Abstract
Objective
To describe hardships experienced by families of children with medical complexity (CMC) and compare them with those experienced by families of children with asthma.
Study design
We assessed hardships in a cohort of 167 families of CMC. Surveys assessed socio-demographics and hardships (e.g., financial: inability to pay bills; social: limited help from family/friends). CMC cohort hardships were compared with those of an established cohort of children hospitalized with asthma using multivariable logistic regression.
Results
CMC had diagnoses in a median of 5 different complex chronic condition categories (most common neurologic/neuromuscular) and the majority (74%) were dependent on technology. Over 80% of families of CMC reported experiencing ≥1 hardship; 68% with financial and 46% with social hardship. Despite higher SES than asthma families, families of CMC often experienced more hardships. For example, families of CMC were significantly more likely to report failure to pay rent/mortgage (aOR 2.6, 95% CI: 1.6, 4.3) and the expectation of little to no help from family/friends (aOR 3.2, 95% CI: 2.1, 5.1).
Conclusions
Families of CMC frequently report financial and social hardships, often at rates higher than asthma families who were generally of lower SES. Identifying and acting upon hardships may be an important addition to the care of CMC.
Advances in medical care have improved the survival of children with chronic, congenital, and critical illness, leading to a rising prevalence of children with medical complexity (CMC).1-3 Such children now account for a disproportionate amount of pediatric healthcare use, an amount that is likely to continue to grow.2, 4 The diagnoses and conditions included in common CMC definitions vary. However, CMC generally share characteristics of chronic, multisystem disease with associated functional limitations including dependence on technology and a need for care provided across multiple clinical sub-specialists and healthcare sectors.4 For example, a child with cerebral palsy, epilepsy, gastrostomy feeding, scoliosis, spasticity, and chronic respiratory insufficiency necessitating respiratory support represents the degree of complexity often present within this population.5
The intensity of care within the healthcare system is augmented by care at home. Families frequently function as a “shadow” healthcare system for CMC.6 Parents become expert caregivers, responsible for the complex, day-to-day care of their child. Parents also fill gaps in the fragmented and uncoordinated healthcare system, functioning as case managers, medical record keepers, and patient advocates.7, 8 As parents assume these roles, their families’ lives are affected both financially and socially. In a national sample of families of CMC, 46% reported spending more than $1,000 out-of-pocket for medical costs per year; 54% reported that a family member stopped working as a result of their child's health.9 A more detailed characterization of these challenges may help to identify ways personnel within the traditional healthcare system could better support families within this “shadow” system.
Financial and social hardships can strain families in ways that make care for children, and especially CMC, more difficult. Traditional markers of poverty and low socioeconomic status (SES) often fail to capture the varied challenges in families’ lives.10-12 Studies have detailed the prevalence and impact of a range of financial and social hardships while also highlighting ways in which typical markers of SES (e.g., income, education, and occupation) are insufficient for children with asthma, the most common chronic disease of childhood.10, 13-16 The construct of financial and social hardship may also provide a more textured characterization of day-to-day challenges families of CMC, similarly dealing with chronic illness, confront in the setting of limited resources. Given the vital role families play in the health of CMC, a deeper understanding of hardships experienced by these families may provide guidance in the development of targeted family-centered interventions. Thus, we sought to first describe the extent of financial and social hardships experienced by a cohort of families of CMC. To benchmark the prevalence and impact of hardship experienced by families of CMC, we then sought to compare hardships faced by families of CMC with those faced by families of children with asthma.
METHODS
Children with Medical Complexity Cohort
We examined data from an observational cohort of 167 families with children who receive primary care through the Complex Care Center at Cincinnati Children's Hospital Medical Center (CCHMC). The Complex Care Center is a medical home to 425 CMC, providing care at both CCHMC's main campus and a satellite facility. In order to be a patient in this program, a child must have a severe, chronic disease, and receive care from ≥3 clinical subspecialists. Families with such children <18 years of age were eligible for inclusion in this study if the primary caregiver understood written or spoken English. Families of children who resided in a nursing home or who were wards of the state were excluded, as we anticipated difficulty in interpreting the day-to-day impact of family-reported hardships.
Eligible families were approached for study enrollment during a clinic visit or were called by phone within 7 days of a clinic visit between November 15, 2013 and July 2, 2014. If an eligible family consented, they completed a 72-question survey administered by study personnel, either face-to-face or via phone. During days that study personnel were not available for recruitment in clinic, families were informed by clinic staff to expect a phone call within 7 days. Each family was called three times that week at varying times of day before being considered a “no contact.” If a family who was considered a “no contact” returned for a second clinic visit during the recruitment period, study personnel attempted to contact them either in-person or with an additional three phone calls.
