Abstract
Objective
This study addressed gaps in the existing literature about correlates of parental perception of child weight using a community sample. We evaluated how weight-status and its perception related to parents’ personal and parenting attitudes/behaviors.
Methods
Participants were parents (N=1007; 65.3% mothers, 34.4% fathers) of children 5–15 years old. Parents completed online measures of personal eating attitudes/behaviors, attitudes/behaviors about their children’s eating and weight, and parental practices related to weight-related attitudes.
Results
Parents frequently underestimated children’s overweight/obesity, even more frequently than their own overweight/obesity (p<.001). Parents’ personal eating attitudes/behaviors were related to their own weight-status (p<.001) and perceived child weight-status (p<.001) but not actual child weight-status. Parents’ child-focused eating attitudes/behaviors were related to actual (p<.001) and perceived child weight-status (p<.001), but not parent weight-status.
Conclusions
In general, parents’ personal attitudes/behaviors did not extend into their perceptions of their child’s weight or their response to it. Results suggest a dual need to improve parent accuracy perceiving children’s overweight/obesity, and to guide parent responses to perceived overweight/obesity. Given the high prevalence of childhood obesity, and the serious consequences during childhood and into adulthood, further research is needed to enhance understanding of parents’ specific needs to engage in prevention and treatment programs.
Keywords: pediatric, parenting, psychosocial research, childhood obesity
Introduction
Pediatric overweight (>85th percentile for body mass index; BMI) and obesity (>95th BMI percentile) remain serious health concerns and the focus of prevention and intervention efforts.1 Families play a critical role in pediatric obesity treatment because of the influence parents have on the home environment.2–4 Parents structure daily routines, choose foods for the home, and model eating and exercise.5,6 Parents facilitate children’s access to health services, including obesity programs,7,8 and parent involvement in these programs leads to better outcomes than youth-only programs.5 Parents who recognize overweight as a health problem for their child report greater readiness to make behavioral changes,7 and parents who perceive child overweight also report greater restriction of their child’s diet.9,10 Yet, research has consistently shown that parents fail to identify pediatric obesity, for example, by underestimating child weight-status.7,8,11–21 Compared with well-documented underestimation, attitudinal/behavioral correlates are under-explored. One study found that parents’ personal weight concerns were unrelated to perceived child weight.18 This was the only study that evaluated parent characteristics with child weight underestimation; however, another study evaluated associated parent perceptions. This study found that when parents underestimated child weight-status, they were less likely to perceive overeating and more likely to perceive (inaccurately) that their child was physically active.16 Other research on misperception has focused almost exclusively on demography. Some evidence indicates parents are more likely to underestimate sons’ than daughters’ weight,11–15 although differences did not arise in other studies.16,17 When examined, racial/ethnic differences have generally not been significant,11,12 although other work has suggested Black and Hispanic mothers were more likely than White and Asian mothers to underestimate.14 Parent obesity has been shown to relate to child weight underestimation,7,11,14 although not in all studies.13 Parents appear more able to perceive obesity in older children, although misperception is still common,11,12 and this age pattern has not arisen consistently.16
An association between underestimation and lower concern about child weight has been suggested11,12,16,18,20 but the direction of this relationship is unknown. Parents could perceive their child not to have obesity and therefore not be concerned about weight-related problems, as suggested by associations between underestimation and parent readiness to change weight-related family behaviors,7 as well as parents’ declining of obesity program enrollment.8 Parents could be unwilling to label their child as overweight/obese.11 Or, as small-sample focus group data suggest, parents could use stereotypes (perceiving laziness or unhealthy eating) and impairments (teasing or difficulty with physical activity) to decide whether their child has obesity instead of body size.20
Weight perception accuracy has been hypothesized to relate to weight-loss behaviors, but evidence concerning this relation is unclear. In one study, parental accuracy about child weight was unrelated to whether parents changed family meal/eating behaviors to promote weight loss.13 However, parent perception of child obesity (accurately and inaccurately) was related to encouraging children’s dieting behavior.13 Accuracy was unrelated to youth’s personal weight loss behaviors, although youths’ self-perceptions were related to weight loss attempts.19
The current study aimed to extend the literature on parental perception of child weight using a community sample to address important knowledge gaps about the correlates of parental perception of child weight. In this cross-sectional study, our goal was to evaluate how weight perception related to parents’ personal eating attitudes/behaviors, their attitudes/behaviors related to their child, and their parenting practices. Based on earlier research that established misperception, we hypothesized that parents would underestimate child obesity. We further hypothesized that parents’ personal eating attitudes/behaviors, and their attitudes/behaviors related to their child’s eating would be directly related to perceived obesity and parental feeding practices encouraging weight loss (e.g., greater restriction when they perceived their child to be a higher weight).
