Abstract
Emergency physicians and radiologists have been increasingly encountering internal concealment of illegal drugs. The packages commonly contain powdered solid drugs such as cocaine, heroin, methamphetamine and hashish, but they may also contain cocaine in the liquid form. The second type of package has recently been more commonly encountered, and poses a greater diagnostic challenge. As clinical evaluation and laboratory tests frequently fail to make the correct diagnosis, imaging examination is typically required. Imaging methods assume a vital role in the diagnosis, follow-up and management. Abdominal X-ray, ultrasonography, CT and MRI are used for the imaging purposes. Among the aforementioned methods, low-dose CT is state-of-the-art in these cases. It is of paramount importance that radiologists have a full knowledge of the imaging characteristics of these packages and accurately guide physicians and security officials.
INTRODUCTION
Transportation of narcotic materials in the gastrointestinal system or other body spaces has been well defined in the medical literature. Since the first report by two Canadian doctors of an ileus case secondary to swallowing a hashish-filled condom in 1973,1 many studies on this subject have been published. Worldwide illegal drug transport using the human body has become increasingly common in recent years. Suspects are usually identified at border controls or airports and brought to hospital emergency departments for definitive diagnosis and management.
Radiology takes a key role in this field by demonstrating packages in body spaces and guiding physicians for follow-up and early diagnosis of possible complications. This article provides general information about the clinical approach to drug smuggling in body spaces and discusses the role of radiology in the diagnosis and management of body-packing suspects, with a review of the current concepts.
TERMINOLOGY AND DESCRIPTIONS
Concealment of illicit drugs may be achieved by different ways and described in different terms.2 The term body packing refers to the act of swallowing a great amount of narcotic material stuffed in a high number of packages, consequently to be concealed in the lumen of the gastrointestinal system and transported to the target destination without being caught by security measures. Drug carriers engaged in this profession are called body packers.2–4 They are also called drug mules, swallowers, internal carriers or couriers.5 Body pushers, on the other hand, fulfil the task of drug transport by placing typically larger drug-filled packages into their rectum or vagina.2–4 However, a single person can be both a body packer and body pusher at the same time.6 A body packer can carry 50–100 packages, each containing 8–10 g of narcotic agents, weighing up to 1 kg in a single transport.5 However, the number of packages and the amount of drugs can be highly variable, and cases have been reported of individuals carrying more than 200 packages.7 The packages can be detected anywhere in the gastrointestinal tract of a body packer. However, in body pushers, the packets are found further distally. Accordingly, the information regarding the suspect's interrogation obtained through the security personnel accompanying the suspect can help the physician identify the starting point for the examination. The term body stuffer is used for persons carrying a lesser number of carelessly packed small packages, concealed when coming across security forces (Table 1).2,5 Drug cartels may also use children8–10 and females who are pregnant6,11 to draw less attention and are able to pass narcotic drug packages without getting caught.
Table 1.
Body packing vs body stuffing
| Body packer | Body stuffer | |
|---|---|---|
| Definition | Persons professionally carrying a large number of packages containing narcotic materials using their body spaces | Persons hiding packages from security forces with the fear of getting caught; often self-abuser or street dealer |
| Synonyms | Swallowers, mules, couriers, internal carriers, burriers | Mini packer, quick swallowers |
| Number of carried packages | High quantity (an average of 50–100 packages) | Low quantity (an average of 1–15 packages) |
| Packet features | ||
| Type of production | Mechanically or handmade | Handmade |
| Features of packaging | Tight and durable | Loose and sloppy |
| Size | 2–8 cm | 0.5–2 cm |
| Contents | Mostly cocaine, heroin, methamphetamine, liquid cocaine | Mostly cocaine (powder or crack) and heroin |
| Clinical importance | Probability of surgical complication (i.e. ileus, perforation) is higher | Probability of intoxication is higher |
| Radiological diagnosis | Relatively easy | More difficult |
| First examination | Plain film, ultrasound or low-dose CT | Low-dose CT |
| Standard of reference | Non-enhanced CT | Non-enhanced CT |
Body packers commonly carry packages filled with cocaine, heroin and methamphetamine. Although, it has become a rare observation, cannabis products such as marijuana and hashish were also encountered frequently in the past.12 However, it has been reported that hallucinogenic or synthetic drugs like amphetamines, 3,4-methylenedioxymethamphetamine (ecstasy) and lysergic acid are also transported.5,12 Drug-filled packages may be handmade or manufactured. Mechanically manufactured packages tend to have a uniform shape and dimension.12 Packages contain solid powder of drugs tightly packed with a synthetic material (e.g. condoms, plastic wraps/bags, latex glove fingers, balloons, aluminium foil, cellophane and glassine).5,12 These packages are also called bolitas.13 Although packages that contain solid drugs are encountered in the majority of body packers, a novel type of smuggling has recently emerged; body packers carrying liquid cocaine-containing packages have increasingly been reported recently (Figure 1).14,15
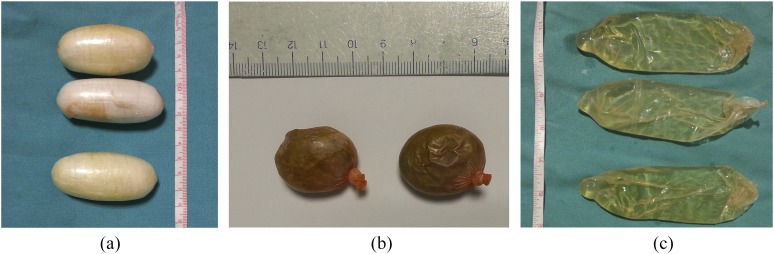
Figure 1.
Package samples obtained from body packers. (a, b) Packages of different sizes and appearances containing solid powdered drugs. (c) Packages containing liquid cocaine.
Body packers use parasympatholytics and constipating agents to prevent premature defaecation of drug packages before arriving at their target location, especially on long journeys. When they arrive at the target region or country, they use laxatives or enemas to facilitate defaecation of packages.5
CLINICAL ASPECTS
Security officers often cannot accurately detect body packers. Rather, some persons with certain features are considered suspects and taken into custody.5,12 Physicians encounter body packers during medical examination after their arrest or custody, or in the case of a drug-induced intoxication or adverse event, such as gastrointestinal obstruction requiring surgical intervention.5,7 Most body packers may not act honestly during interrogation, despite knowing the number and content of packages they carry. In addition, communication with them may become rather a problematic experience owing to language barriers or fear and anxiety.2 Furthermore, albeit rare, drug-induced intoxication may make interrogation impossible.5 However, careful questioning should be carried out with regard to the presence of possible complications (e.g. pain, bloating, vomiting, obstipation and constipation). A physical examination may show signs of toxicity secondary to package rupture.5 Packages can be located through abdominal palpation, rectal and vaginal examination. It must be noted that most of the time, physical examinations are not useful. However, physical examination will be sufficient in most body pusher cases. Urinalysis has a limited role and a low sensitivity in primary diagnosis;2,5 however, it has a very high sensitivity in cases of pack leakage.