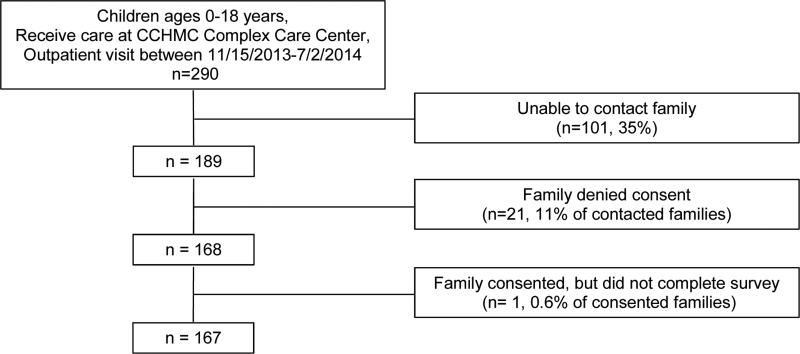
During our recruitment period, 290 families met inclusion criteria (Figure 1; online). Of those, 35% were unable to be contacted, 11% of contacted families denied consent, and one withdrew after consent but before completion of any study procedures. Altogether, study personnel enrolled 88% of families contacted and 58% of all eligible families. Given the desire to minimize impact on patient flow within the clinic, limited study personnel availability during clinic hours, and overwhelming family preference for survey completion by phone, most recruitment and survey completion was done by phone after the visit (n=111, 66.5%).
Figure.
Recruitment diagram for patients and families enrolled in Children with Medical Complexity (CMC) cohort
Greater Cincinnati Asthma Risks Study Cohort
The previously established population-based, prospective observational Greater Cincinnati Asthma Risk Study (GCARS) cohort was used as a comparator. GCARS includes 774 children 1-16 years of age who were hospitalized at CCHMC with asthma or bronchodilator-responsive wheezing between August 11, 2010 and October 20, 2011. Children with significant respiratory or cardiovascular comorbidities (e.g., cystic fibrosis, congenital heart disease) were excluded, as outlined previously.10, 17-20 After consent, study personnel completed face-to-face surveys with English-speaking primary caregivers during the enrollment hospitalization. Given incomplete data on variables of interest, we excluded four respondents from our comparison analysis, yielding a total sample of 770. No children were members of both the CMC and GCARS cohorts.
Measures
The survey given to primary caregivers of CMC included questions focusing on patient and caregiver demographics, measures of SES, and measures of financial and social hardship. These questions, asked of those enrolled in the CMC cohort, were identical to questions used in the GCARS cohort. For the CMC cohort, we also used questions adapted from National Survey of Children with Special Health Care Needs (NS-CSHCN) to assess the family-reported impact of caring for a CMC.9, 21 Medical complexity was evaluated by electronic health record review at the time of enrollment.
Demographic data included patient age, sex, primary and secondary insurer, reported race and ethnicity, and caregiver age, sex, and marital status. Household SES was examined through reported annual household income, educational attainment of the primary caregiver, and assets in the form of home and car ownership. Questions adapted from the NS-CSHCN assessed presence of financial burden, out-of-pocket health-related costs, and necessity of a family member to stop working or cut back on work in order to care for their child.9, 21
Our primary outcomes included measures of financial and social hardships included in the survey. We used nine validated questions that have been previously employed as a part of the U.S. Census Bureau's Survey of Income and Program Participation.13, 14, 22, 23 Financial hardship in the previous year was assessed via a report of having difficulty making ends meet, being unable to pay rent or utilities for financial reasons, borrowing money from others, moving in with others for financial reasons, and any family member not seeking medical care or not filling a prescription for financial reasons. Social hardship was assessed via a family's expectation of little to no help and the inability to borrow money ($1000) from family or friends during times of need. Answers of “yes” to each financial and each social hardship question were considered as indicators of hardship. Each question was analyzed independently.
The electronic health record, reviewed at the time of study enrollment, provided information on the child's clinical characteristics, including complex chronic conditions (CCCs), technology dependence, and the number of subspecialists seen in the prior year. CCCs are defined as “any medical condition that can be reasonably expected to last at least 12 months (unless death intervenes) and to involve either several different organ systems or one system severely enough to require specialty pediatric care and probably some period of hospitalization in a tertiary care center.”24 CCCs are grouped into 11 categories; 25 CCC categories were assessed in both type and number. Technology dependence (e.g., tracheostomy) was defined using the dependence upon medical technology or device subcategory within relevant CCC categories.
Statistical Analyses
Categorical variables were described by counts and frequencies, continuous variables using medians and interquartile ranges (IQR). The CMC and GCARS cohorts were compared with respect to patient and caregiver demographic characteristics and household SES using the Chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables. CMC and asthma families were further compared with respect to hardships using multivariable logistic regression. Covariates in the adjusted models included demographic and SES variables – race, insurance, caregiver age, caregiver marital status, home ownership, and household income. These variables were chosen to account for key demographic differences between cohorts and for potential confounding. Given the distribution of variables and the goal of model stability, we dichotomized race (defined as white vs. non-white), insurance (private vs. public), and marital status (married vs. not married). Results from the multivariable models are presented as adjusted odds ratios (aOR) with associated 95% confidence intervals (CI).
