Abstract
Introduction
Management of urolithiasis in a solitary functioning kidney can be clinically challenging. The aim of this article was to review the outcomes of URS for patients with stone disease in a solitary kidney and critically appraise the existing evidence and outcome reporting standards.
Material and methods
We conducted a systematic review in line with PRISMA checklist and Cochrane guidelines between January 1980 and February 2015. Our inclusion criteria were all English language articles reporting on a minimum of 10 patients with a solitary kidney undergoing ureteroscopy for stone disease.
Results
A total of 116 patients (mean age 50 years) underwent URS for stones in solitary kidney. For a mean stone size of 16.8 mm (range: 5–60 mm) and 1.23 procedures/patient, the mean stone free rate was 87%. No significant change in renal function was recorded in any of the studies although a transient elevation in creatinine was reported in 10 (8.6%) patients. A total of 33 (28%) complications were recorded a majority (n = 21) of which were Clavien grade I. The Clavien grade II/III complications as reported by authors were urosepsis, steinstrasse and renal colic. None of the procedures required conversion to open surgery with no cases of renal haematoma or ureteric perforation.
Conclusions
This contemporary review highlights URS as a viable treatment option for stone disease in patients with a solitary kidney. It is associated with superior clearance rates to SWL and fewer high-risk complications compared to PCNL.
Keywords: solitary kidney, calculi, laser, stone, ureteroscopy
INTRODUCTION
The management of urolithiasis in a solitary functioning kidney poses a serious clinical challenge for the urologist. The objective when treating these complex non-indexed patients is to yield high stone free rates whilst achieving minimal ancillary procedures, renal function compromise and post-intervention morbidity. Long-term preservation of existing renal function is paramount, since the lack of a contra-lateral functioning kidney leads to the loss of a compensatory advantage. Resultant hypertrophy and dilatation of the remaining renal parenchyma present a higher risk of haemorrhage, implicating further difficulties as a result of the loss of existing renal function [1].
In recent years, the advent of new generation flexible ureteroscopes has pushed the barriers of renal stone management [2]. The latest paradigms have seen these ureteroscopes employed effectively for a number of complex scenarios, including larger sized stones, pregnancy and obesity [3]. Percutaneous Nephrolithotomy (PCNL) and Shockwave Lithotripsy (SWL) are the other treatment modalities for such cases. However, each is not without its pros and cons. The optimal treatment option must therefore be carefully considered, based on a number of factors unique to the patient. These should include renal function, age and body mass index, as well as cumulative stone diameter and location. Patient preference and surgeon experience also play a role in what should be a tailor-made decision.
The outcomes of ureteroscopy (URS) for stones in a solitary kidney are still largely under-reported. The aim of this article is, therefore, to review the outcomes of URS for patients with stone disease in a solitary kidney. This will be followed by a critical appraisal of the existing evidence and outcome reporting standards.
MATERIAL AND METHODS
Search strategy
A systematic search of the literature was performed including the electronic databases: Pubmed, Medline, Scopus, Biomed Central, CINAHL, Web of Science, and EMBASE. Reference lists were cross-checked for relevant peer reviewed studies published between January 1980 and February 2015. Individual urological journals and conference proceedings were also hand-searched. A highly sensitive strategy was devised and implemented in line with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist and the Cochrane Collaboration guidelines [4]. Search terms used included ‘ureteroscopy’, ‘stones’, ‘calculi’, ‘solitary’, ‘kidney’, ‘renal’, ‘laser’, ‘laser therapy’ and ‘urolithiasis’. Finally, Boolean operators (AND, OR) were employed to augment this methodical and comprehensive search. The list of studies generated by the search was screened to identify eligible studies. To meet the pre-defined inclusion criteria, studies had to report on at least 10 cases of patients with a solitary kidney undergoing URS for stone disease.
Data extraction
Two authors (P.J. and B.R.) extracted the data independently. Any discrepancies were resolved by consultation with the senior author (BS), by mutual agreement. It was the consensus of all authors that there was insufficient data to carry out a formal meta-analysis.
