Abstract
The objective of this study is to review the history of daily self-weighing for weight control, discuss the possibility that self-weighing may cause adverse psychological symptoms, and propose mechanisms that explain how self-weighing facilitates weight control. A systematic forward (citation) tracking approach has been employed in this study. In the early literature, experimental tests did not demonstrate a benefit of adding daily self-weighing to traditional behavioral modification for weight loss. More recent studies have shown that daily self-weighing combined with personalized electronic feedback can produce and sustain weight loss with and without a traditional weight loss program. Daily self-weighing appears to be effective in preventing age-related weight gain. Apart from these experimental findings, there is considerable agreement that the frequency of self-weighing correlates with success in losing weight and sustaining the weight loss. The early literature suggested frequent self-weighing may be associated with negative psychological effects. However, more recent experimental trials do not substantiate such a causal relationship. In conclusion, daily self-weighing may be a useful strategy for certain adults to prevent weight gain, lose weight, or prevent weight regain after loss. More research is needed to better understand the role of different types of feedback, who benefits most from self-weighing, and at what frequency.
Keywords: self-weighing, weight loss, adults, behavioral strategies, obesity, psychology, body weight
Introduction
The role of daily1 self-weighing as a viable tool for weight management has been evolving quite rapidly. Until recently, frequent weighing for controlling weight has been discouraged. For years, commercial programs advised against self-weighing more than once a week. Cognitive-behavioral interventions for weight loss recommend at most weekly weighing because of the belief that individuals may be discouraged by negligible losses in their weight over short periods of time (Brownell, 2004; Cooper & Fairburn, 2001, 2002). Even weekly “weigh-ins” at group meetings were believed to motivate people to “beat the scale” by engaging in unhealthful weight control practices leading up to the weight measurement (Heckerman, Brownell, & Westlake, 1978).
However, evidence has been accumulating over the past decades, suggesting that frequent weighing may be a hallmark of successful dieters and weight maintainers and that daily weighing may be useful in preventing weight regain after weight loss and in preventing age-related weight gain.
This article expands a previous review of frequent self-weighing as a technique to control body weight (Vanwormer, French, Pereira, & Welsh, 2008) by utilizing a different systematic search strategy, and both including more recent data as well as providing a historical context for daily self-weighing. We (a) review the early history of frequent self-weighing where the efficacy of frequent self-weighing was examined as an adjunct to weight loss therapies, (b) examine the correlation between frequency of self-weighing and success in producing weight loss and preventing weight gain or regain, (c) review more recent data suggesting that daily self-weighing may be sufficient to produce weight loss and prevent weight gain and regain, (d) discuss possible harmful effects of frequent self-weighing, and (e) offer mechanisms through which frequent weighing may increase the ability to control weight.
Method
A systematic forward tracking of literature published between 1967 and 2013 based on seminal works was conducted. This method was required to identify hard-to-find or obscure publications (Greenhalgh & Peacock, 2005). The preliminary step allowed us to address seminal works on the topic of self-weighing. Once seminal works were identified, their references were tracked until we found the earliest mention of having individuals weigh themselves for the purpose of weight control in the published literature (Stuart, 1967). This work was then forward tracked using multiple databases, including Summon, Google Scholar, and Web of Science, as the latter two draw from different archives. Reference librarians were consulted about the extent of overlap between search engines and obtaining the broadest view possible. In addition to Stuart (1967), Romanczyk (1974) was fully forward tracked. This particular article was cited 7 times in Scopus (Summon), 55 times in Web of Science, and 79 times in Google Scholar, reinforcing the importance of using multiple databases.
We examined every citing work when forward tracking. If the title and abstract described a type of self-monitoring other than self-weighing (e.g., cigarette smoking cessation) or the article was about subjects outside the scope of this review (e.g., participants were children or animals), the reference was excluded. We included articles that were written in English and peer-reviewed, considering conference abstracts along with theses and dissertations. If the article passed these initial criteria, we searched for “weigh” or “weighing” to determine the context in which weighing was discussed. The place where the article cited the seminal work (e.g., Romanczyk, 1974; Stuart, 1967) was identified to determine accuracy and context of the citation. Articles not available online were requested through the Cornell Library, or located in their original place of hardcopy publication and scanned. Theses and dissertations were examined and microfilm was used to determine if these works added additional information. All articles were forward and backward tracked to see if any new relevant references appeared. By the end of the search, no new articles were found, indicating that a thorough review of the printed published literature had been conducted.
Results and Discussion
Findings from the published studies are summarized in Table 1, organized by whether they had the objective of weight loss, prevention of weight regain, or prevention of weight gain.
Table 1.
Summary of Studies Providing Information on Self-Weighing in Adults With and Organized by Weight Objective.
| Authors and year | Study design | Intervention | Sample | Total N | n per group | Duration | Results |
|---|---|---|---|---|---|---|---|
| Weight loss | |||||||
| Stuart (1967) | Case studies | Self-weighing 4 times/day, additional behavioral techniques | Not specified; 8 women, obese | 8 | 12 months | Mean weight loss 0.75 lb/week through treatment | |
| Romanczyk, Tracey, Wilson, and Thorpe (1973) | RCT: Sequential dismantling; 7 groups | Community; SNS; ≥15 lb overweight | 102 | 14–15 | 4 weeks before starting “program” | Delayed tx group that self-weighed and charted did not lose weight | |
| Romanczyk (1974) | RCT: Sequential dismantling; 5 groups | Community; SNS; ≥15 lb overweight | 70 | 14 | 4 weeks before starting “program” | Delayed tx group that self-weighed and charted did not lose weight | |
| Mahoney (1974) | RCT; 4 groups |
|
Community; 46 women; 20% overweight | 49 | 11–14 | 2 week baseline period | Self-monitored group did not differ from controls, whereas other two groups lost significantly more weight |
| Mahoney, Moura, and Wade (1973) | RCT; 5 groups |
|
Community; 48 females and 5 males; 48.6% overweight | 53 | 5–16 | 4 weeks | Self-monitoring group (Group 4) lost significantly less weight than the self-reward group (1) and lost the least amount of weight than any of the groups. |
| Heckerman, Brownell, and Westlake (1978) | RCT; 2 groups |
|
Not specified; 20 women; 15 lb or 15% overweight | 23 | 11, 12 | 10 weeks treatment | No significant difference in weight change between groups |
| Linde, Jeffery, French, Pronk, and Boyle (2005) | Cohorta (RCT; 3 groups) |
|
Membership in managed care organization; 1,292 women; BMI ≥ 27.0 kg/m2 | 1,800 | NA | 2 years | Change in weighing frequency significantly p < .0001 associated with weight change—daily associated with loss independent of demographics, tx group, or relevant behaviors (p = .213) |
| VanWormer, Martinez, Benson, et al. (2009) | Cohort | Daily self-weighing on tele-scale, 10 counseling sessions with dietitian, manual | BMI >31 kg/m 2. 91 women | 100 | NA | 6 months treatment, 12- month follow- up without tele-scale | Significant weight loss after 6 months (p < .001), but not at 18- month follow-up |
| Gokee-LaRose, Gorin, and Wing (2009) | RCT; 2 groups; |
|
Community; BMI 27–40 kg/m2 | 40 | 21, 19 | 10 weeks | Both groups had significant weight loss; no difference between groups |
| Oshima, Matsuoka, and Sakane (2013) | RCT; 2 groups; |
|
BMI ~27 kg/m 2, 29 women | 56 | 28, 28 | 12 weeks | Both groups had significant weight loss; Group 2 more than Group 1 (p < .05). |
| Steinberg et al. (2013) | RCT; 2 groups |
|
Overweight, 68 women | 91 | 47, 44 | 6 months | The treatment led to significantly greater weight loss at 6 months compared with controls (p < .001) |
| Prevention of weight regain | |||||||
| Fujimoto et al. (1992) | RCT; 2 groups; | Weighing 4 times/day
|
Hospitalized moderately obese patients; 74 female—all 15 males in charting condition | 89 | 72 (57 female + 15 male); 17 | ≥ 2 years after | No weight regain in group that charted; weight regain in those that charted (females only) |
| Klem, Wing, McGuire, Seagle, and Hill (1997) | Cohort | National Weight Control Registry; 629 women; lost ≥ 30 lb and maintained loss ≥1 year | 784 | NA | Average time weight loss maintained = 5.5 years | 38% weigh daily; 75% ≥ 1x/week | |
| Wing, Tate, Gorin, Raynor, and Fava (2006) |
Cohorta RCT; 3 groups |
|
Community and weight loss programs; 255 women; lost ≥10% body weight in last 2 years | 314 | 104–105 | 1.5 years | Proportion of participants regaining ≥ 5 lb significantly lower in daily weighers compared with less frequent weighers in Internet and face to face but not control groups |
| Prevention of weight gain | |||||||
| Jeffery and French (1997) |
Cohorta RCT; 3 groups; |
|
Community; 594 women; no body weight criterion | 822 | NA | 3 years | Increases in weighing frequency related to < wt gain in all groups (r from −0.14 to −0.21; p < .05) |
| Levitsky, Garay, Nausbaum, Neighbors, and Dellavalle (2006) | RCT; 2 groups |
|
Freshman university students; 75 women; no body weight criterion | 34; 41 (replicated trial on separate year) | 11, 15 (after dropout); 16, 16 (after dropout) | 10 weeks | Experimental groups did not gain weight (p significantly different from 0) control groups gained 6.8, 4.4 lb, respectively. |
| VanWormer, Linde, Harnack, Stovitz, and Jeffery (2012) | Cohort | Worksite | 1,122 | 2 years | Weight reduction among obese daily self-weighers, better weight control with more frequent self- weighing | ||
Note. Studies such as Strimas and Dionne (2010) and Gow, Trace, and Mazzeo (2010) were not included because no direction was given with regard to weight (e.g., prevent weight gain, lose weight). Community sample—those responding to a public advertisement. RCT = randomized controlled trial; SNS = sex not specified; Tx = treatment; BMI = body mass index.
