Abstract
Introduction: The aim of this study was to evaluate the primary and secondary therapeutic successes of different therapy schemes for the treatment of synechia of the labia in pre-pubertal girls. Materials and Methods: The treatment courses of 47 pre-pubertal girls who were treated between February 2007 and February 2013 in the special outpatient clinic for paediatric gynaecology of a department for gynaecology at a German university hospital and for whom information on the course of the disease was available for at least the six months following end of the treatment. 23 of these children were treated with a topical estriol therapy (treatment group A). For 24 of the girls a manual separation of the adhering labia minora was undertaken (treatment group B). Statistical evaluation was performed using the χ2 test, Fischerʼs exact test and the Mann-Whitney U test. Results: For 18 of the 23 (80 %) girls in treatment group A topical estriol therapy alone led to a resolution of the synechia. Five of these 23 children (20 %) required a secondary manual separation. All girls for whom treatment was not successful were under 5 years of age. For all 24 girls (100 %) of treatment group B the primary manual separation was performed with success. The recurrence rates after ≥ 6 months in cases with identical after-care did not differ between the two treatment groups (treatment group A: 34 %, treatment group B: 33 %, χ2 test: p = 0.853). 16 of the 17 recurrences occurred ≥ 3 months after the end of the therapy. Conclusion: Our results show that for children < 5 years of age a 4-week topical therapy with estriol is a promising therapy option for synechia of the labia that is less of a burden for the family situation. Especially for girls ≥ 5 years of age, primary therapy fails in up to 20 % of the cases. Primary manual separation represents a more effective therapeutic option. Irrespective of the treatment applied, a recurrence after ≥ 3 must be expected in one-third of the treated girls.
Key words: labial adhesions, paediatric gynaecology, vulvovaginitis
Abstract
Zusammenfassung
Fragestellung: Ziel dieser Untersuchung war es, den primären und sekundären Therapieerfolg unterschiedlicher Therapieschemata zur Behandlung einer Labiensynechie präpubertaler Mädchen zu evaluieren. Material und Methodik: Retrospektiv wurden die Behandlungsverläufe von 47 präpubertalen Mädchen analysiert, die zwischen Februar 2007 und Februar 2013 wegen einer Labiensynechie in der kindergynäkologischen Spezialsprechstunde einer Universitätsfrauenklinik behandelt wurden und bei denen Informationen über den weiteren Krankheitsverlauf über einen Zeitraum von mindestens 6 Monaten nach Therapieende verfügbar waren. 23 dieser Kinder wurden mit einer topischen Estrioltherapie behandelt (Behandlungsgruppe A). Bei 24 Kindern wurde eine manuelle Separation der adhärenten Labia minora durchgeführt (Behandlungsgruppe B). Die statistische Auswertung erfolgte mithilfe des χ2-Tests, des exakten Tests nach Fisher und des U-Tests nach Mann-Whitney. Ergebnisse: Bei 18 der 23 (80 %) der Mädchen der Behandlungsgruppe A führte die alleinige topische Estrioltherapie zu einer Lösung der Synechie. Fünf dieser 23 Kinder (20 %) mussten sekundär mit einer manuellen Separation behandelt werden. Alle Mädchen mit ausbleibendem Therapieerfolg waren ≥ 5 Jahre. Bei allen 24 Mädchen (100 %) der Behandlungsgruppe B konnte die primäre manuelle Separation erfolgreich durchgeführt werden. Die Rezidivrate nach ≥ 6 Monaten unterschied sich zwischen den beiden Behandlungsgruppen bei identischer Nachbehandlung nicht (Behandlungsgruppe A: 34 %, Behandlungsgruppe B: 33 %, χ2-test: p = 0,853). 16 der 17 Rezidive traten ≥ 3 Monate nach Therapieende auf. Schlussfolgerung: Unsere Ergebnisse zeigen, dass bei Kindern < 5 Jahren eine 4-wöchige topische Therapie mit Estriol eine erfolgversprechende, die familiäre Situation wenig belastende Therapieoption zur Behandlung der Labiensynechie darstellt. Besonders bei älteren Mädchen ≥ 5 Jahren kommt es in bis zu 20 % zu einem primären Therapieversagen. Die primäre manuelle Separation stellt eine wirkungsvollere Therapieoption dar. Unabhängig von der durchgeführten Behandlung muss mit einem Rezidiv nach ≥ 3 Monaten in einem Drittel der behandelten Mädchen gerechnet werden.