The outcomes of interest were initial stone free rate (SFR), final SFR, post-operative creatinine, operative time and procedure related complications, graded according to the Clavien-Dindo system. Data was also extracted on baseline characteristics, including information on age, BMI, stone location and composition.
Quality assessment of studies
Levels of evidence and recommendation of the included studies were evaluated using the criteria set by the Centre for Evidence Based Medicine (CEBM) [5]. The quality of reporting outcomes was performed according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [6]. The quality of procedure related complications reported was evaluated against the criteria set by the Martin's system [7] – a tool designed to aid accurate and comprehensive reporting of surgical complications.
RESULTS
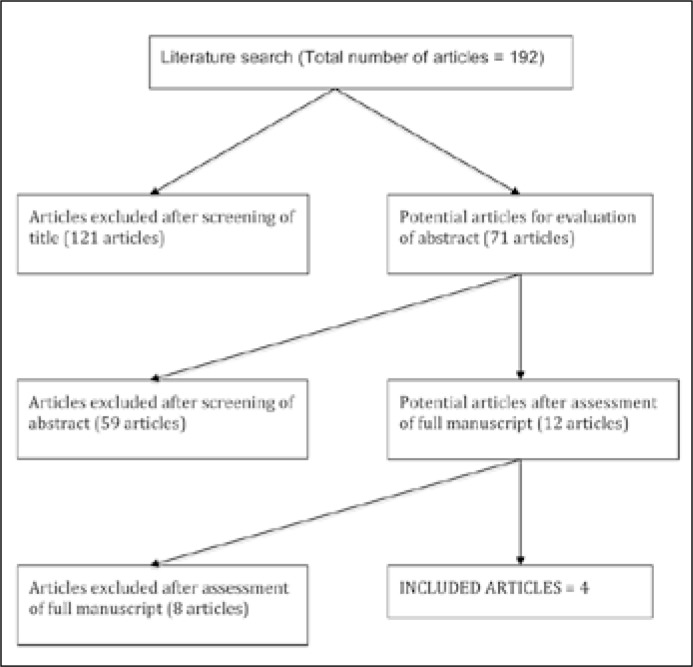
A total of 192 studies were screened. Only 4 studies met the inclusion criteria and were included in the review [8–11] (Figure 1). Three studies were case series and one was a cohort study (comparing URS with SWL), published between 2013 and 2014 (Tables 1 and 2).
Figure 1.
PRISMA flowchart of literature search.
Table 1.
Summary of study information and patient demographics (ND = not documented, *confirmed by dimercaptosuccinic acid renography)
| Author | Journal | Year | Country | Level of evidence | Number of patients | Male: Female | Mean age +/- 1 SD (years) | Mean BMI +/-1 SD (kg/m2) | Mean pre-operative creatinine +/- SD (mg/dL) | Aetiology of solitary kidney | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contra-lateral nephrectomy | Congenital agenesis | Non-functioning contra-lateral kidney * | ||||||||||
| Atis | Urology | 2013 | Turkey | 4 | 24 | 14:10 | 44.41 +/-2.15 | ND | 1.54 +/-0.55 | 9 | 5 | 10 |
| Yuruk | Journal of Endourology | 2014 | Turkey | 4 | 18 | 9:9 | 47.1 +/-13.8 | 25.5 +/-4.2 | 1.38 +/-0.4 | ND | ND | ND |
| Gao | Journal of Endourology | 2014 | China | 4 | 45 | 29:16 | 51.04 +/-1.67 | ND | 1.29 +/-0.61 | 13 | 7 | 25 |
| Giusti | World Journal of Urology | 2014 | Italy | 4 | 29 | 17:12 | 55.7 +/-12.3 | 25.1 +/-2.5 | 1.5 +/-0.6 | 14 | 6 | 9 |
Table 2.