Methods
Participants
Participants (N=1007) completed a survey on parents’ opinions about weight and eating on the Mechanical Turk website. Participants were aged 21–65, had a child aged 5–15, and were primary caregivers. Participants were mothers (n=658, 65.3%) and fathers (n=346, 34.4%; n=3 gender not reported), most of whom were biological parents (n=891, 88.5%). Parents self-identified as White (n=848, 84.2%), Black (n=66, 6.6%), Hispanic (n=60, 6.0%), Asian (n=37, 3.7%), Multiracial (n=24, 2.4%), or Other (n=21, 2.1%). Parent education was high school or less (n=139, 13.8%), some college (n=395, 39.2%), or college degree or higher (n=472, 46.9%). On average, parents were aged 35.99 (SD=7.86) and had BMIs of 29.06 kg/m2 (SD=7.91). Survey items focused on one child; responses pertained to daughters (n=497, 49.4%) and sons (n=497, 49.4%). On average, children were aged 10.16 (SD=3.02) with 66.17th BMI percentiles (SD=32.56; BMI z-score M=0.59, SD=1.41). This study received ethical approval.
Measures
Body Mass Index (BMI)
Parents reported anthropometric data for themselves and their child. Parent weight-status was classified by BMI (kg/m2): underweight <18.5; healthy-weight 18.5–25; overweight 25–30; obesity >30. Child weight-status was classified by BMI percentile (based on age- and sex-specific growth curves): underweight <5th; healthy-weight 5–85th; overweight 85–95th; obesity >95th.
Child Feeding Questionnaire (CFQ)
This measure of parental feeding practices has 31 items rated on five-point scales22 and was scored following the Anderson and colleagues model,23 which showed superior fit to the original factor-structure in a diverse community sample. Items yielded internally consistent subscale (Perceived Responsibility, Concerns about Child Weight, Restriction, Pressure to Eat, and Monitoring) scores in the development sample, α=.70–.92,22 and the current study, α=.78–.91. Items assessing weight perception came from the original CFQ; these items were not included in the subscales by the Anderson scoring method.
Eating Disorder Examination Questionnaire (EDE-Q)
The EDE-Q retrospectively measures eating attitudes/behaviors over 28 days24; we used a brief seven-item version demonstrating superior psychometric properties in nonclinical25 and clinical26 populations. Items are scored on a seven-point scale. Subscales (Restraint, Overvaluation, Dissatisfaction) were internally consistent in earlier work, α=.89–.91,25 and in the current study α=.89–.92. Additionally, EDE-Q items were adapted (EDE-Q-PV) to assess parents’ restraint of their child’s diet, parents’ overvaluation of themselves according to their child’s weight/shape, and parents’ dissatisfaction with their child’s weight/shape. Adaptations changed “you” to “your child.” The brief EDE-Q-PV was internally consistent, α=.66–.95.
Fat Talk Questionnaire (FTQ)
This 16-item measure of negative conversations about weight (“fat talk”) common among young adult women27 was adapted to assess how parents talk in front of their child about their own weight, persons with obesity, and their child’s weight. Items are scored on a five-point scale. The FTQ had excellent internal consistency in the development study (α=.93) and in the current study (self α=.96, persons with obesity α=.97, child α=.96).
Statistical Analyses
Z-tests for proportions compared parents’ perceptions of child weight with their own weight perceptions. Pearson correlations compared inaccuracy (underestimation and overestimation) with continuous variables and chi-squares compared inaccuracy with categorical variables. Correlations used a Bonferroni correction for multiple comparisons within each scale’s set of subscales. An exploratory chi-square analysis evaluated inaccuracy (underestimation and overestimation) between parents whose children were 5–12 years old (school-aged), and parents whose children were 13–15 years old (adolescents).
Analyses of variance (ANOVAs) evaluated parents’ personal eating attitudes/behaviors, their attitudes/behaviors related to their child’s eating and body image, fat talk, and parental feeding practices. Child weight-status, perceived child weight-status, and parent weight-status were independent variables in separate analyses. Missing data were deleted listwise from individual analyses. Omnibus findings used a Bonferroni correction for multiple comparisons within each set of analyses; alpha for significance was adjusted to 0.017. Significant omnibus findings were evaluated pairwise using Tukey adjustment for multiple comparisons.
Results
Perceptions of Weight-Status
Table 1 shows proportions of parents who correctly labeled the weight-status of their child and themselves. About their child, 49.0% of parents correctly labeled their child’s weight-status; 45.2% classified their child with a lighter weight-status than they actually had (underestimated), and 5.8% classified their child with a heavier weight-status than they actually had (overestimated). About themselves, 62.8% correctly labeled their own weight-status; 30.1% underestimated, and 7.1% overestimated. Parents were significantly less likely to be accurate about their child’s overweight than their own overweight (Z=−7.75, p<.001), as well as about obesity (Z=−9.60, p<.001).
Table 1.