Analyses were performed with SAS v.9.3 (SAS Institute, Cary, NC). The CCHMC Institutional Review Board approved this study.
RESULTS
Of the 167 CMC enrolled, the median age was ~8 years; 63% were male (Table I). Nearly 83% of CMC were reported to be of white race and >40% were covered by a private insurer. Children in the CMC cohort had CCCs in a median of five categories (IQR: 3-6) (Table I). The three most common CCC categories were neurologic or neuromuscular (74%), congenital or genetic defect (69%), and gastrointestinal (68%). Nearly three-quarters of children were dependent on at least one form of technology; with gastrointestinal (65%), respiratory (27%), and neurologic (11%) being the most common. In the year prior to enrollment, children had seen a median of seven different subspecialists (IQR: 5-10). Children in the CMC cohort did not differ from the Complex Care Center population with respect to age, sex, insurance, types of CCC, or technology dependence. They were, however, more likely to be white (83% vs. 65%, p=<0.001), less likely to be Hispanic (1% vs. 7%, p=0.007), had more CCC diagnoses (median 5 vs. 4, p=0.03), and had seen more subspecialists in prior year (median 7 vs. 6, p<0.001).
Table 1.
Demographic for the Children with Medical Complexity (CMC) cohort and the Greater Cincinnati Asthma Risks Study (GCARS) comparator cohort
| CMC Cohort (n=167) | GCARS Cohort (n=770) | p-value* | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
|
Patient Characteristics
| |||||
| Age in years [median, (IQR)] | 7.8 | (4.2-12.3) | 5.4 | (2.9-9.0) | <0.0001 |
| Male sex | 105 | 62.9 | 500 | 64.9 | 0.61 |
| Race | <0.0001 | ||||
| White | 138 | 82.6 | 254 | 33.0 | |
| Black | 23 | 13.8 | 440 | 57.1 | |
| Other | 6 | 3.6 | 76 | 9.8 | |
| Hispanic Ethnicity | 2 | 1.2 | 25 | 3.3 | 0.15 |
| Primary Insurer | <0.0001 | ||||
| Private | 67 | 40.1 | 171 | 22.2 | |
| Public | 100 | 59.9 | 599 | 77.8 | |
| Secondary Insurer | 131 | 81.4 | |||
|
Caregiver Characteristics | |||||
| Age in years[median, (IQR)] | 40 | (32-46) | 30 | (26-35) | <0.0001 |
| Male sex | 24 | 14.4 | 81 | 10.5 | 0.15 |
| Marital Status | <0.0001 | ||||
| Single | 33 | 19.9 | 484 | 66.3 | |
| Married | 98 | 59.0 | 209 | 28.6 | |
| Separated | 14 | 8.4 | 34 | 4.7 | |
| Divorced | 18 | 10.8 | 3 | 0.4 | |
| Widowed | 3 | 1.8 | 0 | 0 | |
|
Clinical Characteristics (Patients in CMC Cohort) | |||||
| Complex Chronic Conditions | |||||
| Neurologic/Neuromuscular | 119 | 74.4 | |||
| Congenital/Genetic defect | 113 | 70.6 | |||
| Gastrointestinal | 109 | 68.1 | |||
| Cardiovascular | 83 | 51.9 | |||
| Respiratory | 77 | 48.1 | |||
| Metabolic | 54 | 33.8 | |||
| Renal | 53 | 33.1 | |||
| Transplant/Miscellaneous | 46 | 28.8 | |||
| Neonatal | 40 | 25.0 | |||
| Hematology/Immunodeficiency | 29 | 18.1 | |||
| Malignancy | 17 | 10.6 | |||
| CCC count [median, (IQR)] | 5 | [3-6] | |||
| Technology Dependence | 119 | 71.3 | |||
| Gastrointestinal | 104 | 65.0 | |||
| Miscellaneous | 46 | 28.8 | |||
| Respiratory | 44 | 27.5 | |||
| Neurologic/Neuromuscular | 18 | 11.3 | |||
| Cardiovascular | 13 | 8.1 | |||
| Renal | 14 | 8.8 | |||
| Metabolic | 4 | 2.5 | |||
| Number of Subspecialists [median, (IQR)] | 7 | [5-10] | |||
p-value assessing comparison between CMC and GCARS cohorts using Chi-square test for categorical variables and Wilcoxon Rank Sum test for continuous variables
Compared with those enrolled in GCARS (Table I), children in the CMC cohort were significantly older, and more likely to be white and privately insured (all p<0.0001). Caregivers of CMC were significantly older and more likely to be married than caregivers of GCARS patients (both p<0.0001).