If study design is italicized, this describes how the sample was used for these analyses. The intended study design is presented in parentheses.
Early Attempts to Examine Frequent Self-Weighing to Facilitate Weight Loss
In 1967, Stuart’s manuscript titled, “Behavioral Control of Overeating,” claimed patients encountered moderate weight loss success. As part of a behavioral plan to lose weight, he had patients weigh themselves 4 times a day (Stuart, 1967). In addition, weight was charted over time to visualize progress. Based on behavioral theory, weighing was thought to serve as a mildly aversive stimulus and a reinforcer by helping patients notice deviations in their weight throughout the day. This cognitive awareness was believed to assist participants in stabilizing their eating patterns by showing direct evidence of the effect of eating and drinking on their weight. Stuart believed that this would minimize overeating, and remind patients of the weight loss program in which they were enrolled.
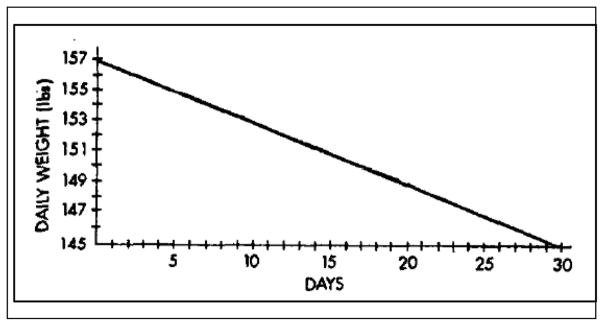
Soon after Stuart’s behavioral approach was published, Fisher, Green, Friedling, and Levenkron (1976) published the first clinical study on the effectiveness of self-weighing to produce a weight loss. They reported the weight loss of 11 case studies in which participants were instructed to weigh themselves daily and graph their weight on a chart. The graph also contained a line connecting the subjects’ starting weight to a goal weight approximately 8 to 12 lb lower than their starting weight over the course of about 30 days. Figure 1 is taken from the original publication. The descending line on the graph started 2 lb above the participants’ starting weight and continued diagonally to their target weight to give the participants a sense of success at the beginning of treatment. Participants were not given specific dietary or physical activity instructions but were simply told to graph their weight daily on this chart and to try to keep their weight below the sloped goal line. Ten of the 11 participants lost an average of 9.6 lb over a period of 39 days.
Figure 1.
Graph indicating rate of weight loss on which participants were supposed to plot their daily weight.
Although the results of Fisher et al.’s (1976) publication seemed to substantiate daily self-weighing as a technique to aid weight reduction, this information was based on case studies. Because no control group was used, a causal inference cannot be made as to the effectiveness of self-weighing. A few years later, Loro, Fisher, and Levenkron (1979) performed one of the first experimental tests of the effectiveness of self-weighing as an adjunct to other behaviors to facilitate weight loss. They compared three different treatments: (a) one focused on controlling eating in response to external eating cues, (b) one focused on changing eating behavior, and (c) one centered on enabling participants to initiate their own treatment. This self-initiated treatment group was given an informational booklet about self-control and instructed to employ daily weighing and charting using a personalized target weight line similar to that used by Fisher et al. cited above. All participants signed treatment contracts, made refundable preprogram deposits prior to treatment to minimize attrition, and received group counseling and nutrition information. The participants in eating behavior control groups were also asked to weigh and graph their weight daily, but their graph did not contain the line representing the targeted rate of weight loss. Later, adding the target weight to the graph had no effect on the average amount of weight lost. In fact, after 6 weeks, no difference in weight loss between any of the three treatments was observed.
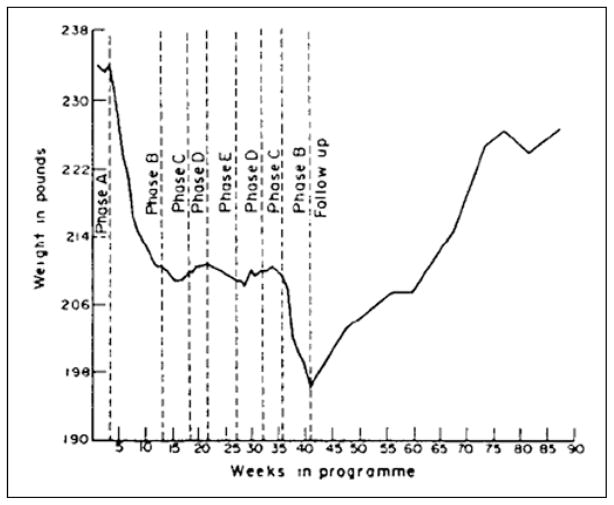
Stuart’s “weighing four times a day and graphing” approach was further tested along with other self-monitoring techniques in a clinical study of a mildly retarded adult female conducted in a residential training center (Joachim, 1977). The study was divided into nine phases as indicated in Figure 2. In Phase B, the patient weighed herself 4 times a day and recorded the time, the amount, and the circumstances during which she ate or drank—a procedure modeled after Stuart. Phase B resulted in the greatest weight loss (21 lb in 10 weeks). Then, in various phases, portions of the behavioral program were eliminated, except for the frequent weighing, to estimate the contribution of each strategy to the overall effectiveness of frequent weighing. Although none of the aspects of behavioral modification had an appreciable effect on body weight, weight regain was successfully prevented. Reimposing all of the elements of the original behavioral modification procedure (Phase B) again seemed to stimulate further weight loss. Interestingly, when all treatments were terminated, including the frequent self-weighing, at 40 weeks, weight returned to its pretreatment level.
Figure 2.
Mean body weight as a function of time and phase.
Source. Joachim (1977).
Using a more conventional experimental design, Mahoney, Moura, and Wade (1973) compared self-weighing with other behavioral treatment methods used to help obese patients lose weight. The five strategies studied included (a) self-reward, (b) self-punishment, (c) self-reward and self-punishment, (d) self-monitoring, and (e) an information control group. Groups (a–d) were instructed to weigh themselves daily and chart their weight. Participant’s weight was measured twice a week by the experimenters. The self-reward and self-punishment groups used financial incentives as motivational strategies in addition to the self-weighing. At the end of 4 weeks, the weight loss of the self-monitoring group was significantly less than the self-reward group. There was no mention of whether the weight loss of the self-monitoring group (which included self-weighing) was different from the control group. Mahoney and colleagues found weight loss of the self-monitoring group to be less than half of what was achieved by two self-reward groups (one self-reward and one self-reward plus self-punishment) after 4 months. Thus, the results of this study suggest that self-weighing by itself, without the use of either self-reward or self-punishment, does not produce a significant weight loss.
The lack of effectiveness of self-weighing compared with other kinds of self-control techniques used to promote weight loss was corroborated in a succeeding study by Mahoney (1974). Using obese patients, he compared the following interventions: (a) self-reward for weight loss, (b) self-reward for habit improvement, (c) self-monitoring, and (d) a delayed treatment control group. Similar methods as outlined in the previous study were used to produce the groups. All three groups lost significantly more weight than the self-monitoring group, the group that used daily self-weighing.
Similarly, Romanczyk (1974) found that frequent self-weighing did not enhance behavioral modification techniques to facilitate weight loss in a group of overweight people. His study was designed to differentiate between the relative contributions of (a) no treatment, (b) self-weighing, (c) self-monitoring caloric intake and self-weighing, (d) behavior management and stimulus control, and (e) behavior management and stimulus control with self-weighing and self-monitoring caloric intake. Adding self-weighing to weight reduction treatments offered no benefit to any the weight loss procedures under any condition. Although not tested statistically, it is interesting to note that controls gained about 0.5 lb during the 4-week trial, whereas the group instructed to only weigh themselves gained 0.09 lb during this period. Much of the same data were published a year earlier (Romanczyk, Tracey, Wilson, & Thorpe, 1973).