Accuracy proportions by weight-status
| Correct Underweight1 | Correct Healthy-Weight2 | Correct Overweight3 | Correct Obese4 | |
|---|---|---|---|---|
| Parent Perception of Child Weight | 52.3% | 75.7% | 26.9%* | 10.2%* |
| Beliefs about Others’ Perception of Child Weight | 53.9% | 75.9% | 21.7%* | 11.3%* |
| Parent Perception of Parent Weight | 44.4% | 81.3% | 64.1% | 47.1% |
Note.
Significantly (p<.001) lower than proportion of parents who correctly perceived their own weight-status in this category.
n=65 youths were underweight (BMI percentile <5), n=27 parents were underweight (BMI <18.5).
n=498 youths were healthy-weight (BMI percentile 5–85), n=320 parents were healthy-weight (BMI 18.5–25).
n=175 youths were overweight (BMI percentile 85–95), n=284 parents were overweight (BMI 25–30).
n=247 youths were obese (BMI percentile >95), n=367 parents were obese (BMI >30).
Table 2 shows correlations examining relations among misperception of child weight and parents’ personal eating attitudes/behaviors, parenting eating attitudes/behaviors, fat talk, parental feeding practices, and demographic characteristics. Underestimation of child weight-status was significantly related to higher parent BMI (r=−.08, p=.02), younger child age (r=.11, p=.001), male child gender (χ2=28.34, p<.001, φ=.170), and less fat talk about persons with obesity (r=.11, p=.001) and their child (r=.09, p=.005). Because of the significant correlation of underestimation with child age, an exploratory analysis evaluated the relation between inaccuracy and child age group (child 5–12 years old compared with adolescent 13–15 years old). Parents were more likely to underestimate children (47.6%) than adolescents (36.5%, p=.004), and were more likely to correctly estimate adolescents (57.5%) than children (46.6%, p=.004), but overestimation did not significantly differ (p=.92).
Table 2.
Correlations with Child and Self Weight Misperception
| Child Weight Misperception (r) | Parent Weight Misperception (r) | |
|---|---|---|
| Personal Eating Attitudes/Behaviors | ||
| Restraint | .05 | .04 |
| Overvaluation | −.01 | .08** |
| Dissatisfaction | −.004 | .03 |
| Attitudes/Behaviors about Child’s Eating and Body Image | ||
| Restraint | −.02 | −.04 |
| Overvaluation | .01 | .05 |
| Dissatisfaction | −.02 | .01 |
| Fat Talk | ||
| Self | .02 | .10** |
| Obese Persons | .11*** | .05 |
| Child | .09** | .01 |
| Parental Feeding Practices | ||
| Perceived Responsibility | −.02 | .06*† |
| Concern about Child Weight | .01 | .03 |
| Restriction | .02 | .04 |
| Pressure to Eat | −.07*† | −.01 |
| Monitoring | .02 | .04 |
| Demographic Characteristics | ||
| Age (Parent) | .06 | .01 |
| Age (Child) | .11** | −.01 |
| Years of Education (Parent) | .03 | .05 |
Note. N=1007.
p<.05,
p<.01,
p<.001,
No longer significant with Bonferroni correction for multiple comparisons. Positive correlations indicate underestimation is associated with less of the variable and negative correlations indicate underestimation is associated with more of the variable.
Parents were more likely to underestimate their weight-status if they were Black (χ2=13.28, p=.001, φ=.134) or fathers (χ2=65.44, p<.001, φ=.256), and less likely to underestimate if they were Asian (χ2=14.27, p=.001, φ=.139). Parents’ self-underestimation was related to lower overvaluation of their own shape/weight (r=.08, p=.01), and less fat talk about themselves (r=.10, p=.002).
Eating Attitudes/Behaviors
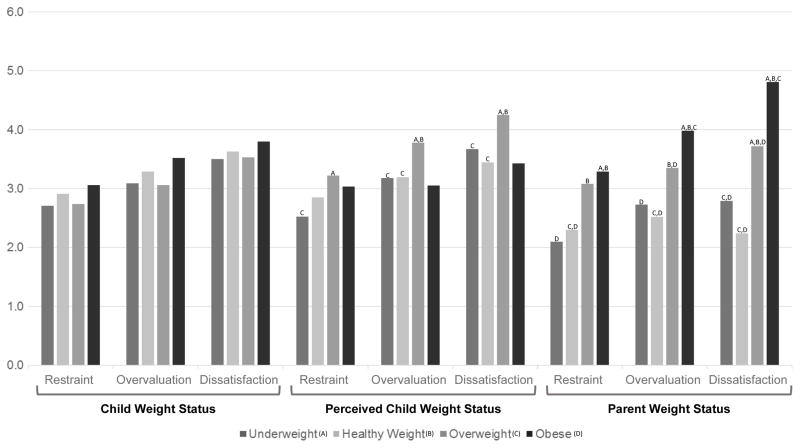
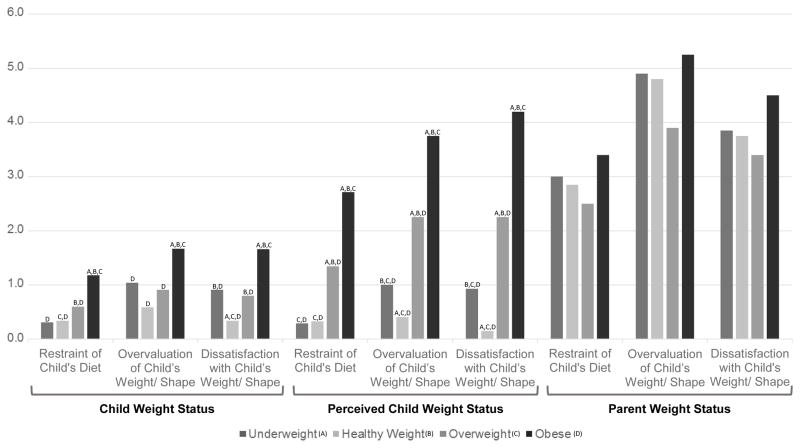
ANOVAs evaluated whether child weight-status, perceived child weight-status, and parent weight-status were associated with EDE-Q (Figure 1) and EDE-Q-PV (Figure 2) subscales.