Schlüsselwörter: Labienadhäsionen, Kindergynäkologie, Vulvovaginitis
Introduction
The term synechia of the labia is used to describe a superficial adhesion or fusion of the labia minora at their medial edges. Apart from the term synechia of the labia, labial synechia, labial adhesions, and vulval synechia are also found in the literature, which besides adhesions of the labia minora often include adhesion of the vulva margins (labial adhesion, labial agglutination, labial fusion and synechia vulvae) 1. Especially afflicted are girls in the hormonal dormancy period with a particular concentration in ages between 2 and 4 years 1. The incidence rate is reported to be 1.8–3.5 % 2. The study by McCann et al., in which an incidence of 38.9 % was found in pre-pubertal, asymptomatic girls, represents an exception 3. For the aetiology, a primarily occurring superficial skin irritation in the physiological hormonal dormancy period 4, which may also occur in combination with a superficial vulvovaginitis, is assumed. Depending on the age, these inflammations can have different causes such as a bacterial infection, a threadworm infection or a topical dermatitis. The most frequent causes are an inadequate or often a too intensive intimate hygiene through an irritation of the skin by excessive topical application of soaps, foam baths, hip baths or other irritating substances as well as tight-fitting clothes. An unfavourable defaecation or micturition position may also represent a triggering cause. Lichen sclerosis must also be considered in the differential diagnosis. In the afflicted girls the superficial skin irritation on the non-oestrogenised mucous membrane leads to a re-epithelisation which, in combination with the also irritated labia on the other side, results in a non-vascularised adhesion. On histology, this consists of keratinised layers of squamous epithelium. The diagnosis is made on the basis of a clinical examination. Typically an extremely thin, translucent membrane that closes the introitus is observed (Fig. 1). The symptoms depend decisively on the extent of the adhesion. This can occur on a segment of the labia minora (ventral, dorsal, central) or over the complete length of the labia minora (complete synechia of the labia). The more pronounced the adhesion is the earlier does the afflicted child experience complaints. As a result of a complete synechia of the labia urinary incontinence (dribbling) may occur in pot-trained children and this further supports the local inflammatory reaction. Differing data have been published on the association with urinary tract infections (5–14 %) and unspecific bacteriuria (2–20 %) 5. Isolated cases of obstruction of the upper urinary tract have been described 6. The most frequent local finding is vulvitis or vulvovaginitis. The children themselves only rarely report complaints such as vaginal burning or itching or pain in connection with micturition. In the case of less extensive adhesions, the finding is often made in the course of routine medical check-ups in the absence of complaints. The parents are often seen to be anxious or frightened by the clinical picture and should be actively involved in the treatment process.
Fig. 1.

Clinical picture of typical pre-pubertal synechia of the labia in a 5-year-old girl.
Treatment recommendations for labial synechia vary widely depending on the literature source. Some groups recommend the sole application of 0.1 % estriol ointment without any manual measures 1. A hormone deficiency has not yet been detected in any clinical trials 7. Other authors prefer the topical oestrogen pre-treatment with subsequent manual separation 8, 9 or primary operative separation 10 when the oestrogen therapy fails. As alternatives there are treatment schemes with topical corticosteroids (betamethasone 0.05 %) 11, 12 or 0.1 % gentamycin ointment 13. Other groups favour the immediate manual separation of the labia in the sense of a rapid solution to the problem 14 or, respectively, surgical separation of the labia 15.
Possible side effects of the above-mentioned therapies need to be taken into consideration. Reddening or a burning sensation of the vulva and labial pigmentation have been mentioned as possible side effects of therapy 16. In rare cases, premature thelarche, adrenarche, uterine bleeding or psychological traumatisation have been described 17. At present no data are available to answer the question of whether any of the treatment methods could have an influence on the consecutive development of genital lichen sclerosis.
