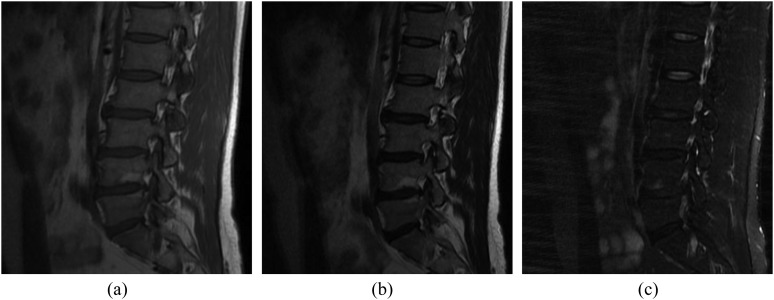
Figure 2.
The mixed Modic signal changes at L4–L5 level (Modic II–I). MRI images of Modic change Types II–I. (a) T1 weighted image, (b) T2 weighted image (T2WI), (c) T2WI-fat saturation. MRI shows a mixture of fatty and oedematous signal changes at L4–L5, with predominant fatty change.
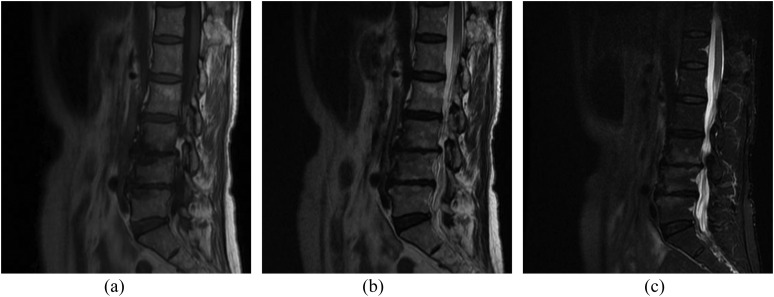
Figure 3.
The mixed Modic signal changes at the L3–L4 level (Modic I–III). MRI images of Modic change Types I–III. (a) T1 weighted image, (b) T2 weighted image (T2WI), (c) T2WI-fat saturation. MRI shows a mixture of oedematous and sclerotic changes at L3–L4, with predominant oedematous change.
Classification of Modic changes in 52 patients were first carried out on the basis of T1WI, T2WI and T2WI-FS MR images. The end plates were graded into Modic I, II, III, I–II, II–I, I–III, III–I, II–III, III–II and I–III, as defined previously. The end plate sclerosis was evaluated from the CT images and was qualitatively analyzed by comparing the sagittally reconstructed CT and MR images at a workstation. The results of end plate sclerosis were defined as yes or no.
RESULTS
End plate oedema
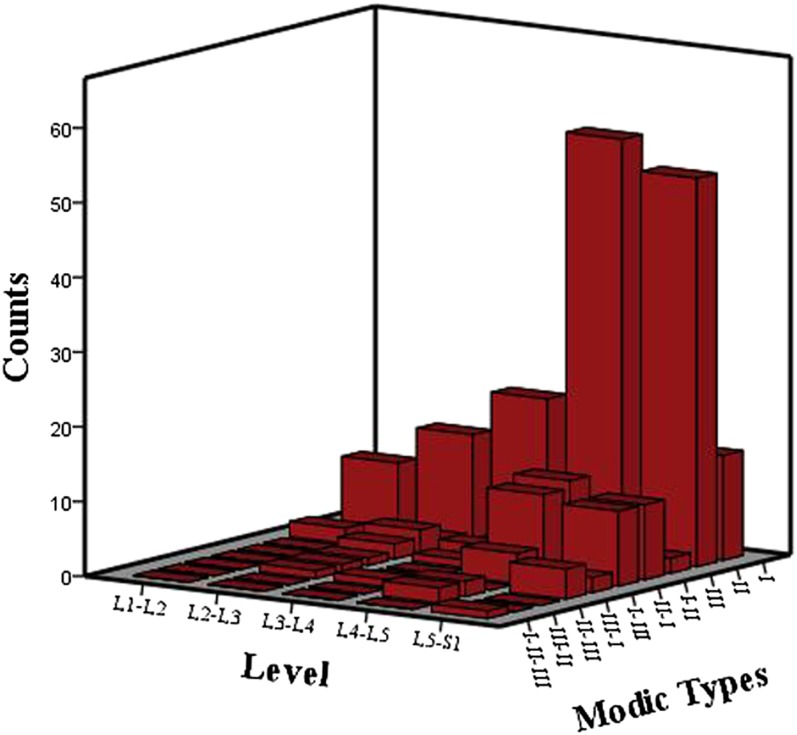
A total of 302 end plates (altogether 2760 end plates) were estimated to present Modic changes and analyzed in this study. Tables 1 and 2 give the overall grades of Modic changes. 92.7% mixed Modic changes showed end plate oedema. End plate oedema made the majority of mixed types, especially Types I–II and Types II–I. Modic changes were found to be most common at L4–L5 and L5–Sl. In this study, 76% of the changes were located at these two levels (Table 3, Figure 4). End plate oedema was also found to be the most common at L4–L5 and L5–S1.