Heckerman et al. (1978) also reported the inability of self-weighing to enhance weight loss among a group of overweight participants. They tested whether it was more beneficial for people who wanted to lose weight to focus on their weight or to focus on the behaviors that determine their weight such as eating and exercise. They directed participants to either weigh themselves daily or to avoid weighing themselves between the weekly weigh-ins. Instead of focusing on their weight, the latter group was asked to focus on making behavioral changes for the 10 weeks of the weight loss study. All participants were weighed weekly. Both groups lost a significant amount of weight. Frequent weighing did not facilitate weight loss compared with weekly weighing at 2.5 months (intervention) or at follow-up at 3.5 months and 6 months.
Quayle and Powers (1979) examined the use of daily weighing and charting of weight as part of a sequence of strategies used for weight reduction in six overweight students. The daily weight monitoring stage lasted for a minimum of 2 weeks, with participants moving to the next stage when their weight was stable. Significant weight loss was not observed in any of the participants for the weight monitoring stage (average weight change −0.2 lb). However, when an additional self-monitoring technique, self-recording of bites, was introduced, an increase in weight loss (−2.9 lb) emerged.
A clinical study of the use of multiple weigh-ins within a day to prevent weight regain was reported by Fujimoto et al. (1992). Like Stuart’s (1967) original report, Fujimoto et al. had one group of subjects weigh themselves 4 times each day. This group and a control group (no weighing) received 8 months of behavioral modification. They observed no statistical difference in rate of weight loss in the two groups.
The preponderance of evidence up to the early 1990s did not support the idea that the addition of self-weighing to standard weight loss techniques enhances weight loss beyond the loss the techniques themselves produce.
Daily Self-Weighing With Personalized Messaging to Promote Weight Loss
Contrary to lack of support for daily self-weighing as an adjunct to traditional weight loss methods as discussed, more recent evidence suggests that daily self-weighing combined with other aids may be effective in producing a weight loss. VanWormer, Martinez, Benson, et al. (2009) randomized a group of participants from a large managed health care organization into an intervention group and 6-month delayed intervention group. The intervention consisted of daily self-weighing (weight was transmitted via Internet to a website), the use of food and activity logbooks, observing a weekly weight chart, and using an action planner and a digital pedometer. Participants also had access to up to 10 telephone consultations with a weight control consultant. Over the first 6 months, the intervention group lost 7.5 ± 1.5 lb while the nonintervention control group’s loss was statistically insignificant, 1.3 ± 1.4 lb. More important, the intervention group maintained this weight loss over the next 12 months.
Steinberg et al. (2013) randomized adult overweight participants into two groups. The intervention group was (a) given an Internet-based scale and asked to weigh daily, (b) sent an updated chart of their weight daily, (c) given personalized suggestions to lose weight weekly, and (d) given 22 weekly weight control lessons transmitted over the Internet. The control group received no intervention during the 6-month trial period. The results indicated the intervention group lost considerably more weight (6.55%, 95% confidence interval [CI] = [−7.7, −5.4]) than the controls (0.35%, 95% CI = [−1.5, 0.79]).
Bertz et al. (2012) randomized overweight and obese postpartum women to diet only, exercise only, diet and exercise combined treatment, or control, in a 12-week treatment followed by a 9-month follow-up period. The women receiving the two dietary treatments were provided with scales and instructed to weigh at least 3 times per week during the 12-week treatment. They received individual dietary counseling on two occasions for a total of 2.5 hr. The dietary modification treatment was designed to integrate self-weighing in two ways. First, guided by their weight readings, the women were advised to introduce four key dietary modifications, one at a time, at a pace that facilitated a weekly weight loss goal of 0.5 kg. Second, the women were contacted biweekly with cell phone text messages to report and receive feedback on body weight change. After the 12-week treatment, the dietary treatments resulted in ~10% weight loss, and more important, this weight loss was sustained during the 9 months following treatment termination (main effect of dietary treatment p < .001 at both times).
In the three more recent studies cited above, although weight loss was produced, the effects of daily self-weighing cannot be separated from the accompanying aids such as tailored advice or feedback.
Daily Self-Weighing Combined With Electronic Feedback Only to Promote Weight Loss
Oshima, Matsuoka, and Sakane (2013) randomized overweight Japanese adults into two groups. One group was instructed to weigh themselves daily while the second group was asked to weigh themselves twice a day, once immediately after rising from bed then again immediately before going to bed at night. This group also viewed an updated chart of their weight that exhibited the difference between their targeted weight and actual weight on a LCD screen attached to scale. Both groups lost a significant amount of weight after the 12-week trial period. However, the group who weighed themselves twice a day and viewed a chart of their weight lost significantly more weight (2.7 ± 9.1 kg) than the group that weighed themselves once each day (1.0 ± 1.4 kg; p < .05).
In a recently completed PhD thesis, Pacanowski had participants self-weigh and enter their daily weight into a website. The website retuned a graph of their weight and, after eight entries, included a horizontal line representing their starting weight. Once the participants’ daily weight was stable, the line was lowered by 1% of their starting weight and participants were asked to decrease energy intake or increase energy expenditure to reach the horizontal line. Again, when their weights stabilized around the line, the line was lowered by another 1%. This process continued until the participants reached 10% weight loss. They were then instructed to maintain that weight loss for 1 year. The technique resulted in statistically significant weight loss of 5.7 lb compared with a nonsignificant gain of 1.0 lb in the control group. More importantly, like the VanWormer, Martinez, Benson, et al. (2009) study, the weight loss was sustained for 1 year following the intervention.
In summary, recent studies have shown that daily self-weighing combined with electronic feedback only can produce a small but sustained weight loss.
Self-Weighing as a Correlate of Weight Control
Jeffery et al. (1984) offered another approach to the evaluation of daily self-weighing. They examined the behavior of a group of middle-aged men who completed a 15-week weight reduction treatment with a 2-year follow-up by using questionnaires. The more frequently the men reported having weighed themselves, the more successful they were at losing weight. Even more impressive was the observation that those who reported weighing themselves more frequently maintained their weight loss better 1 year after completing the weight loss treatment, than those who weighed themselves less frequently, though the difference disappeared by the end of the second year.
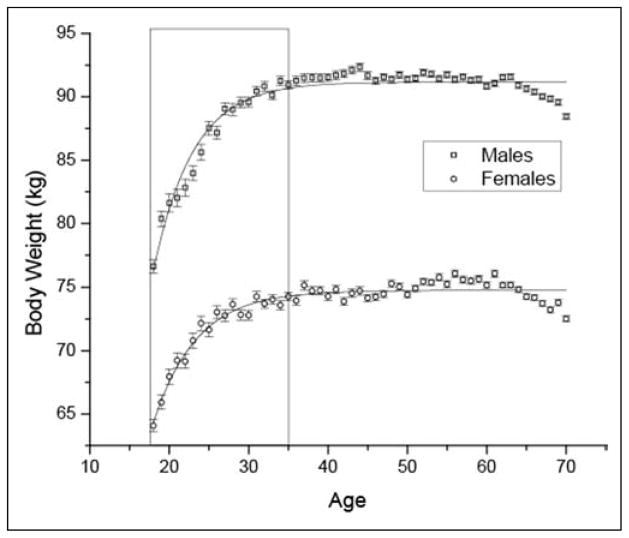
The relationship between the frequency of self-weighing and success at weight control was substantiated by a later study by Jeffery and French (1997) in which researchers attempted to prevent age-related weight gain. Age-related weight gain is the observed increase in body weight with age once maximum height has been reached. As indicated in Figure 3, it continues from late adolescence until about the age of 40. Jeffery and colleagues randomly assigned participants to one of three conditions. Two of the intervention groups received educational information through a newsletter describing techniques to avoid gaining weight. The information focused on five strategies, one of which was weighing (at least once a week). One of these two intervention groups received the same information but, in addition, was offered a prize (incentive) for following the instructions. The third group acted as a nonintervention control group. The participants were examined at the end of 1 year. None of the procedures effectively prevented age-related weight gain. However, an analysis of the aggregated data, regardless of treatment group, indicated that the more frequently participants reported having weighed themselves, the less weight they gained (r values −.14 to −.21; p values < .05). This negative correlation between frequency of self-weighing and weight gain remained highly significant (p < .01) for each of the 3 years of the study, Year 1 (−0.16), Year 2 (−0.15), Year 3 (−0.11), as well as over the entire 3-year examination period (−0.11).
Figure 3.
Increase in body weight as a function of age and gender.
In the same year, researchers reported the results from a group of exceptional individuals. Self-enrolled members of the National Weight Control Registry (NWCR) had to verify that they lost at least 30 lb and successfully maintained this weight loss for at least 1 year. An examination of the behaviors of this group revealed that 75% of the successful weight loss maintainers reported that they weighed themselves at least once per week (Klem, Wing, McGuire, Seagle, & Hill, 1997). This high rate of self-weighing was confirmed 10 years later in a larger study of the participants in the NWCR where 79% of successful weight maintainers reported that they weighed themselves at least once a week (Butryn, Phelan, Hill, & Wing, 2007).