The aim of our study was to analyse the therapeutic effects as well as the recurrence rates in dependence on the applied therapy and the age of the treated child in a retrospective investigation.
Materials and Method
Patient collective
Between February 2007 and February 2013, 64 girls were referred to the special outpatient clinic for paediatric gynaecology of a department for gynaecology at a German university hospital for treatment of labial synechia. For 47 of the children information on the further clinical course over a period of at least 6 months after the end of the treatment from control examinations or findings of the paediatrician responsible for after-care.
None of the girls included in the study suffered from a recurrent labial synechia or a dermatological disease with urogenital manifestations. Fig. 2 shows the age distribution of the young patients at first presentation.
Fig. 2.
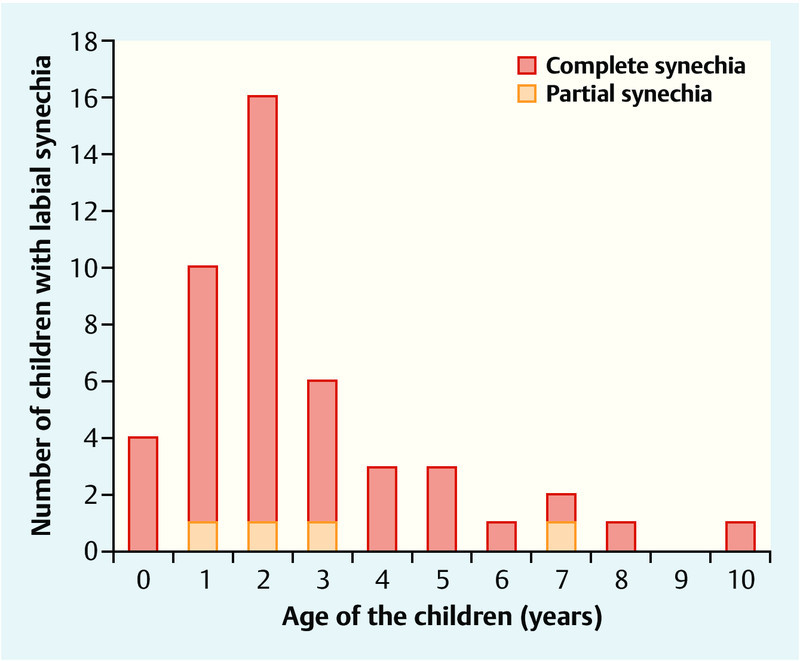
Age distribution of the pre-pubertal girls with labial synechia at first presentation (n = 47).
30 of the girls (64 %) were younger than 3 years, 12 (25 %) were between 3 and 5 years, and 5 (11 %) were between 6 and 10 years of age (range: 0–10 years, median: 1.9 years). The corresponding characteristics of the 17 girls without follow-up data were comparable (64 % [n = 11] < 3 years, 24 % [n = 4] 3 to 5 years, 2 [12 %] 6 to10 years; range: 0–10 years, median: 1.8 years).
The girls were referred to the clinic for the reasons listed in Table 1.
Table 1 Reason for referral of the pre-pubertal girls with labial synechia (n = 47).
| Indication for referral* | Numbern (%) |
|---|---|
| * multiple selections possible | |
| Incidental finding in the course of a medical check-up | 21 (45) |
| Recurrent reddening of the vulva | 14 (30) |
| Recurrent vulvovaginitis | 9 (20) |
| Urinary dribbling | 1 (2) |
| Suspicion of urinary tract infection | 2 (4) |
| Pain on micturition | 3 (6) |
| Delayed micturition | 1 (2) |
| Suspicion of vesicourethral reflux | 1 (2) |
For all children a standardised new case history was taken. The already undertaken external pre-treatments were determined. 96 % of all girls (45 of 47 children) had been treated with estriol ointments for varying lengths of time by the referring colleagues. 29 girls (64 %) had received a single pre-treatment cycle while the remaining 16 children (36 %) had undergone multiple pre-treatment cycles.
The finding was validated by means of a standardised paediatric gynaecological examination by a qualified female specialist and classified as complete (≥ 50 % of the introitus covered) or, respectively, partial labial synechia (< 50 %). For 43 of the 47 children (92 %) a complete labial synechia was diagnosed while the remaining 4 girls (8 %) each had a partial dorsal labial synechia. A specific vulvitis was excluded by means of microbiological smear diagnostics.