Fatal toxic adverse effects may emerge as a result of leaky or ruptured packages. This condition was first described as body packer syndrome by Wetli and Mittleman in 1981.16 Since the description of the first case, many cases of fatal and non-fatal drug toxicity secondary to body packing have been reported.17 Physical examination and laboratory investigation are an essential part of management in such cases because packet leaks within the intestinal lumen can be fatal. Cocaine absorption through intestinal mucosa is massive and rapid. The contents of a single packet of cocaine exceed the acute oral lethal dose (1.2 g) by many times.5,18 Body stuffers are at an even greater risk of overdose because they swallow quickly and carelessly packaged drugs.19 Methamphetamine toxicity secondary to intravaginal body stuffing has also been reported.20
RADIOLOGICAL EVALUATION
In suspected cases, radiologic imaging has to be used to confirm the diagnosis of body packing.5 Plain abdominal radiography, contrast-enhanced abdominal radiography, ultrasonography, CT and MRI have been used in the diagnosis of these cases (Table 2). Among these, abdominal X-ray and ultrasonography can reportedly be used as screening tests.5
Table 2.
Imaging characteristics of different types of drug packets
| Imaging | Solid substance-powder | Liquid cocaine |
|---|---|---|
| Plain film | ||
| Radiodensity | Radiolucent to radiopaque | Radiopaque |
| Specific signs | Double-condom sign | Thin lucent lines |
| Tic-tac sign | ||
| Parallelism sign | ||
| Rosette sign | ||
| Dense material sign | ||
| Ultrasound | ||
| Echogenicity | Hyperechoic smooth surface with strong clean shadow | Hyperechoic irregular surface with clean shadow |
| Specific signs | Not described | Not described |
| CT | ||
| Density | Hypodense, isodense, hyperdense | Hyperdense |
| Specific signs | Double-condom sign | Thin hypodense lines |
| Tic-tac sign | Jigsaw pattern | |
| Parallelism sign | ||
| Rosette sign | ||
| MRI | ||
| Intensity | Hypointense, both in T1 weighted and T2 weighted images | Variable |
| Specific signs | Not described | Thin hypointense lines |
| Common imaging characteristics | Multiple ovoid–oblong, sharp-contoured foreign bodies with a smooth surface | Multiple foreign bodies without a regular shape, which take the form of the lumen they are in, with irregular contours |
| Owing to hard inner structure and shape, they align in consecutive, parallel or transverse array | Owing to soft inner structure, they appear one within the other and give the impression as if they were adherent | |
Plain abdominal radiography
The most widely used imaging for the detection of drug-filled packages is abdominal X-ray.3,4,12 This technique is often preferred because of the advantages of involving a lower radiation dose and being relatively inexpensive and fast.21 However, studies on its role in body packaging reported sensitivity levels that ranged between 40 and 100%.2–6 This variability in sensitivity level may be related to variations in drug type and degree of purity, packaging material used, number and size of packages, location in the gastrointestinal system and expertise of the radiologist.6
The basic factors that complicate radiographic diagnosis are the following: cases in which few, small-sized packages are carried (especially in body stuffers), use of enema, bowel movements, increased bowel content and gas distention. In addition, factors independent of the suspect such as the inexperience of the radiologist and lower contrast resolution of radiography may also further complicate diagnosis.2,12,13,22–24 Moreover, body packers may use some tricks to further complicate the identification of the packages.12,13 Packages may sometimes be swallowed together with liquid materials of radiographic density to make it more difficult to differentiate packages from intestinal content.12 The specificity of abdominal plain film is higher, with figures above 90% having been reported. Hardened faeces (faecalomas formed by hardened faeces may mimic the appearance of packages owing to their similar shape with packages), intra-abdominal calcifications, foreign materials and even gas and faeces in the bowel lumen can all inadvertently lead to a misdiagnosis of body packing.6 Low-dose CT, which provides definite diagnosis with roughly similar dose level as plain film, shall be the preferred method, when available.
In recent years, liquid cocaine smuggling has been reported in the medical literature. While clinical and radiologic knowledge of this method is limited, it has been reported that these types of packages may lead to false-negative results because they can take the shape of the intestinal lumen and appear in similar density with intestinal content on plain films.14,15 In one of the most comprehensive studies on this subject, the sensitivity and specificity of X-ray for the detection of liquid cocaine-filled packages were found to be significantly lower than those for the detection of packages containing solid drugs.25
Packages that contain drugs in solid form are more easily recognized owing to their packing features and shape. Some of the imaging features of these packages that can be used to detect them have already been defined in the literature and are now very well known. In suspected cases, the diagnosis is made by visualizing regular-shaped foreign bodies of varying densities, which can be distinguished from the gastrointestinal lumen (Figure 2a). Double-condom sign,26 rosette sign,27 tic-tac sign,24 parallelism sign24 and dense material sign6,24 are defined as ancillary imaging findings. Unfortunately, packages that contain liquid cocaine do not exhibit the above signs. In this case, “thin lucent lines” visualized by abdominal X-ray produced by the air trapped in the interface between the packets may aid in the diagnosis (Figure 2b).28
Figure 2.
Abdominal X-ray images of packages that contain narcotic materials in solid and liquid forms. (a) A 34-year-old male body packer. In the intestinal lumens, multiple dense packages consisting of powdered cocaine with a scattered formation and ovoid morphology are observed. (b) A 48-year-old male body packer. In the colonic loops, widespread density increments with obscure contours and subtle serpiginous lucencies are observed. Be aware of the fact that contrary to solid drug-containing packages, these types of packages that contain cocaine in liquid form cannot be clearly distinguished.
Some studies have sought for a relationship between the chemical content of a package and package densities on abdominal X-ray.12,21,25,29 In these studies, the radiographic imaging characteristics of drugs like hashish, heroin and cocaine have been determined in comparison with air and faeces. There is, however, a poor correlation between the studies. This has been explained by the fact that the degree of purity of packet contents and manufacturing processes (e.g. wrapping and compression of packages) may be quite variable.6,12,25 An additional issue to consider is that it is still unclear how the radiologic predictability of package content is clinically important.
Ultrasonography
Ultrasonography has certain advantages such as being readily accessible, reproducible, relatively inexpensive and does not involve ionizing radiation. However, it also has some disadvantages such as requiring expertise and being operator dependent.6 Furthermore, examination of the whole gastrointestinal tract is time consuming, and it requires the examiner to get physically close to a possibly dangerous potential criminal. Although ultrasonography has been used in the diagnostic assessment of body packers for years, the literature knowledge of this subject is still limited.23,30–32 Ultrasonography can be used as the first choice in the detection of intestinal obstruction secondary to packages and intra-abdominal free fluid.12 Furthermore, it has been reported that an intravaginal package was detected in a suspect using sonography.33 Gas and faeces that surround drug packages in the intestinal lumen may reduce diagnostic accuracy of the method and lead to non-identification of packages.34,35
Former articles on this subject have reported that X-ray and ultrasonography had similar accuracies in demonstrating packages.23,36,37 In contrast, Meijer and Bots30 determined that the positive-predictive value and accuracy rate of ultrasonography were 97.6% and 94%, respectively. The authors reported that abdominal ultrasonography was a valuable method with results available within minutes, one that could be used as a screening method to detect suspected cases of body packing at airports.30 Cengel et al32 in a recent study, in which ultrasonography and CT were compared, reported that ultrasonography had a sensitivity and specificity of 91% and 70%, respectively. Ultrasonography accurately predicted the presence and absence of packages in 39 of 45 suspects.32
Packages that contain drugs in solid form are visualized as multiple, immobile, smooth-contoured, ovoid, hyperechogenic masses in intestinal lumen. Another distinctive feature of packages is that they cause strong posterior clean shadowing.23,30,32 Furthermore, reverberation artefacts can be visualized behind packages owing to trapped air in the sheath.6 Ingesting liquid materials facilitates visualization of packages by forming an acoustic window.3,32 Despite the fact that liquid cocaine-containing packages have similar sonographic features, their irregular surface is their most distinctive feature. However, differentiation of this type of package from intestinal gas and faeces is difficult, and ultrasonography may face certain challenges in the differential diagnosis (Figure 3).32
Figure 3.