Figure 1.
Comparisons of parents’ personal eating attitudes/behaviors. Note. Letters denote significant pairwise comparisons (using Tukey correction for multiple comparisons) at the p<.05 level compared with a=underweight, b=healthy-weight, c=overweight, or d=obese. Omitted letters indicate nonsignificant pairwise comparisons.
Figure 2.
Comparisons of parenting eating attitudes/behaviors. Note. Letters denote significant pairwise comparisons (using Tukey correction for multiple comparisons) at the p<.05 level compared with a=underweight, b=healthy-weight, c=overweight, or d=obese. Omitted letters indicate nonsignificant pairwise comparisons.
Parents’ personal EDE-Q scores were not associated with child weight-status (Restraint: F(3,982)=0.93, p=.43, ηp2=.005; Overvaluation: F(3,982)=2.10, p=.10, ηp2=.006; Dissatisfaction: F(3,982)=0.79, p=.50, ηp2=.002). EDE-Q scores on Overvaluation (F(3,999)=4.47, p=.004, ηp2=.013) and Dissatisfaction (F(3,999)=7.92, p<.001, ηp2=.023) were significantly associated with perceived child weight-status, but Restraint was not significant (F(3,998)=2.95, p=.03, ηp2=.009). EDE-Q scores were higher when parents perceived child overweight compared with perceived child healthy-weight and underweight. EDE-Q scores were even more strongly associated with parents’ weight-status, Restraint (F(3,999)=14.29, p<.001, ηp2=.041; Overvaluation: F(3,999)=33.99, p<.001, ηp2=.093; Dissatisfaction: F(3,999)=131.27, p<.001, ηp2=.283). EDE-Q scores were generally higher in overweight/obesity than underweight/healthy-weight.
EDE-Q-PV scores were associated with child weight-status (Restraint-PV: F(3,982)=35.49, p<.001, ηp2=.098; Overvaluation-PV: F(3,982)=27.18, p<.001, ηp2=.077; Dissatisfaction-PV: F(3,982)=51.64, p<.001, ηp2=.136). Scores were even more strongly associated with perceived child weight-status (Restraint-PV: F(3,999)=101.81, p<.001, ηp2=.234; Overvaluation-PV: F(3,999)=134.17, p<.001, ηp2=.287; Dissatisfaction-PV: F(3,999)=294.16, p<.001, ηp2=.469). EDE-Q-PV scores were generally higher for actual and perceived child obesity compared with actual and perceived child underweight, healthy-weight, and overweight. EDE-Q-PV scores were not associated with parent weight-status (Restraint-PV: F(3,999)=1.37, p=.25, ηp2=.004; Overvaluation-PV: F(3,999)=1.63, p=.18, ηp2=.005; Dissatisfaction-PV: F(3,999)=1.32, p=.27, ηp2=.004).
