Abstract
Giant polyps in the esophagus are rarely occurring benign tumors and may contain lipomas, fibrovascular polyps, fibrolipomas or neurofibromas polyps. Clinical symptoms include dysphagia, vomiting, retrosternal pain, shortness of breath, and asthma. In some cases, the polyps are regurgitated into the oral cavity and represent a spectacular manifestation. The reported case in this study was of a 50‐year‐old man who complained of emesia for half a year and dysphagia for one month before being hospitalized. Occasionally, a fleshly mass reached into his mouth. The results of endoscopic ultrasonography, barium swallow in the upper digestive tract, and a computed tomography scan demonstrated a giant polyp in the esophagus, which was subsequently removed by gastroscopy. Pathological examination determined a fibrovascular polyp.
Keywords: Dysphagia, esophageal polyp, esophagus, gastroscopy, giant fibrovascular polyp
Introduction
Giant esophageal polyps are rarely occurring benign tumors and represent about 0.03% of all neoplasms in the esophagus.1 Most esophageal polyps arise from the cervical or upper esophagus.2 No symptoms are initially perceived, but with the growth of the neoplasm, symptoms such as dysphagia, vomiting, retrosternal pain, shortness of breath, and/or asthma may occur. A fresh mass may also be regurgitated into the mouth.3 Current treatment for this complication includes resection through a cervical incision, thoracotomy or treatment by endoscopy.4 Endoscopy is preferred as it causes less damage than other surgical methods. In the present case, we report a patient with an esophageal polyp who suffered from dysphagia; the polyp was successfully removed by gastroscopy.
Case Report
A 50‐year‐old man was admitted to the General Hospital of the People's Liberation Army after complaining of a month of dysphagia, six months of vomiting, and infrequent regurgitation of a fresh mass into the oral cavity (Fig 1a). No treatment was provided until the dysphagia became worse. Barium swallow demonstrated a giant neoplasm which almost occupied the whole esophageal lumen, 22 cm apart from the incisor and 18 cm in length. The mucosal surface of the neoplasm was smooth, suggesting a giant submucosal neoplasm in the esophagus with a high probability of an esophageal polyp (Fig 1b). Chest computed tomography (CT) demonstrated a huge neoplasm, extending from the cervical esophagus to the cardia; the largest diameter of the polyp was 6 cm (Fig 1c). The lumen of esophagus was also distended. Ultrasonic endoscopy showed a neoplasm originating from the submucosa of the cervical esophagus, the base of which was about 5 cm in diameter, occupying almost half of the esophageal lumen (Fig 1d). These data indicated an esophageal polyp measuring 18 cm in length and 5–6 cm in diameter, extending from the cervical esophagus to the stomach cavity. After preparation, the patient was treated via gastroscopy under general anesthesia. Because of the large dimension of the polyp, it could not be completely removed; therefore, it was cut into small pieces by snare and removed piece by piece. The procedure lasted about three hours and approximately two‐thirds of the tumor was removed. Surgery was discontinued after heavy edema in the esophageal mucosa. After surgery, the patient was supported with nutritional therapy (oral food and water were not permitted), and orally treated with mannitol, dexamethasone, and gentamycin to reduce swelling and prevent infection. Gastroscopy was repeated a week later, resulting in the total removal of the tumor. The patient left the hospital and no abnormality was found by gastroscopy one month later (Fig 2). Pathological examination confirmed that a fibrovascular polyp was successfully removed. The patient was followed up for more than two years and no recurrence was observed.
Figure 1.