Abdominal ultrasonography images of the packages that contain narcotic materials in solid and liquid forms. (a) A 30-year-old female body pusher. In the lower abdominal ultrasonography images that are obtained on sagittal plane, intravaginally settled hyperechogenic packages filled with cocaine are observed (arrowheads). The acoustic window formed by the full urinary bladder eases the imaging of the packages (UB, urinary bladder; U, uterus). (b) The long-axis view of a drug-containing package in the intestinal lumen in a 36-year-old female body packer. In the anterior, the front surface of the package is seen as a hyperechogenic line (arrowheads), whereas there is a strong acoustic shadowing (asterisk) formed in the posterior. (c) In a case of a 43-year-old male body packer, short-axis view of two packages that contain cocaine in the intestinal lumen (arrowheads). (d) In a case of 27-year-old male body packer, packages containing liquid cocaine in the intestinal lumen are seen as non-uniform-surfaced posterior shadow-forming foreign bodies (arrowheads). Note that the appearances of these packages resemble intestinal gas and faeces. (e) A 23-year-old female who is pregnant with intestinal drug packages. Upon abdominal sonography inspection, the package containing drugs in the intestinal lumen is seen as a hyperechogenic straight line with a strong posterior shadowing (arrowheads). Furthermore, a 10-week-old foetus (F) is observed in the uterine cavity.
CT
Unenhanced CT is the most valued imaging modality in body packers. It is the preferred confirmatory imaging method in highly suspected cases when abdominal plain film fails to make the diagnosis.4 In this examination method, the presence, size, localization and number of packages can be accurately determined. If the exact number of ingested packages can be determined, additional imaging may not need to be performed before discharge of the suspect. Moreover, rupture of package sheathes and drug leaks can also be demonstrated.3,21 CT can easily detect packages located in the stomach, small and large intestines and rectum and even those in the vagina.4,25 The widely accepted view in the literature about the CT protocol for use in suspected cases is that it should be taken without rectal or oral contrast material administration because luminal contrast material may complicate the visualization of packages that have a similar density to the contrast material.3,4,6,35 Moreover, contrast material may augment intestinal peristalsis and trigger intestinal obstruction.4 It has been reported that in a suspected case, contrast material in the gastrointestinal lumen did not facilitate making the diagnosis; conversely, it prevented CT detection of a single remaining package in the intestinal lumen.38,39 Intravenous contrast material is not routinely needed either.
CT images should be evaluated in both abdominal and lung windows. It has been reported that the use of lung windows facilitates the evaluation of packages.3,4,6,21,40 Lung window shows trapped air in packages to a better degree.3 However, a recent study demonstrated that the examinations only included abdominal window and those that included both abdominal and lung windows had a similar overall diagnostic accuracy.41 Still, especially in body stuffers, it is recommended that lung window be used to detect packages which are iso-hypodense to intestinal content and small packages.3 A scout image taken before starting CT examination may be useful. A study on pig cadavers suggested that scout imaging on two planes was five times more sensitive (56% vs 11%) than conventional radiography and emitted one-third of the latter's radiation dose.42 The sensitivity of CT for the diagnosis of body packing has been reported to range between 96.5 and 100% and its specificity between 94.1 and 100%.25,43,44 Flach et al43 reported one false-positive but no false-negative results in 35 suspected cases. In that study, CT featured 100% sensitivity in all body packer, body pusher and body stuffer subgroups. Nevertheless, radiography had a significantly lower sensitivity (28.6%) in body stuffers. Unfortunately, the majority of CT studies performed to date included body packers, and we have no knowledge of its diagnostic role in body stuffers. In another article, unenhanced CT failed to correctly detect a case of cocaine body stuffing.45
CT appearances of packages vary in accordance with their drug content, the drug's degree of purity and packing pattern. Multiple, ovoid-shaped, sharp-contoured packages of variable density can be visualized in the gastrointestinal lumen. Sometimes, larger packages that contain smaller packages may also be seen (Figures 4–6). Findings on plain films that have already been mentioned above can be more accurately demonstrated in CT.3,4,6 Packages that contain liquid cocaine appear as irregularly shaped homogeneous, hyperdense structures, which take the form of the intestinal lumen.6,25,28 Some air content may also be visualized inside packages. Thin, hypodense band formations caused by trapped air between the package sheath and packages are specific. In addition, the so-called “jigsaw” pattern may be noted as a result of packages interlocking with each other (Figure 7).25,28
Figure 4.
CT images of packages containing solid drugs with isodense appearances. (a) In a case of a 34-year-old-male body packer, isodense packages containing methamphetamine can hardly be detected. However, when looked at carefully, a thin halo belonging to the covering of the package wrapping the drug and the air trapped inside make them easier to identify. (b) In a case of a 23-year-old-male body packer, the oral contrast matter given has increased the visibility of the packages that contain methamphetamine (asterisks).
Figure 6.
A 35-year-old male body packer. (a) There is no clear evidence for drug-filled packets with CT localizer image. (b) Multiple low-density packages are observed in the gastric lumen using unenhanced CT scan. A total amount of 612 g of 49 heroin packets were obtained from this case.
Figure 7.
A 56-year-old male body packer. (a) Multiple nested hyperdense packages filling the colonic segments and hypodense lines that separate these packages from each other are observed (arrowheads). (b) Packages in the rectum lumen forming a jigsaw pattern. (c) In three-dimensional volume-rendering technique images, package structures that are adjacent can partially be identified. A total amount of 2200 g of 42 liquid cocaine-containing packages were obtained from this case.
Figure 5.
A 25-year-old male body packer and body pusher. (a) Sagittal CT imaging of the intestinal loop lumens without contrast material reveal multiple hyperdense drug-filled capsules along with two bigger sized packages in the lumen of the rectum. (b) In three-dimensional volume-rendering technique images, capsules can be distinguished more easily. A total amount of 1093 g of 60 cocaine capsules were obtained from this case.