Socioeconomic status
Families of CMC reported annual household incomes with a bell-shaped distribution: 22% reported income <$15,000 and 22% reported income ≥$90,000 (Table II). Most caregivers reported receiving education beyond high school (80%). A total of 55% reported home ownership and 89% car ownership. Compared with families of GCARS, families of CMC reported significantly higher income, caregiver educational attainment, and rates of home and car ownership (all p<0.0001; Table II).
Table 2.
Socioeconomic status of the Children with Medical Complexity (CMC) cohort and the Greater Cincinnati Asthma Risks Study (GCARS) comparator cohort
| CMC Cohort | GCARS Cohort | p-value* | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Household Income | <0.0001 | ||||
| <$15,000 | 35 | 21.6 | 261 | 34.3 | |
| $15,000 – 29,999 | 41 | 25.3 | 212 | 27.9 | |
| $30,000 – 59,999 | 35 | 21.6 | 154 | 20.3 | |
| $60,000 – 89,999 | 16 | 9.9 | 78 | 10.3 | |
| ≥$90,000 | 35 | 21.6 | 55 | 7.2 | |
| Caregiver Educational Attainment | <0.0001 | ||||
| Less than high school graduate | 9 | 5.4 | 128 | 16.7 | |
| High school graduate or GED | 24 | 14.4 | 212 | 27.6 | |
| Some college | 44 | 26.4 | 224 | 29.2 | |
| 2-year college/technical school graduate | 28 | 16.8 | 86 | 11.2 | |
| 4-year college graduate | 40 | 24.0 | 83 | 10.8 | |
| Any postgraduate work | 22 | 13.2 | 34 | 4.4 | |
| Assets | |||||
| Homeowner | 92 | 55.1 | 170 | 22.1 | <0.0001 |
| Car | 146 | 88.5 | 553 | 72.0 | <0.0001 |
p-value assessing comparison between CMC and GCARS cohorts using Chi-square test for categorical variables and Wilcoxon Rank Sum test for continuous variables
Financial and social hardships
Although 44% of families of CMC reported out-of-pocket medical costs of <$250 in the last year, nearly half reported financial problems resulting from their child's health (Table III). Changes to employment were frequent, with 60% reporting that a family member stopped working and nearly 66% reporting that a family member cut back on work to care for their child (Table III).
Table 3.
Family Reported Impact of Caring for a Child with Medical Complexity (CMC).*
| CMC Cohort (n=167) | ||
|---|---|---|
| n | % | |
| Family's out of pocket health care costs in last 12 months | ||
| <$250 | 73 | 44.0 |
| $250-499 | 27 | 16.3 |
| $500-999 | 21 | 12.7 |
| $1,000-4,999 | 30 | 18.1 |
| ≥$5,000 | 15 | 9.0 |
| Child's health care caused financial problems | 82 | 49.7 |
| Family member stopped working because of child's health | 101 | 60.5 |
| Family member cut work to care for the child | 110 | 65.9 |
| Family member avoided changing jobs to maintain health insurance | 64 | 39.0 |
| Hours/week spent in care coordination [median, (IQR)] | 3 | (1-7) |
Questions adapted from National Survey of Children with Special Health Care Needs (NS-CSHCN)
Approximately 68% reported a financial hardship and >50% a social hardship; ~80% reported ≥1 experienced hardship (Table IV). The most common financial hardship reported by families of CMC was the expressed need to borrow money in the past 12 months (46%). Nearly One-half of families expected little to no help from family/friends when needed and 33% could not count on family/friends for a $1,000 loan.
Table 4.
