Abstract
Liposarcoma arising in the mediastinum is extremely rare. Herein we present a case of a 47‐year‐old man with a huge posterior mediastinal tumor that extended to the bilateral thorax. The patient underwent a complete resection of the tumor and experienced an uneventful recovery. Postoperative pathology finally revealed liposarcoma. The patient underwent follow‐up for 25 months, during which time no recurrence was found.
Keywords: Liposarcoma, mediastinum, radiotherapy, surgery
Introduction
Liposarcoma is the most common soft tissue sarcoma and usually occurs in the limbs and retroperitoneum, accounting for approximately 20% of all mesenchymal malignancies.1 Liposarcomas arising in the mediastinum are very rare and asymptomatic in early stage. As the liposarcoma continues to grow, symptoms related to direct invasion or compression of other thoracic organs may present, such as cough, dysphagia, and shortness of breath. Surgical resection is the optimal treatment for mediastinal liposarcoma.2 We report a case of giant primary mediastinal liposarcoma in a 47‐year‐old man. The patient underwent a complete tumor resection and experienced an uneventful recovery. No evidence of recurrence or distant metastasis was discovered during 25 months of follow‐up after surgery.
Case report
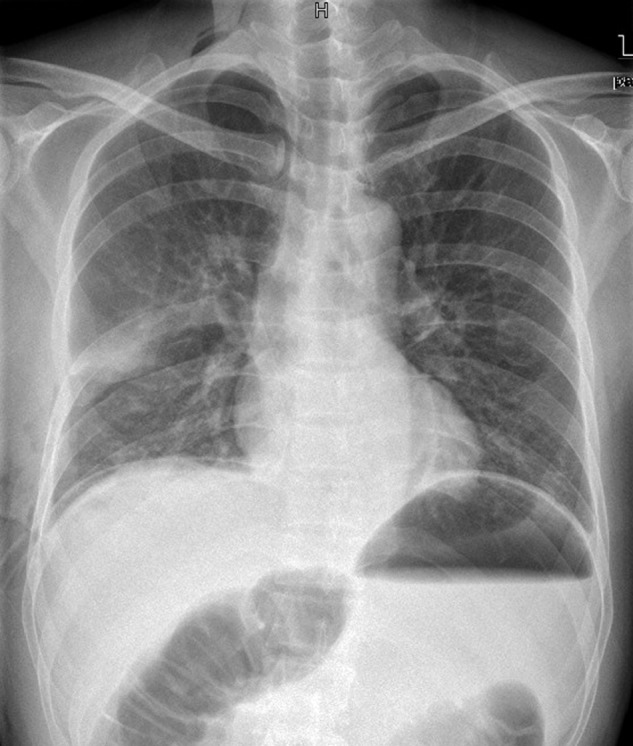
A 47‐year‐old man presented with a two‐month history of constant cough, chest distress, and slight dysphagia. Physical examination revealed that breathing sounds were markedly decreased throughout the right thorax and the sound of the heart had moved to the left side. Chest radiography showed a high‐density shadow in the lower two‐thirds of the right thorax (Fig 1a). Enhanced computed tomography (CT) of the chest confirmed a huge mass with fat tissue density in the posterior mediastinum, which extended to the bilateral thorax and compressed the heart, aorta, and bilateral lung (Fig 1b). Upper gastrointestinal contrast showed an obvious dislocated esophagus, resulting from compression of the mass. Bronchoscopy revealed that the right middle and lower lobe bronchi were distorted, and the lumen had become severely narrowed. Cranial and abdominal CT scans and a bone scan excluded the potential metastasis of the tumor. Blood biochemistry and serum cancer markers were all normal.
Figure 1.

(a) Chest radiography showed a high‐density shadow in the lower two‐thirds of the right thorax. (b) Enhanced computed tomography of the chest confirmed a huge tumor with fat tissue density in the posterior mediastinum. The tumor extended to the bilateral thorax and compressed the heart, aorta, and bilateral lung.
The patient declined percutaneous needle biopsy; therefore, surgical intervention was applied for diagnosis and treatment. The patient underwent the placement of a stomach tube before surgery. Anesthesia was induced while the patient was in the horizontal position. Using positive‐pressure separate lung ventilation to avoid compression of the heart and lungs by the large tumor, the patient was moved to the left lateral position. Vital signs, including arterial blood pressure, central venous pressure, and heart rate, were monitored carefully. After confirmation of stable anesthesia, right posterolateral thoracotomy was performed in the fifth intercostal space. The sixth rib was resected in order to better expose the huge mass. Intraoperatively, a giant, well‐capsulated yellow tumor without abundant blood supply was found, which almost occupied the whole right thorax. The tumor had not invaded any other organs, such as the lung, chest wall, or pericardium; only moderate adhesion existed in the thorax. The partial tumor in the right thorax was smoothly removed in two blocks after cutting off the adhesion. The esophagus, phrenic nerve, and inferior vena cava (IVC) were carefully protected during surgery. The esophagus and IVC were then mobilized from the tumor. The tumor of the left thorax was drawn upward through the space between the esophagus and IVC, and the rest of the tumor was gradually separated and successfully removed. The atelectatic right middle and lower lobes obtained good pneumatization when both lungs were ventilated.
The gross size of the tumor was 30 cm × 25 cm × 20 cm and it was covered with a capsule (Fig 2). The cut surface appeared lobulated in shape and was pale yellow in color. Pathology showed that the tumor comprised abundant atypical adipocytes with dispersed smooth muscle proliferation (Fig 3). The final pathological diagnosis was well‐differentiated liposarcoma. The patient experienced an uneventful recovery. Postoperative chest radiography showed a normal right lung (Fig 4). No sign of recurrence or distant metastasis was detected during 25 months of follow‐up after surgery.
Figure 2.