Baseline values of stones (ND – no data)
| Study | Laterality, left/right | Mean stone size +/-1 SD (mm) | Stone location, n (%) | Stone composition, n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Renal Pelvis | Upper Pole | Middle Pole | Lower Pole | Multiple | Calcium Oxalate | Uric Acid | Struvite | Mixed | |||
| Atis et al. 2013 | ND | 19.83 +/-5.9 | 9 (25) | 6 (16.66) | 7 (19.44) | 14 (38.88) | ND | 18 (75) | 3 (12.5) | 3 (12.5) | 0 |
| Yuruk et al. 2014 | 9/9 | 16 +/-2.6 | 7 | 11 | ND | ND | ND | ND | ND | ||
| Gao et al. 2014 | 23/22 | 18.4 +/-1.9 | 13 (28.88) | 1 (2.22) | 1 (2.22) | 10 (22.22) | 20 (44.44) | ND | ND | ND | ND |
| Giusti et al. 2014 | ND | 13 +/-4.0 | 18 (62.1) | 2 (6.9) | 3 (10.3) | 6 (20.7) | ND | 15 (51.7) | 2 (6.9) | 4 (13.8) | 8 (27.6) |
Baseline characteristics
A total of 116 patients (69 males vs. 47 females) underwent ureteroscopy. All of the procedures were carried out under general anaesthesia. The mean age of this population was 49.6 years (range: 14–74). The mean BMI was reported in 2 studies and was 25.3 (range: 21–30) [9, 11]. Three studies provided details of the aetiology of the solitary kidney and a non-functioning kidney (confirmed by dimercaptosuccinic acid renography) was determined to be the cause in the greatest number of cases (44.9%) [8, 10, 11]. The mean stone size was 16.8 mm (range: 5–60 mm). The majority of documented stones (62.3%) were composed of calcium oxalate (Table 2). Only one study reported the number of patients who underwent pre-operative stenting [11]. All of the studies mentioned the routine use of post-operative stenting [8–11]. The mean follow up period was 14 months (range 3–72 months). However, only Giusti et al. recorded a follow up period, which exceeded 12 months [11]. Table 3 highlights the inclusion and exclusion criteria for each study.
Table 3.
Inclusion/Exclusion Criteria for studies (ND – no description)
| Study | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Atis et al. 2013 | Failed SWL Patient preference Surgeon preference |
ND |
| Yuruk et al. 2014 | Functional or anatomically single kidneys | ND |
| Gao et al. 2014 | Failed SWL Contradindication of PCNL Patient preference |
Severe hydronephrosis Large, staghorn stones |
| Giusti et al. 2014 | Age >18 years Renal stones up to 2 cm diameter |
Pregnancy Urinary tract abnormalities Positive urine culture |
Outcome measures
The mean number of procedures carried out was 1.23 (range: 1–4), the mean operating time was 64.9 minutes (range: 18–190 minutes) and for the 3 studies reporting the initial SFR, the mean value was 73.4% (range: 64.4–83.3%) [8, 10, 11]. Across all of the studies, the final (SFR) was 87.2% (Table 4). The mean pre-operative and post- operative creatinine was 1.43 mg/dL and 1.52 mg/dL respectively. No significant change in renal function was recorded in any of the studies.
Table 4.
Outcomes of the included studies (ND – not documented, AUR – acute urinary retention)
| Author | Mean operating time +/-1 SD (mins) | Mean number of procedures | Mean postoperative creatinine +/-SD (mg/dL) and time measured | Initial SFR% | Final SFR% | Definition of SFR |
Failures (n) | Complications (n) | No. of Martin criteria met |
|---|---|---|---|---|---|---|---|---|---|
| Atis | 55.83 +/-10.90 |
1.17 | 1.56 +/-0.50 (2 weeks) |
83.3 | 95.8 | Fragments <4 mm | Failed to reach stone on second stage URS (1) | Febrile UTI (4) | 6 |
| Yuruk | 52.05 +/-17.54 |
1.06 | 1.46 +/-0.51 (3 months) |
ND | 66.66 | ND | ND | Fever (1), haematuria (1), colicky pain (5) | 5 |
| Gao | 76.4 +/-40.14 |
1.44 | 1.34 +/-0.71 (Time measured not specified) |
64.44 | 93.33 | Fragments <2 mm | 60mm stone needed 4 URS sessions, PCNL contra indicated (1) | Transient elevation of creatinine (10), sepsis (2), AUR (2) | 6 |
| Giusti | 75.2 +/-12.00 |
1.24 | 1.7 +/-0.6 (1 month) |
72.4 | 93.1 | Fragments <2 mm | Residual stones <5 mm but asymptomatic (2) | Fever (4), AUR (1), haematuria (2), Steinstrasse causing anuria and acute renal inury | 6 |
ND = No Data
Subgroup analysis revealed URS for a smaller stone size achieved better results. Atis et al. reported that for stones <20 mm, the final clearance rate was 100% but in the >20 mm group it was 92.3%. Gao et al. reported the stone free rate was 93.33% in the sub group with stones <20 mm and 85.71% in the >20 mm group.