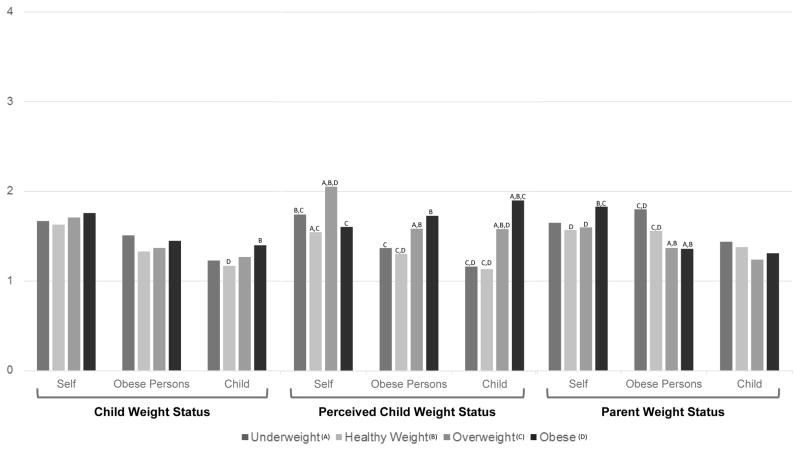
Fat Talk
ANOVAs evaluated whether child weight-status, perceived child weight-status, and parent weight-status were associated with parents’ fat talk (Figure 3). Child weight-status was associated with how parents talked about their child’s weight (F(3,983)=8.85, p<.001, ηp2=.027). Parents engaged in more child-fat talk with their children with obesity than those with healthy-weight. Child weight-status was not associated with parents’ self-fat talk (F(3,971)=3.03, p=.20, ηp2=.005), or fat talk about persons with obesity, F(3,971)=3.32, p=.09, ηp2=.007. Perceived child weight-status was associated with all forms of fat talk, Self: F(3,988)=20.14, p<.001, ηp2=.058; Persons with Obesity: F(3,988)=9.76, p<.001, ηp2=.029; Child: F(3,987)=46.03, p<.001, ηp2=.123. Perceived child overweight was associated with more frequent fat talk (Self, Persons with Obesity, and Child) compared with perceived child underweight and healthy-weight.
Figure 3.
Comparisons of parents’ fat talk. Note. Letters denote significant pairwise comparisons (using Tukey correction for multiple comparisons) at the p<.05 level compared with a=underweight, b=healthy-weight, c=overweight, or d=obese. Omitted letters indicate nonsignificant pairwise comparisons.
Parent weight-status was associated with how parents’ self-fat talk (F(3,988)=7.09, p<.001, ηp2=.021), and fat talk about persons with obesity (F(3,987)=7.34, p<.001, ηp2=.022). Parents with obesity engaged in self-fat talk than those with healthy-weight or overweight. Parents with overweight or obesity engaged in fat talk about persons with obesity less than those with underweight or healthy-weight. Parent weight-status was not associated with child-fat talk (F(3,987)=1.30, p=.27, ηp2=.004).
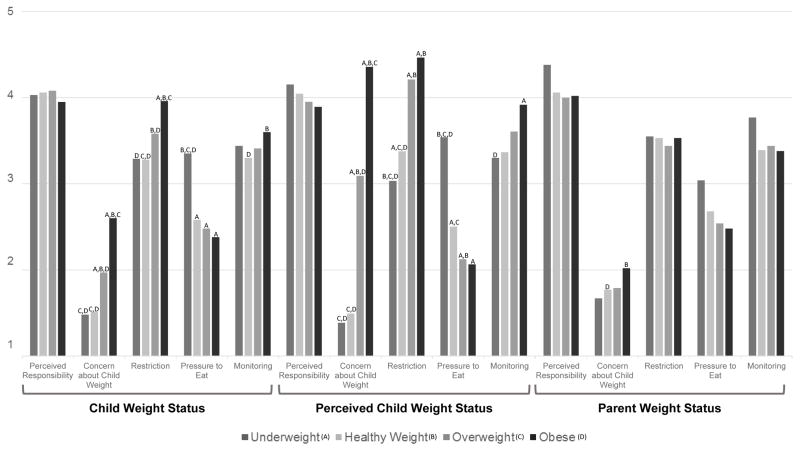
Parental Feeding Practices
ANOVAs evaluated associations among parental feeding practices and child weight, perceived child weight, and parent weight (Figure 4). Child weight-status was associated with Concern about Child Weight (F(3,982)=60.98, p<.001, ηp2=.157), Restriction (F(3,982)=15.34, p<.001, ηp2=.045), Pressure to Eat (F(3,982)=13.76, p<.001, ηp2=.040), and Monitoring (F(3,980)=3.99, p=.01, ηp2=.012). Parents were more concerned and practiced more restriction of their child with overweight and obesity than healthy-weight or underweight. Parents reported greater pressure to eat for underweight children than those with healthy-weight, overweight, or obesity. Parents monitored the eating of children with obesity eating more than that of healthy-weight children. Child weight-status was not associated with perceived responsibility for their child’s eating (F(3,980)=1.04, p=.37, ηp2=.003).
Figure 4.
Comparisons of parental feeding practices. Note. Letters denote significant pairwise comparisons (using Tukey correction for multiple comparisons) at the p<.05 level compared with a=underweight, b=healthy-weight, c=overweight, or d=obese. Omitted letters indicate nonsignificant pairwise comparisons.