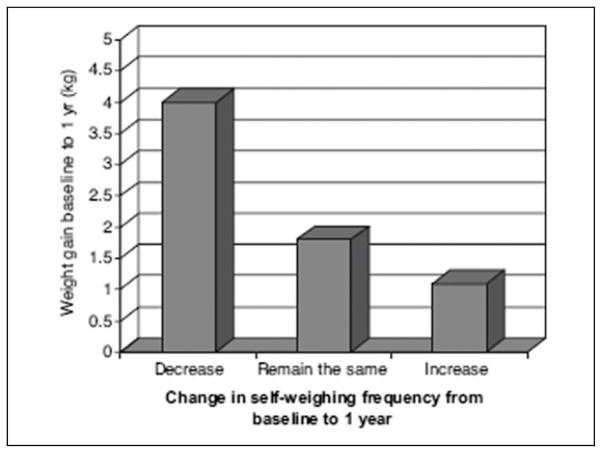
Succeeding examinations of the NWCR and other data corroborated this relationship between successful maintenance of weight loss and the frequency of self-weighing. In a large telephone survey of the U.S. population, McGuire, Wing, and Hill (1999) confirmed that the frequency of self-weighing in successful weight loss maintainers was significantly greater than in the population at large (55.1% and 34.5%, respectively; McGuire et al., 1999). This comparison was important because the studies of the NWCR did not have an estimate of the frequency of weighing among controls or people who did not lose weight. Moreover, from the telephone survey, it was observed that people who tried to lose weight but regained their weight, reported a significantly lower rate of self-weighing (35.7%) than the successful weight loss maintainers, a finding very similar to that observed by the follow-up of the NWCR as depicted in Figure 4 (Butryn et al., 2007).
Figure 4.
Mean weight gain as a function of change in the frequency of weighing.
McGuire et al. (1999) also found that those who decreased their frequency of self-weighing gained more weight than those who increased their frequency of self-weighing. These results, however, appear to conflict with the findings of Kayman, Bruvold, and Stern (1990), who reported no difference in the reported frequency of self-weighing between a group of weight maintainers and a group of weight regainers (Kayman et al., 1990). However, Kayman’s sample size was small (n = 64) compared with the NWCR (n = 3,003) and his response measure was dichotomous (watches weight on scale: yes/no) rather than offering more than two categories.
More recently, Linde, Jeffery, French, Pronk, and Boyle (2005) found a significant correlation between frequency of weighing and success in maintaining body weight. They examined the behavior of successful and unsuccessful obese participants in a large-scale weight loss study (Weigh-To-Be) and a large weight maintenance study (Pound-of-Prevention). They observed, “… regular self-weighing of at least weekly frequency was associated with lower BMI and greater weight losses over time in these two groups” (Linde et al., 2005, p. 214). Although the frequency of self-weighing was associated with other healthy behaviors such as eating less fat, increasing exercise, and not smoking, when these variables were controlled in their statistical models, the effect of frequent self-weighing remained.
A similar correlation between frequency of weighing and success with weight control was found in a group of obese adults by VanWormer, Martinez, Martinson, et al. (2009). Frequency of self-weighing was a significant predictor of the amount of weight lost during the 6 months of weight loss treatment. By the termination of treatment, the percentage of participants who lost at least 5% of their weight was significantly higher in those who weighed themselves at least weekly (46%) compared with those who weighed themselves less than weekly (8%); this difference disappeared 1 year later.
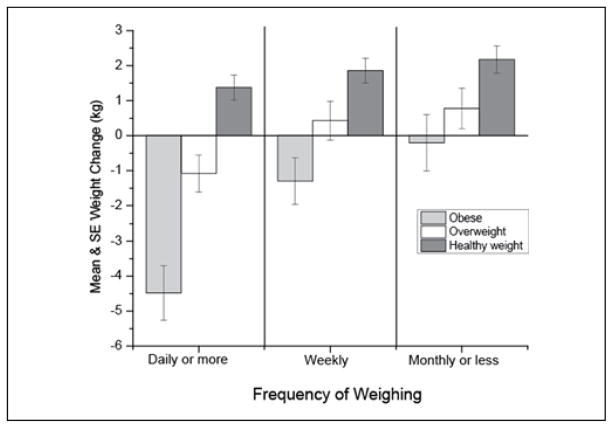
VanWormer, Linde, Harnack, Stovitz, and Jeffery (2012) also examined the effects of the introducing daily self-weighing in a workplace environment. By utilizing a health care system called Healthworks, VanWormer and colleagues studied 1,747 employees in six worksites. Researchers introduced a program delivering information about health, diet, and exercise and installed a number of scales in the workplace. Aggregate weight data was provided in monthly newsletters. At the end of 2 years, weight data and frequency of weighing was collected and analyzed; data are presented in Figure 5. Not only was there a significant correlation between the frequency of self-weighing and the prevention of weight gain but also the greater the initial body weight, the greater the suppressing effect of self-weighing on weight gain prevention.
Figure 5.
Change in weight as a function of the frequency of weighing for healthy weight, overweight, and obese participants.
Source. VanWormer, Linde, Harnack, Stovitz, and Jeffery (2012).
Studies evaluating self-weighing as a correlate of weight control were fairly consistent in demonstrating a relationship between frequency of self-weighing and weight control. However, all confounded daily self-weighing with additional intervention factors and were correlational in nature. Because they were correlational, it is difficult to draw the causal inference that the act of self-weighing is responsible for improved weight control. It is equally as valid to conclude that personal motivation prompted individuals to control their weight as it is to conclude that frequent self-weighing enabled them to control their weight. However, even as correlations, these findings support the relationship between frequent self-weighing and weight control.
Self-Weighing and Prevention of Weight Regain
The studies cited above all aimed at producing a weight loss. However, the major problem with programs aimed at producing weight loss is not that they cannot produce weight loss, but rather their inability to help people sustain weight loss (J. W. Anderson, Konz, Frederich, & Wood, 2001). One of the first attempts specifically examining the effects of self-weighing to prevent weight regain was performed by Wing, Tate, Gorin, Raynor, and Fava (2006). They conducted a randomized controlled trial, using participants who had already lost at least 10% of their body weight in the past 2 years (Wing et al., 2006). Participants were randomly assigned to one of three groups: a face-to-face intervention, an Internet intervention, or a control group (received quarterly newsletters). Both intervention groups were provided with a scale and instructed to monitor their weight daily and report back to the researchers weekly. In addition, the participants were rewarded for preventing weight regain. They were also instructed to resume weight loss behaviors if they regained more than a specified amount of weight. Participants in each of the intervention groups who reported weighing themselves daily were significantly less likely to regain weight than those who reported weighing less frequently after a year and a half of the trial (Wing et al., 2006). Because participants who weighed themselves also received additional nutritional advice, it is not possible to attribute the success of this group solely to self-weighing.
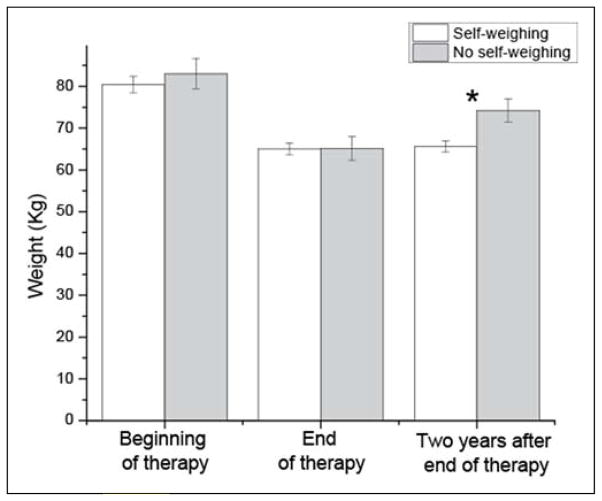
As stated above, Fujimoto et al. (1992) did not find an advantage of adding daily weighing to a behavioral weight loss program in losing weight. However, they continued to follow the participants after the treatment was completed. As shown in Figure 6, 2 years following the termination of behavioral therapy, the group that continued weighing themselves did not regain the lost weight, whereas the nonweighing control group regained about half of the weight lost during therapy.
Figure 6.
Mean body weight of a group of patients who lost weight through behavioral modification therapy and followed up for 2 years.
Source. Fujimoto et al. (1992).
Note. One group weighed themselves several times daily while the other group did not.
*p < .05.
Gokee-Larose, Gorin, and Wing (2009) randomized young adults into two groups, a behavioral self-regulation group or a standardized behavioral treatment group. Both underwent 10 group sessions of behavioral modification during which they lost about the same amount of weight. Following the weight loss sessions, one group was asked to weigh themselves daily and use the weight information to make adjustments in their subsequent energy intake or expenditure behaviors while the other group was asked to weigh weekly but not to focus on their weight. At the end of the 10 weeks of maintenance, participants in the daily weighing group continued to lose weight (−0.18 kg), whereas those in the weekly weighing group regained some weight (+0.37 kg; Gokee-Larose et al., 2009). The sample size was too small and/or the length of the maintenance period was insufficient (10 weeks) to allow the difference to be statistically significant, if a true difference was observed. Interestingly, at the postintervention follow-up (20 weeks) about 70% of the participants in the daily weighing group reported that they continued to weigh themselves daily, whereas only about 17% of those in the weekly weighing group continued the behavior postintervention.
