Abstract
Background
Training of foreign medical graduates in surgical oncology may be an undervalued intervention to improve global cancer care. The aim of this work is to describe the design and results of a clinical training program for international surgeons from a single comprehensive cancer center.
Study Design
Out of 39 international fellows trained over 20 years, 34 were surveyed about education, research, and current context of surgical practice. A citation and H-index query (h number of publications that each has at least h citations) was performed to assess scientific productivity of each graduated fellow.
Results
Twenty-one of 39 (54%) came from countries in which English is not the primary language; Europe was the continent with the most graduates 17 of 39 (43%) while only 5 of 39 (13%) were from Latin America. Three of 39 (8%) were women. Thirty-one of 39 graduated fellows (80%) returned to their countries of origin. The survey response rate was 73% (25 out of 34). Seventeen out of twenty-five (68%) work in an academic setting and thirteen (52%) reported surgical oncology as the main clinical practice. Total number of citations and H-index are homogeneous among the different regions from which the fellows originated with a median of 165 citations and median H-index of 5.
Conclusions
The International General Surgical Oncology Fellowship has successfully trained foreign surgeons for an academic practice in surgical oncology. Most of the graduates have returned to their country of origin and contributed to education and research.
Keywords: Education, International Fellowship, Surgical Oncology, Global
Introduction
Surgery prevails as an essential component of medical care worldwide; at least 11% of the global burden of disease requires surgical management. Nineteen percent of the surgical burden is related to malignant neoplasms.1 Thus, cancer is recognized as a major public health priority. Surgeons and surgery are at the center of care for most patients with solid tumors worldwide, especially in countries with few if any medical or radiation oncologists.
Globally, surgical oncology training has high variability regarding educational curricula and training paradigms. In many countries there are little to no subspecialties within general surgery, and surgical oncology is not recognized as a defined specialty. Frequently no educational infrastructure exists to respond to the local burden of cancer.2 It is rare to have surgeons play a major role in national cancer control policies given a lack of an oncology focus within their careers.
A significant intervention in cancer care is possible with the education of a highly qualified surgical oncology workforce that understands local needs and can foster change towards care improvement, creating a sustainable model of intellectual and technological infrastructure for cancer management.3 Despite the existence of formal core curricula in surgical oncology training4, a meaningful educational experience must be adjusted to the context of each trainee, focusing not only on the acquisition of base knowledge and technical skills, but also on a framework for developing learning skills for continuous self-improvement.
The aim of this work is to describe the design and outcomes of the International General Surgical Oncology Clinical Fellowship at Memorial Sloan Kettering Cancer Center (MSKCC).
Methods
Description of the (MSKCC) General Clinical Surgical Oncology International Fellowship
MSKCC has a long tradition of educating Foreign Medical Graduates (FMG), dating back to the early 20th Century. The majority of such graduates came as residents, spent time on clinical services, and returned to their country of origin. From 1981 to 1993, International fellows were accepted in an ad hoc fashion. Graduates came at varying levels of training, often subsequently completing formal American Board residencies. This process was formalized in 1994. There are 11 standard surgical training programs (i.e. Thoracic, General Surgical Oncology, Head and Neck, Neuro-surgery, Urology, Gynecology, Orthopedics, Pediatrics, Breast, Hepatobiliary and Colorectal) and 12 non-surgical clinical programs (medicine, pediatrics, pathology and radiology) where international medical graduates with a valid ECFMG certificate are eligible to apply. In addition to the surgical oncology fellowships, three other programs are specifically designed for international trainees (gynecologic-oncology, breast imaging training program, and breast pathology).
The International fellows in General Surgical Oncology participate in all perioperative care and obtain direct surgical experience in the operating room, wards and clinics. It is expected that they develop ownership of the patients and participate in all therapeutic decision-making on inpatient rounds, outpatient visits and operative cases. This requires the development and improvement of communication skills with patients, peers and health-allied staff, as often English is not the first language for the fellow. Given the varied backgrounds and health systems from which International fellows come, there can be a major adjustment process to the US health system and culture.
The fellows are encouraged to disclose their interests in specific rotations before starting the training program. These requests are fulfilled as possible while designing their 1 year rotation schedule. Trainees are fully funded by MSKCC.
Through multidisciplinary disease management meetings, case presentations, literature discussion and workup plan assessment during clinical encounters, the fellow learns decision-making and subtle details of oncology care, under the supervision of an experienced surgical oncology attending. They also develop the skills to present cases and relevant literature at multidisciplinary meetings. During the year, there is opportunity to be involved in clinical and health outcomes research, starting from the basics of databases and methodology, to the preparation of a scientific paper and a well-structured talk.