Table 1.
The classification of Modic changes
| Classification | ||||
|---|---|---|---|---|
| Modic I | Modic II | Modic III | Mixed Modic changes | Total |
| 64 | 151 | 5 | 82 | 302 |
| 21.2% | 50.0% | 1.7% | 27.2% | 100% |
Table 2.
The classification of mixed Modic changes
| Classification of mixed Modic changes | |||||||
|---|---|---|---|---|---|---|---|
| Types I–II | Types II–I | Types I–III | Types III–I | Types II–III | Types III–II | Types I–III | Total |
| 39 | 24 | 7 | 5 | 4 | 2 | 1 | 82 |
| 47.6% | 29.3% | 8.5% | 6.1% | 4.9% | 2.4% | 1.2% | 100.0% |
Table 3.
Total number of Modic changes at different levels (n = 302) and the number (proportion) of end plate oedema with changes
| Modic changes | Level |
Total | ||||
|---|---|---|---|---|---|---|
| L1–L2 | L2–L3 | L3–L4 | L4–L5 | L5–S1 | ||
| I | 4 | 3 | 8 | 35 | 14 | 64 |
| II | 9 | 14 | 20 | 56 | 52 | 151 |
| III | 0 | 1 | 1 | 1 | 2 | 5 |
| I–II | 2 | 3 | 2 | 12 | 20 | 39 |
| II–I | 0 | 2 | 1 | 11 | 10 | 24 |
| I–III | 0 | 1 | 0 | 4 | 2 | 7 |
| III–I | 0 | 1 | 0 | 0 | 4 | 5 |
| II–III | 0 | 1 | 0 | 2 | 0 | 4 |
| III–II | 0 | 0 | 0 | 2 | 0 | 2 |
| I–III | 0 | 0 | 0 | 0 | 1 | 1 |
| Total | 15 | 26 | 33 | 123 | 105 | 302 |
| End plate oedema | 6 | 10 | 11 | 62 | 51 | 140 |
Figure 4.
Total number of Modic changes at different levels (n = 302) and the number (proportion) of end plate oedema with changes.
End plate sclerosis
A total of 520 end plates were evaluated by the two radiologists who were blinded to clinical data. Each radiologist separately analyzed each set of images. If they had some incompatible results about the classification of Modic changes, the third radiologist would decide the grade of the classification of Modic changes. Then, the end plate sclerosis was qualitatively analyzed from the sagittally reconstructed CT images by comparing the MR images on one workstation by the two radiologists. The results of end plate sclerosis were defined as yes or no, if the two radiologists had some incompatible results, the third radiologist would decide the results of the end plate sclerosis. The results are given in Table 4. 34 (36.6%) end plates with Modic changes had sclerosis in CT images. But Modic Type III does exist in all types of Modic changes, especially in mixed Modic types. Figures 5 and 6 demonstrate Modic change Type I and Type II in MRI in two different patients with sclerosis in CT.
Table 4.
The results of Modic changes and end plate sclerosis
| Modic changes | Sclerosis |
Total | |
|---|---|---|---|
| CT | |||
| Yes [n (%)] | No [n (%)] | ||
| Type I | 4 (44.4) | 5 (55.6) | 9 (100%) |
| Type II | 7 (14.8) | 47 (85.2) | 54 (100%) |
| Type III | 1 (100) | 0 (0.0) | 1 (100%) |
| Types I–II | 6 (46.2) | 7 (53.8) | 13 (100%) |
| Types II–III | 6 (100) | 0 (0.0) | 6 (100%) |
| Types I–III | 8 (100) | 0 (0.0) | 8 (100%) |
| Types I–III | 2 (100) | 0 (0.0) | 2 (100%) |
| Total | 34 (36.6) | 57 (63.4) | 93 (100%) |
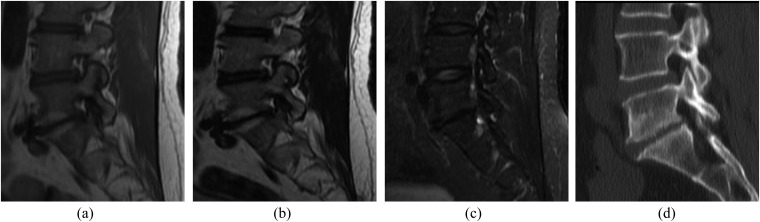
Figure 5.