Studies have been conducted for many years in an attempt to predict the type of narcotic material, based on the density characteristics of packages.6,21,25,29 Wackerle et al29 investigated the correlation between drug type and package density for the first time by making in vitro Hounsfield unit (HU) measurements. However, there is discordance between subsequent studies published on this subject. Packages that contain solid drugs can have a wide range of density levels ranging from −520 HU to 700 HU.29 These packages can have a very heterogeneous internal structure depending on drug mixture. Conversely, packages that contain liquid cocaine appear more homogeneous and have average HU levels of 155–31025 and 177–240,28 depending on the study. Such packages can be easily detected because their densities are considerably higher than that of intestinal contents. On the other hand, oral or rectal contrast administration would complicate the evaluation.25 In vitro studies with dual-energy CT suggested that cocaine and heroin can be distinguished with this method.46–48 However, it is unclear what clinical implications of use of this modality would have in vivo.
CT is the best imaging modality for the visualization of foreign materials in the human body.49 However, its major disadvantages include its absence at airports, high cost and, most importantly, a high dose of radiation.6 It was reported in a body packer series that routine-dose CT examinations had mean effective radiation dose levels as high as 8.33 mSv25 and 8.77 mSv,32 depending on the series. The increased amount of radiation to which the general population is exposed due to more common use of CT has raised concerns about being a serious public health issue in the future.50 Quality images can be acquired using low-dose radiation with recent advances in CT technology and the introduction of iterative reconstruction methods.6 Low-dose CT may replace conventional radiography as the initial imaging modality in suspected cases of body packing.49 Poletti et al51 calculated the estimated radiation dose 1.7 ± 0.2 mSv for females and 1.2 ± 0.1 mSv for males in examinations performed with a lowered milliampere second level (30 mAs). However, in the same series, the abdominal X-ray doses were 2.0 ± 0.7 mSv in females and 1.3 ± 0.4 mSv in males. Furthermore, it has been argued that ultra-low-dose CT examinations performed with an estimated dose of nearly 0.36 mSv provided adequate and evaluable images.6 In a recent study, Aissa et al52 have shown that the mean radiation dose level was 1.06 ± 0.49 mSv, by utilizing low-tube voltage (100 kVp) with automated tube-current modulation.
MRI
MRI has a limited role in spotting foreign bodies in the intestinal lumen.29 Based on this information, a general opinion predominated until recently that MRI was unsuccessful at detecting packages in the gastrointestinal lumen of body packers. Although one personal communication argued that MRI was beneficial for the diagnosis of body packing, it was deemed impractical owing to its cost and low availability.13,53 However, a feasibility study that included 16 suspects by Bulakci et al54 showed that this method was useful from a diagnostic standpoint. In that case series, 10 suspects who were carrying solid drugs and 3 suspects who were carrying 3 liquid cocaine packages were correctly diagnosed using MRI. The absence of packages was also correctly established in two suspects. However, one suspect was wrongly diagnosed because of intestinal gas. There is still a need for more large-scale studies to determine the diagnostic utility of MRI in this field.6,54
In vitro signal characteristics of packages have previously been reported, and no differences in the appearances of different drug types have been observed.29 In vivo signal characteristics have also been defined for packages that contain both solid and liquid drugs. Unfortunately, the only in vivo study on this subject contains a low number of cases with low diversity and thus offers limited information. It has been reported that packages with solid drug contents appear markedly hypointense, both in T1 weighted and T2 weighted series, and those that contain liquid cocaine are mildly hyperintense or at water intensity in T2 weighted series.54 Solid drug packages are easily diagnosed in the stomach, small intestine and rectum, but dense colonic gas surrounds packages and complicates their recognition in the colonic lumen. However, morphologic and luminal localization features of packages may aid in their differentiation from intestinal contents (Figure 8). Liquid cocaine-filled packages, on the other hand, have high signal properties, which makes them easier to be distinguished from intestinal gas.54 However, it should be kept in mind that liquid cocaine-containing packages may have variable signal intensity (Figure 9). Therefore, packages that contain liquid cocaine are harder to distinguish from faeces when they are mildly hyperintense and from intestinal gas when they are hypointense. Administration of medications that reduce intestinal peristalsis and gas may increase diagnostic efficacy. The additional benefits of using sequences and techniques other than conventional T1 weighted and T2 weighted are a subject of interest.
Figure 8.
A 32-year-old female body packer. Packages that contain powder cocaine in the gastric and intestinal loop lumens are clearly seen as hypointense on T2 weighted axial (a) (asterisks) and coronal (b) MR images.
Figure 9.
Multiple amorphous packages in the colonic lumen containing liquid cocaine in a case of a 28-year-old female body packer. (a) Hyperintense areas that do not have sharp borders are seen in a T1 weighted axial MR image. (b) When looked at carefully, separable packages with different signals and one within the other (asterisks) and the air/liquid levels (arrowheads) inside them can be observed using T2 weighted axial MRI. (c) In a scout image, while packages are found to be in liquid intensity, hypointense lines (arrowheads) that separate the packages can be identified more clearly. (d) A non-enhanced axial CT scan reveals the existence of the packages in a more detailed way.
MRI is a reliable, non-ionizing radiation technique that can be safely used, especially in children and females who are pregnant. However, with regard to detection of body packing, it has some disadvantages like low availability, high cost and long examination time. Furthermore, suspect can easily render the MR images non-diagnostic by moving during the exam. Besides, if the packaging material contains ferromagnetic materials, MRI may harm the body packer. Owing to the fact that MRI has the aforementioned drawbacks and its exact role in body packers is not yet clear, the use of this method may be limited, particularly when low-dose CT is available.
MANAGEMENT OF SUSPECTS
There may be differences between the approaches of countries and healthcare facilities with respect to management of body packers. Radiologists should have a thorough knowledge of local legislation related to imaging of such cases. Obtaining an informed consent is mandatory in some countries; however, it is not obligatory in all countries, and radiologic tests can be performed on the request of custom officers or other security personnel.4 Diagnostic processes and follow-up procedures of children and females who are pregnant are more complicated and care should be taken.
Radiologists face three diagnostic challenges in these cases. The first is the need for radiologic confirmation as to whether a suspect who has been brought to the hospital actually carries package(s). The second problem is related to determining whether signs of complications such as package rupture, obstruction and perforation are evidenced by the radiologic examination. The third relates to the determination as to whether a residual package has been left after multiple defaecations.23,32,55 Here, the role of a radiologist is vital, bringing many legal and ethical responsibilities. False-negative reports will lead to the inadvertent release of a true suspect and delivery of illegal material(s) to the public. False-positive results, on the other hand, will cause innocent travellers to be unjustly detained. In addition, these inconveniences will keep healthcare facilities and personnel busy for no reason, which leads to extra costs and loss of valuable time.56 Another point that radiologists should consider is that, to avoid being caught, drug smugglers may apply some misleading, evasive techniques that complicate the diagnosis.13,57
Body packing harbours serious risks for the carrier. Many fatal complications have been reported in the medical literature since its first description. Serious conditions that have been reported to have required intervention include gastric obstruction,18 intestinal obstruction,1,18,25,58,59 small intestinal perforation,60 large intestinal perforation,61 oesophageal obstruction,62 oesophageal perforation,62 gastric ulceration63 and respiratory arrest owing to aspiration of package content.64 Radiology assumes an important role in the diagnosis of these complications. Plain films, ultrasonography and CT may be used in the diagnosis. However, CT is the most valuable imaging modality.