Therapy concepts A and B
The parents or guardians were comprehensively informed of the alternative therapeutic options:
Treatment option A: topical therapy with estriol
The children were prescribed an estriol ointment (estriol 1 mg/g) (Oekolp®, Dr. Kade Pharma gmbH, Berlin, Germany), that was to be applied every night over 4 weeks by the care-giving person according to detailed instructions (exact application on the fusion site, if necessary with the help of a cotton-tipped stick with mild pressure and traction).
Treatment option B: manual separation of the labia
For preparation of the children 60 min prior to the planned intervention, lidocaine gel 2 % (Xylocain® 2 %, Astra Zeneca GmbH, Wedel, Germany) was thinly applied to the genital region by the care-giver. 30 min later the children were give a weight-adjusted premedication with midazolam 0.25 mg/kg body weight (Midazolamsaft, 2 mg/mL, Ratiopharm, Ulm, Germany) and ibuprofen 10 mg/kg body weight (Dolorminsaft® for children 2 %, McNell, Neuss, Germany). For the manual labial separation the child is usually placed on the care-giverʼs lap in a backrest position. In analogy to the traction method in paediatric gynaecological examinations, the non-epithelised synechia is carefully placed under tension and opened from ventral to dorsal with a moistened cotton swab. This separation takes 1–2 seconds. For after-care the parents are instructed to apply a gentamycin ointment 0.1 % (Infectogenta® 0.1 %, Infectopharm GmbH, Heppenheim, Germany) twice daily for 10 days.
23 parents initially chose the continuation of the topical therapy (treatment group A). 24 parents or guardians decided in favour of the manual separation of the labia (treatment group B).
The procedure was explained in detail to all the parents and they were given an information leaflet on the optimal intimate hygiene for their daughters. Concomitantly use of an astringent skin care preparation on a paraffin oil basis several times daily was recommended (Deumavan®, Kaymogyn, Wiesbaden, Germany). The parents were instructed to inspect the childʼs genitals once per week in order to detect a possible recurrence as early as possible.
Paediatric gynaecological diagnostics
At the follow-up examination after 4 weeks the therapeutic success was evaluated by the same medical team. The children in treatment group A for whom the topical therapy was not successful were then treated secondarily by means of manual separation corresponding to that of treatment group B.
The parentsʼ satisfaction with the chosen treatment was evaluated by means of a questionnaire.
For evaluation of the recurrence rate the paediatric gynaecological diagnostics of the 47 girls included in the study were evaluated after a period of at least 6 months from the end of the therapy. The average follow-up time was 20 months in the median (range: 6–66 months).
Statistical evaluation
Non-normally distributed metric variables are given as the median and range. The comparison of not-normally distributed metric variables between the two groups was made with the Mann-Whitney U test. Depending on the minimally expected frequency, the χ2 test or, respectively, Fisherʼs exact test was used for the comparison of the categorical variables between the two groups. Statistical significance is assumed at p < 0.05. Data evaluation and analysis was done with the help of the statistical software package SPSS Statistics® (Version 17.0, SPSS Inc. Chicago, USA).
Results
Altogether, the data for 47 girls who were referred for the first time to the special outpatient clinic for paediatric gynaecology in the period from February 2007 to February 2013 for treatment of labial synechia were evaluated. 23 children received a primary topical therapy (treatment group A), of these 5 children with a lack of therapeutic success after 4 weeks were treated by a secondary manual separation (treatment group B after A). At the request of their parents 24 children underwent a primary manual separation (treatment group B) (Table 2).