A patient with a sclerotic Type I Modic change at the L4–L5 disc level. (a) T1 weighted image, (b) T2 weighted image (T2WI), (c) T2WI-fat saturation. Pure Modic I signal changes at the L4–L5 disc level. (d) Sagittal reconstructed CT images show sclerosis at the upper and lower end plates of L4–L5.
Figure 6.
A patient with a sclerotic Type II Modic change at the L5–S1 disc level. (a) T1 weighted image, (b) T2 weighted image (T2WI), (c) T2WI-fat saturation. Pure Modic II signal changes at the L5–S1 disc level. (d) Sagittal reconstructed CT images show sclerosis at the upper and lower end plate of L5–S1.
DISCUSSION
The cartilaginous end plate consists of a thin layer of hyaline cartilage between the disc and the vertebral bodies. It has an average thickness of about 0.5 mm and is generally thin at the region of the nucleus pulposus. Modic changes are end plate lesions adjacent to degenerative lumbar intervertebral discs.1,2
Modic changes were identified in 20–50% of patients with low back pain, and their incidence increased with age.6 The Modic classification is constant and reliable in nature, hence several authors have made an attempt to correlate Modic changes with clinical outcomes. Kjaer et al10 stated that Modic changes played a major role in the degenerative process around the disc in relation to the history of low-back pain and clinical findings. Biological findings share a similar relationship with the clinical inflammatory profile. Reports of patients with chronic low back pain and Modic Type I changes have been reported with increased levels of C-reactive protein in the serum and increased expression of tumour necrosis factor alpha in vertebral end plates.11 Modic Type I change is considered to be the earliest and most active stage in the process of evolution of end plate changes. Weishaupt et al12 have demonstrated that Modic Type II changes can be much painful; however, being a more quiescent stage in the process of evolution of end plate changes, Modic Type II can be reasonably expected to produce less pain than Modic Type I;13 hence, it is very important to give an accurate assessment of classification and distribution of Modic changes, especially the end plate oedema. In this study, we used T1WI, T2WI and T2WI-FS sequences to evaluate the Modic changes of all patients. FS MR images have several important potential advantages over conventional spin-echo images in the detection of bony oedematous lesions. The reduced background signal intensity of marrow fat makes the high-signal-intense lesions more conspicuous. The dynamic range of image display is expanded when the high signal intensity of fat is suppressed, followed by the contribution of improved tissue contrast.14 Therefore, T2WI-FS is very important to detect the Modic Type I and mixed types.
In the current study, 27.2% vertebral end plates showed mixed signals depending on the experience of the observers. This mixed signal corresponds to the conversion of each type of Modic changes described earlier.13,15 Many authors suggest that all Modic changes can progress from one type to another type presenting different stages of the same pathological process. Mixed Modic changes are assumed to develop before the conversion of the true Modic type takes place. The natural conversion of Type I to Type II takes place over 2–3 years and is probably a continuum.12
An important finding in our study was end plate oedema that made a large proportion in all types of Modic changes and in mixed types. In recent years, many scholars discussed the effect of Modic end plate changes on the clinical results of lumbar fusion and lumbar disc replacement. Weishaupt et al16 found superior results after lumbar fusion in patients with Modic Type I. Blondel et al6 analyzed the influence of Modic type on the clinical results of total lumbar arthroplasty with a 2-year follow-up, and the clinical results were best seen in patients with Modic Type I on MR images. End plate oedema represents an active inflammatory phase of disc degeneration. Performing a discectomy during the active inflammatory process may be more beneficial in the reduction of radicular pain, whereas vertebral end plate abrasion helps in improving fusion rate in case of arthrodesis.17 Thereupon having a precise concept of Modic changes is important for patient selection and in pre-operative patient counseling. The combination of TIWI, T2WI and T2WI-FS is highly effective for the evaluation of Modic changes.