Perceived child weight-status was related to Concern about Child Weight (F(3,998)=254.38, p<.001, ηp2=.433), Restriction (F(3,998)=32.50, p<.001, ηp2=.089), Pressure to Eat (F(3,998)=58.12, p<.001, ηp2=.149), and Monitoring (F(3,996)=4.59, p=.003, ηp2=.014). Perceived child overweight and obesity were associated with greater concern compared with perceived healthy-weight and underweight, and parents restricted the eating of children with perceived overweight and obesity more than perceived underweight and healthy-weight children. Parents monitored the eating of children with obesity more than that of underweight children, and pressured underweight children to eat more than those with healthy-weight, overweight, and obesity. Perceived child weight-status was not associated with Perceived Responsibility (F(3,996)=1.81, p=.14, ηp2=.005).
Parent weight-status was related to Concern about Child Weight (F(3,998)=3.64, p=.01, ηp2=.011) and Pressure to Eat (F(3,998)=3.61, p=.01, ηp2=.011). Parents with obesity were more concerned about their child’s weight than parents with healthy-weight. Parent weight-status was not associated with Perceived Responsibility (F(3,996)=1.83, p=.14, ηp2=.005), Restriction (F(3,998)=0.33, p=.81, ηp2=.001), and Monitoring (F(3,996)=1.12, p=.34, ηp2=.003).
Discussion
This study contributes three sets of findings to the literature on parental perception of child weight. First, we replicated findings that showed parent underestimation of child weight, and extended this work by showing that parents’ misperceptions of child overweight/obesity were significantly more frequent than their self-misperceptions of overweight/obesity. Second, parents’ personal eating attitudes/behaviors (restriction, overvaluation of weight/shape, body dissatisfaction, and self-fat talk) were related to their own weight-status and perceived child weight-status but not actual child weight-status. Third, parenting eating attitudes/behaviors (child dietary restriction, overvaluation by child weight/shape, dissatisfaction with child weight/shape, child fat talk, pressure to eat, monitoring) were related to actual and perceived child weight-status, but not parent weight-status.
Findings that parents were more accurate perceiving their own overweight/obesity than their child’s are important because they suggest that child weight perception is a distinct task rather than the same task transposed from one person (the parent) to another (the child). Furthermore, the difference in correlates with child weight underestimation (higher parent BMI, younger child age, male child gender) from correlates with self-underestimation (Black race, male parent gender), as well as non-significant correlates, suggest that specific factors have variable salience. Perceived child overweight/obesity might be tied to perceived stigma. That is, parents could see weight as less stigmatizing for younger children (who may still carry “baby fat”), for boys (for whom larger can be seen as healthier), and when the parent him/herself has excess weight. The exploratory findings that parents were more likely to underestimate children’s weight-status than adolescents’ weight-status also speak to this potential explanation because adolescence is seen as the time of transition from childhood to adulthood, including the time of establishing enduring healthy habits and health. Not perceiving a weight problem could, in turn, be related to misperceiving weight-status and research needs to evaluate weight perceptions with stigma.
Our findings also enhance understanding of the role of parents’ eating attitudes/behaviors with weight perceptions. One study found that parents’ personal weight/shape concerns were not related to child weight perceptions or concerns.18 Our findings extend this work by showing a relation of parents’ personal eating attitudes/behaviors with parent weight-status (medium to large effect size) and with perceived child weight (small effect size), and differentiating these from parenting eating attitudes/behaviors that were associated with child weight-status (medium to large effect size) and perceived child weight (large effect size). This could indicate a heightened sensitivity to weight that was also reflected in personal eating attitudes/behaviors. Further evidence of this potential explanation is parents’ fat talk by their own weight-status (parents with obesity did more self-fat talk than overweight and healthy-weight parents) and by perceived child weight-status (parents who perceived child overweight engaged in the most self-fat talk). Weight may have increased salience for parents who perceive child overweight, and they may attempt to use self-fat talk to create empathy or to model self-awareness. With this finding, it is important to note that the fat talk measured by the FTQ is strongly negative, using words such as “criticize,” “hate” and “disgusting.” Youth-focused findings that weight comments can be associated with impairment28 indicate further research should evaluate the effects of parental fat talk, and if needed, develop prevention and treatment programs to replace this form of parenting. Interestingly, patterns of fat talk and perceived weight-status were not paralleled with actual child weight-status. This departure is striking in the context of group differences in parental feeding practices, which were largely similar by actual and perceived child weight.
The last set of results showed parental feeding practices were related to actual and perceived child weight-status, but not parent weight-status. The exception to this pattern was perceived responsibility: responsibility was the same across child weight-status, perceived child weight-status, and parent weight-status. This is consistent with the theoretical frame for feeding proposed by Satter, which divides the responsibility for providing food and meal structure (parent) from the responsibility for eating the provided food (child).29 Of the other, significant parenting practices, restriction is thought to be related to weight gain through associations with poor self-regulation skills and eating in the absence of hunger, but monitoring children’s food and eating is thought to be associated with healthy-weight development.30 In the current study, there were clear group differences such that parents with children with heavier actual and perceived weight-status practiced the most restriction (medium effect size). However, the same pattern was not clear for monitoring: parents were more likely to monitor children with (and perceived to have) obesity eating than healthy-weight (and perceived underweight) children’s eating (small effect size), but other group differences were non-significant. As with earlier work13 this pattern suggests that actual and perceived child weight might be associated encouraging short-term dieting, but not behaviors promoting sustained weight loss.