Table 2 Treatment schemes for the pre-pubertal girls with labial synechia (n = 47).
| Number of girls | ||
|---|---|---|
| Treatment option A | estriol topical therapy | 23 |
| secondary manual separation | 5 | |
| Treatment option B | primary manual separation | 24 |
Fig. 3 shows the age distribution in regard to the performed treatment of all 47 girls. For the age group of 2-year-old and younger girls (n = 30) significantly more parents (22 of 30 parents, 73 %) decided in favour of manual separation rather than the topical therapy (8 of 30 parents, 27 %, χ2 test: p = 0.043). In contrast, the majority of parents of the 3- to 5-year-old patients (n = 12) chose the topical therapy option (11 of 12 parents, 82 %). Only one pair in this group of parents (8 %) decided in favour of the manual separation (Fisherʼs exact test: p = 0.032). The parents of the older children in the age group 6 to 10 years (n = 5) exhibited a similar behaviour. In this collective also only one pair of parents (20 %) chose the primary manual therapy. The other 4 parent pairs decided in favour of the topical treatment option (4 of 5 parents, 80 %, Fisherʼs exact test: p = 0.042). For all 24 children who were primarily treated by manual separation, the intervention could be carried out successfully within 1–2 seconds without general anaesthesia and without complications.
Fig. 3.
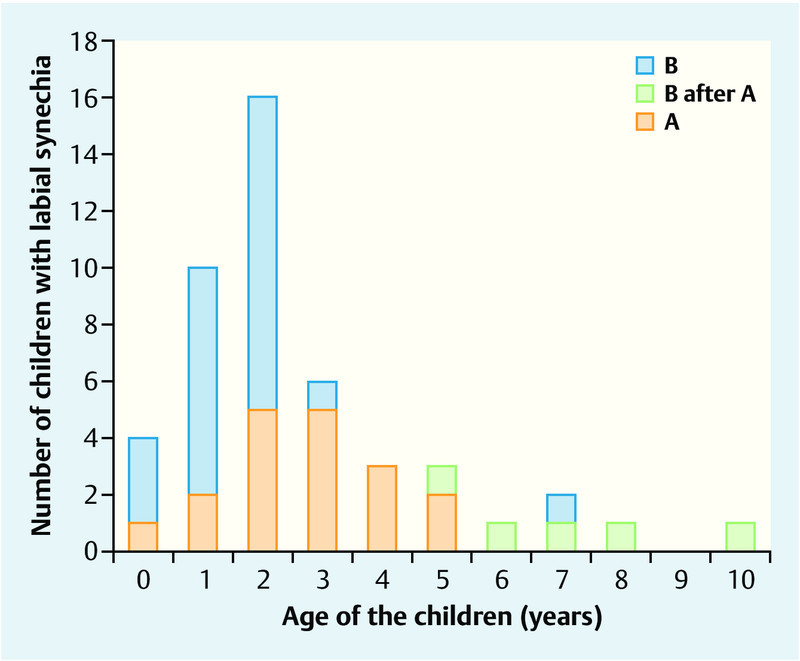
Age distribution with regard to treatment group of the pre-pubertal girls with labial synechia (n = 47).
Paediatric gynaecological findings after 4 weeks
At the first follow-up examination after 4 weeks a treatment success in the sense of a complete resolution of the synechia was seen in 18 of the 23 girls (80 %) in treatment group A. All 24 of the children primarily treated with manual separation were free of recurrences. Thus a significantly better result could be achieved through manual separation (χ2 test: p = 0.041; Fig. 4, Table 3).
Fig. 4.
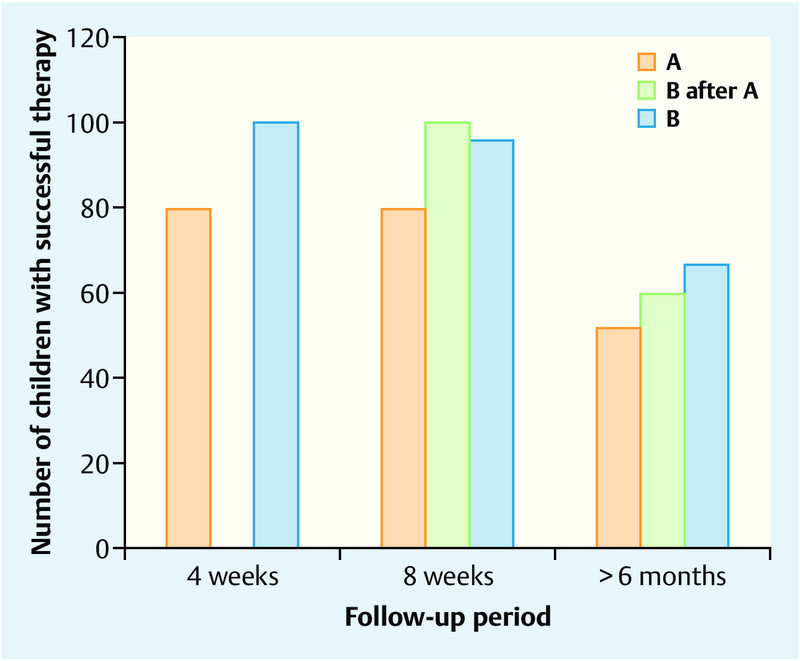
Therapeutic success in pre-pubertal girls with labial synechia (n = 47).