Survey Assessment of Clinical Practice and Educational Outcomes
A web-based survey (SurveyMonkey, TM) was constructed consisting of 25 items grouped in five domains: general background, clinical activity, academic activity, research and education, and a set of two open questions to determine the most relevant life changing effects and suggestions to improve the learning experience of the fellowship. Questions for the survey were generated by a senior surgeon (M.F.B) and two international fellows (I.D.R. and V.M). Two current international fellows were excluded from the survey and citation analysis; contact confirmation was unsuccessful with three fellows. The web-based survey was sent to 34 fellows for whom contact information was previously confirmed by personal email.
Canadian graduates were excluded from the study because they are enrolled in the two year program offered to U.S. fellows, in addition to similarities on cultural, language and graduate education background. An introductory letter accompanied three separate e-mailings over a 3-month period.
A citation query was performed through ISI Web of Science. All publications from each fellow were considered after the year of fellowship graduation. The authors reviewed each publication to confirm authorship and avoid name synonyms. Self-citations were excluded. H index was measured for each author as an indicator of the number and quality of publications. An index of h means that the author has published h publications that each has at least h citations.5 Descriptive non parametric statistics were used to summarize the results using IBM SPSS statistics (version 22). Significance was considered as p<0.05 after Mann-Whitney test.
Results
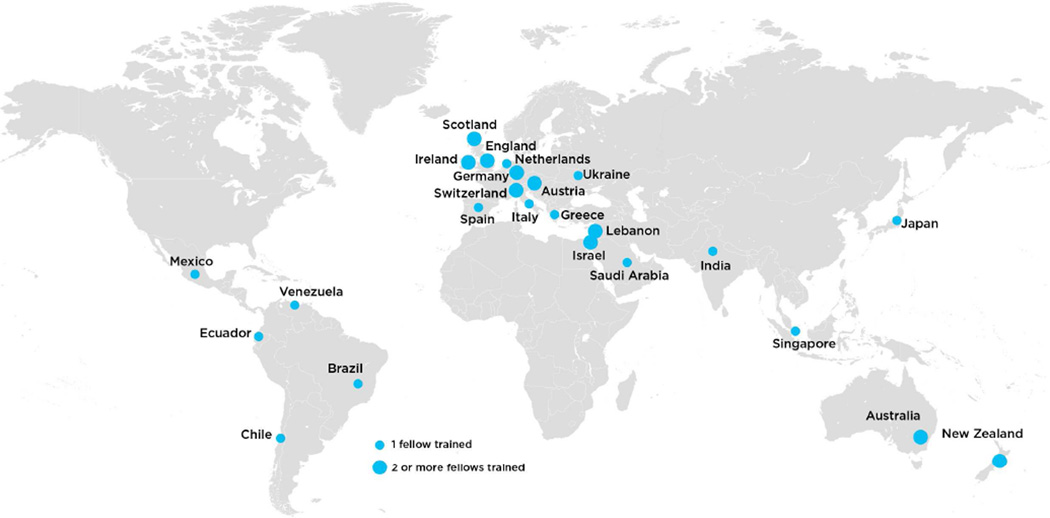
From 1994 to 2014, 39 international fellows from 24 different countries completed the program. Eight (20%) migrated definitively from their country of origin; five before fellowship, completing postgraduate training in general surgery in the U.S. Twenty-one (54%) fellows came from non- native English speaking countries. The regional distribution was: 17(44%) from Europe, 8(21%) from Australia/New Zealand, 6(15%) from Middle East, 5(13%) from Latin America and 3(7%) from Asia. Figure 1
Figure 1.
Worldwide Distribution of Memorial Sloan Kettering Cancer Center International Surgical Oncology Fellows.
Median age at the end of fellowship was 36 years (32–46) with 3 (8%) female trainees. From the group of 25 responders, median age was 36 years (32–46) with 1 (4%) female trainee. Four (16%) migrated from their country of origin; two before and two after the fellowship. The regional distribution was: 11(44%) from Europe, 7 (25%) from Australia/New Zealand, 1 (4%) from Middle East, 3 (12%) from Latin America and 3 (12%) from Asia. No statistical differences were found when comparing to the complete cohort. The median time from training to survey completion was 10 years.
Currently, two international fellows have participated in 408 procedures in a 12-month period (Table 1).
Table 1.