Financial and social hardships of the Children with Medical Complexity (CMC) cohort and the Greater Cincinnati Asthma Risks Study (GCARS) comparator cohort
| CMC Cohort | GCARS Cohort | Unadjusted OR and 95% CI | Adjusted OR and 95% CI* | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Financial Hardship | 113 | 67.7 | 554 | 72.0 | ||||
| Difficulty making ends meet | 48 | 28.9 | 211 | 27.4 | 1.08 | [0.74, 1.56] | 1.36 | [0.82, 2.24] |
| Unable to pay rent or mortgage | 53 | 32.1 | 140 | 18.3 | 2.12 | [1.46, 3.08] | 2.36 | [1.44, 3.88] |
| Unable to pay utilities | 75 | 44.9 | 273 | 35.6 | 1.47 | [1.05, 2.07] | 1.71 | [1.10, 2.68] |
| Borrowed money | 76 | 45.8 | 412 | 53.5 | 0.74 | [0.52, 1.03] | 1.20 | [0.77, 1.87] |
| Moved in with others | 18 | 10.9 | 97 | 12.6 | 0.85 | [0.50, 1.45] | 1.13 | [0.58, 2.20] |
| Did not see doctor/dentist | 63 | 37.7 | 93 | 12.1 | 4.40 | [3.00, 6.43] | 4.65 | [2.80, 7.73] |
| Did not fill prescription | 38 | 22.8 | 89 | 11.6 | 2.25 | [1.47, 3.44] | 2.02 | [1.18, 3.46] |
| Social Hardship | 93 | 55.7 | 373 | 48.4 | ||||
| Would expect little to no help from family/friends if needed | 77 | 46.4 | 208 | 27.1 | 2.33 | [1.65, 3.29] | 2.94 | [1.86, 4.65] |
| Cannot count on family/friends/bank/other source for $1000 loan if needed | 54 | 32.7 | 323 | 42.1 | 0.67 | [0.47, 0.95] | 1.27 | [0.77, 2.10] |
Obtained from multivariable logistic regression adjusting for household income, homeownership, marital status, patient race, insurer, and caregiver age
Compared with families of GCARS, families of CMC experienced similar-to-higher levels of financial and social hardship (Table IV). After controlling for key demographic SES differences, families of CMC were significantly more likely to report the inability to pay rent/mortgage (aOR 2.4, 95% CI: 1.4, 3.9) and utilities (aOR 1.7, 95% CI: 1.1, 2.7). They were additionally more likely to report that a family member had not seen the doctor or dentist (aOR 4.7, 95% CI: 2.8- 7.7) or filled a prescription (aOR 2.0, 95% CI 1.2, 3.5) due to financial reasons. Additionally, families with CMC were more likely to report an expectation of little to no help from family/friends if needed (aOR 3.2, 95% CI: 2.1, 5.1). Families with CMC less frequently reported difficulty making ends meet, the need to borrow money or move in with others, and the inability to count on family/friends for a loan. However, in adjusted analyses accounting for demographic and socioeconomic differences there was a non-significant tendency towards families with CMC experiencing these hardships more often than families of GCARS (eg, difficulty making ends meet aOR 1.36, 95% CI: 0.82, 2.24).
DISCUSSION
Families of CMC frequently experienced financial and social hardships – four out of five reported at least one. The striking frequencies observed, despite relatively high measures of household SES, suggest that families of CMC may face greater challenges than previously recognized.12 When compared with a relatively socioeconomically disadvantaged cohort of children hospitalized with asthma, CMC experienced similar to higher frequency for many of the assessed hardships even after adjusting for sociodemographic differences.
Our findings are consistent with work detailing the financial and social impact a child's complex chronic medical illness can have on families. In a national sample of families of CMC from the NS-CSHCN, ~50% reported financial problems and employment changes due to their child's medical needs.9 Our findings mirror those with 50% of families in our cohort of CMC reporting financial problems and >60% a change in employment. However, out-of-pocket medical costs were found to be relatively low compared with previously published national samples, suggesting that out-of-pocket expenditures may not be the only driver of financial hardship. We believe that the relatively low out-of-pocket costs to be a reflection of the high number of CMC who were receiving primary or secondary public insurance as a result of their complex medical needs. Insurance premium payouts, a family healthcare expenditure which may lower out-of-pocket expenses, were not assessed in our study.
Only 50% of families in our study reported that a child's health care had caused financial problems, yet nearly 70% reported experiencing financial hardships in the past year. The relationship between a child's chronic illness and family finances is likely complex and may not be reflected in typical measures of SES.26, 27 The costs of care incurred by families of CMC often exceed those captured by out-of-pocket direct costs (e.g., co-pays, deductibles, medications) to include indirect costs such as transportation, child care for siblings, and lost income. Although economic burdens may be universal for all families of children with chronic illness,27-30 families of CMC reported financial hardships more frequently than families of children with asthma, the most common chronic disease of childhood. We hypothesize that this greater impact on CMC families is a consequence of sustained high-intensity, high-cost healthcare use, frequent hospitalizations, and outpatient provider appointments as well as intensive home health care needs.4 Given the sustained intensity of care for CMC, work disruptions are common – the majority of families of CMC in our study reported that a family member either cut back on work hours or stopped working altogether. The economic impact of such work disruptions certainly changes family finances and may explain the high prevalence of several of the financial hardships examined. For example, an existing mortgage payment may become unaffordable as a family's income trajectory changes with work disruptions to care for their child. Prospective studies that longitudinally assess income, medical expenditures, financial hardships, and financial coping strategies (e.g., fundraising, borrowing) are needed to understand the full economic impact of caring for CMC.