Table 3 Therapeutic success of the different treatment schemes for pre-pubertal girls with labial synechia (n = 47).
| Treatment scheme | Length of follow-up (months) | ||
|---|---|---|---|
| 1 | 2 | > 6 months | |
| A (topical therapy) | 18/2380 % | 18/2380 % | 12/1866 % |
| B after A (secondary manual separation after topical therapy) | 5/5100 % | 3/560 % | |
| B (primary manual separation) | 24/24100 % | 23/2496 % | 16/2467 % |
The 5 girls in treatment group A for whom topical therapy was unsuccessful were all ≥ 5 years old (Fig. 3). Three of these girls showed such extensive adhesions that the indication for manual separation under general anaesthesia had to be applied. Complete resolution of the synechia was achieved for each of these girls.
Paediatric gynaecological findings after 8 weeks
At the second follow-up examination after 8 weeks (Fig. 4, Table 3) one 2-year-old girl from the group that had been treated by means of primary manual separation showed an early recurrence. All other children in the different groups were free of recurrence at this time point.
Paediatric gynaecological findings after > 6 months
In the further course of a follow-up period of at least 6 months, 6 recurrences in treatment group A and further 7 recurrences in treatment group B were diagnosed. The average time until occurrence of a recurrence in treatment group A amounted to 5.1 months (range: 4–21 months) and in treatment group B to 6.7 months (range: 3–17 months). Thus there were no significant differences in the rates of recurrence (treatment group A: 34 % vs. treatment group B: 33 %, χ2 test: p = 0.853) or the period of time up to the recurrence between the two treatment groups (Mann-Whitney U test: p = 0.715).
The satisfaction of the parents with the applied treatment differed between the therapy concepts. Whereas all parents of children in treatment groups A as well as B after A (altogether 23 parents) were also retrospectively satisfied with their decision, 3 of the 24 parents (13 %) in the treatment group B reported that they would not decide for the chosen therapy concept again because they found the treatment regimen to be too stressful for the child and for the family (Fisherʼs exact test: p = 0.065).
Discussion
Since the recommendations in the relevant literature for the treatment of labial synechia in childhood are rather inhomogeneous, we have involved the parents in the decision-making process by explaining in detail the diagnosis and the conservative and invasive the treatment options (topical estriol therapy, primary or, respectively, secondary manual labia separation). The parentsʼ decision making was influenced by numerous factors. These factors concerned both the child and the parents. The dependence on the age of the child was statistically significant. Whereas almost ¾ of the parents whose children were 2 or less years old decided in favour of the primary manual separation which can be performed in a single therapeutic sitting, only ⅕ of the parent pairs of the 3- to 5-year-old children or, respectively, of the 6- to 10-year old girls made the same decision. It is possible that the parents of the small, nappy-wearing babies felt themselves to be overtaxed by the unsupervised performance of the local therapy or were afraid that they could accidently injure their children or cause them pain.
In the literature there is a pronounced controversy as to how to treat pre-pubertal labial synechia. Many authors recommend the application of estriol-containing external preparations 1, 2, 16. The success rates vary between 50 and 90 % 11, 12. Our observed healing rate of 80 % in treatment group A comprising the treatment of girls aged between 4 months and 10 years over a 4-week period with 1 % estriol ointment is in accord with these data. Since most (96 %) of the treated girls had already undergone pre-treatment with a comparable therapy cycle, it seems that at least two treatment cycles are reasonable. We found a relationship between the age of the girls and the result of the treatment in the sense that especially the synechia of children who were more than 5 years old at the time of treatment could often not be treated successfully with the topical hormone therapy. As recommended by the groups of Anthuber et al. (2004) and Buck et al. (2010) in their publications, we successfully treated these patients with a secondary manual separation 8, 9.