Complications
All of the studies used the Clavien-Dindo grading system for complications. A total of 33 complications were recorded (28.4% of all patients). The majority (n = 21) of the complications were Clavien grade I (Table 5). The remainder were Clavien grade II/III complications. Transient elevation in creatinine was reported in 10 cases (8.6% of patients, Table 5). Interestingly, Yuruk et al. classified 5 cases of renal colic as grade 3a [9]. However, the authors did not mention the nature of the intervention. They suggested that the local population might have a lower pain threshold than normal. None of the procedures required conversion to open surgery. Furthermore, there were no cases of renal haematoma or ureteric perforation. Finally, across all of the studies there were no reported deaths.
Table 5.
Nature of complication, frequency and Clavien grade (according to the papers)
| Nature of complication | Frequency | Clavien grade |
|---|---|---|
| Fever | 5 | I |
| Transient haematuria | 3 | I |
| Acute urinary retention | 3 | I |
| Transient elevation of creatinine | 10 | I |
| Urosepsis | 6 | II |
| Steinstrasse causing anuria and acute renal injury | 1 | III |
| Colicky pain | 5 | IIIa |
Quality of included studies and outcome reporting
Overall, the scientific rationale and specific objectives were well reported by the 4 studies. However, the methods of follow up were poorly described. The studies also failed to discuss how potential sources of bias and loss to follow up data were addressed. All of the author groups discussed the relative limitations of their study, however they did not comment on the generalizability and thus external validity of their results. Table 6 illustrates the evaluation of the quality of the included studies, according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. In the reporting of complications, the methods of accruing data were well defined and each study utilised a validated grading system. However, none of the studies provided evidence of risk stratification in their analyses, nor were mortality rates consistently recorded. Longer periods of follow up would allow for evaluation of late complications such as ureteral stenosis. Table 7 outlines the breakdown of complication reporting, according to the Martin criteria. The mean number of Martin criteria satisfied was 6.25/10 [7].
Table 6.
STROBE checklist for included studies (Y – yes, N – no, P – partial)
| Article section | STROBE checklist | Atis | Yuruk | Gao | Giusti | |
|---|---|---|---|---|---|---|
| Title and abstract | 1 | Indicate the study's design with a commonly used term in the title or the abstract | N | P | P | P |
| Provide in the abstract an informative and balanced summary of what was done and what was found | Y | Y | Y | Y | ||
| Introduction | ||||||
| Background | 2 | Explain the scientific background and rationale for the investigation being reported | Y | Y | Y | Y |
| Objectives | 3 | State specific objectives, including any pre-specified hypotheses | Y | Y | Y | P |
| Methods | ||||||
| Study design | 4 | Present key elements of study design early in the paper | Y | Y | Y | Y |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | Y | Y | P | Y |
| Participants | 6 | Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up | P | P | P | P |
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | P | P | N | N |
| Data sources | 8 | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | Y | Y | Y | Y |
| Bias | 9 | Describe any efforts to address potential sources of bias | N | N | N | N |
| Study size | 10 | Explain how the study size was arrived at | Y | Y | Y | Y |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | N | N | P | P |
| Statistical methods | 12 | Describe all statistical methods, including those used to control for confounding | Y | Y | Y | Y |
| Describe any methods used to examine subgroups and interactions | Y | Y | Y | N | ||
| Explain how missing data were addressed | N | N | N | N | ||
| If applicable, explain how loss to follow-up was addressed | N | N | N | N | ||
| Results | ||||||
| Participants | 13 | Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyse | N | N | N | N |
| Give reasons for non-participation at each stage | N | N | N | N | ||
| Consider use of a flow diagram | N | N | N | N | ||
| Descriptive data | 14 | Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | Y | Y | Y | Y |