Surgical Case Participation by 2 International Fellows in a 12-Month Period.
| 2014 | Fellow 1 | Fellow 2 | SSO requirements/year |
|---|---|---|---|
| Colorectal | 67 | 49 | 10 |
| Melanoma | 36 | 35 | 10 |
| Complex upper GI | 35 | 34 | 15 |
| Endocrine | 2 | 5 | 4 |
| Thoracic | 47 | 34 | 3 |
| Sarcomas | 36 | 28 | 5 |
| Total | 223 | 185 | 120 |
SSO, Society of Surgical Oncology
The web based survey response rate was 73% (25 out of 34), after excluding two current international fellows and three whose contact information was not confirmed.
Before starting the international fellowship, 9 of 25(36%) had previous surgical oncology training, 9 (36%) research fellowship and 6 (24%) a PhD. After the fellowship, 6 (24%) pursued further surgical oncology training, 1 (4%) research experience and 1(4%) a PhD.
Current Clinical Practice and Educational Outcomes
Median time to first professional appointment after the fellowship was 14 (range 1–30) months, being 3 months (1–30) months in those who returned to their home countries. The most frequent appointments were attending surgeon 56% (14/25) and professor of surgery 52% (13/25). The surgical practice of graduating fellows is based mostly in academic centers 17 (68%). Thirteen (52%) fellows reported general surgical oncology as their current area of practice, and 10 (40%) are still involved in general surgery cases (Table 2).
Table 2.
Surgical Practice and Appointments after the International Fellowship.
| Variable | Frequency of 25 responders, n (%) |
|---|---|
| Appointments After Fellowship | |
| Attending Surgeon | 14 (56) |
| Professor of Surgery | 13 (53) |
| Program Director | 7 (28) |
| Chair | 4 (16) |
| Dean | 1 (4) |
| Context of Surgical Practice | |
| Academic | 17 (68) |
| Public/Government | 12 (48) |
| Private Practice | 7 (28) |
| Administrative | 1 (4) |
| Type of Practice | |
| Surgical Oncology | 13 (52) |
| General Surgery | 10 (40) |
| Thoracic Surgery | 5 (20) |
| Head and Neck | 2 (8) |
Leadership of disease management multidisciplinary meetings in their current centers was reported by 9 (36%) fellows. Personal (76%) and collaborative research contact (14%) is maintained with MSKCC faculty; contact with co-fellows remains for personal (81%) and research (9%) purposes. Membership in National and International cancer societies was reported by 40% and 28% respectively. Only 4 had executive positions in National societies and two in NGOs.
Research lab director appointment was reported by 5 (20%) fellows; 2 (8%) have a journal editor appointment. Involvement on international research collaborations is reported by 54% as well as 68% of participation in clinical trials design. Mentoring has been particularly directed to general surgery residents and medical students with median mentees per fellow of 15 (1–100) and 12 (1–100) respectively. There was less involvement with PhD, Masters and research mentees.
Clinical training was the highest rated contribution from MSKCC fellowship (52%) followed by academic education (33%) and leadership (14%).
Original articles were the most frequent scientific literature published by fellows with a median per fellow of 25 (1–100); 8 (1–100) as first author and 4 (0–100) as last author.
The median H index was 5 (0–23) and median number of citations 165 (0–1698). We found no differences among fellows who originated from native English [H index 6(0–23)/Citations 182(0–1698)] vs. non-native English speaking countries [(H index 5(0–23)/Citations 151(0–1643)](p=0.6) and no differences between those who immigrated [H index 9(2–23)/Citations 476(18–1643)] and those who stayed in their home countries [H index 5(0–23)/Citations 151(0–1698)](p=0.1). Those with more than 10 years of completing the program had significantly higher H index and citations than fellows with less than 10 years of completion [H index 6(2–23) vs 2.5(0–10), p=0.01/Citations 278(13–1698) vs 14(0–521), p=0.001].
No differences among regions of origin were found as shown in Table 3.
Table 3.
Scientific Productivity of 37 Graduates According to Their Countries of Practice.
| Region | H-index | Citations |
|---|---|---|
| Europe | 7 (0–23) | 246(0–1633) |
| Australia/ NZ | 5 (0–17) | 79(0–1698) |
| Middle East | 5 (1–23) | 207(2–1643) |
| Asia | 4 (1–6) | 62(2–278) |
| Latin-America | 2 (1–3) | 18(2–29) |
All data presented as median (range)
Responses from the open questions raised the need for increased time for training of fellows interested in more specialized areas of surgical oncology. Regarding the relevance of the educational experience, a highly positive impact on personal and professional life was the most frequent response of graduates, emphasizing the strong academic-orientation and thoroughness of surgical training.