These studies corroborate the idea that although daily self-weighing may not produce a large weight loss, it may play a role in the prevention of weight regain.
Self-Weighing and the Prevention of Age-Related Weight Gain
As illustrated in Figure 3, body weight accumulates throughout most of life. It is perhaps most conspicuous in college freshman (D. A. Anderson, Shapiro, & Lundgren, 2003; Butler, Black, Blue, & Gretebeck, 2004; Cooley & Toray, 2001; Delinsky & Wilson, 2008; Economos, Hildebrandt, & Hyatt, 2008; Edmonds et al., 2008; Hajhosseini et al., 2006; Hivert, Langlois, Berard, Cuerrier, & Carpentier, 2007; Hoffman, Policastro, Quick, & Lee, 2006; Holm-Denoma, Joiner, Vohs, & Heatherton, 2008; Hovell, Mewborn, Randle, & Fowler-Johnson, 1985; Hull, Morrow, Dinger, Han, & Fields, 2007; Hull, Morrow, Heesch, et al., 2007; Jung, Bray, & Martin Ginis, 2008; Kasparek, Corwin, Valois, Sargent, & Morris, 2008; Levitsky, Halbmaier, & Mrdjenovic, 2004; Lloyd-Richardson, Bailey, Fava, & Wing, 2009; Lowe et al., 2006). Levitsky, Garay, Nausbaum, Neighbors, and Dellavalle (2006) took advantage of this natural weight gain to test the efficacy of using self-weighing as a means of preventing freshman weight gain. They conducted two studies, 1 year apart, in which freshmen females were randomized to a control or experimental group and tracked for the first 4 months (first semester) of their undergraduate experience. The experimental participants were given digital bathroom scales, asked to weigh themselves the first thing every morning, and then email their weight to the researchers daily. On a weekly basis, the freshmen received a graph of their weight containing daily weights and a regression line of the last 7 points (days). The only instructions given were to try to maintain the slope of the line as close to zero as possible to keep their weight at or below their starting weight. A matched group of controls were measured at the beginning and end of the semester. Change in weight by group over the first semester is displayed in Figure 7. The mean change in body weight of the experimental group was not significantly different from zero, whereas the control group gained about 3 kg in the first study and about 2 kg in the second study (Levitsky et al., 2006), both values significantly different than zero.
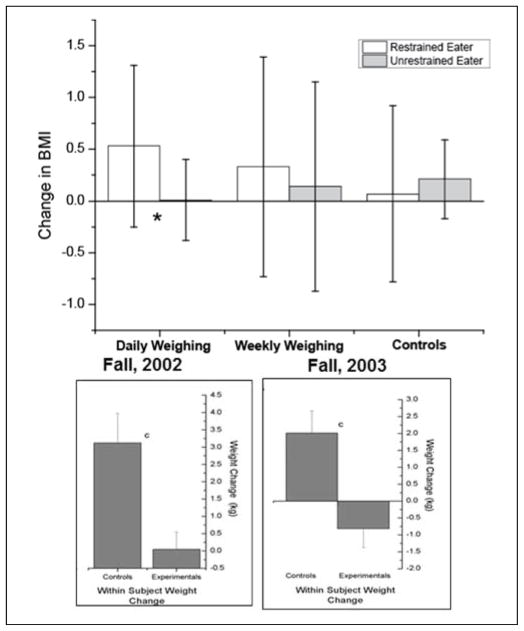
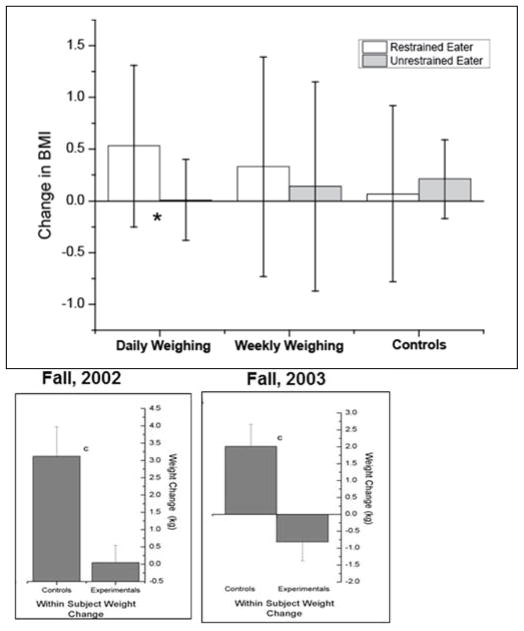
Figure 7.
Weight change in restrained and unrestrained participants as a function of the frequency of self-weighing.
Source. Strimas and Dionne (2010).
*p < .05.
Gow, Trace, and Mazzeo (2010) also examined the effectiveness of self-weighing to prevent weight gain in first-year college students. Intervention effects were evaluated by comparing (a) an education group, (b) an education and weight feedback group (where participants self-weighed weekly and emailed the principal investigator [PI] similar to the method used in Levitsky et al., 2006), and (c) a weight feedback only group (weighed weekly and emailed the chart of their weight) during a 6-week intervention. A significant body mass index (BMI) change was found between the combined intervention (weight change −0.12 ± 2.92 kg) and the other groups, but contrary to the findings of Levitsky et al. (2006), there was no significant benefit of either the feedback (weight change 1.20 ± 2.55) or Internet education (weight change 1.47 ± 3.22) alone as compared with the control group (weight change 1.04 ± 3.45). One possible reason for this lack of effect to prevent weight gain was that no statistically significant weight gain was found in the control group, most likely because insufficient time (6 weeks) was allowed for significant weight gain among the controls to occur.2
Strimas and Dionne (2010) also examined the effects of daily weighing on the prevention of gain in weight in freshmen, focusing on detecting possible negative effects on restrained eaters. One of the authors had published a warning of the dangers of self-weighing several years earlier (Dionne & Yeudall, 2005). Student volunteers from an introductory psychology course were randomly allocated to (a) daily weighing group, (b) a weekly weighing group, or (c) a control group and asked to monitor their heart rate once a week. These three groups were further subdivided into an approximately equal number of restrained and unrestrained eaters using the Herman and Polivy (1980) Restraint Scale. It is important to note that participants were not instructed to resist gaining weight or to maintain a record of their weight. The results of the effect of the various conditions on a change in BMI are shown graphically in Figure 8. No main effect of group, restraint, or time (beginning vs. end of the semester) was observed. The only subset of participants that demonstrated a statistically significant change in BMI over the semester was the restrained eaters in the group who were required to weigh themselves daily; they gained 0.53 BMI units. Although these results must be taken seriously because they may point out a danger of frequent self-weighing for particular segments of the population (see section below for further discussion), this is the first observation that daily self-weighing may cause a weight gain.
Figure 8.
Change in body weight of students given scales to weigh themselves daily and their controls in two experimental studies.
Source. Levitsky, Garay, Nausbaum, Neighbors, and Dellavalle (2006).
The experimental evidence that self-weighing prevents age-related weight gain is inconclusive. Levitsky et al. (2006) successfully blocked weight gain, whereas two other studies utilizing frequent self-weighing did not. In these latter studies, the participants were not motivated or instructed to maintain weight, nor provided with a target weight or electronic graphic feedback, which may be crucial components to achieve the prevention of weight gain.
Summary of Role of Daily Weighing in the Control of Body Weight
From the evidence presented above, it appears that (a) daily weighing does not facilitate further weight loss when added to traditional methods of weight loss; (b) the frequency of weighing correlates with successful weight loss and weight maintenance; (c) daily weighing when either combined with or without electronic messaging can produce a small, but significant weight loss; (d) daily weighing appears to be effective in inhibiting weight regain after weight loss; and (e) daily weighing combined with graphic feedback appears to inhibit age-related weight gain.
One limitation of this research on self-weighing, however, that impedes acceptance of daily self-weighing as an effective method to control body weight is that in most studies where the effect of self-weighing is experimentally examined, the participants knew that their weight was being monitored. There is evidence showing that weight control is enhanced when people know they are being observed compared with when they think they are not being observed (Harvey-Berino, Pintauro, & Gold, 2002; Tate, Jackvony, & Wing, 2003, 2006; Tate, Wing, & Winett, 2001). Therefore, it is not clear how much of the effectiveness of frequent self-weighing is due to the act of self-weighing and how much is due to the realization that someone else was watching their weight.
It is important to note the sample size of studies on self-weighing. More research is necessary to determine the appropriate frequency of weighing for different weight control states (loss, prevention of regain, maintenance) and also to assess the relationship between weight status (normal weight, overweight, obese) and weighing. There are many factors yet to be explored to identify categories of individuals who might benefit from daily weighing (e.g., personality facets, temperament).
Potential Hazards of Frequent Weighing
Concerns have been raised about the safety of daily self-weighing and the potential of causing eating disorders. Ogden and Whyman (1997) were the first to suggest an adverse consequence of frequent self-weighing in the published literature. They concluded from a small study of undergraduates that “subjects who weighed themselves every day for 2 weeks reported deterioration in mood in terms of increases in both anxiety and depression” (p. 128). Fifteen years later, Mercurio and Rima (2011) reported higher body dissatisfaction in participants in the frequent self-weighing group.