Financial hardships were paralleled by prevalent social hardships for families of CMC. Social support of family and friends can help caregivers cope with the child's illness, and provide an opportunity for respite and normalcy.26, 31 Compared with families of children with asthma, families of CMC more frequently reported social isolation. A lower degree of social isolation in children with asthma may be due to its higher prevalence, especially among poor, urban populations like the GCARS cohort. Alternatively, families of children with asthma may feel this burden but feel it differently at different times over the course of the year, given asthma's seasonal nature. Regardless, having a CMC portends a daily, persistent, high burden of care. Previous studies have described this difficulty families of CMC face in attaining support from others family members, often stemming from limited time and energy for socialization.26, 32
Financial and social hardships help to paint a picture of the day-to-day challenges and stresses faced by these families. Even though these stresses are often overlooked in the clinical care of CMC, it is easy to imagine how the described hardships may impact health outcomes. For example, a family's need to pay rent or utilities may result in cost-shifting away from a child's medical care (ie, pay rent or electricity bill over a child's medications or gas to allow travel to appointments).33 Similarly, limited social supports may affect a family's ability to deal with even routine stressors. For example, the illness of a primary caregiver could translate into an unnecessary respite hospitalization without available social supports. Hardships, competing priorities, and day-to-day routine complexities have been shown to influence health outcomes of children with asthma.10, 34, 35 Our study findings highlight a critical need to understand the causes and consequences of financial and social hardships for CMC.
There are several limitations. First, potential bias exists as we relied on caregiver report for hardship outcome variables. However, if there was a social desirability bias in caregiver responses, we may have expected less report of hardship. Second, there were differences in accrual methods between the CMC and GCARS cohorts. Caregivers of children with asthma completed study questionnaires during hospitalizations. It is possible that family perception and report of hardship may be different during a stressful hospitalization. Further, we experienced challenges in contacting families of CMC for study participation. The families that we were not able to contact by phone may experience hardships differently than those in our cohort. Also, our results may not be generalizable to all families of CMC. Indeed, differences exist between the cohort of CMC and the Complex Care Center population. For example, we were not able to recruit non-English speaking families. In our center, this represents < 5% of the population. It is possible that caregivers with limited English proficiency may face even greater hardships.36 Finally, the children in our cohort receive care in a medical home dedicated to the care of CMC. Children referred to a complex care program may have more severe disease and more intense healthcare needs than the general population of CMC, making them more likely to experience hardships. However, it is also possible that our study may underestimate the true prevalence of hardships in other populations of CMC as this medical home is staffed by physicians, nurses, care coordinators, and social workers with intimate knowledge of patients and families who strive to address the child's medical needs and the family's social needs.37 Evidence suggests that hardships are reduced when CMC receive coordinated care in just such a medical home.28
Further studies are needed to understand the relationship between family-experienced hardships and resource utilization of CMC, as well as to identify characteristics of CMC (e.g., CCC category, type of technology dependence, receipt of home health care) associated with hardships. Identifying and acting upon family-experienced hardships may be an important addition to the care of CMC. Programs that have been used to address social determinants of poor health in high risk populations, including children with asthma, should be considered to address the financial and social challenges faced by families of CMC. At-risk patients and families can be connected to appropriate resources both within the healthcare system as well as within the community.38-40 Many hospitals and primacy care centers serving families of CMC have access to medical-legal partnerships, financial counseling services, and/or mental health services.41-44 These resources, in conjunction with enhanced care coordination and home caregiver support may be particularly important for families of CMC affected by financial and social hardship.45 Similarly, these families may benefit from referrals to private charities, non-profit agencies, or parent support groups that may exist outside the walls of the health system.46 Should such referrals prove to be of value for families of CMC, there may be policy implications within evolving payment models. Indeed, as payment schemes move away from fee-for-service and toward pay- for-performance programs like accountable care organizations and patient-centered medical homes, services, referrals, and programs that reduce hardship and improve health may prove cost-effective and worthy of coverage. Further research into the value of such interventions is warranted.
Families of CMC frequently experience financial and social hardships, despite often reassuring measures of SES. In fact, similar to higher levels of hardship were reported by CMC families compared with relatively disadvantaged asthma families. Traditional measures of financial burden (eg, SES, out-of-pocket spending) seem to underestimate struggles experienced by families of CMC. Identifying and acting upon hardships may be an important addition to the care of children with medical complexity.
Acknowledgments
The Greater Cincinnati Asthma Risks Study was funded by the National Institutes of Health (NIH; 1R01A188116 [PI: R.K; co-investigators: A.B. and J.S.]). J.T. was supported by National Research Service Award (T32HP10027-14). The use of REDCap was supported by the Center for Clinical and Translational Science and Training (National Center for Research Resources/NIH UL1-RR026314-01).