Many algorithms have been proposed for the clinical and radiologic management of suspected cases (Figure 10). Plain film is the most commonly employed and recommended imaging method for the initial diagnosis and screening of suspected cases. However, ultrasonography5,30,32 and low-dose CT51,65 have also been recommended for use for this purpose. The use of routine-dose CT, especially for initial assessment and for screening purposes, is not recommended because of its high radiation dose. Diagnosis can usually be made with all modalities because suspects carry a high number of packages at the time of examination.6 As packages are defecated during follow-up, the number of packages in the gastrointestinal lumen decreases and radiologic imaging becomes harder with time.6 This condition reportedly causes hardship in the sonographic32 and X-ray51,55 follow-up of body packers. Cengel et al32 developed a modified screening method in which the gastric lumen, caecum and rectosigmoid region were screened after making the suspect drink an amount of water; the authors recommended a sonography-based algorithm. In a comparative study with CT, Poletti et al51 showed that abdominal plain film had a markedly reduced sensitivity in body packers who carried less than 12 packages. In another study that supported this finding, X-ray evaluation missed 70% of residual packages left after two empty defaecations.55 Rousset et al55 concluded that CT is mandatory to safely discharge body packers. Schulz et al65 suggested a low-dose CT-based algorithm and recommended the use of post-processing techniques such as maximum intensity projection images and coronal and sagittal multiplanar reformatted images. These types of reconstructed images facilitate the determination of the actual number of packages.
Figure 10.
A sample algorithm for the clinical and radiologic management of body packers. This algorithm was prepared based on the results of various studies in the literature. Each centre can modify this algorithm in accordance with local laws or hospital policies. X-ray, ultrasonography or low-dose CT can each be selected as the initial imaging technique. Although variable, the generally accepted time period required to be referred to as package retention ranges between 5 and 7 days (LD CT, unenhanced low-dose CT).
Plain film, ultrasonography or low-dose CT have been reported as the initial imaging modality. Nevertheless, based on the recent literature, low-dose CT has been the preferred method in both initial and pre-discharge imagings of suspects. Ultrasonography and MRI would be appropriate in children and females who are pregnant (Figure 3e). Body packers are easily and highly accurately diagnosed by unenhanced CT. However, it is important that CT evaluation before discharge procedures should not be made by an emergency physician, but rather by an experienced radiologist with sufficient expertise in this field.41
Jones and Shorey66 proposed a clinical staging system based on symptoms and signs to determine which treatment and interventional protocols should be used in cases of body packing. According to their staging system, each case is categorized as one of four grades, and medical and surgical interventional options are applied accordingly. Asymptomatic cases defecate packages without difficulty after oral polyethylene glycol administration.67 Some other authors have recommended oil-based laxatives.68 However, suspects can also be followed up without the administration of whole-body irrigation or laxatives. There is no clear consensus as to how long body packers should be monitored. A prospective study reported that the defaecation of packages containing solid drugs was completed between 6 h and 9 days, at a mean of 54 h, and liquid cocaine-containing packages between 1 h and 14 h, at a mean of 9 h. In two cases in that series, packages became stuck in the stomach and were removed using gastrostomy on the eighth and ninth days.32 The residence time of packages in the body may show great variations. A heroin-containing package that was stuck in the gastric pylorus was removed without any complication 21 days after ingestion in a male drug smuggler aged 27 years.69 Although it is not clear when to intervene in asymptomatic cases in which packages cannot be completely discharged, there are reports recommending to do so at 570 and 7 days.68 Here, the concern is that packages retained in the stomach may rupture owing to the effect of gastric acid. Laparotomy is typically the recommended surgical approach. Endoscopic or laparoscopic approaches may introduce risks related to damage or rupture of packages during the procedure.68
It should be ensured that all packages are definitely defecated before initiating discharge procedures in suspects who are asymptomatic. It has been reported that a normal abdominal X-ray obtained after two5,70 or three68 empty defaecations can be used as a clearance test. If the suspect has a false-negative initial imaging, then an abdominal CT should be taken.70 However, it seems more logical to make the pre-discharge examination with a CT, owing to the inadequacy of X-ray in detecting residual packages.55 Here, another debated subject is whether routine-dose CT or low-dose CT should be used. Rousset et al55 used routine-dose CT as pre-discharge imaging and reported substantially high radiation doses, as much as 11.3 mSv in males and 13.4 mSv in females. Obviously, this may create some serious ethical issues. On the other hand, the latest data in the literature suggest that low-dose CT can be preferred over routine-dose CT.
Imaging does not take an important role in the management of body stuffers.45 Imaging can be resorted to when no packages are found in the stool or when patient anamnesis and clinical findings are incompatible with a history of package swallowing.45 Among other things, it is also controversial as to which imaging method should be used in these types of cases because the literature data concerning the role of imaging are limited.44 It has been reported that abdominal X-ray was very poor at visualizing packages in these suspects.45,71–74 Thus, it has been reported to be of no use for the management of body stuffers.45,71 The use of CT may overcome the problem of routine radiographies' lower resolution.75 A number of case reports concluded that CT was successful with body stuffers.38,75 However, CT failed in a male aged 37 years, who had swallowed a large package containing 15–20 other smaller packages; the package was subsequently removed through laparotomy after nine empty defaecations.45 West et al's76 series included 55 cases of body stuffing, involving methamphetamine as the drug material. Abdominal radiographs were taken in 18 cases, abdominal CT in 4 cases and ultrasonography in 1 case; all imaging modalities failed to detect the packages. Yet, Schmidt et al44 used a phantom in a CT study and reported a sensitivity of 86.5% and specificity of 100%. However, more large-scale in vivo studies are required on this subject.
CONCLUSION
Emergency room physicians and radiologists encounter increasingly more cases of drug smuggling in body spaces. Radiologic imaging techniques assume a vital role in the diagnosis, follow-up and treatment of these cases. Drug smugglers may use some confusing methods to puzzle security officers and physicians. Moreover, this subject also involves some difficult medicolegal and ethical issues for radiologists and other healthcare professionals. It is of paramount importance for the management of body packers, body stuffers and body pushers that radiologists have a thorough knowledge of the imaging signs of each smuggling type and different packages. The radiologic diagnosis of body stuffers is more challenging and abdominal radiograms may fail to diagnose them because they carry fewer smaller packages. Abdominal plain film and ultrasonography could be used as the initial imaging methods for screening purposes in body packers. The main problem with these methods is, however, their low negative-predictive value. CT is the gold standard imaging used when complications arise or for confirmatory purposes in difficult cases. It is also recommended as a pre-discharge imaging method. In particular, low-dose CT shall be preferred to avoid large amounts of radiation. The diagnostic role of MRI in suspected cases is a subject that needs more research, and this modality is not yet part of the routine radiologic algorithm. Despite this, it may be selected along with ultrasonography in paediatrics and females who are pregnant.
Acknowledgments
ACKNOWLEDGMENTS
We would like to thank Dr Omer Bulakci for his great support in translation of the articles in German and in preparation of the flow chart.
Contributor Information
Mesut Bulakci, Email: mesutbulakci@yahoo.com.
Ferhat Cengel, Email: doc_20_1@hotmail.com.
