Abstract
Aims: The present study investigated the effect of different surface treatments on shear bond strength (SBS) of resin cement to zirconia.
Materials and methods: Ninety zirconia blocks were prepared and divided into 6 groups of 15 by treatment. Group 1 served as the control group, whereas groups 2 and 3 were treated with air abrasion and a universal primer (Monobond plus), respectively. The remaining zirconia copings were treated with a fractional CO2 laser for 10 seconds using 10 W/10 mJ (group 4), 10 w/14 mJ (group 5) or 20 W/10 mJ (group 6). A luting cement (Clearfil SA) was bonded to the treated zirconia surfaces and cured for 40 seconds. SBS was measured with a universal testing machine and the type of bond failure was determined.
Results: There was a statistically significant difference in SBS among the study groups (p<0.001). The highest SBS values were observed in the groups treated with the fractional CO2 laser at settings of 20 W/10 mJ (28.1 MPa) or 10 W/14 mJ (27.4 MPa), followed by the specimens treated with the universal primer (22.8 MPa). The control specimens exhibited the lowest SBS (9.4 MPa) among the study groups (p<0.05). There was no significant difference in the distribution of failure modes among the groups (p=0.871).
Conclusions: The application of fractional CO2 laser can improve bond strength of resin cement to zirconia ceramic, and thus it could be considered as an appropriate alternative to conventional methods of zirconia surface treatment.
Keywords: Zirconia, bond strength, laser, ceramic, porcelain, fractional, CO2, surface treatment, resin cement
Introduction
Partially stabilized zirconium oxide (zirconia) has attained a growing use in all-ceramic fixed dental restorations because of its great advantages including enhanced esthetic qualities, improved mechanical properties, and excellent chemical stability and biocompatibility 1). Bonding to zirconia prostheses, however, has been considered as a challenging issue in dentistry. The conventional methods of surface preparation such as etching with hydrofluoric acid are not effective against zirconia because of the absence of a glassy matrix in highly crystalline ceramics on which these substances act 1).
Several attempts have been made to develop micromechanical and chemical retention in order to ensure reliable and predictable bonding strength to dental oxide ceramic restorations in the clinical situation. A variety of mechanical techniques have been suggested for surface modification of oxide ceramics including grinding/polishing, air-borne particle abrasion with aluminum oxide particles, tribochemical silicon dioxide (silica) coating, and laser conditioning 2). These techniques are mainly aimed to roughen the cementation surface of the ceramic, which leads to increased surface area and micromechanical interlocking, thereby improving the bond strength. Furthermore, the use of resin cements or primers containing 10-methacryloxydecyl dihydrogen phosphate (MDP) has been shown to enhance the strength of the adhesion by providing chemical retention to zirconia, although the durability of the chemical bond may be compromised in the clinical conditions 1–3).
Lasers have been used for different purposes in dentistry among which is conditioning tooth structure or restorative surfaces 4–9). Previous studies employed different lasers such as neodymium-doped yttrium aluminum garnet (Nd:YAG) 10, 11), neodymium-doped yttrium aluminum perovskite (Nd:YAP) 12), erbium-doped yttrium aluminum garnet (Er:YAG) 13), and carbon dioxide (CO2) 14, 15) for surface modification of zirconia ceramic, and reported varying degrees of success. The CO2 laser is generally employed for intraoral soft tissue surgery because of its great absorption in water 16). The wavelength of the CO2 laser (10600 nm) is also well absorbed by ceramic materials, making it a suitable instrument for ceramic surface treatment 17, 18). To date, a few studies investigated the efficacy of conventional CO2 laser for enhancing adhesion of bonding cement to metal oxide ceramics 14, 15, 19–21), but to the authors’ knowledge, no study employed a fractional type of CO2 laser for zirconia surface treatment.
The concept of fractional photothermolysis was introduced in 2003 22) in order to reduce the adverse effects of skin resurfacing with ablative CO2 and Er:YAG lasers such as prolonged downtime, long-lasting erythema, edema, burning and scarring 18, 23, 24). Fractional laser therapy is a non-invasive treatment that uses a device to generate thousands of microscopic treatment zones by scanning the target area, radiating a fraction of the skin at a time. This is analogous to a photographic image being enhanced or altered pixel by pixel. The tissues surrounding to the microscopic treatment zones remain healthy and untreated, and thus supporting the wound healing process 18, 23, 24). Fractional laser treatment has bridged the gap between the ablative and non-ablative laser techniques used to treat sun-damaged and aged skin. Whilst ablative laser treatments work mainly on the epidermis (surface skin cells) and non-ablative treatments work solely on dermal collagen (mid-layer of skin), fractional laser treatment works at both the epidermal and dermal layers of the skin 25).