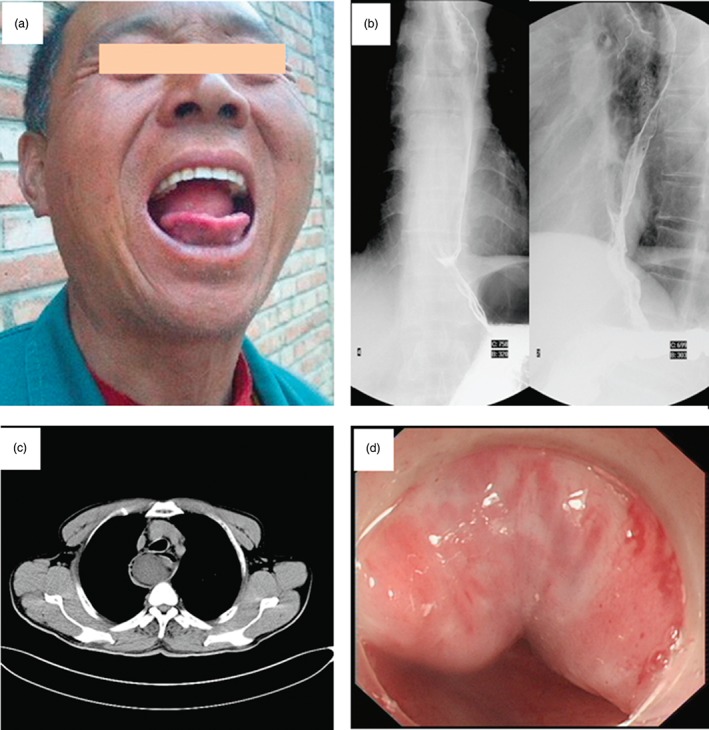
The diagnosis of esophageal polyb. (a) A giant neoplasm regurgitated into the mouth. (b) A polyp with a long pedicle detected by barium esophagogram. (c) A neoplasm almost occupying the whole lumen detected by computed tomography (CT). (d) The neoplasm detected by gastroscopy.
Figure 2.
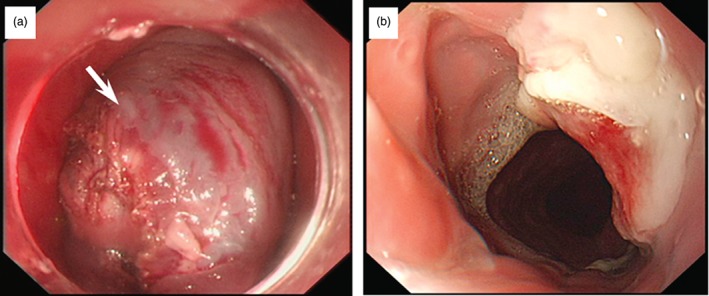
The removal of esophageal polyp by gastroscopy. (a) The giant neoplasm in the esophageal lumen. (b) The esophagus after surgery.
Discussion
Esophageal polyps are a kind of rare benign tumor of the esophagus, consisting of material such as fibrous tissue, blood vessels, and adipose tissue, with a morbidity rate lower than that of esophageal laevicellulare.5 Esophageal polyps are commonly located at the upper third of the esophagus, originating from mucosa or submucosa. Neoplasms in the esophageal lumen can result in nutrition problems, such as anemia and cachexia. Furthermore, emergencies, such as asphyxia, may occur when the polyp enters into the airway. Esophageal polyps should be removed surgically as soon as possible after confirmation to reduce such risks.
The detection of an esophageal polyp relies on barium esophagogram, gastroscopy, and chest CT. Barium study is commonly used, but its sensitivity is relatively low for polyps with normal surfaces. In addition, it cannot show the pedicle of the neoformation. Detection of a polyp by gastroscopy may be difficult because of the occupation of the esophageal lumen by the polyp. Ultrasonic endoscopy might help find the origin and range of the neoplasm pedicle. Chest CT and magnetic resonance imaging could help determine the volume and range of large polyps, in order to determine the proper surgical approach. Although many detection methods can be used, an esophageal polyp is always misdiagnosed because of its rarity. The patient in this study had consulted several hospitals and been diagnosed with an esophageal sarcoma or leiomyosarcoma before being hospitalized in our institution.
Therapies for esophageal polyps generally include surgical intervention or removal by endoscopy, mainly determined by the lesion size and vessels that nourish the polyp. Surgical intervention can remove low risk esophageal polyps; however, neoplasm resection by endoscopy cannot be performed as an endoscopy cannot support severe bleeding.6 As reviewed in Table 1, esophageal polyps have been successfully removed by surgery; however, numerous reports have shown that bleeding complications of polyp removal by endoscopy could be avoided by comprehensive evaluation before surgery and careful surgical technique.12, 13 The giant neoplasm in this case was successfully removed by endoscopy after accurate definition of the cervical origin of the neoplasm and the realm of its pedicle by careful examination under ultrasonic gastroscopy. Preparations were made in case of bleeding during endoscopical therapy. Because of the close localization of the esophagus and air tube, surgery was very carefully performed to avoid breaking the wall of esophagus.
Table 1.