In Mercurio and Rima’s study, the dependent variable examined was a measure of body dissatisfaction. However, an earlier study by Ogden and Evans (1996) also measured body dissatisfaction, but found no change in body dissatisfaction following 2 weeks of self-weighing. Similarly, in 2009, Welsh, Sherwood, VanWormer, Hotop, and Jeffery failed to find any difference in the change in body dissatisfaction in a group of dieters who weighed themselves frequently compared with a group who weighed themselves less frequently. Therefore, the robustness of conclusion that daily weighing causes a decrease in body dissatisfaction is unsubstantiated.
The deterioration in mood observed by Ogden and Whyman (1997) was not replicated in succeeding studies. Wing and colleagues (2007) measured frequency of self-weighing, depression (measured by the Beck Depression Inventory), binge eating episodes (Eating Disorder Questionnaire), and disinhibition (Eating Inventory) in a group of participants involved in an 18-month prevention of weight regain study. They observed self-weighing to be associated with an increase in dietary restraint and a decrease in disinhibition and depressive symptoms. Of note, an increase in dietary restraint also has been associated with successful weight loss maintainers observed from the NWCR (Klem, Wing, McGuire, Seagle, & Hill, 1998).
A similar lack of deterioration in mood was reported by Gokee-Larose et al. (2009) in a weight loss study of young adults. They analyzed changes in body image (Body Shape Questionnaire), binge eating behavior, depressive symptoms (Beck Depression Inventory), and subscales of an eating disorder questionnaire (Eating Disorder Examination-Self-Report Questionnaire) in a group of young adults who were asked to weigh themselves daily during a 10-week period of weight maintenance following weight loss. All of these psychological measures improved with treatment and rate of improvement was not different in a group of controls who did not weigh themselves. The authors concluded, “Daily weighing was not associated with any adverse changes in psychological symptoms” (Gokee-Larose et al., 2009).
Quick, Larson, Eisenberg, Hannan, and Neumark-Sztainer (2012) analyzed the results of a survey sent to 2,287 young adults intended to measure their health behaviors. They observed that 18% of women and 12% of men weighed themselves at least “a few times a week.” They observed significant correlations between self-weighting and unhealthy weight-control practices. Some of the behaviors classified as unhealthy weight control practices, using food substitutes, or skipping meals may not necessarily be considered “unhealthy” if the participants were trying to lose weight and this was medically justifiable. Using food substitutes (meal replacements) is a weight control strategy with strong supporting evidence and was endorsed in position papers of the (former) American Dietetic Association (Fitch & Keim, 2012; Jonnalagadda, Jones, & Black, 2005; Seagle, Strain, Makris, & Reeves, 2009). In addition to finding relationships between weighing and unhealthy weight-control practices, Quick et al. (2012) reported positive relationships between weighing and health weight-control practices as well. They concluded that “young adults who monitored their weight a few times per week or more reported significantly more depressive symptoms (in women) and poorer body satisfaction (in men) compared with young adults who monitored their weight less often” (p. 472). While these results appear to contradict previously discussed studies (Gokee-Larose et al., 2009; Wing et al., 2007) and support the original warning by Ogden and Whyman (1997), the results of the Quick et al. (2012) study were correlational. It is equally plausible that depressed females or males with poor body satisfaction chose to weigh themselves more frequently than nondepressed, body-satisfied females or males as it is that frequent self-weighing causes depression or poor body satisfaction.
One mediating factor between self-weighing frequency and the behaviors addressed by Quick et al. (2012) may be feelings about one’s shape and weight. Klos, Esser, and Kessler (2012) surveyed undergraduate students to investigate the relationship between frequency of self-weighing and several different dimensions of body image using the Multidimensional Body-Self Relations Questionnaire (MBSRQ) and the Eating Disorder Examination-Questionnaire (EDE-Q). After controlling for body mass index, self-weighing frequency was positively associated with the following dimensions of the MBSRQ in men: Health Orientation (adjusted r2 = .37; p < .01), Health Evaluation (adjusted r2 = .26; p < .05), Fitness Orientation (adjusted r2 = .23; p < .05), and Body Areas Satisfaction (adjusted r2 = .24; p < .05). There were no significant associations between dimensions of the EDE-Q and self-weighing frequency. However, in women, a significant correlation was found between self-weighing frequency and Appearance Orientation (adjusted r2 = .16; p < .05), Fitness Evaluation (adjusted r2 = .18; p < .05), Overweight Preoccupation (adjusted r2 = .31; p < .001), and Shape Concern (adjusted r2 = .20; p < .01). As with the Quick et al. (2012) study, it is not possible to determine whether these perceptions about one’s body lead to frequent weighing or vice versa. Though they provide useful information, these studies do not provide evidence to support or refute the safety of self-weighing in healthy young adult populations.
Finally, studies that deceive people of knowing their true weight have been used as an argument that frequent self-weighing may be harmful. Ogden and Evans (1996) randomly allocated participants into fictional height and weight categories: overweight, normal weight, or underweight. They found higher measures of depression among those who had been told that they were in the overweight category than those assigned to normal or underweight categories. Anxiety was not affected. McFarlane, Polivy, and Herman (1998) replicated this finding by demonstrating that weighing people on a scale that indicated they weighed 5 lb heavier than they actually weighed, increased measures of depression in restrained, but not unrestrained individuals. More recently, Winstanley and Dives (2005) also showed that by deceiving people by having them weigh themselves on a bogus scale that displayed their weight to be 7 lb above their true weight increased measures of anxiety and depression in all participants compared with those that weighed themselves using an accurate scale. Despite the consistency of the results, the argument against self-weighing based on adverse effects of being deceived by “rigged” scales may be relevant, but less so with higher frequency of weighing. False weight information may be perceived as depressing to anyone interested in maintaining a healthy weight or preventing weight gain. However, an individual weighing near daily will learn to differentiate the “noise” of day-today weight fluctuations from the underlying trend.
In summary, although there are hints from the literature that frequent self-weighing may be harmful to certain individuals, a behavioral or psychological parameter that consistently reflects harm caused by frequent self-weighing has not been reported as of yet. The evidence is stronger in adolescents showing that frequent weighing may be associated with harmful behaviors.
Potential Mechanisms Through Which Frequent Self-Weighing May Defend Against Weight Gain or Regain
Daily self-weighing may enhance weight control through at least three mechanisms. First, viewing a graph of body weight over time provides feedback indicating individuals’ current status of energy balance. Although there is considerable daily variation in measured weight due to changes in body water, body glycogen content, and the contents of the gastrointestinal tract, graphing repeated measures of weight reveals a pattern of change indicating a change in body tissue. This information can then be used to estimate the amount of food that should be consumed or the amount of physical energy that should be exerted during the day to maintain body weight at a certain level. From studies of Internet weight control programs, it has been found that providing frequent feedback to participants is one of most powerful predictors of the efficacy of the program (Haapala, Barengo, Biggs, Surakka, & Manninen, 2009; Krukowski, Harvey-Berino, Bursac, Ashikaga, & West, 2013; Turk et al., 2012).
The second mechanism through which frequent weighing may affect energy intake and expenditure behaviors is that the scale may act as a source of negative or positive reinforcement. Noting an increase in morning body weight may negatively reinforce behaviors that may have led to the increase in weight, such as consistently having lunch in a restaurant or eating dessert after dinner. Alternatively, observing a loss in morning body weight may positively reinforce the consumption of a small meal replacement, or skipping dessert, behaviors that might have occurred during the previous day.
Finally, stepping on the scale may act as a priming stimuli that sensitizes the individual to stimuli in the environment that may cause eating. For example, there is evidence that individuals will eat less when in the presence of a bathroom scale (Brunner, 2010). The memory of the scale along with the informational display on the graph may affect the individuals’ vulnerability to environmental cues associated with eating. More research on the use of frequent weighing is necessary not only to determine its effectiveness in preventing weight gain or regain but also to determine the processes through which it affects behavior to maximize its effect.
Conclusion
This review extends the conclusions reached in an earlier review by Vanwormer et al. (2008) that daily self-weighing appears to be a useful tool for successful weight management. This review suggests that daily self-weighing does not lead to enhanced weight loss when added to traditional weight loss programs. Rather, published data appear to strongly suggest that people who weigh themselves frequently lose more weight and can maintain their reduced weight longer than people who do not weigh themselves frequently. Such data may mean that the frequency of weighing may be an indicator of the motivation to lose and/or sustain a weight loss. However, several experimental studies have demonstrated that the use of daily self-weighing may be an effective technique to prevent individuals from regaining weight following weight loss treatment and also to prevent of age-related weight gain. Although we must be vigilant of possible negative side effects of frequent self-weighing on restrained eaters and people who might be vulnerable to eating disorders, the data, so far, does not present a cogent argument for daily self-weighing as a serious risk. Like other medical treatments, some groups with other conditions or comorbidities will benefit more from other types of interventions. This critical review of the literature suggests that daily self-weighing, with or without personalized messaging, may be an effective tool to help individuals counter the subtle effects of the many food-related stimuli in our obesogenic environment that seduce us to eat a little bit more, causing us to gain a little more weight. More research is needed to better understand the role of different types of feedback, who benefits from self-weighing, and at what frequency. Some subgroups of the population may benefit from different frequencies and others may not benefit.