| Indicate number of participants with missing data for each variable of interest | N | N | N | N | ||
| Summarise follow-up time (eg, average and total amount) | P | P | P | P | ||
| 15 | Report numbers of outcome events or summary measures over time | Y | Y | Y | Y | |
| 16 | Give unadjusted estimates and, if applicable, confounder- adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included | N | N | N | N | |
| If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | N | N | N | N | ||
| 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses | Y | Y | Y | N | |
| Discussion | ||||||
| Key results | 18 | Summarise key results with reference to study objective | Y | Y | Y | Y |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | Y | P | Y | P |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | Y | Y | P | Y |
| Generalisabilty | 21 | Discuss the generalisability (external validity) of the study results | N | N | N | N |
| Other information | ||||||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | N | N | N | N |
Table 7.
Martin criteria of complications (Y –yes, N – no)
| Martin criteria | Atis | Yuruk | Gao | Giusti |
|---|---|---|---|---|
| Method of accruing data defined | Y | Y | Y | Y |
| Duration of follow-up indicated | N | N | Y | Y |
| Outpatient information included | Y | N | Y | Y |
| Definition of complications provided | N | N | N | N |
| Mortality rate and causes of death listed | N | N | N | N |
| Morbidity rate and total complications indicated | Y | Y | Y | Y |
| Procedure-specific complications included | Y | Y | Y | Y |
| Severity grade utilised | Y | Y | Y | Y |
| Length-of-stay data | Y | Y | Y | Y |
| Risk factors included in the analysis | N | N | N | N |
| Total (n/10) | 6/10 | 5/10 | 7/10 | 7/10 |
DISCUSSION
This is the first systematic review to evaluate the outcomes of URS for urolithiasis in a solitary functioning kidney. The review suggests that URS is a feasible option in the management of single kidney calculi, with high stone free rates without significant compromise of biochemical renal functions. Meanwhile, it can still maintain an acceptable high-risk complication rate. The risk of obstructive uropathy from residual fragments is imminent in this cohort of patients. It is therefore vital that these patients are managed in a timely manner, so as to avoid life threatening consequences and permanent kidney damage – which would require future long-term renal replacement therapy. All of the patients in this review were post-operatively managed with a ureteric stent. This would seem a pragmatic approach in this cohort of patients, considering the risks associated with obstructing residual fragments.
Shockwave lithotripsy
SWL offers a non-invasive approach and usually does not require general anaesthesia. SWL has been reported to yield lower stone clearance rates in comparison to both URS and PCNL [12]. The number of repeat sessions is also greater as reported by Resorlu et al. [13]. Only the study by Yuruk et al.. compared URS with another intervention (SWL). The authors recorded a notably lower final stone free rate of 66.6% in the URS group vs. 73.3% in the SWL group [9]. However, despite the SWL group recording a superior stone free rate, 7 patients required salvage URS and overall, the patients undergoing URS required a significantly lower number of sessions to achieve a stone free status (1.06 vs. 2.2, p = 0.0001). El-Assmy et al. reported findings from their study of 156 patients with a solitary kidney who had undergone SWL [14]. 12.8% of the sample required secondary procedures and the overall SFR was 80.8%. Recent studies on URS have consistently reported much higher SFR values compared to the final SFR recorded by Yuruk et al. Of note, Jessen et al. reported a final SFR of 100% in their retrospective cohort study of 111 patients who underwent URS at a tertiary care centre [15]. Post-procedure steinstrasse is associated with SWL and occurs in approximately 4–7% of cases [16]. Evidence would suggest that patients with a solitary kidney are at a greater risk of developing steinstrasse, especially if a large stone burden is present [17, 18]. While the short term effects of SWL have been evaluated in detail, its potential deleterious effects on renal function at long term follow up remain under reported. However, a recent systematic review by Fankhauser et al., concluded that insufficient evidence exists to suggest that SWL leads to chronic kidney disease [19].