It has been suggested that only Modic Type III shows end plate sclerosis, and the Modic Type III changes are presented by decreased signal intensity on both T1WI and T2WI, whereas it appears as obvious high density on CT image. Modic Type I and Type II show no definite correlation with sclerosis on radiography, but according to our knowledge, there are few literature studies that demonstrate the comparison of end plate sclerosis and a specific Modic change. In the current study, Modic Type I, Modic Type II and mixed Modic changes were also associated with end plate sclerosis. It clearly states that end plate sclerosis exist in all types of Modic changes. Therefore, in clinical work, end plate sclerosis on CT image may not just mean Modic Type III which is a stable stage in the process of evolution of end plate changes but may also be associated with patients' clinical outcome.
MRI could not obviously show the appearance of calcification and bone sclerosis. To some extent, the mixed signal of oedema, fat and sclerosis may affect the observer's evaluation. Modic Type I changes are associated with subchondral oedema and has been described as disruption and fissuring of end plate with some regions of degeneration, regeneration and vascular granulation tissue.1 Pathological analysis of trauma, inflammation and tumour reveals woven bone or immature osteoid formation, which reflects the healing process of the lesion. Shaikh et al18 observed low signal intensity reactive sclerosis in both T1WIs and T2WIs in osteoblastoma. Histopathological studies of reactive sclerosis show heavy mineralization of matrix associated with increased fibrovascular tissue within the marrow and perivascular infiltration of lymphocytes and plasma cells.19 Osteosclerosis can be defined as a quantitative increase in bone volume. Sclerosis may be fully or partly mineralized in which the amount of calcium deposition is less compared with fully mineralized sclerosis.20 The signal intensity on MR is mainly a reflection of the vertebral body marrow contents, whereas the plain radiograph and CT reflect the dense mineralized bony content of the vertebral body rather than the marrow contents. The amount of mineralization in reactive sclerosis affects the MR signal intensity.
Modic Type II changes are observed as increased signal intensity on both T1WIs and T2WIs, portraying disruption of the end plates with increased formation of reactive bone and granulation tissue, as under certain conditions, matured osteoblasts and adipocytes can transform into one another and even to fibroblasts,21 haematopoietic elements in the vertebrae are also replaced by fat abundantly.1 The sclerosis observed on CT images and plain film radiographs of Modic Type II change may also represent the mineralization of new reactive bone.
CONCLUSION
End plate oedema is present in a large proportion of mixed types, and Types I–II and Types II–I make up the majority of mixed types. This helps in patient selection and in pre-operative counseling of patients. End plate sclerosis exists in all types of Modic change which is better depicted on CT images and may also correlate with patients' clinical outcomes. End plate sclerosis reflects vertebral body mineralization rather than the change in the bone marrow. Hereby, we conclude that Modic change is a complex and pathological process.
Contributor Information
Lei Xu, Email: Xufeng900427@163.com.
Bin Chu, Email: chubin900427@sina.com.
Yang Feng, Email: fengyangqwer@sina.com.
Feng Xu, Email: Xufeng900427@163.com.
Yue-Fen Zou, Email: zouyuefendc@126.com.
REFERENCES
- 1.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 1988; 166: 193–9. doi: 10.1148/radiology.166.1.3336678 [DOI] [PubMed] [Google Scholar]
- 2.Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology 1988; 168: 177–86. doi: 10.1148/radiology.168.1.3289089 [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Videman T, Niemelainen R, Battie MC. Quantitative measures of Modic changes in lumbar spine magnetic resonance imaging: intra- and inter-rater reliability. Spine (Phila Pa 1976) 2011; 36: 1236–43. doi: 10.1097/BRS.0b013e3181ecf283 [DOI] [PubMed] [Google Scholar]