Acknowledgments
Funding
The author(s) received no financial support for the research and/or authorship of this article.
Biographies
Carly R. Pacanowski is a National Institute of Health (NIH) postdoctoral fellow at the University of Minnesota. She studies self-weighing, yoga, obesity, and eating disorders.
Fredrik C. Bertz is a registered dietitian from Sweden. He has a PhD in clinical nutrition.
David A. Levitsky is professor of nutrition and psychology, Cornell University. His major area of research is the identification of the determinants of food intake and body weight.
Footnotes
The words “daily self-weighing” and “frequent self-weighing” are used interchangeably in this article. Currently, there is no standard definition of frequent self-weighing. Moreover, although most experimental studies begin by asking subjects to weigh themselves daily, most participants do not.
Two unpublished doctoral theses also examined self-weighing using a similar method to Levitsky, Garay, Nausbaum, Neighbors, and Dellavalle (2006) but failed to find self-weighing significantly prevented weight gain among freshman (Butryn, Phelan, Hill, & Wing, 2007; Katterman, 2010). However, as in the Gow, Trace, and Mazzeo (2010) study, both studies failed to find a significant weight gain in the control group.
Authors’ Note
This review was compiled as part of the first author’s doctoral dissertation.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson DA, Shapiro JR, Lundgren JD. The freshman year of college as a critical period for weight gain: An initial evaluation. Eating Behaviors. 2003;4:363–367. doi: 10.1016/S1471-0153(03)00030-8. [DOI] [PubMed] [Google Scholar]
- Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: A meta-analysis of US studies. American Journal of Clinical Nutrition. 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- Bertz F, Brekke HK, Lars E, Rasmussen KM, Wennergren M, Winkvist A. Diet and exercise weight-loss trial in lactating overweight and obese Women. American Journal of Clinical Nutrition. 2012;96:698–705. doi: 10.3945/ajcn.112.040196. [DOI] [PubMed] [Google Scholar]
- Brownell KD. The LEARN program for weight management. 10. Dallas, TX: American Health Publishing; 2004. [Google Scholar]
- Brunner TA. How weight-related cues affect food intake in a modeling situation. Appetite. 2010;55:507–511. doi: 10.1016/j.appet.2010.08.018. [DOI] [PubMed] [Google Scholar]
- Butler SM, Black DR, Blue CL, Gretebeck RJ. Change in diet, physical activity, and body weight in female college freshman. American Journal of Health Behavior. 2004;28:24–32. doi: 10.5993/ajhb.28.1.3. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: A key component of successful weight loss maintenance. Obesity. 2007;15:3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- Centers of Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- Cooley E, Toray T. Disordered eating in college freshman women: A prospective study. Journal of American College Health. 2001;49:229–235. doi: 10.1080/07448480109596308. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. A new cognitive behavioral approach to the treatment of obesity. Behaviour Research and Therapy. 2001;39:499–511. doi: 10.1016/s0005-7967(00)00065-6. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. Cognitive-behavioral treatment of obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. New York, NY: Guilford Press; 2002. pp. 465–479. [Google Scholar]
- Delinsky SS, Wilson GT. Weight gain, dietary restraint, and disordered eating in the freshman year of college. Eating Behaviors. 2008;9:82–90. doi: 10.1016/j.eatbeh.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Dionne MM, Yeudall F. Monitoring of weight in weight loss programs: A double-edged sword? Journal of Nutrition Education and Behavior. 2005;37:315–318. doi: 10.1016/s1499-4046(06)60162-0. [DOI] [PubMed] [Google Scholar]
- Economos CD, Hildebrandt ML, Hyatt RR. College freshman stress and weight change: Differences by gender. American Journal of Health Behavior. 2008;32:16–25. doi: 10.5555/ajhb.2008.32.1.16. [DOI] [PubMed] [Google Scholar]
- Edmonds MJ, Ferreira KJ, Nikiforuk EA, Finnie AK, Leavey SH, Duncan AM, Simpson JA. Body weight and percent body fat increase during the transition from high school to university in females. Journal of the American Dietetic Association. 2008;108:1033–1037. doi: 10.1016/j.jada.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Fisher EB, Green L, Friedling C, Levenkron J, Porter FL. Self-monitoring of progress in weight-reduction: A preliminary report. Journal of Behavior Therapy and Experimental Psychiatry. 1976;7:363–365. [Google Scholar]
- Fitch C, Keim KS. Position of the academy of nutrition and dietetics: Use of nutritive and nonnutritive sweeteners. Journal of the Academy of Nutrition and Dietetics. 2012;112:739–758. doi: 10.1016/j.jand.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Sakata T, Etou H, Fukagawa K, Ookuma K, Terada K, Kurata K. Charting of daily weight pattern reinforces maintenance of weight-reduction in moderately obese patients. American Journal of the Medical Sciences. 1992;303:145–150. doi: 10.1097/00000441-199203000-00002. [DOI] [PubMed] [Google Scholar]
- Gokee-Larose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: A randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2009;6:10. doi: 10.1186/1479-5868-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gow RW, Trace SE, Mazzeo SE. Preventing weight gain in first year college students: An online intervention to prevent the “freshman fifteen. Eating Behaviors. 2010;11:33–39. doi: 10.1016/j.eatbeh.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: Audit of primary sources. British Medical Journal. 2005;331:Article 1064. doi: 10.1136/bmj.38636.593461.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: A 1-year effectiveness study. Public Health Nutrition. 2009;12:2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- Hajhosseini L, Holmes T, Mohamadi P, Goudarzi V, McProud L, Hollenbeck CB. Changes in body weight, body composition and resting metabolic rate (RMR) in freshmen students first-year university. Journal of the American College of Nutrition. 2006;25:123–127. doi: 10.1080/07315724.2006.10719522. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Pintauro SJ, Gold EC. The feasibility of using Internet support for the maintenance of weight loss. Behavior Modification. 2002;26:103–116. doi: 10.1177/0145445502026001006. [DOI] [PubMed] [Google Scholar]
- Heckerman CL, Brownell KD, Westlake RJ. Self and external monitoring of weight. Psychological Reports. 1978;43:375–378. doi: 10.2466/pr0.1978.43.2.375. [DOI] [PubMed] [Google Scholar]
- Herman CP, Polivy J. Restrained eating. In: Stunkard AJ, editor. Obesity. Philadelphia, PA: Saunders; 1980. pp. 208–225. [Google Scholar]
- Hivert MF, Langlois MF, Berard P, Cuerrier JP, Carpentier AC. Prevention of weight gain in young adults through a seminar-based intervention program. International Journal of Obesity. 2007;31:1262–1269. doi: 10.1038/sj.ijo.0803572. [DOI] [PubMed] [Google Scholar]
- Hoffman DJ, Policastro P, Quick V, Lee SK. Changes in body weight and fat mass of men and women in the first year of college: A study of the “freshman 15. Journal of American College Health. 2006;55:41–45. doi: 10.3200/JACH.55.1.41-46. [DOI] [PubMed] [Google Scholar]
- Holm-Denoma JM, Joiner TE, Vohs KD, Heatherton TF. The “freshman fifteen” (the “freshman five” actually): Predictors and possible explanations. Health Psychology. 2008;27:S3–S9. doi: 10.1037/0278-6133.27.1.S3. [DOI] [PubMed] [Google Scholar]
- Hovell MF, Mewborn CR, Randle Y, Fowler-Johnson S. Risk of excess weight gain in university women: A three-year community controlled analysis. Addictive Behaviors. 1985;10:15–28. doi: 10.1016/0306-4603(85)90049-8. [DOI] [PubMed] [Google Scholar]
- Hull HR, Morrow ML, Dinger MK, Han JL, Fields DA. Characterization of body weight and composition changes during the sophomore year of college. BMC Women’s Health. 2007;7:Article 21. doi: 10.1186/1472-6874-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull HR, Morrow ML, Heesch KC, Dinger MK, Han JL, Fields DA. Effect of the summer months on body weight and composition in college women. Journal of Women’s Health. 2007;16:1510–1515. doi: 10.1089/jwh.2006.0329. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Preventative Medicine. 1984;13:155–168. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, French SA. Preventing weight gain in adults: Design, methods and one year results from the Pound of Prevention study. International Journal of Obesity and Related Metabolic Disorders. 1997;21:457–464. doi: 10.1038/sj.ijo.0800431. [DOI] [PubMed] [Google Scholar]
- Joachim R. The use of self-monitoring to effect weight loss in a mildly retarded female. Journal of Behavior Therapy and Experimental Psychiatry. 1977;8:213–215. [Google Scholar]
- Jonnalagadda SS, Jones JM, Black JD. Position of the American Dietetic Association: Fat replacers. Journal of the American Dietetic Association. 2005;105:266–275. doi: 10.1016/j.jada.2004.12.011. [DOI] [PubMed] [Google Scholar]