The use of fractional CO2 laser may be associated with several advantages: when applied for surface treatment, it allows the clinician to predetermine the radiation area where the laser irradiates multiple zones with predefined space between them, so eliminating the need for manual movement of the laser handpiece by the clinician. This should result in attaining a more homogenous etching pattern on the surface, while reducing the risk of thermal damage to the underlying tissues 18). For these reasons, even if up today it is not yet commonly used in dentistry, we think it may be useful for surface treatment of zirconia copings.
The present study investigated the effect of several surface preparation methods including air abrasion, a universal primer and fractional CO2 laser irradiation on bond strength of a resin cement to zirconia ceramic.
Materials and methods
Ninety blocks each measuring 8 × 8 mm (5 mm thick) were fabricated from high-purity zirconium oxide ceramic (Dental Direkt GmbH, Spenge, Germany) according to the manufacturer's instructions. The zirconia ceramic specimens were free of cracks or surface defects and were mounted horizontally in acrylic resin blocks ensuring that the ceramic surface remained intact for the bonding procedure. The ceramic surfaces were cleaned with ethyl alcohol and then randomly assigned into 6 groups of 15 each. The surface treatment procedures in the study groups were as follows:
Group 1 received no surface treatment and served as the control group. The specimens in group 2 underwent air abrasion with 50 µm aluminum oxide (Al2O3) particles, which was applied at 2.5 bar pressure for 15 seconds. The device was held at the distance of 10 mm and perpendicular to the ceramic surface. The specimens were then rinsed thoroughly under tap water to remove aluminum oxide particles and air dried. In group 3, a universal primer containing MDP (Monobond plus; Ivoclar Vivadent, Schaan, Liechtenstein) was employed as a method of surface treatment. The primer was applied over the ceramic surface with a disposable applicator and allowed to dry for 1 minute.
The surfaces of the specimens in groups 4 to 6 were etched with a fractional CO2 laser (wavelength 10.6 µm; Lutronic Inc., Princeton Junction, NJ, USA) (Fig 1) with different parameters. These parameters were drawn from a previous study 18) and the results of our pilot study (data have not been presented) to find the minimum laser parameters to modify the zirconia surface. The laser apparatus was run in the dynamic mode and the setting was so that a square area of 4 mm × 4 mm was irradiated at the middle of the ceramic specimen. The tip of the laser was held manually perpendicular to the zirconia ceramic at the distance of 3 cm. The frequency of 200 Hz (pulse per second) and irradiation time of 10 seconds were used in all laser groups, while the choice of power, energy and pulse duration was different. The specimens were treated at 10 W/10 mJ in group 4, 10 W/14 mJ in group 5 and 20 W /10 mJ in group 6. The durations of the pulse were 1.25 msec, 1.75 msec and 0.58 msec in groups 4, 5 and 6, respectively. Due to the different power settings and pulse durations, the energy delivered to each treated surface was approximately 23 J in group 4, 28 J in group 5 and 24 J in group 6, as calculated by the laser device.
Fig. 1:
The fractional CO2 laser used in this study
After the surface preparations mentioned in the study groups, a MDP-containing resin cement (Clearfil SA Luting; Kurary, Kurashiki, Okayama, Japan) was prepared using equal lengths of base and catalyst pastes according to the manufacturer's instructions. The cement was then poured into plastic molds measuring 2 mm in height and 1.5 mm in diameter positioned over the surfaces of the specimens. The excess cement was removed with the explorer tip from the periphery of the mold and the luting agent was then photopolymerized for 40 seconds from four opposite directions (10 seconds each) using Bluephase C8 (Ivoclar Vivadent, Schaan, Liechtenstein) light emitting diode (LED) at power density of 650 mW/cm2. After 30 minutes, the plastic molds were cut and carefully removed and the specimens were immersed in distilled water for 24 hours at room temperature. Each sample was then subjected to shear bond strength (SBS) test, which was performed by an Instron Universal testing machine (Santam, model STM-20, Tehran, Iran) at a cross head speed of 1 mm/min. The shear force was applied parallel to the bonded surface of the zirconia ceramic until failure. The SBS was recorded in Newtons and then converted to megapascals (MPa) by dividing the failure load by the bonding area (mm2).