- 4.Schistad EI, Espeland A, Rygh LJ, Roe C, Gjerstad J. The association between Modic changes and pain during 1-year follow-up in patients with lumbar radicular pain. Skeletal Radiol 2014; 43: 1271–9. doi: 10.1007/s00256-014-1928-0 [DOI] [PubMed] [Google Scholar]
- 5.Nguyen C, Bendeddouche I, Sanchez K, Jousse M, Papelard A, Feydy A, et al. Assessment of ankylosing spondylitis criteria in patients with chronic low back pain and vertebral endplate Modic I signal changes. J Rheumatol 2010; 37: 2334–9. doi: 10.3899/jrheum.100165 [DOI] [PubMed] [Google Scholar]
- 6.Blondel B, Tropiano P, Gaudart J, Huang RC, Marnay T. Clinical results of lumbar total disc arthroplasty in accordance with Modic signs, with a 2-year-minimum follow-up. Spine (Phila Pa 1976) 2011; 36: 2309–15. doi: 10.1097/BRS.0b013e31820f7372 [DOI] [PubMed] [Google Scholar]
- 7.Määttä JH, Wadge S, MacGregor A, Karppinen J, Williams FM. ISSLS Prize Winner: vertebral endplate (Modic) change is an independent risk factor for episodes of severe and disabling low back pain. Spine (Phila Pa 1976) 2015; 40: 1187–93. doi: 10.1097/BRS.0000000000000937 [DOI] [PubMed] [Google Scholar]
- 8.Wu HL, Ding WY, Shen Y, Zhang YZ, Guo JK, Sun YP, et al. Prevalence of vertebral endplate Modic changes in degenerative lumbar scoliosis and its associated factors analysis. Spine (Phila Pa 1976) 2012; 37: 1958–64. doi: 10.1097/BRS.0b013e31825bfb85 [DOI] [PubMed] [Google Scholar]
- 9.Fayad F, Lefevre-Colau MM, Drape JL, Feydy A, Chemla N, Quintero N, et al. Reliability of a modified Modic classification of bone marrow changes in lumbar spine MRI. Joint Bone Spine 2009; 76: 286–9. doi: 10.1016/j.jbspin.2008.09.012 [DOI] [PubMed] [Google Scholar]
- 10.Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J 2006; 15: 1312–19. doi: 10.1007/s00586-006-0185-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohtori S, Inoue G, Ito T, Koshi T, Ozawa T, Doya H, et al. Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back Pain and Modic type 1 or type 2 changes on MRI. Spine (Phila Pa 1976) 2006; 31: 1026–31. doi: 10.1097/01.brs.0000215027.87102.7c [DOI] [PubMed] [Google Scholar]
- 12.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology 1998; 209: 661–6. doi: 10.1148/radiology.209.3.9844656 [DOI] [PubMed] [Google Scholar]
- 13.Mitra D, Cassar-Pullicino VN, McCall IW. Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine. Eur Radiol 2004; 14: 1574–81. doi: 10.1007/s00330-004-2314-4 [DOI] [PubMed] [Google Scholar]
- 14.Mitchell DG, Vinitski S, Rifkin MD, Burk DL, Jr. Sampling bandwidth and fat suppression: effects on long TR/TE MR imaging of the abdomen and pelvis at 1.5 T. AJR Am J Roentgenol 1989; 153: 419–25. doi: 10.2214/ajr.153.2.419 [DOI] [PubMed] [Google Scholar]
- 15.Rahme R, Moussa R. The Modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. AJNR Am J Neuroradiol 2008; 29: 838–42. doi: 10.3174/ajnr.A0925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weishaupt D, Zanetti M, Hodler J, Min K, Fuchs B, Pfirrmann CW, et al. Painful lumbar disk derangement: relevance of endplate abnormalities at MR imaging. Radiology 2001; 218: 420–7. doi: 10.1148/radiology.218.2.r01fe15420 [DOI] [PubMed] [Google Scholar]
- 17.Chataigner H, Onimus M, Polette A. Surgery for degenerative lumbar disc disease. Should the black disc be grafted? [in French.] Rev Chir Orthop Reparatrice Appar Mot 1998; 84: 583–9. [PubMed] [Google Scholar]
- 18.Shaikh MI, Saifuddin A, Pringle NJ, Natail C, Sherazi Z. Spinal osteoblastoma: CT and MR imaging with pathological correlation. Skeletal Radiol 1999; 28: 33–40. [DOI] [PubMed] [Google Scholar]
- 19.Kuisma M, Karppinen J, Haapea M, Lammentausta E, Niinimaki J, Tervonen O. Modic changes in vertebral endplates: a comparison of MR imaging and multislice CT. Skeletal Radiol 2009; 38: 141–7. doi: 10.1007/s00256-008-0590-9 [DOI] [PubMed] [Google Scholar]
- 20.Ott S. Theroetical and methodological approach. In: Bilezikian S, Raisz L, Rodan G, editors. Principles of bone biology. Academic Press: San Diego, CA; 1996. p. 231–41. [Google Scholar]
- 21.Schilling T, Noth U, Klein-Hitpass L, Jakob F, Schutze N. Plasticity in adipogenesis and osteogenesis of human mesenchymal stem cells. Mol Cell Endocrinol 2007; 271: 1–17. doi: 10.1016/j.mce.2007.03.004 [DOI] [PubMed] [Google Scholar]