- Jung ME, Bray SR, Martin Ginis KA. Behavior change and the freshman 15: Tracking physical activity and dietary patterns in 1st-year university women. Journal of American Collage Health. 2008;56:523–530. doi: 10.3200/JACH.56.5.523-530. [DOI] [PubMed] [Google Scholar]
- Kasparek DG, Corwin SJ, Valois RF, Sargent RG, Morris RL. Selected health behaviors that influence college freshman weight change. Journal of American College Health. 2008;56:437–444. doi: 10.3200/JACH.56.44.437-444. [DOI] [PubMed] [Google Scholar]
- Katterman S. An evaluation of daily weight monitoring as a method of weight gain prevention. Doctoral dissertation. 2010 doi: 10.1177/1359105315589446. Retrieved from https://idea.library.drexel.edu/islandora/object/idea%3A3337. [DOI] [PubMed]
- Kayman S, Bruvold W, Stern JS. Maintenance and relapse after weight loss in women: Behavioral aspects. American Journal of Clinical Nutrition. 1990;52:800–807. doi: 10.1093/ajcn/52.5.800. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. American Journal of Clinical Nutrition. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. Psychological symptoms in individuals successful at long-term maintenance of weight loss. Health Psychology. 1998;17:336–345. doi: 10.1037//0278-6133.17.4.336. [DOI] [PubMed] [Google Scholar]
- Klos LA, Esser VE, Kessler MM. To weigh or not to weigh: The relationship between self-weighing behavior and body image among adults. Body Image. 2012;9:551–554. doi: 10.1016/j.bodyim.2012.07.004. [DOI] [PubMed] [Google Scholar]
- Krukowski RA, Harvey-Berino J, Bursac Z, Ashikaga T, West DS. Patterns of success: Online self-monitoring in a web-based behavioral weight control program. Health Psychology. 2013;32:164–170. doi: 10.1037/a0028135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitsky DA, Garay J, Nausbaum M, Neighbors L, Dellavalle D. Monitoring weight daily blocks the freshman weight gain: A model for combating the epidemic of obesity. International Journal of Obesity. 2006;30:1003–1010. doi: 10.1038/sj.ijo.0803221. [DOI] [PubMed] [Google Scholar]
- Levitsky DA, Halbmaier CA, Mrdjenovic G. The freshman weight gain: A model for the study of the epidemic of obesity. International Journal of Obesity Related Metabolic Disorders. 2004;28:1435–1442. doi: 10.1038/sj.ijo.0802776. [DOI] [PubMed] [Google Scholar]
- Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Annals of Behavioral Medicine. 2005;30:210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson EE, Bailey S, Fava JL, Wing R. A prospective study of weight gain during the college freshman and sophomore years. Preventive Medicine. 2009;48:256–261. doi: 10.1016/j.ypmed.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loro A, Fisher EB, Levenkron JC. Comparison of established and innovative weight-reduction treatment procedures. Journal of Applied Behavior Analysis. 1979;12:141–155. doi: 10.1901/jaba.1979.12-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe MR, Annunziato RA, Markowitz JT, Didie E, Bellace DL, Riddell L, … Stice E. Multiple types of dieting prospectively predict weight gain during the freshman year of college. Appetite. 2006;47:83–90. doi: 10.1016/j.appet.2006.03.160. [DOI] [PubMed] [Google Scholar]
- Mahoney MJ. Self-reward and self-monitoring techniques for weight control. Behavior Therapy. 1974;5:48–57. [Google Scholar]
- Mahoney MJ, Moura NG, Wade TC. Relative efficacy of self-reward, self-punishment, and self-monitoring techniques for weight loss. Journal of Consulting and Clinical Psychology. 1973;40:404–407. doi: 10.1037/h0034565. [DOI] [PubMed] [Google Scholar]
- McFarlane T, Polivy J, Herman CP. Effects of false weight feedback on mood, self-evaluation, and food intake in restrained and unrestrained eaters. Journal of Abnormal Psychology. 1998;107:312–318. doi: 10.1037//0021-843x.107.2.312. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Hill JO. The prevalence of weight loss maintenance among American adults. International Journal of Obesity and Related Metabolic Disorders. 1999;23:1314–1319. doi: 10.1038/sj.ijo.0801075. [DOI] [PubMed] [Google Scholar]
- Mercurio A, Rima B. Watching my weight: Self-weighing, body surveillance, and body dissatisfaction. Sex Roles. 2011;65:47–55. [Google Scholar]
- Ogden J, Evans C. The problem with weighing: Effects on mood, self-esteem and body image. International Journal of Obesity and Related Metabolic Disorders. 1996;20:272–277. [PubMed] [Google Scholar]
- Ogden J, Whyman C. The effect of repeated weighing on psychological state. European Eating Disorder Review. 1997;5:121–130. [Google Scholar]
- Oshima Y, Matsuoka Y, Sakane N. Effect of weight-loss program using self-weighing twice a day and feedback in overweight and obese subject: A randomized controlled trial. Obesity Research & Clinical Practice. 2013;7:e361–e366. doi: 10.1016/j.orcp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Quayle CM, Powers RB. The self-recording of weights and bites in the treatment of obesity. The Psychological Record. 1979;29:517–522. [Google Scholar]
- Quick V, Larson N, Eisenberg ME, Hannan PJ, Neumark-Sztainer D. Self-weighing behaviors in young adults: Tipping the scale toward unhealthy eating behaviors? Journal of Adolescent Health. 2012;51:468–474. doi: 10.1016/j.jadohealth.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanczyk RG. Self-monitoring in the treatment of obesity: Parameters of reactivity. Behavior Therapy. 1974;5:531–540. [Google Scholar]
- Romanczyk RG, Tracey DA, Wilson GT, Thorpe GL. Behavioral techniques in the treatment of obesity: A comparative analysis. Behaviour Research and Therapy. 1973;11:629–640. doi: 10.1016/0005-7967(73)90120-4. [DOI] [PubMed] [Google Scholar]
- Seagle HM, Strain GW, Makris A, Reeves RS. Position of the American Dietetic Association: Weight management. Journal of the American Dietetic Association. 2009;109:330–346. doi: 10.1016/j.jada.2008.11.041. [DOI] [PubMed] [Google Scholar]
- Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodgea C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and email. Obesity. 2013;21:1789–1797. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strimas R, Dionne MM. Differential effects of self-weighing in restrained and unrestrained eaters. Personality and Individual Differences. 2010;49:1011–1014. [Google Scholar]
- Stuart R. Behavioral control of overeating. Behavior Research and Therapy. 1967;5:357–365. doi: 10.1002/j.1550-8528.1996.tb00249.x. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. Journal of the American Medical Association. 2003;289:1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Archives of Internal Medicine. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. Journal of the American Medical Association. 2001;285:1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- Turk MW, Elci OU, Wang J, Sereika SM, Ewing LJ, Acharya SD, … Burke LE. Self-monitoring as a mediator of weight loss in the SMART randomized clinical trial. International Journal of Behavioral Medicine. 2012;20:556–561. doi: 10.1007/s12529-012-9259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanwormer JJ, French SA, Pereira MA, Welsh EM. The impact of regular self-weighing on weight management: A systematic literature review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5:Article 54. doi: 10.1186/1479-5868-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanWormer JJ, Linde JA, Harnack LJ, Stovitz SD, Jeffery RW. Self-weighing frequency is associated with weight gain prevention over 2 years among working adults. International Journal of Behavioral Medicine. 2012;19:351–358. doi: 10.1007/s12529-011-9178-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanWormer JJ, Martinez AM, Benson GA, Crain A, Martinson BC, Cosentino DL, Pronk NP. Telephone counseling and home telemonitoring: The weigh by day trial. American Journal of Health Behavior. 2009;33:445–454. doi: 10.5993/ajhb.33.4.10. [DOI] [PubMed] [Google Scholar]
- VanWormer JJ, Martinez AM, Martinson BC, Crain AL, Benson GA, Cosentino DL, Pronk NP. Self-weighing promotes weight loss for obese adults. American Journal of Preventive Medicine. 2009;36:70–73. doi: 10.1016/j.amepre.2008.09.022. [DOI] [PubMed] [Google Scholar]
- Welsh EM, Sherwood NE, VanWormer JJ, Hotop AM, Jeffery RW. Is frequent self-weighing associated with poorer body satisfaction? Findings from a phone-based weight loss trial. Journal of Nutrition Education and Behavior. 2009;41:425–428. doi: 10.1016/j.jneb.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. The New England Journal of Medicine. 2006;355:1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: Are there negative effects of daily weighing? Journal of Consulting and Clinical Psychology. 2007;75:652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- Winstanley S, Dives L. Effects on mood of a bogus weight gain. European Eating Disorders Review. 2005;13:424–426. [Google Scholar]