Finally, the fractured interfaces of the samples were examined under a stereomicroscope at 10 X magnification to determine the type of bond failure. The failure modes were classified as adhesive (failure at the interface of the luting cement and ceramic), cohesive (failure inside the resin cement or ceramic) and mixed (a combination of adhesive and cohesive failures).
Statistical analysis
The Kolmogorov-Smirnov test confirmed the normal distribution of the data. One way analysis of variance (ANOVA) was run to determine any significant difference in bond strength among the study groups followed by Duncan post hoc test for pairwise comparisons. The failure modes were scored as adhesive=1, cohesive=2 and mixed=3, and the difference in failure modes between the groups was analyzed by Fisher's exact test. The statistical analysis was performed by SPSS software (Statistical Package for Social Sciences, Version 16.0, SPSS Inc, Chicago, Ill, USA) and the significance level was set at p<0.05.
Results
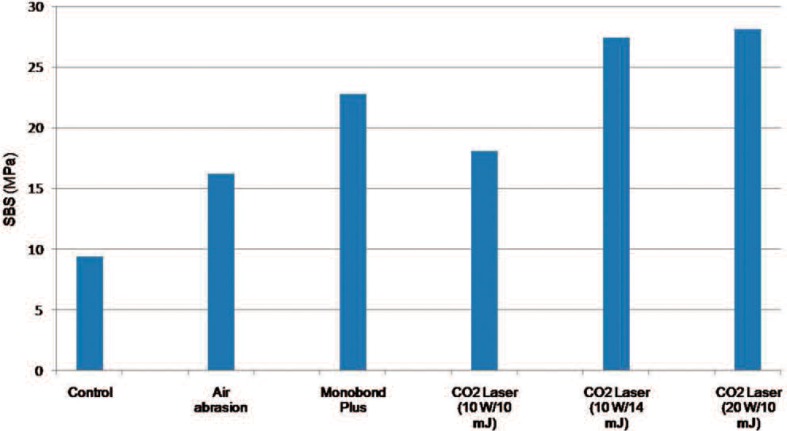
Table 1 presents the descriptive statistics and the results of statistical analysis for comparison of SBS values (MPa) among the study groups. The greatest bond strength was observed when the fractional CO2 laser was employed at settings of 20 W/10 mJ (28.1 MPa) or 10 W/14 mJ (27.4 MPa). The next SBS pertained to the specimens treated with Monobond Plus (22.8 MPa). The control specimens exhibited the lowest strength of resin cement to zirconia (9.4 MPa) among the study groups (Table 1, Fig 2).
Table 1: The mean (MPa), standard deviation (SD), range, and the results of statistical analysis for comparing SBS of zirconia specimens in the study groups.
| Group | Definition | Mean | SD | Range | Pairwise comparison* |
|---|---|---|---|---|---|
| 1 | Control | 9.4 | 1.8 | 6.4–11.7 | a |
| 2 | Air abrasion | 16.2 | 2.6 | 12.5–20.5 | b |
| 3 | Monobond Plus | 22.8 | 5.7 | 17.8–23.4 | c |
| 4 | CO2 Laser (10 W/10 mJ) | 18.1 | 3.1 | 14.5–24.5 | b |
| 5 | CO2 Laser (10 W/14 mJ) | 27.4 | 3.7 | 11.8–43.6 | d |
| 6 | CO2 Laser (20 W/10 mJ) | 28.1 | 4.9 | 18.2–36.5 | d |
| Statistical significance (ANOVA) | P<0.001 | ||||
Duncan post-hoc comparison test; the groups that have been marked with different letters show significant differences at p<0.05; whereas those with the same letters are statistically comparable (p>0.05).