In analogy to the recommendations of the authors Thibaud et al. (2003) and Watanabe et al. (2010), we treated the girls in treatment group B by means of a primary manual separation 14, 15. Resolution of the synechia was achieved in all these children. Thus, the immediate therapeutic success rate was significantly better than that for the local therapy with estriol ointment.
However, there are also critical appraisals of the mechanical solution in the literature with regard to a potential traumatisation of the girl 11, 12. On the other hand, there are also reports in which the procedure is recommended as therapy of choice on account of the rapidly achieved therapeutic success and the high success rates 15, 16. Frequently the anxiety about a possibly painful experience for the child in the manual separation of the labia in spite of the offered analgesic premedication dominates among the parents. However when the indication for topical estriol therapy is present, it must also be considered and explained that the sole therapy with oestrogen ointment is protracted, requires a high compliance from both the childʼs and the parentsʼ sides and can possibly be accompanied by the side effects listed above.
Almost ¾ of the treated girls did not show any symptoms (45 %) resulting from the labial synechia or exhibited only a sporadically occurring reddening of the vulva (30 %). Since the synechia exhibit markedly more intense adhesions with increasing age, therapy should be initiated rapidly upon the first diagnosis in school age, even for asymptomatic children. Timely treatment can prevent progression of the adhesion with scar formation in the region of contact between the two labia and thus spare the afflicted girl from a possible surgical intervention under general anaesthesia. Also in the collective examined here all 3 girls who required a general anaesthesia for the manual separation were 5 or more years of age.
Both treatment groups showed a recurrence rate of ⅓ after at least 6 months (treatment group A: 34 % vs. treatment group B: 33 %). These data are in agreement with the published recurrence rates of up to 41 % irrespective of the treatment concept that was applied in the primary intervention 1, 2, 6. Our study does not confirm the data published by Myers et al. (2006) who demonstrated a higher risk of recurrence for children treated with a primary separation 11.
With one exception, the observed recurrent synechia occurred > 3 months after the end of the therapy. This time course must be taken into consideration, especially when informing the parents with regard to the period during which a consequently carried out, optimal genital hygiene is needed.
Our investigations have shown that the parents were more satisfied by an initial topical therapy that was followed in the case failure after 4 weeks by secondary manual separation than when the manual separation was performed as primary procedure, but the difference was not significant. On the basis of the collected data and our experience with the girls and their parents, the most important factor is a detailed consultation with the parents and, depending on her age, also the child at the first presentation. Explanations to the parents about the aetiology and the complications of this clinical entity as well as the possible therapeutic options and information about recommended age-adjusted hygiene measures is urgently needed in order to involve the parents in the treatment process and so minimise the risk of recurrence.
Practical Conclusions
On the basis of the collected data and under consideration of the published studies, the authors consider that it is advisable to treat a symptomatic labial synechia with two treatment cycles of topical estriol therapy for up to 4 weeks. The parents should be informed of the 80 % success rate for this therapy concept. About ⅕ of the children will require a secondary manual separation. Therapeutic failures will be seen especially among the girls aged ≥ 5 years. Therapy failures can be due to a lack of continuity of the treatment by the care-giver. As an alternative, the primary manual separation should be offered whereby the problem can be solved in a single treatment sitting. In the consultations, the lower acceptance of this treatment concept by the childʼs parents/guardian has to be taken into consideration. Irrespective of the nature of the primary therapy, one third of the children will experience a recurrence of the labial synechia after ≥ 3 months. On account of the low tendency for progression of existing labial adhesions on leaving the synechia alone and the high remission rate up to reaching the age of menarche, the therapeutic indication for girls with asymptomatic labial synechia, especially in children of nursery and pre-school age, as well as for the occurrence of a recurrence, should be made with caution.
Footnotes
Conflicts of Interest The authors declare that they have no financial connections with any companies of relevance for this article.