Abbreviations
- CMC
children with medical complexity
- CCC
complex chronic condition
- CI
confidence interval
- GCARS
Greater Cincinnati Asthma Risks Study
- CCHMC
Cincinnati Children's Hospital Medical Center
- SES
socioeconomic status
- IQR
interquartile range
- aOR
adjusted odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
REFERENCES
- 1.Berry JG, Hall M, Hall DE, Kuo DZ, Cohen E, Agrawal R, et al. Inpatient growth and resource use in 28 children's hospitals: a longitudinal, multi-institutional study. JAMA pediatrics. 2013;167:170–7. doi: 10.1001/jamapediatrics.2013.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burns KH, Casey PH, Lyle RE, Bird TM, Fussell JJ, Robbins JM. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126:638–46. doi: 10.1542/peds.2009-1658. [DOI] [PubMed] [Google Scholar]
- 3.Simon TD, Berry J, Feudtner C, Stone BL, Sheng X, Bratton SL, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126:647–55. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127:529–38. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srivastava R, Stone BL, Murphy NA. Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–87. doi: 10.1016/j.pcl.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Schuster MA, Chung PJ, Vestal KD. Children with health issues. Future Child. 2011;21:91–116. doi: 10.1353/foc.2011.0017. [DOI] [PubMed] [Google Scholar]
- 7.Bookman A, Harrington M. Family caregivers: a shadow workforce in the geriatric health care system? J Health Polit Policy Law. 2007;32:1005–41. doi: 10.1215/03616878-2007-040. [DOI] [PubMed] [Google Scholar]
- 8.Putney AP. Across State Lines, A Family Navigates Medical Complexity And Medicaid Hurdles. Health Aff (Millwood) 2015;34:1241–4. doi: 10.1377/hlthaff.2015.0431. [DOI] [PubMed] [Google Scholar]
- 9.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A National Profile of Caregiver Challenges Among More Medically Complex Children With Special Health Care Needs. Arch Pediatr Adolesc Med. 2011;165:1020–6. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133:431–9. doi: 10.1542/peds.2013-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–84. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- 12.Kuo DZ, Goudie A, Cohen E, Houtrow A, Agrawal R, Carle AC, et al. Inequities in health care needs for children with medical complexity. Health Aff (Millwood) 2014;33:2190–8. doi: 10.1377/hlthaff.2014.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danziger S, Corcoran M, Danziger S, Heflin CM. Work, income, and material hardship after welfare reform. J Consum Aff. 2000;34:6–30. [Google Scholar]
- 14.Jencks C, Mayer S. Poverty and the distribution of material hardship. J Hum Resources. 1989;24:88–114. [Google Scholar]
- 15.Suglia SF, Duarte CS, Sandel MT, Wright RJ. Social and environmental stressors in the home and childhood asthma. J Epidemiol Community Health. 2010;64:636–42. doi: 10.1136/jech.2008.082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howrylak JA, Spanier AJ, Huang B, Peake RW, Kellogg MD, Sauers H, et al. Cotinine in children admitted for asthma and readmission. Pediatrics. 2014;133:e355–62. doi: 10.1542/peds.2013-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moncrief T, Beck AF, Olano K, Huang B, Kahn RS. Routinely sleeping away from home and the association with child asthma readmission. J Community Health. 2014;39:1209–15. doi: 10.1007/s10900-014-9880-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newman NC, Ryan PH, Huang B, Beck AF, Sauers HS, Kahn RS. Traffic-related air pollution and asthma hospital readmission in children: a longitudinal cohort study. J Pediatr. 2014;164:1396–402. e1. doi: 10.1016/j.jpeds.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spanier AJ, Beck AF, Huang B, McGrady ME, Drotar DD, Peake RW, et al. Family hardships and serum cotinine in children with asthma. Pediatrics. 2015;135:e416–23. doi: 10.1542/peds.2014-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Dyck PC, McPherson M, Strickland BB, Nesseler K, Blumberg SJ, Cynamon ML, et al. The national survey of children with special health care needs. Ambulatory pediatrics : the official journal of the Ambulatory Pediatric Association. 2002;2:29–37. doi: 10.1367/1539-4409(2002)002<0029:tnsocw>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Ouellette T, Burstein N, Long D, Beecroft E. Measures of material hardship: Final report. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; Washington, DC: 2004. [Google Scholar]
- 23.United States Census Bureau Survey of Income and Program Participation; [May 1, 2014]. http://www.census.gov/programs-surveys/sipp/about.html. [Google Scholar]
- 24.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths Attributed to Pediatric Complex Chronic Conditions: National Trends and Implications for Supportive Care Services. Pediatrics. 2001;107:e99–e. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 25.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC pediatrics. 2014;14:199. doi: 10.1186/1471-2431-14-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103:1235–42. doi: 10.1542/peds.103.6.1235. [DOI] [PubMed] [Google Scholar]