The gross size of the tumor was 30 cm × 25 cm × 20 cm and it was covered with a capsule.
Figure 3.

Pathology showed that the tumor was comprised of abundant atypical adipocytes with dispersed smooth muscle proliferation presented as fascicles and clusters dispersed throughout the adipose tissue component (hematoxylin and eosin stain 200×).
Figure 4.
Postoperative chest radiography showed a normal right lung.
Discussion
Liposarcoma is a common mesenchymal malignancy that mostly occurs in the lower limbs and retroperitoneum in adults.3 Primary liposarcoma arising from the mediastinum is extremely rare, and accounts for less than 1% of all mediastinal tumors.4 Five main pathological types of liposarcomas have been previously described, including well‐differentiated, dedifferentiated, myxoid, pleomorphic, and round cell liposarcomas.5 The well‐differentiated type has less potential for local recurrence and distant metastasis.6
The mediastinal liposarcomas reported previously were more often found in the anterior mediastinum, adherent to the pericardium, and tended to involve the diaphragm. In this case, the tumor was located atypically in the posterior mediastinum with extension to the bilateral thorax. The patient presented symptoms of cough, chest distress, and slight dysphagia, which corresponded to the expression of the tumor.
In chest radiography, mediastinal liposarcoma usually presents as a widened mediastinum or a high‐density shadow of the chest. A CT scan can distinguish a tumor with fat density from other mediastinal tumors, such as teratomas, fibromas, and cysts. Needle biopsy is helpful for preoperative diagnosis and choice of treatment. In this case, however, the patient refused needle biopsy and insisted on surgical treatment.
Extensive surgical resection is the optimal treatment for mediastinal liposarcoma because of the malignant nature of the tumor. Based on our experience, complete resection of well‐capsulated liposarcoma was feasible because the tumor was non‐invasive and had no rich blood supply. However, the management of huge a mediastinal tumor is always challenging. An optimal operative field is crucial for safety. In this case, the methods, including expanded incision and piecemeal resection, ensured a clear operative field. The placement of a stomach tube as an intraoperative position mark was helpful for the safe resection of the massive tumor in the posterior mediastinum. In special conditions, cardiopulmonary bypass should be prepared in order to complete the expanded excision of the tumor.
Radiotherapy was once thought to be effective as postoperative adjuvant treatment for diffusely infiltrating nonencapsulated mediastinal liposarcomas; however, tissue adhesion caused by radiation therapy generally hindered the second surgical procedure when local recurrence occurred postoperatively.7 Moreover, in some studies, postoperative radiation therapy did not display obvious benefits in reducing recurrence.8 Thus, our patient did not receive further adjuvant radiotherapy based on the nature of the tumor and the complete resection.
In conclusion, we successfully performed the radical resection of a huge mediastinum liposarcoma that extended to the bilateral thorax. Long‐term follow‐up is still necessary in order to discover any potential relapse in time.
Disclosure
No authors report any conflict of interest.
References
- 1. Dei Tos AP. Liposarcoma: New entities and evolving concepts. Ann Diagn Pathol 2000; 4: 252–266. [DOI] [PubMed] [Google Scholar]
- 2. Pawlik TM, Ahuja N, Herman JM. The role of radiation in retroperitoneal sarcomas: A surgical perspective. Curr Opin Oncol 2007; 19: 359–366. [DOI] [PubMed] [Google Scholar]
- 3. Grobmyer SR, Luther N, Antonescu CR, Singer S, Brennan MF. Multiple primary soft tissue sarcomas. Cancer 2004; 101: 2633–2635. [DOI] [PubMed] [Google Scholar]
- 4. Schweitzer DL, Aguam AS. Primary liposarcoma of the mediastinum. Report of a case and review of the literature. J Thorac Cardiovasc Surg 1977; 74: 83–97. [PubMed] [Google Scholar]
- 5. Bolen JW, Thorning D. Liposarcomas: A histogenetic approach to the classification of adipose tissue neoplasms. Am J Surg Pathol 1984; 8: 3–17. [PubMed] [Google Scholar]
- 6. Sato T, Nishimura G, Nonomura A, Miwa K. Intra‐abdominal and retroperitoneal liposarcomas. Int Surg 1999; 84: 163–167. [PubMed] [Google Scholar]
- 7. Ohta Y, Murata T, Tamura M, Sato H, Kurumaya H, Katayanagi K. Surgical resection of recurrent bilateral mediastinal liposarcoma through the clamshell approach. Ann Thorac Surg 2004; 77: 1837–1839. [DOI] [PubMed] [Google Scholar]
- 8. Hirai S, Hamanaka Y, Mitsui N, Uegami S, Matsuura Y. Surgical resection of primary liposarcoma of the anterior mediastinum. Ann Thorac Cardiovasc Surg 2008; 14: 38–41. [PubMed] [Google Scholar]