Supporting Information
References
- 1.Heinz M. Symptome und Erkrankungen des äußeren Genitale und der Brust bei Mädchen. Gynäkologe. 2011;44:452–462. [Google Scholar]
- 2.Van Eyk N, Allen L, Giesbrecht E. et al. Pediatric vulvovaginal disorders: a diagnostic approach and review of the literature. J Obstet Gynaecol Can. 2009;31:850–862. doi: 10.1016/S1701-2163(16)34304-3. [DOI] [PubMed] [Google Scholar]
- 3.Mc Cann J, Wells R, Voris S. et al. Genital findings in prepubertal girls selected for nonubuse: a decriptive study. Pediatrics. 1990;86:428–439. [PubMed] [Google Scholar]
- 4.Todd I P. Labial adhesions in children. Br Med J. 1946;2:13–14. [PMC free article] [PubMed] [Google Scholar]
- 5.Leung A K, Robson W L. Labial fusion and asymptomatic bacteruria. Eur J Pediatr. 1993;152:250–251. doi: 10.1007/BF01956155. [DOI] [PubMed] [Google Scholar]
- 6.Weissenrieder N, Lochmüller E M. Rezidivierende Vulvasynechien – Differentierte Therapieoptionen. Korasion. 2013;28:19–26. [Google Scholar]
- 7.Caglar M K. Serum estradiol levels in infants with and without labial adhesions: the role of estrogen in the etiology and treatment. Pediatr Dermatol. 2007;24:373–375. doi: 10.1111/j.1525-1470.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- 8.Anthuber S, Anthuber C, Hepp H. Operative Korrektur genitaler Fehlbildungen. Gynäkologe. 2004;37:822–829. [Google Scholar]
- 9.Buck G, Kreienberg R. Kinder- und Jugendgynäkologie: Basiswissen für die Frauenarztpraxis. Gynäkologe. 2010;43:499–516. [Google Scholar]
- 10.Nurzia M J, Eickhorst K M, Ankem M K. et al. The surgical treatment of labial adhesions in pre-pubertal girls. J Pediatr Adolesc Gynecol. 2003;16:21–23. doi: 10.1016/s1083-3188(02)00208-5. [DOI] [PubMed] [Google Scholar]
- 11.Eroglu E, Yip M, Oktar T. et al. How should we treat prepubertal labial adhesions? Retrospective comparison of topical treatments: estrogen only, betamethasone only, and combination estrogen and betamethasone. J Pediatr Adolesc Gynecol. 2011;24:389–392. doi: 10.1016/j.jpag.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Mayoglou L, Dulabon L, Martin-Alguacil N. Success of treatment modalities for labial fusion: a retrospective evaluation of topical and surgical treatments. J Pediatr Adolesc Gynecol. 2009;22:247–250. doi: 10.1016/j.jpag.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Myers J B, Sorensen C M, Wisner B P. et al. Betamethasone cream for the treatment of pre-pubertal labial adhesions. J Pediatr Adolesc Gynecol. 2006;19:407–411. doi: 10.1016/j.jpag.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe T, Matsubara S, Fujinaga Y. et al. Manual separation followed by local cleanliness for pediatric labial adhesion. J Obstet Gynecol Res. 2010;36:667–670. doi: 10.1111/j.1447-0756.2010.01192.x. [DOI] [PubMed] [Google Scholar]
- 15.Thibaud E, Duflos C. Plaidoyer pour lʼenfant: le traitement de la coalescence des petites lèvres est inutile. Arch Pediatr. 2003;10:465–466. doi: 10.1016/s0929-693x(03)00099-x. [DOI] [PubMed] [Google Scholar]
- 16.Leung A K, Robson W L, Kao C P. et al. Treatment of labial fusion with topical estrogen therapy. Clin Pediatr. 2005;44:245–247. doi: 10.1177/000992280504400308. [DOI] [PubMed] [Google Scholar]
- 17.Schober J, Dulabon L, Martin-Alguacil N. et al. Significance of topical estrogens to labial fusion and vaginal introital integrity. J Pediatr Adolesc Gynecol. 2006;19:337–339. doi: 10.1016/j.jpag.2006.06.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