Percutaneous nephrolithotomy
PCNL is associated with the highest stone clearance rates, especially for large stone burdens and is superior to URS in this respect [10, 20]. However, the risk of haemorrhage is significant with PCNL [21]. El-Nahas et al., in their review of over 3800 PCNL cases, identified a solitary kidney as a significant risk factor for severe bleeding [1]. The rate of transfusion in patients with a single kidney has been recorded at 10% [22]. As for SWL, controversy exists in regards to the impact of PCNL on renal function. Akman et al. reported a stable or improved renal function in 90.1% of patients with a solitary kidney at the 6 month follow up post PCNL monotherapy [21]. Severe bleeding has been recorded in up to 17.5% of cases [23]. Other recorded complications include colonic injury and urinary extravastation. Bucuras et al. recorded fever and perforation(s) in 13.3% and 4.3% of cases respectively, in their study of PCNL in solitary kidneys [22].
Safety
Patients on anticoagulant therapy or with known bleeding disorders cause added concern for SWL and PCNL treatment. Similarly, with the rise in obesity, a known risk factor for nephrolithiasis, SWL has limited feasibility. Technical success via PCNL is therefore very difficult to achieve. In contrast, URS has been proven safe for both patients with a bleeding diathesis and obese patients while still being able to yield effective outcomes [24, 25]. Furthermore, success rates for larger stones (20–40 mm) have been shown to be comparable to PCNL [26].
In comparison to URS, a greater number of studies have investigated the outcomes of PCNL in patients with a solitary kidney. However, most evidence has been drawn from retrospective single centre studies with small sample sizes. Wong et al. reported an initial SFR of 59% and final SFR of 77% in their retrospective analysis of 17 patients who underwent PCNL with a single functioning kidney [27]. Ozturk et al. have previously highlighted that while PCNL is an increasingly successful technique, it is the potential complication of major haemorrhage that is the critical factor which may favour selection of an alternative therapy such as URS [28].
Limitations and implications for practice
There is a paucity of published data on the outcomes of patients with a solitary kidney undergoing URS for stone disease. A key limitation, therefore, in regard to this review is the low number of eligible studies. The majority of the studies were retrospective in design and all were carried out at single institutions. Heterogeneity was added to by the lack of standardized end points. Thus, a further limitation is the low quality of the included studies. As highlighted by the Clinical Research Office Of the Endourological Society (CROES) URS Global Study, there is no universally agreed criteria for declaring stone free status. And similarly, there is an entire range of imaging techniques which have been employed to detect residual fragments [29]. Somani et al. have recently suggested the use of “Stone Free Level” as an outcome measure of intervention for renal tract calculi [30]. This is a simple model; however, it will require acceptability and validation before being put to widespread use. More effort and research is required to design similar models.
Future research
For dissemination of widespread standardized practice, there is a requirement for high quality evidence. Further research in the form of randomized studies, prospective collaborative studies or large volume single series are required to establish the safety and feasibility of URS in solitary kidneys. Furthermore, the comparison of outcomes of URS with SWL and PCNL in solitary kidneys will be required in a randomized control trial setting.