A primary strength of this study is its inclusion of actual and perceived weight-status across the spectrum of parent and child BMI in a large community sample. Additionally, this study extends earlier work by examining parent and child correlates of perceived weight-status. Limitations include the cross-sectional design, which precludes comments about causality. Future research with longitudinal and experimental designs should assess directionality to inform prevention and treatment efforts. Our sample was also limited in racial/ethnic diversity, and findings that Black and Asian race/ethnicity were associated with greater underestimation and overestimation indicate that further research on cultural influences on weight perception is warranted. Another limitation to the current study is that all data, including weight and height, were reported by parents, which means that significant correlations may be biased by shared method variance. Additionally, sources of potential bias, including influence of co-parents, siblings, peers, and community, are not known, but could influence parents’ perceptions of whether they and their child were underweight, healthy weight, or overweight. Further research would benefit from evaluating youth using multiple reporters and assessing sources of influence on reporters’ weight perceptions. Future research could also evaluate children’s perceptions of parent weight status, as this is potentially a source of information body size that could influence youth’s body dissatisfaction and weight-control behaviors. Regarding height and weight specifically, reported and measured anthropometric data are consistently highly correlated, but have higher reported height and lower reported weight compared with measured values.31 Importantly, in a clinical eating-disorder sample, these discrepancies were not associated with race, eating attitudes/behaviors, or depressive symptoms, although heavier individuals underreported BMI to a greater extent.32 Additionally, a comparison of youth’s weight self-perceptions with their measured and reported weight-status showed similar misperception with measured and reported data, although greater underestimation occurred with measured than reported BMI.33 By extension, we could expect measured weight-status to produce greater underestimation in our study; however, comparisons of measured and parent-reported BMI should be evaluated.
Findings suggest potential implications for pediatric obesity prevention and treatment. There is a dual need to improve parent accuracy in child overweight/obesity perceptions, and to refine parent responses to perceived overweight/obesity. Associations of concern about child weight with actual and perceived child overweight/obesity suggest that accurate perception might be part of the instigation for seeking treatment, although this is likely more complex. Additionally, the association of higher concern for child weight for parents with obesity compared with healthy-weight potentially speaks to parents’ awareness of their influence (biologically or through the home environment) on their child’s weight. Given the high prevalence and serious consequences of child overweight/obesity into adulthood, further research should enhance understanding of parents’ specific needs to improve universal prevention programs, targeted prevention programs, and treatment programs.
What’s Known on This Subject
Many parents underestimate their child’s weight-status.
Underestimation might be related to specific parent and child demographic characteristics (e.g., male child gender), although findings vary.
Attitudinal and behavioral correlates of parents’ perception of child weight are under-explored.
What This Study Adds
Parents more frequently misperceive children’s overweight/obesity than their own overweight/obesity.
Parents’ personal eating attitudes/behaviors were related to their own weight-status and perceived child weight-status but not actual child weight-status.
Parents’ child-focused eating attitudes/behaviors were related to actual and perceived child weight-status, but not parent weight-status.
Acknowledgments
Funding Source: This research was supported, in part, by National Institutes of Health grant K24 DK070052 (Dr. Grilo).
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014 Feb 26;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epstein LH, Wing RR, Koeske R, Andrasik F, Ossip DJ. Child and parent weight loss in family-based behavioral modification programs. J Consult Clin Psychol. 1981;49:674–685. doi: 10.1037//0022-006x.49.5.674. [DOI] [PubMed] [Google Scholar]
- 3.Pesch MH, Harrell KJ, Kaciroti N, Rosenblum KL, Lumeng JC. Maternal styles of talking about child feeding across sociodemographic groups. J Am Diet Assoc. 2011;111:1861–1867. doi: 10.1016/j.jada.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. The relationship between parent and child self-reported adherence and weight loss. Obes Res. 2005;13:1089–1096. doi: 10.1038/oby.2005.127. [DOI] [PubMed] [Google Scholar]
- 5.Golan M. Parents as agents of change in childhood obesity--from research to practice. Int J Pediatr Obes. 2006;1:66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- 6.Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: A review. Int J Pediatr Obes. 2011;6:e12–27. doi: 10.3109/17477166.2011.566339. [DOI] [PubMed] [Google Scholar]