Recent reports of esophageal polyps and their removal
| Polyp size | Location of polyp | Detection method | Surgical approach | Ref |
|---|---|---|---|---|
| 23 cm × 9 cm × 9 cm | Upper esophageal sphincter | Chagas serology, esophageal manometry, endoscopy, and chest CT | Esophagectomy | 7 |
| 18 cm × 5.4 cm × 4 cm | Hypopharynx below the left arytenoid cartilage | Gastroscopy, CT, EUS | Cervicotomy and pharyotomy | 5 |
| 23 cm × 3 cm x 3 cm | Posterior aspect of esophagus, below the cricopharyngeus | Barium swallow study, esophagoscopy | Larygopharyngoscopy | 8 |
| 10.5 cm × 5.5 cm × 3.5 cm | Barium esophagogram, MRI | Right anterior mucosal wall of the cervical esophagus | Esophagotomy | 9 |
| 16 cm × 7 cm x 7 cm | Chest CT, endoscopy | Below the Killian's area, in a small hiatus hernia | Esophagotomy | 10 |
| 4 cm × 4 cm; 6 cm × 6 cm | Esophago‐gastro‐duodenoscopy | Upper third of esophagus | Esophagotomy | 3 |
| 20 cm × 3–4 cm | Upper gastrointestinal endoscopy, CT, barium esophagogram | Cervical esophagus | Esophagotomy and laparoscopic gastrotomy | 11 |
CT, computed tomography; EUS, endoscopic ultrasound.
In conclusion, an esophageal polyp is a kind of benign neoplasm that rarely occurs in the esophagus. An esophageal polyp should be removed immediately by surgery or endoscopy, preferably via endoscopy as the technique causes less damage to the patient.
Disclosure
No authors report any conflict of interest.
References
- 1. Kau RL, Patel AB, Hinni ML. Giant fibrolipoma of the esophagus. Case Rep Otolaryngol 2012; 2012: 406167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goenka AH, Sharma S, Ramachandran V, Chattopadhyay TK, Ray R. Giant fibrovascular polyp of the esophagus: Report of a case. Surg Today 2011; 41: 120–124. [DOI] [PubMed] [Google Scholar]
- 3. Lee SY, Chan WH, Sivanandan R, Lim DT, Wong WK. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol 2009; 15: 3697–3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Caceres M, Steeb G, Wilks SM, Garrett HE Jr. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg 2006; 81: 393–396. [DOI] [PubMed] [Google Scholar]
- 5. Pallabazzer G, Santi S, Biagio S, D'Imporzano S. Difficult polypectomy‐giant hypopharyngeal polyp: Case report and literature review. World J Gastroenterol 2013; 19: 5936–5939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vagli P, Solito B, Neri E et al Giant fibrovascular polyp of the esophagus‐imaging techniques for proper treatment planning: Report of two cases. Abdom Imaging 2012; 37: 512–518. [DOI] [PubMed] [Google Scholar]
- 7. Madeira FP, Justo JWR, Wietzycoski CR, Burttet LM, Kruel CDP, da Rosa AP. Giant fibrovacular polyp of the esophagus: A diagnostic challenge. Arq Bras Cir Dig 2013; 26: 71–73. [DOI] [PubMed] [Google Scholar]
- 8. Kau RL, Patel AB, Hinni ML. Giant fibrolipoma of the esophagus. Case Rep Otolaryngol 2012; 2012: 406167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yannopoulos P, Manes K. Giant fibrovascular polyp of the esophagus‐imaging techniques can localize, preoperatively, the origin of the stalk and designate the way of surgical approach: A case report. Cases J 2009; 2: 6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. García‐Pérez B, arcía‐Paredes R, Ono‐Ono A, iras‐López M, ons‐Miñano JA, Carballo LF. Giant fibrovascular esophageal tumor. Endoscopic vision. Rev Esp Enferm Dig 2012; 104: 104–106. [DOI] [PubMed] [Google Scholar]
- 11. Jose P, Scott N, Sarela AI. Two‐stage removal of giant fibrovascular polyp of the oesophagus. BMJ Case Rep 2010; pii: bcr0520103011; doi: 10.1136/bcr.05.2010.3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Park JS, Bang BW, Shin JY et al A case of esophageal fibrovascular polyp that induced asphyxia during sleep. Clin Endosc 2014; 47: 101–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ozdemir S, Gorgulu O, Selcuk T, Akbas Y, Sayar C, Sayar H. Giant fibrovascular polyp of the hypopharynx: Per‐oral endoscopic removal. J Laryngol Otol 2011; 125: 1087–1090. [DOI] [PubMed] [Google Scholar]