CONCLUSIONS
This contemporary review highlights URS as a viable treatment option for stone disease in patients with a solitary kidney; the technique is able to yield good stone clearance with minimal morbidity. URS is associated with superior clearance rates to SWL and fewer high-risk complications compared to PCNL. Further studies are needed, firstly to confirm these findings and secondly, to formally establish the role of ureteroscopy in the management of stone disease in the solitary kidney.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.El-Nahas AR, Shokeir AA, El-Assmy AM, et al. Post-percutaneous nephrolithotomy extensive hemorrhage: a study of risk factors. J Urol. 2007;177:576–579. doi: 10.1016/j.juro.2006.09.048. [DOI] [PubMed] [Google Scholar]
- 2.Wendt-Nordahl G, Mut T, Krombach P, Michel MS, Knoll T. Do new generation flexible ureterorenoscopes offer a higher treatment success than their predecessors? Urol Res. 2011;39:185–188. doi: 10.1007/s00240-010-0331-0. [DOI] [PubMed] [Google Scholar]
- 3.Caskurlu T, Atis G, Arikan O, Pelit ES, Kilic M, Gurbuz C. The impact of body mass index on the outcomes of retrograde intrarenal stone surgery. Urol. 2013;81:517–521. doi: 10.1016/j.urology.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 5.OCEBM levels of evidence working group. The Oxford levels of evidence 1. Oxford Centre for Evidence-Based Medicine; 2011. http://www.cebm.net/index.aspx?o=1025. [Google Scholar]
- 6.Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklists. STROBE Statement. Website. http://www.strobe-statement.org/index.php?id=available-checklists.
- 7.Martin RC, II, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–813. doi: 10.1097/00000658-200206000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atis G, Gurbuz C, Arikan O, et al. Retrograde intrarenal surgery for the treatment of renal stones in patients with a solitary kidney. Urol. 2013;82:290–294. doi: 10.1016/j.urology.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Yuruk E, Binbay M, Ozgor F, Sekerel L, Berberoglu Y, Muslumanoglu AY. Comparison of Shockwave Lithotripsy and Flexible Ureteroscopy for the Treatment of Kidney Stones in Patients with a Solitary Kidney. J Endourol. 2015;29:463–467. doi: 10.1089/end.2014.0613. [DOI] [PubMed] [Google Scholar]
- 10.Gao X, Peng Y, Shi X, Li L, Zhou T, Xu B, Sun Y. Safety and efficacy of retrograde intrarenal surgery for renal stones in patients with a solitary kidney: a single-center experience. J Endourol. 2014;28:1290–1294. doi: 10.1089/end.2014.0295. [DOI] [PubMed] [Google Scholar]
- 11.Giusti G, Proietti S, Cindolo L, et al. Is retrograde intrarenal surgery a viable treatment option for renal stones in patients with solitary kidney? World J Urol. 2015;33:309–314. doi: 10.1007/s00345-014-1305-6. [DOI] [PubMed] [Google Scholar]
- 12.Kruck S, Anastasiadis AG, Herrmann TR, et al. Minimally invasive percutaneous nephrolithotomy: an alternative to retrograde intrarenal surgery and shockwave lithotripsy. World J Urol. 2013;31:1555–1561. doi: 10.1007/s00345-012-0962-6. [DOI] [PubMed] [Google Scholar]
- 13.Resorlu B, Kara C, Oguz U, Bayindir M, Unsal A. Percutaneous nephrolithotomy for complex caliceal and staghorn stones in patients with solitary kidney. Urol Res. 2011;39:171–176. doi: 10.1007/s00240-010-0321-2. [DOI] [PubMed] [Google Scholar]
- 14.el-Assmy A, el-Nahas AR, Hekal IA, Badran M, Youssef RF, Sheir KZ. Long-term effects of extracorporeal shock wave lithotripsy on renal function: our experience with 156 patients with solitary kidney. J Urol. 2008;179:2229–2232. doi: 10.1016/j.juro.2008.01.095. [DOI] [PubMed] [Google Scholar]