Fig. 2:
Shear bond strength (MPa) of the study groups
Comparison of SBS values by ANOVA indicated a significant difference among the study groups (Table 1). Duncan test revealed that bond strength was significantly lower in the untreated zirconia controls than all other groups (p<0.05). The use of fractional CO2 laser at 10 W/14 mJ (group 5) or 20 W/10 mJ (group 6) yielded bond strength values that were comparable to each other and both were significantly greater than that of the other study groups (p<0.05). The bond strength of the specimens treated by Monobond Plus was significantly greater than that of the other groups except groups 5 and 6. No significant difference was found in SBS among the air-abraded specimens and those irradiated with the fractional CO2 laser at settings of 10 W/10 mJ (p>0.05, Table 1).
Table 2 indicates the frequency of different failure types in the samples. The failure mode was predominantly adhesive in all the study groups followed by mixed mode fracture. The Fisher's exact test revealed no significant difference in the distribution of failure modes among the study groups (p=0.871).
Table 2: The frequency (and percentage) of failure modes in the experimental groups.
| Group | Definition | Adhesive | Cohesive | Mixed |
|---|---|---|---|---|
| 1 | Control | 11 (73) | 4 (27) | |
| 2 | Air abrasion | 11 (73) | 1 (7) | 3 (20) |
| 3 | Monobond Plus | 10 (67) | 5 (33) | |
| 4 | CO2 Laser (10 W/10 mJ) | 12 (80) | 3 (20) | |
| 5 | CO2 Laser (10 W/14 mJ) | 9 (60) | 2 (13) | 4 (27) |
| 6 | CO2 Laser (20 W/10 mJ) | 11 (73) | 1 (7) | 3 (20) |
Discussion
This study indicated that the resin-zirconia bond strength is significantly influenced by the employed surface treatment. The SBS values of the specimens prepared with the fractional CO2 laser (10 W/14 mJ or 20 W/10 mJ) were significantly greater than that of the other groups, followed by those treated by Monobond Plus primer. As expected, the untreated zirconia surfaces, which were not subjected to any surface preparation technique exhibited the lowest SBS among the study groups. The luting agent used in this study (Clearfil SA) is a dual cured resin cement containing MDP. The use of resin cements is associated with advantages such as low solubility and high optical properties 1). Furthermore, previous studies have shown that resin cements containing phosphate ester groups could make a chemical bond with metal oxides such as zirconium oxide and thus provide enhanced adhesion to all-ceramic restorations 1, 3, 26).
Air-borne particle abrasion, also defined as sandblasting, is usually performed by aluminum oxide particles and is one of the most commonly used mechanical methods for surface preparation of zirconia copings 3). This technique roughens the ceramic surface and increases the surface area for bonding, thus enhancing the bond strength 27–29). Some authors considered surface damage and significant removal of substances from the surface as drawbacks of the sandblasting procedure, which can cause a reduction in flexural strength of the ceramics 3, 30). In a review literature, however, it was revealed that air abrasion produced an excellent clinically outcome with no ceramic fractures over up to 15 years observation time, indicating the lack of strength-reducing effect on oxide ceramic restorations in a clinical-based level 2). In the present study, air abrasion with Al2O3 particles produced a mean bond strength value that was nearly twice as that of the untreated controls but significantly lower than those treated by fractional CO2 laser (10 W/14 mJ or 20 W/10 mJ) or Monobond Plus.
The use of MDP-based primers or cements has been advocated to produce a chemical interaction between the hydroxyl groups of zirconia and the phosphate ester groups of MDP 1, 31). In the present study, the application of Monobond Plus which contains MDP caused a significant increase in resin to zirconia adhesion compared to that of the control and air abraded specimens. Kern 2) noticed that the use of a MDP containing primer in combination with a MDP-based luting cement caused a debonding rate of 13.3% over a follow- up period of 53 months. Foxton et al 32) indicated that the application of a ceramic primer containing phosphate monomer, without any additional surface treatment, resulted in a durable bond between a dualcured resin cement and zirconium oxide ceramic. Attia and coworkers 33) reported that the use of a universal primer containing a silane and a phosphate monomer (Monobond Plus) improved the strength of the adhesion to zirconia ceramic. In contast, Yi et al 34) found that control and Monobond Plus groups indicated the lowest bond strength values to zirconia ceramic compared to the groups treated by sandblasting or Z-PRIME Plus primer. Sanohkan et al 35) showed that the SBS of resin composite to zirconia was not significantly different among the surfaces treated with Monobond Plus and untreated controls. It should be noted that the chemical bond between MDP and the as-received zirconia surface is susceptible to hydrolytic degradation following long term water storage and/or thermal cycling 2). Therefore, most authors believe that the combination of a mechanical method such as air abrasion and a MDP-containing luting resin or primer is required to attain durable bonding to zirconia ceramic under the humid and stressful oral conditions 1–3, 36–41).