REFERENCES
- 1.Deitel M, Syed AK. Intestinal obstruction by an unusual foreign body. Can Med Assoc J 1973; 109: 211–2. [PMC free article] [PubMed] [Google Scholar]
- 2.Booker RJ, Smith JE, Rodger MP. Packers, pushers and stuffers—managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J 2009; 26: 316–20. doi: 10.1136/emj.2008.057695 [DOI] [PubMed] [Google Scholar]
- 3.Sica G, Guida F, Bocchini G, Iaselli F, Iadevito I, Scaglione M. Imaging of drug smuggling by body packing. Semin Ultrasound CT MR 2015; 36: 39–47. doi: 10.1053/j.sult.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 4.Pinto A, Reginelli A, Pinto F, Sica G, Scaglione M, Berger FH, et al. Radiological and practical aspects of body packing. Br J Radiol 2014; 87: 20130500. doi: 10.1259/bjr.20130500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Traub SJ, Hoffman RS, Nelson LS. Body packing—the internal concealment of illicit drugs. N Engl J Med 2003; 349: 2519–26. doi: 10.1056/NEJMra022719 [DOI] [PubMed] [Google Scholar]
- 6.Berger FH, Nieboer KH, Goh GS, Pinto A, Scaglione M. Body packing: a review of general background, clinical and imaging aspects. Radiol Med 2015; 120: 118–32. doi: 10.1007/s11547-014-0458-0 [DOI] [PubMed] [Google Scholar]
- 7.Bulstrode N, Banks F, Shrotria S. The outcome of drug smuggling by “body packers”—the British experience. Ann R Coll Surg Engl 2002; 84: 35–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Traub SJ, Kohn GL, Hoffman RS, Nelson LS. Pediatric “body packing”. Arch Pediatr Adolesc Med 2003; 157: 174–7. doi: 10.1001/archpedi.157.2.174 [DOI] [PubMed] [Google Scholar]
- 9.Beno S, Calello D, Baluffi A, Henretig FM. Pediatric body packing: drug smuggling reaches a new low. Pediatr Emerg Care 2005; 21: 744–6. doi: 10.1097/01.pec.0000186428.07636.18 [DOI] [PubMed] [Google Scholar]
- 10.Chakrabarty A, Hydros S, Puliyel JM. Smuggling contraband drugs using paediatric “body packers”. Arch Dis Child 2006; 91: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cordero DR, Medina C, Helfgott A. Cocaine body packing in pregnancy. Ann Emerg Med 2006; 48: 323–5. doi: 10.1016/j.annemergmed.2006.02.019 [DOI] [PubMed] [Google Scholar]
- 12.Hergan K, Kofler K, Oser W. Drug smuggling by body packing: what radiologists should know about it. Eur Radiol 2004; 14: 736–42. doi: 10.1007/s00330-003-2091-5 [DOI] [PubMed] [Google Scholar]
- 13.Algra PR, Brogdon BG, Marugg RC. Role of radiology in a national initiative to interdict drug smuggling: the Dutch experience. AJR Am J Roentgenol 2007; 189: 331–6. doi: 10.2214/AJR.07.2306 [DOI] [PubMed] [Google Scholar]
- 14.Burillo-Putze G, Becker LT, Rodrı´guez MG, Torres JS, Nogue´ S. Liquid cocaine body packers. Clin Toxicol (Phila) 2012; 50: 522–4. doi: 10.3109/15563650.2012.687742 [DOI] [PubMed] [Google Scholar]
- 15.de Bakker JK, Nanayakkara PW, Geeraedts LM, Jr, de Lange ES, Mackintosh MO, Bonjer HJ. Body packers: a plea for conservative treatment. Langenbecks Arch Surg 2012; 397: 125–30. doi: 10.1007/s00423-011-0846-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wetli CV, Mittleman RE. The “bodypacker syndrome”—toxicity following ingestion of illicit drugs packaged for transportation. J Forensic Sci 1981; 26: 492–500. [PubMed] [Google Scholar]
- 17.Koehler SA, Ladham S, Rozin L, Shakir A, Omalu B, Dominick J, et al. The risk of body packing: a case of a fatal cocaine overdose. Forensic Sci Int 2005; 151: 81–4. doi: 10.1016/j.forsciint.2004.07.005 [DOI] [PubMed] [Google Scholar]
- 18.Pidoto RR, Agliata AM, Bertolini R, Mainini A, Rossi G, Giani G. A new method of packaging cocaine for international traffic and implications for the management of cocaine body packers. J Emerg Med 2002; 23: 149–53. doi: 10.1016/S0736-4679(02)00505-X [DOI] [PubMed] [Google Scholar]
- 19.Püschel K, Stein S, Stobbe S, Heinemann A. Analysis of 683 drug packages seized from “body stuffers”. Forensic Sci Int 2004; 140: 109–11. doi: 10.1016/j.forsciint.2003.10.025 [DOI] [PubMed] [Google Scholar]
- 20.Kashani J, Ruha AM. Methamphetamine toxicity secondary to intravaginal body stuffing. J Toxicol Clin Toxicol 2004; 42: 987–9. doi: 10.1081/CLT-200042554 [DOI] [PubMed] [Google Scholar]
- 21.Ab Hamid S, Abd Rashid SN, Mohd Saini S. Characteristic imaging features of body packers: a pictorial essay. Jpn J Radiol 2012; 30: 386–92. doi: 10.1007/s11604-012-0069-4 [DOI] [PubMed] [Google Scholar]
- 22.Karhunen PJ, Suoranta H, Penttilä A, Pitkäranta P. Pitfalls in the diagnosis of drug smuggler's abdomen. J Forensic Sci 1991; 36: 397–402. doi: 10.1520/JFS13042J [DOI] [PubMed] [Google Scholar]
- 23.Hierholzer J, Cordes M, Tantow H, Keske U, Maurer J, Felix R. Drug smuggling by ingested cocaine-filled packages: conventional X-ray and ultrasound. Abdom Imaging 1995; 20: 333–8. doi: 10.1007/BF00203366 [DOI] [PubMed] [Google Scholar]
- 24.Niewiarowski S, Gogbashian A, Afaq A, Kantor R, Win Z. Abdominal X-ray signs of intra-intestinal drug smuggling. J Forensic Leg Med 2010; 17: 198–202. doi: 10.1016/j.jflm.2009.12.013 [DOI] [PubMed] [Google Scholar]
- 25.Bulakci M, Kalelioglu T, Bulakci BB, Kiris A. Comparison of diagnostic value of multidetector computed tomography and X-ray in the detection of body packing. Eur J Radiol 2013; 82: 1248–54. doi: 10.1016/j.ejrad.2012.12.022 [DOI] [PubMed] [Google Scholar]
- 26.Pinsky MF, Ducas J, Ruggere MD. Narcotic smuggling: the double condom sign. J Can Assoc Radiol 1978; 29: 79–81. [PubMed] [Google Scholar]
- 27.Beerman R, Nunez D, Jr, Wetli CV. Radiographic evaluation of the cocaine smuggler. Gastrointest Radiol 1986; 11: 351–4. doi: 10.1007/BF02035108 [DOI] [PubMed] [Google Scholar]