Discussion
Cancer is overtaking communicable diseases as a high priority health problem in low and middle-income countries. This is a consequence of population aging and changes in lifestyle and standard of living. Unfortunately, although the incidence of cancer is lower than in developed countries, mortality is higher. Delayed diagnosis, lack of primary preventive interventions and inadequate cancer treatment contribute to this burden.6
Surgical oncology education is a crucial intervention to address the global needs of cancer, and the steps to follow towards improvement of survival and quality of care. A trainee, who has had the opportunity to see better standards of care, can lead the process of assessment, -planning, -implementation, -training- and innovation to improve upon previous experiences of global health efforts.7 This can be accomplished through opportunities of formal training as residency, fellowship and even research and short term observerships.
The MSKCC International Fellowship in General Surgical Oncology gives high value to developing an intellectual and surgical expertise background that will serve the trainee in their lifetime practice as an oncologist. The program gives a broad exposure to different areas in surgery and fulfills the recommendations from the Society of Surgical Oncology (SSO) regarding training competences.8 The amount of cases in which the International fellows participate surpasses the minimum 120 cases per year required by the SSO without interfering with the training of U.S. fellows.
Most of the fellows achieved a professional appointment in a short time after completion of fellowship and are practicing as surgical oncologists with concomitant exposure to general surgery cases. A survey from MSKCC U.S. fellows published in 1999 reported that 69% of graduates were involved in academic positions with a high level of job satisfaction.9 Similarly, the International program fosters an academic practice and commitment to mentoring and scientific productivity.
Even though high-income countries (HIC) are the source of most scientific publications on cancer10, H-index of graduated fellows is similar among different regions of origin with no differences between those who migrated to HICs and those who did not.
It is compelling that International fellows are highly involved in the education of medical students and general surgery residents, as this is the time when adequate exposure to surgical mentors may develop interest in young trainees towards an academic surgical career.11
US residency and/or fellowship assures an adequate and standardized learning experience, however, returning to the country of origin has been a remarkable problem in the training of FMGs.12 This perpetuates the cycle of inadequate quality of care, decrease workforce morale and dissuades medical students from enrolling into local training, and as a consequence, promotes further emigration.13
The International fellowship achieved its global surgical oncology education goal, as 80% of trainees returned home. This has been achieved by active enrollment of surgeons with long-term plans of practice and development in their home countries. Less median time to first professional appointment in those who returned home could be a contributing factor that facilitates reinsertion, particularly if fellows already had a planned work position. Opening training opportunities to full trained foreign surgeons is an underestimated educational intervention that may support the shortage of residents choosing highly demanding subspecialties in the U.S., and by the same token, would train surgeons that will succeed returning to their home countries and improve the quality of care. As such, board certification for a foreign surgeon who plans to return home becomes a barrier to access specialized training and promotes FMGs to stay in the US. This is the consequence of being 5 to 7 years away from home in order to be board certified, with no chance to build a professional network that facilitates the reinstatement process. Strengthening relations with foreign governments and academic institutions is needed to assure an efficient educational relationship; this will guarantee support to establish a surgical practice and personnel development.
Defined fellowships such as those offered at MSK, are effective and contribute significantly to subsequent surgical oncology leadership in the country of origin. Currently, from 26 NCCN member institutions, only two offer dedicated international surgical oncology fellowships. However the contribution of one program is small and cannot assist developing nations, when the requirements for entry are the USMLE and at least 5 years surgical experience. Alternative programs are needed.
Brief exposure to U.S. Cancer Care is provided by short-term observerships, such as the ACS International Scholarship Program. During 40 years, 212 surgeons from 62 countries have participated in the program with a positive effect on their practice and opening the possibility of international leadership and remarkable social interactions among surgeons.14 In addition, international teleconferences of educational seminars and disease and management meetings can be explored as a feasible source of continued oncology education.3
Underrepresentation of women in the fellowship, reflects the former status of a male dominated specialty worldwide, which is turning towards being more attractive and inclusive, with no distinction of gender or life roles.15,16
The limitations of this study are the reporting bias that results from obtaining data from a survey and the inclusion of recently graduated fellows who are just starting their practice. Most of the fellows have come from HICs, which limit the generalization of the outcomes to less favored settings.