- 27.Bona K, Dussel V, Orellana L, Kang T, Geyer R, Feudtner C, et al. Economic impact of advanced pediatric cancer on families. J Pain Symptom Manage. 2014;47:594–603. doi: 10.1016/j.jpainsymman.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuhlthau K, Hill KS, Yucel R, Perrin JM. Financial burden for families of children with special health care needs. Maternal and child health journal. 2005;9:207–18. doi: 10.1007/s10995-005-4870-x. [DOI] [PubMed] [Google Scholar]
- 29.Okumura MJ, Van Cleave J, Gnanasekaran S, Houtrow A. Understanding factors associated with work loss for families caring for CSHCN. Pediatrics. 2009;124(Suppl 4):S392–8. doi: 10.1542/peds.2009-1255J. [DOI] [PubMed] [Google Scholar]
- 30.Parish SL, Shattuck PT, Rose RA. Financial burden of raising CSHCN: association with state policy choices. Pediatrics. 2009;124(Suppl 4):S435–42. doi: 10.1542/peds.2009-1255P. [DOI] [PubMed] [Google Scholar]
- 31.Hudson SM, Newman SD, Hester WH, Magwood GS, Mueller M, Laken MA. Factors influencing hospital admissions and emergency department visits among children with complex chronic conditions: a qualitative study of parents' and providers' perspectives. Issues Compr Pediatr Nurs. 2014;37:61–80. doi: 10.3109/01460862.2013.855844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caicedo C. Families With Special Needs Children: Family Health, Functioning, and Care Burden. Journal of the American Psychiatric Nurses Association. 2014 doi: 10.1177/1078390314561326. [DOI] [PubMed] [Google Scholar]
- 33.Bona K, London WB, Guo D, Abel G, Lehmann L, Wolfe J. Prevalence and impact of financial hardship among New England pediatric stem cell transplantation families. Biol Blood Marrow Transplant. 2015;21:312–8. doi: 10.1016/j.bbmt.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Moncrief T, Beck AF, Simmons JM, Huang B, Kahn RS. Single parent households and increased child asthma morbidity. J Asthma. 2014;51:260–6. doi: 10.3109/02770903.2013.873806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith LA, Bokhour B, Hohman KH, Miroshnik I, Kleinman KP, Cohn E, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–9. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 36.Eneriz-Wiemer M, Sanders LM, Barr DA, Mendoza FS. Parental limited English proficiency and health outcomes for children with special health care needs: a systematic review. Academic pediatrics. 2014;14:128–36. doi: 10.1016/j.acap.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Perrin JM. Patient-centered medical home for high-risk children with chronic illness. JAMA. 2014;312:2625–6. doi: 10.1001/jama.2014.16514. [DOI] [PubMed] [Google Scholar]
- 38.Garg A, Sandel M, Dworkin PH, Kahn RS, Zuckerman B. From medical home to health neighborhood: transforming the medical home into a community-based health neighborhood. J Pediatr. 2012;160:535–6. e1. doi: 10.1016/j.jpeds.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 39.Henize AW, Beck AF, Klein MD, Adams M, Kahn RS. A Road Map to Address the Social Determinants of Health Through Community Collaboration. Pediatrics. 2015;136:e993–e1001. doi: 10.1542/peds.2015-0549. [DOI] [PubMed] [Google Scholar]
- 40.Beck AF, Tschundy MM, Coker TR, Mistry KB, Cox J, Gitterman B, et al. Determinants of Health and Pediatric Primary Care Practices. Pediatrics. 2015 doi: 10.1542/peds.2015-3673. in press. [DOI] [PubMed] [Google Scholar]
- 41.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children--outcomes from a successful partnership between professions. J Health Care Poor Underserved. 2013;24:1063–73. doi: 10.1353/hpu.2013.0147. [DOI] [PubMed] [Google Scholar]
- 42.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children's well-child care visits: the WE CARE Project. Pediatrics. 2007;120:547–58. doi: 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 43.Cohen E, Fullerton DF, Retkin R, Weintraub D, Tames P, Brandfield J, et al. Medical-legal partnership: collaborating with lawyers to identify and address health disparities. J Gen Intern Med. 2010;25(Suppl 2):S136–9. doi: 10.1007/s11606-009-1239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Worley G, Rosenfeld LR, Lipscomb J. Financial counseling for families of children with chronic disabilities. Dev Med Child Neurol. 1991;33:679–89. doi: 10.1111/j.1469-8749.1991.tb14945.x. [DOI] [PubMed] [Google Scholar]
- 45.Peckham A, Spalding K, Watkins J, Bruce-Barrett C, Grasic M, Williams AP. Caring for caregivers of high-needs children. Healthcare quarterly (Toronto, Ont) 2014;17:30–5. doi: 10.12927/hcq.2014.24017. [DOI] [PubMed] [Google Scholar]
- 46.Garg A, Sarkar S, Marino M, Onie R, Solomon BS. Linking urban families to community resources in the context of pediatric primary care. Patient Educ Couns. 2010;79:251–4. doi: 10.1016/j.pec.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]