- 28.Mozes O, Guranda L, Portnoy O, Apter S, Konen E, Amitai MM. Radiographic features of intracorporeally smuggled liquid cocaine. Forensic Sci Med Pathol 2014; 10: 535–42. doi: 10.1007/s12024-014-9607-y [DOI] [PubMed] [Google Scholar]
- 29.Wackerle B, Rupp N, von Clarmann M, Kahn T, Heller H, Feurbach S. Demonstration of narcotic packages in ‘‘body packers’’ by various imaging methods. In vitro and in vivo investigations (Detection of narcotic-containing packages in “body-packers” using imaging procedures. Studies in vitro and in vivo) [in German.] Fortschr Roengenstr 1986; 145: 274–7. doi: 10.1055/s-2008-1048932 [DOI] [PubMed] [Google Scholar]
- 30.Meijer R, Bots ML. Detection of intestinal drug containers by ultrasound scanning: an airport screening tool? Eur Radiol 2003; 13: 1312–5. [DOI] [PubMed] [Google Scholar]
- 31.Chung CH, Fung WT. Detection of gastric drug packet by ultrasound scanning. Eur J Emerg Med 2006; 13: 302–3. doi: 10.1097/00063110-200610000-00012 [DOI] [PubMed] [Google Scholar]
- 32.Cengel F, Bulakci M, Selcuk T, Savas Y, Ceyhan M, Kocak A, et al. The role of ultrasonography in the imaging of body packers comparison with CT: a prospective study. Abdom Imaging 2015; 40: 2143–51. doi: 10.1007/s00261-015-0430-z [DOI] [PubMed] [Google Scholar]
- 33.Horrocks AW. Abdominal radiography in suspected “body packers”. Clin Radiol 1992; 45: 322–5. doi: 10.1016/S0009-9260(05)80084-4 [DOI] [PubMed] [Google Scholar]
- 34.Deuel W, Munch U, Zollinger U, Augustiny N, Siegenthaler-Zuber G, Vetter W. Intestinal drug smuggling—a new diagnostic and therapeutic problem [in German.] Schweiz Rundsch Med Prax 1989; 78: 55–61. [PubMed] [Google Scholar]
- 35.Lee K, Koehn M, Rastegar RF, van Hoorn F, Roy E, Berger FH, et al. Body packers: the ins and outs of imaging. Can Assoc Radiol J 2012; 63: 318–22. doi: 10.1016/j.carj.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 36.Beck NE, Hale JE. Cocaine “body packers”. Br J Surg 1993; 80: 1513–6. doi: 10.1002/bjs.1800801205 [DOI] [PubMed] [Google Scholar]
- 37.Hierholzer J, Tantow H, Cordes M, Maurer J, Keske U, Koch E, et al. X-ray detection of intracorporeal smugglers: Radiologic and legal considerations (Roentgen diagnosis of body packers—radiological and forensic considerations) [in German.] Aktuelle Radiol 1995; 5: 157–60. [PubMed] [Google Scholar]
- 38.Cranston PE, Pollack CV, Jr, Harrison RB. CT of crack cocaine ingestion. J Comput Assist Tomogr 1992; 16: 560–3. doi: 10.1097/00004728-199207000-00011 [DOI] [PubMed] [Google Scholar]
- 39.Hahn IH, Hoffman RS, Nelson LS. Contrast CT scan fails to detect the last heroin packet. J Emerg Med 2004; 27: 279–83. doi: 10.1016/j.jemermed.2004.04.012 [DOI] [PubMed] [Google Scholar]
- 40.Sengupta A, Page P. Window manipulation in diagnosis of body packing using computed tomography. Emerg Radiol 2008; 15: 203–5. doi: 10.1007/s10140-007-0652-7 [DOI] [PubMed] [Google Scholar]
- 41.Asha SE, Cooke A. Sensitivity and specificity of emergency physicians and trainees for identifying internally concealed drug packages on abdominal computed tomography scan: do lung windows improve accuracy? J Emerg Med 2015; 49: 268–73. doi: 10.1016/j.jemermed.2015.02.009 [DOI] [PubMed] [Google Scholar]
- 42.Ziegeler E, Grimm JM, Wirth S, Uhl M, Reiser MF, Scherr MK. Computed tomography scout views vs. conventional radiography in body-packers—delineation of body-packs and radiation dose in a porcine model. Eur J Radiol 2012; 81: 3883–9. doi: 10.1016/j.ejrad.2012.06.030 [DOI] [PubMed] [Google Scholar]
- 43.Flach PM, Ross SG, Ampanozi G, Ebert L, Germerott T, Hatch GM, et al. “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol 2012; 81: 2518–26. doi: 10.1016/j.ejrad.2011.11.025 [DOI] [PubMed] [Google Scholar]
- 44.Schmidt S, Hugli O, Rizzo E, Leopori D, Gudinchet F, Yersin B, et al. Detection of ingested cocaine-filled packets—diagnostic value of unenhanced CT. Eur J Radiol 2008; 67: 133–8. doi: 10.1016/j.ejrad.2007.07.017 [DOI] [PubMed] [Google Scholar]
- 45.Eng JG, Aks SE, Waldron R, Marcus C, Issleib S. False-negative abdominal CT scan in a cocaine body stuffer. Am J Emerg Med 1999; 17: 702–4. doi: 10.1016/S0735-6757(99)90166-3 [DOI] [PubMed] [Google Scholar]
- 46.Leschka S, Fornaro J, Laberke P, Blum S, Hatem A, Niederer I, et al. Differentiation of cocaine from heroin body packs by computed tomography: impact of different tube voltages and the dual-energy index. J Forensic Radiol Imaging 2013; 1: 46–50. doi: 10.1016/j.jofri.2013.03.041 [DOI] [Google Scholar]
- 47.Grimm J, Wudy R, Ziegeler E, Wirth S, Uhl M, Reiser MF, et al. Differentiation of heroin and cocaine using dual-energy CT-an experimental study. Int J Leg Med 2014; 128: 475–82. doi: 10.1007/s00414-014-0980-6 [DOI] [PubMed] [Google Scholar]
- 48.Laberke PJ, Fornaro J, Kim SK, Blum S, Augsburger M, Alkadhi H, et al. Dual-energy CT behavior of heroin, cocaine, and typical adulterants. Forensic Sci Med Pathol 2015; 11: 20–8. doi: 10.1007/s12024-014-9643-7 [DOI] [PubMed] [Google Scholar]
- 49.Maurer MH, Niehues SM, Schnapauff D, Grieser C, Rothe JH, Waldmuller D, et al. Low-dose computed tomography to detect body-packing in an animal model. Eur J Radiol 2011; 78: 302–6. doi: 10.1016/j.ejrad.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 50.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007; 357: 2277–84. doi: 10.1056/NEJMra072149 [DOI] [PubMed] [Google Scholar]
- 51.Poletti PA, Canel L, Becker CD, Wolff H, Elger B, Lock E, et al. Screening of illegal intracorporeal containers (“body packing”): is abdominal radiography sufficiently accurate? a comparative study with low-dose CT. Radiology 2012; 265: 772–9. doi: 10.1148/radiol.12112767 [DOI] [PubMed] [Google Scholar]