- 15.Ather MH, Shrestha B, Mehmood A. Does ureteral stenting prior to shock wave lithotripsy influence the need for intervention in steinstrasse and related complications? Urol Int. 2009;83:222–225. doi: 10.1159/000230028. [DOI] [PubMed] [Google Scholar]
- 16.Jessen JP, Honeck P, Knoll T, Wendt-Nordahl G. Flexible ureterorenoscopy for lower pole stones: influence of the collecting system's anatomy. J Endourol. 2014;28:146–151. doi: 10.1089/end.2013.0401. [DOI] [PubMed] [Google Scholar]
- 17.Hyams ES, Munver R, Bird VG, Uberoi J, Shah O. Flexible ureterorenoscopy and holmium laser lithotripsy for the manage- ment of renal stone burdens that measure 2 to 3 cm: A multi-institutional experience. J Endourol. 2010;24:1583–1588. doi: 10.1089/end.2009.0629. [DOI] [PubMed] [Google Scholar]
- 18.Mariani AJ. Combined electrohydraulic and holmium:YAG laser ureteroscopic nephrolithotripsy of large (greater than 4 cm) renal calculi. J Urol. 2007;177:168–173. doi: 10.1016/j.juro.2006.08.066. [DOI] [PubMed] [Google Scholar]
- 19.Fankhauser CD, Kranzbühler B, Poyet C, Hermanns T, Sulser T, Steurer J. Long-term Adverse Effects of Extracorporeal Shock-wave Lithotripsy for Nephrolithiasis and Ureterolithiasis: A Systematic Review. Urology. 2015;85:991–1006. doi: 10.1016/j.urology.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Bryniarski P, Paradysz A, Zyczkowski M, Kupilas A, Nowakowski K, Bogacki R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol. 2012;26:52–57. doi: 10.1089/end.2011.0235. [DOI] [PubMed] [Google Scholar]
- 21.Akman T, Binbay M, Tekinarslan E, et al. Outcomes of percutaneous nephrolithotomy in patients with solitary kidneys: a single-centre experience. Urology. 2011;78:272–276. doi: 10.1016/j.urology.2010.12.029. [DOI] [PubMed] [Google Scholar]
- 22.Bucuras V, Gopalakrishnam G, Wolf JS, et al. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: nephrolithotomy in 189 patients with solitary kidneys. J Endourol. 2012;26:336–341. doi: 10.1089/end.2011.0169. [DOI] [PubMed] [Google Scholar]
- 23.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 24.Turna B, Stein RJ, Smaldone MC, et al. Safety and efficacy of flexible ureterorenoscopy and holmium: YAG lithotripsy for intrarenal stones in anticoagulated cases. J Urol. 2008;179:1415–1419. doi: 10.1016/j.juro.2007.11.076. [DOI] [PubMed] [Google Scholar]
- 25.Caskurlu T, Atis G, Arikan O, Pelit ES, Kilic M, Gurbuz C. The impact of body mass index on the outcomes of retrograde intrarenal stone surgery. Urology. 2013;81:517–521. doi: 10.1016/j.urology.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Riley JM, Stearman L, Troxel S. Retrograde ureteroscopy for renal stones larger than 2.5 cm. J Endourol. 2009;23:1395–1398. doi: 10.1089/end.2009.0391. [DOI] [PubMed] [Google Scholar]
- 27.Wong KA, Sahai A, Patel A, Thomas K, Bultitude M, Glass J. Is percutaneous nephrolithotomy in solitary kidneys safe? Urology. 2013;82:1013–1016. doi: 10.1016/j.urology.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 28.Yesil S, Ozturk U, Goktug HN, Tuygun C, Nalbant I, Imamoglu MA. Previous open renal surgery increased vascular complications in percutaneous nephrolithotomy (PCNL) compared with primary and secondary PCNL and extracorporeal shock wave lithotripsy patients: a retrospective study. Urol Int. 2013;91:331–334. doi: 10.1159/000351968. [DOI] [PubMed] [Google Scholar]
- 29.Skolarikos A, Gross AJ, Krebs A, et al. Outcomes of flexible ureteroscopy for solitary renal stones in the Clinical Research Office of Endourological Society URS Global study. J Urol. 2015;194:137–143. doi: 10.1016/j.juro.2015.01.112. [DOI] [PubMed] [Google Scholar]
- 30.Somani BK, Desai M, Traxer O, Lahme S. Stone-free rate (SFR): a new proposal for defining levels of SFR. Urolithiasis. 2014;42:95. doi: 10.1007/s00240-013-0630-3. [DOI] [PubMed] [Google Scholar]