- 7.Rhee KE, DeLago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116:e94–e101. doi: 10.1542/peds.2004-2479. [DOI] [PubMed] [Google Scholar]
- 8.Taveras EM, Hohman KH, Price SN, et al. Correlates of participation in a pediatric primary care-based obesity prevention intervention. Obesity. 2011;19:449–452. doi: 10.1038/oby.2010.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obes Res. 2004;12:1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- 10.Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: maternal and child characteristics. Appetite. 2001;37:231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- 11.Doolen J, Alpert PT, Miller SK. Parental disconnect between perceived and actual weight status of children: A metasynthesis of the current research. J Am Acad Nurse Pract. 2009;21:160–166. doi: 10.1111/j.1745-7599.2008.00382.x. [DOI] [PubMed] [Google Scholar]
- 12.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003 May;111:1226–1231. [PubMed] [Google Scholar]
- 13.Neumark-Sztainer D, Wall M, Story M, van den Berg P. Accurate parental classification of overweight adolescents’ weight status: Does it matter? Pediatrics. 2008;121:e1495–1502. doi: 10.1542/peds.2007-2642. [DOI] [PubMed] [Google Scholar]
- 14.Boutelle K, Fulkerson JA, Neumark-Sztainer D, Story M. Mothers’ perceptions of their adolescents’ weight status: Are they accurate? Obes Res. 2004;12:1754–1757. doi: 10.1038/oby.2004.217. [DOI] [PubMed] [Google Scholar]
- 15.Fisher L, Fraser J, Alexander C. Caregivers’ inability to identify childhood adiposity: A cross-sectional survey of rural children and their caregivers’ attitudes. Aust J Rural Health. 2006;14:56–61. doi: 10.1111/j.1440-1584.2006.00764.x. [DOI] [PubMed] [Google Scholar]
- 16.Mathieu ME, Drapeau V, Tremblay A. Parental misperception of their child’s body weight status impedes the assessment of the child’s lifestyle behaviors. Int J Pediatr. 2010 doi: 10.1155/2010/306703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chaimovitz R, Issenman R, Moffat T, Persad R. Body perception: Do parents, their children, and their children’s physicians perceive body image differently? J Pediatr Gastroenterol Nutr. 2008;47:76–80. doi: 10.1097/MPG.0b013e31815a34. [DOI] [PubMed] [Google Scholar]
- 18.Lampard AM, Byrne SM, Zubrick SR, Davis EA. Parents’ concern about their children’s weight. Int J Pediatr Obes. 2008;3:84–92. doi: 10.1080/17477160701832552. [DOI] [PubMed] [Google Scholar]
- 19.Chen HY, Lemon SC, Pagoto SL, Barton BA, Lapane KL, Goldberg RJ. Personal and parental weight misperception and self-reported attempted weight loss in US children and adolescents, National Health and Nutrition Examination Survey, 2007–2008 and 2009–2010. Prev Chronic Dis. 2014;11:E132. doi: 10.5888/pcd11.140123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001 May;107:1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 21.Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: Do parents recognize this health risk? Obes Res. 2003;11:1362–1368. doi: 10.1038/oby.2003.184. [DOI] [PubMed] [Google Scholar]
- 22.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001 Jun;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 23.Anderson CB, Hughes SO, Fisher JO, Nicklas TA. Cross-cultural equivalence of feeding beliefs and practices: The psychometric properties of the child feeding questionnaire among Blacks and Hispanics. Prev Med. 2005;41:521–531. doi: 10.1016/j.ypmed.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- 25.Grilo CM, Reas DL, Hopwood CJ, Crosby RD. Factor structure and construct validity of the eating disorder examination-questionnaire in college students: Further support for a modified brief version. Int J Eat Disord. 2015 Apr;48:284–289. doi: 10.1002/eat.22358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grilo CM, Crosby RD, Peterson CB, et al. Factor structure of the eating disorder examination interview in patients with binge-eating disorder. Obesity. 2010;18:977–981. doi: 10.1038/oby.2009.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Royal S, MacDonald DE, Dionne MM. Development and validation of the Fat Talk Questionnaire. Body Image. 2013;10:62–69. doi: 10.1016/j.bodyim.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Lo WS, Ho SY, Mak KK, Wong YM, Lai YK, Lam TH. Prospective effects of weight perception and weight comments on psychological health among Chinese adolescents. Acta Paediatr. 2009;98:1959–1964. doi: 10.1111/j.1651-2227.2009.01472.x. [DOI] [PubMed] [Google Scholar]
- 29.Satter EM. Internal regulation and the evolution of normal growth as the basis for prevention of obesity in children. J Am Diet Assoc. 1996;96:860–864. doi: 10.1016/s0002-8223(96)00237-4. [DOI] [PubMed] [Google Scholar]
- 30.Birch LL. Child feeding practices and the etiology of obesity. Obesity. 2006;14:343–344. doi: 10.1038/oby.2006.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 32.White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: Misreport is not related to psychological factors. Obesity. 2010;18:1266–1269. doi: 10.1038/oby.2009.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dalton WT, III, Wang L, Southerland JL, Schetzina KE, Slawson DL. Self-reported versus actual weight and height data contribute to different weight misperception classifications. South Med J. 2014;107:348–355. doi: 10.14423/01.SMJ.0000450708.52011.7c. [DOI] [PMC free article] [PubMed] [Google Scholar]