- 52.Aissa J, Rubbert C, Boos J, Schleich C, Thomas C, Kröpil P, et al. Low-tube voltage 100 kVp MDCT in screening of cocaine body packing: image quality and radiation dose compared to 120 kVp MDCT. Abdom Imaging 2015; 40: 2152–8. doi: 10.1007/s00261-015-0464-2 [DOI] [PubMed] [Google Scholar]
- 53.Brogdon BG, Vogel H. Search of the person. In: Brogdon BG, Vogel H, McDowell JD, editors. A radiologic atlas of abuse, torture, terrorism, and inflicted trauma. Boca Raton, FL: CRC Press; 2003: 307–13. [Google Scholar]
- 54.Bulakci M, Ozbakir B, Kiris A. Detection of body packing by magnetic resonance imaging: a new diagnostic tool? Abdom Imaging 2013; 38: 436–41. doi: 10.1007/s00261-012-9972-5 [DOI] [PubMed] [Google Scholar]
- 55.Rousset P, Chaillot PF, Audureau E, Rey-Salmon C, Becour B, Fitton I, et al. Detection of residual packets in cocaine body packers: low accuracy of abdominal radiography—a prospective study. Eur Radiol 2013; 23: 2146–55. doi: 10.1007/s00330-013-2798-x [DOI] [PubMed] [Google Scholar]
- 56.Sormaala MJ, Salonen HM, Mattila VM, Kivisaari A, Autti T. Feasibility of abdominal plain film images in evaluation suspected drug smuggler. Eur J Radiol 2012; 81: 2118–21. doi: 10.1016/j.ejrad.2011.08.016 [DOI] [PubMed] [Google Scholar]
- 57.Flach PM, Ross SC, Thali MJ. Forensic and clinical usage of X-rays in body packing. In: Thali MJ, Viner MD, Brogdon BG, editors. Brogdon's forensic radiology. 2nd edn. New York, NY: CRC Press; 2011: 311–34. [Google Scholar]
- 58.Brown JA, Phang PT, Enns R, Butchart MK, Filipenko JD, Mason AC, et al. Computed tomography to detect body packing: an unusual cause of small bowel obstruction. Can Assoc Radiol J 2002; 53: 84–6. [PubMed] [Google Scholar]
- 59.Aldrighetti L, Graci C, Paganelli M, Vercesi M, Catena M, Ferla G. Intestinal occlusion in cocaine-packet ingestion [in Italian.] Minerva Chirurgica 1993; 48: 1233–7. [PubMed] [Google Scholar]
- 60.Hutchins KD, Pierre-Louis PJ, Zaretski L, Williams AW, Lin RL, Natarajan GA. Heroin body packing: three fatal cases of intestinal perforation. J Forensic Sci 2000; 45: 42–7. doi: 10.1520/JFS14639J [DOI] [PubMed] [Google Scholar]
- 61.Cawich SO, Downes R, Martin AC, Evans NR, Mitchell DI, Williams E. Colonic perforation: a lethal consequence of cannabis body packing. J Forensic Leg Med 2010; 17: 269–71. doi: 10.1016/j.jflm.2010.02.012 [DOI] [PubMed] [Google Scholar]
- 62.Johnson JA, Landreneau RJ. Esophageal obstruction and mediastinitis: a hard pill to swallow for drug smugglers. Am Surg 1991; 57: 723–6. [PubMed] [Google Scholar]
- 63.Miller JS, Hendren SK, Liscum KR. Giant gastric ulcer in a body packer. J Trauma 1998; 45: 617–9. doi: 10.1097/00005373-199809000-00037 [DOI] [PubMed] [Google Scholar]
- 64.Cobaugh DJ, Schneider SM, Benitez JG, Donahoe MP. Cocaine balloon aspiration: successful removal with bronchoscopy. Am J Emerg Med 1997; 15: 544–6. doi: 10.1016/S0735-6757(97)90207-2 [DOI] [PubMed] [Google Scholar]
- 65.Schulz B, Grossbach A, Gruber-Rouh T, Zangos S, Vogl TJ, Eichler K. Body packers on your examination table: how helpful are plain X-ray images? A definitive low-dose CT protocol as a diagnosis tool for body packers. Clin Radiol 2014; 69: e525–30. doi: 10.1016/j.crad.2014.08.019 [DOI] [PubMed] [Google Scholar]
- 66.Jones OM, Shorey BA. Body packers: grading of risk as a guide to management and intervention. Ann R Coll Surg Engl 2002; 84: 131–2. [PMC free article] [PubMed] [Google Scholar]
- 67.Farmer JW, Chan SB. Whole body irrigation for contraband bodypackers. J Clin Gastroenterol 2003; 37: 147–50. doi: 10.1097/00004836-200308000-00011 [DOI] [PubMed] [Google Scholar]
- 68.Veyrie N, Servajean S, Aissat A, Corigliano N, Angelakov C, Bouillot JL. Value of a systematic operative protocol for cocaine body packers. World J Surg 2008; 32: 1432–7. doi: 10.1007/s00268-007-9432-5 [DOI] [PubMed] [Google Scholar]
- 69.Stewart A, Heaton ND, Hogbin B. Body packing—a case report and review of the literature. Postgrad Med J 1990; 66: 659–61. doi: 10.1136/pgmj.66.778.659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mandava N, Chang RS, Wang JH, Bertocchi M, Yrad J, Allamaneni S, et al. Establishment of a definitive protocol for the diagnosis and management of body packers (drug mules). Emerg Med J 2011; 28: 98–101. doi: 10.1136/emj.2008.059717 [DOI] [PubMed] [Google Scholar]
- 71.Sporer KA, Firestone J. Clinical course of crack cocaine body stuffers. Ann Emerg Med 1997; 29: 596–601. doi: 10.1016/S0196-0644(97)70246-4 [DOI] [PubMed] [Google Scholar]
- 72.June R, Aks SE, Keys N, Wahl M. Medical outcome of cocaine body stuffers. J Emerg Med 2000; 18: 221–4. doi: 10.1016/S0736-4679(99)00198-5 [DOI] [PubMed] [Google Scholar]
- 73.Jordan MT, Bryant SM, Aks SE, Wahl M. A five-year review of the medical outcome of heroin body stuffers. J Emerg Med 2009; 36: 250–6. doi: 10.1016/j.jemermed.2007.06.022 [DOI] [PubMed] [Google Scholar]
- 74.Yamamoto T, Malavasi E, Archer JR, Dargan PI, Wood DM. Management of body stuffers presenting to the emergency department. Eur J Emerg Med May 2015. Epub ahead of print. doi: 10.1097/MEJ.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 75.Pollack CV, Jr, Biggers DW, Carlton FB, Jr, Achord JL, Cranston PE, Eggen JT, et al. Two crack cocaine body stuffers. Ann Emerg Med 1992; 21: 1370–80. [DOI] [PubMed] [Google Scholar]
- 76.West PL, McKeown NJ, Hendrickson RG. Methamphetamine body stuffers: an observational case series. Ann Emerg Med 2010; 55: 190–7. doi: 10.1016/j.annemergmed.2009.08.005 [DOI] [PubMed] [Google Scholar]