Improving cancer prevention, early diagnosis and support of research relevant to regional needs, is required to overcome the challenges of cancer.6 Education plays a major role in order to seize the myths of cancer control: unnecessary, unaffordable, unattainable, inappropriate.17 These can be confronted with innovation, global solidarity and building long term infrastructure and research capacity.18,19
The Academic global surgical community has a moral responsibility to decrease the disparities in surgical oncology care. More must be done to break the cycle of inequality.
Acknowledgments
Support: This project was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
References
- 1.WHO. Geneva, Switzerland: [Accessed February 20, 2015]. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Available at: http://www.who.int/bulletin/volumes/86/8/07-050435/en/ [Google Scholar]
- 2.Are C, Malik M, Patel A, et al. The training and certification of surgical oncologists globally. Ann Surg Oncol. 2015;22(3):710–718. doi: 10.1245/s10434-014-4343-9. [DOI] [PubMed] [Google Scholar]
- 3.Brennan M. The Role of U.S. Cancer Centers in Global Cancer Care. Ann Surg Oncol. 2015;22(3):747–749. doi: 10.1245/s10434-014-4341-y. [DOI] [PubMed] [Google Scholar]
- 4.Gershenwald JE, Petrelli N. Fellowship training in surgical oncology--an international affair. Surg Oncol. 2008;17(4):277–279. doi: 10.1016/j.suronc.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch JE. An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A. 2005;102(46):16569–16572. doi: 10.1073/pnas.0507655102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goss PE, Lee BL, Badovinac-Crnjevic T, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol. 2013;14(5):391–436. doi: 10.1016/S1470-2045(13)70048-2. [DOI] [PubMed] [Google Scholar]
- 7.Culp M, Mollura DJ, Mazal J. 2014 RAD-AID Conference on International Radiology for Developing Countries: The Road Ahead for Global Health Radiology. J Am Coll Radiol. 2015;12(5):475–480. doi: 10.1016/j.jacr.2015.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Berman RS, Kurtzman SH, Posner MC, Gershenwald JE. Society of surgical oncology fellowship training: where we have been, where we are now, and where we are going. J Surg Oncol. 2009;100(3):179–181. doi: 10.1002/jso.21305. [DOI] [PubMed] [Google Scholar]
- 9.Heslin MJ, Coit DG, Brennan MF. Surgical oncology fellowship: viable pathway to academic surgery? Ann Surg Oncol. 1999;6(6):542–545. doi: 10.1007/pl00021735. [DOI] [PubMed] [Google Scholar]
- 10.Bakker IS, Wevers KP, Hoekstra HJ. Geographical distribution of publications in the scientific field of surgical oncology. J Surg Oncol. 2013;108(8):505–507. doi: 10.1002/jso.23441. [DOI] [PubMed] [Google Scholar]
- 11.Debas HT, Bass BL, Brennan MF, et al. American Surgical Association Blue Ribbon Committee Report on Surgical Education: 2004. Ann Surg. 2005;241(1):1–8. doi: 10.1097/01.sla.0000150066.83563.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brennan MF. The international medical graduate in the US surgical training system: Perspectives of an aging warrior. Surgery. 2006;140(Fig 1):362–366. doi: 10.1016/j.surg.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;6736(15) doi: 10.1016/j.surg.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Fong Y, Early K, Deane Sa, et al. American College of Surgeons International scholarship programs: 40-year history of support for International Surgical Education. J Am Coll Surg. 2010;211(2):279–284. doi: 10.1016/j.jamcollsurg.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Nadelson CC. Women in surgery. Arch Surg. 1971;102(3):234–235. doi: 10.1001/archsurg.1971.01350030072024. [DOI] [PubMed] [Google Scholar]
- 16.McLemore EC, Ramamoorthy S, Peterson CY, Bass BL. Women in surgery: bright, sharp, brave, and temperate. Perm J. 2012;16(3):54–59. doi: 10.7812/tpp/12.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knaul FM, Atun R, Farmer P, Frenk J. Seizing the opportunity to close the cancer divide. Lancet. 2013;381(9885):2238–2239. doi: 10.1016/S0140-6736(13)60176-2. [DOI] [PubMed] [Google Scholar]
- 18.Kingham TP, Alatise OI. Establishing Translational and Clinical Cancer Research Collaborations Between High- and Low-Income Countries. Ann Surg Oncol. 2015;22(3):37–40. doi: 10.1245/s10434-014-4342-x. [DOI] [PubMed] [Google Scholar]
- 19.Schecter WP. Academic Global Surgery: A Moral Imperative. JAMAsurg. 2015;150(7):605–606. doi: 10.1001/jamasurg.2015.0408. [DOI] [PubMed] [Google Scholar]