The present study reports successful results with a fractional CO2 laser for surface preparation of zirconia ceramic. The SBS values of the specimens treated with the fractional CO2 laser at either 10 W/14 mJ or 20 W/10 mJ were higher than any of the other treatment groups. This finding could be attributed to the efficacy of fractional CO2 laser in roughening the bonding surface through the process of thermomechanical ablation, which increases micromechanical retention, thereby enhancing the bond strength at the cement/zirconia interface. There is also the possibility of chemical alteration of the irradiated ceramic surface in the benefit of improved adhesion, although further studies are warranted to verify this assumption.
Although there is no study regarding the use of fractional CO2 laser for increasing bond strength of allceramic copings to resin cements, controversial reports exist on the use of conventional CO2 laser for zirconia surface modification. Kasraee et al 15) observed higher bond strength values in CO2 laser treated zirconia compared to the control and Er:YAG laser-treated groups. Ural et al 21) demonstrated that CO2 laser etching caused a significant increase in bond strength of zirconi ceramic compared to the control, air abraded and HF acid-treated groups. In contrast, Akhavan Zanjani et al 14) reported that air abrasion had a greater efficacy than CO2 and Er,Cr:YSGG lasers in conditioning the zirconia surfaces to enhance their bonding strengths to resin cement. Paranhos et al 20) observed significant microcracks and reduced bond strength in zirconia specimens treated with the CO2 laser compared to that of the Nd:YAG laser-treated groups. Akin et al 19) found that the lowest SBS was recorded in the CO2 laser-treated group, whereas the highest SBS pertained to the specimens prepared with the Nd:YAG laser in contact mode. The differences between the results of this study and those of previous investigations could be attributed to the laser apparatus employed and also to the use of different laser parameters and durations of application in these studies. Furthermore, the manual movement of the laser's handpiece as used by previous authors carries the risk of creating inhomogeneous etching pattern, whereas manual scanning is not required when using a fractional CO2 laser for surface conditioning.
A previous study 18) recommended the use of fractional CO2 laser at settings of 10 W/10 mJ for treatment of feldspathic porcelain, which yielded favorable strength results without damaging the porcelain surface. In the present study, the application of fractional CO2 laser at 10 w/10 mJ produced bond strength that was comparable to that of the Al2O3 air abrasion group but significantly lower than that achieved with higher power or energy settings (10 W/14 mJ or 20 W/10 mJ). This may be related to the great percentage of zirconium oxide in zirconia ceramic, which justifies the use of higher laser parameters for surface modification. Further studies are warranted to test the effect of different parameters of fractional CO2 laser on surface morphology and surface roughness of all-ceramic copings and assess the resultant bond strength in the clinical conditions.
The mode of failure was examined in this study to obtain further information about the quality of the bond and the resin-cement interface. The failures were mostly adhesive between the luting cement and zirconia followed by mixed mode fracture. Few cases treated with air abrasion or fractional CO2 laser showed cohesive type of fracture. In general, cohesive failure occurs when the adhesion of luting cement to ceramic is higher than the shear strength of the ceramic or cement itself. Although SBS values in this study were high in the specimens treated by the fractional CO2 laser or Monobond Plus, the frequency of cohesive failure was not significantly greater in these groups compared to that of the other study groups. This indicates that the type of bond failure is not only influenced by the bond strength value, but also other factors can affect the bonding interface 42, 43).
It is believed that values equal to or greater than 20 MPa could provide sufficient bond strength regardless of the test method employed 3). Others considered the higher limit of 25 MPa to represent sufficient bond strength for clinical practice 3). Keeping this in mind, the findings of the present study indicate that treatment of zirconia ceramic either with a fractional CO2 laser or with a MDP-containing primer could provide sufficient bond strength between a MDP-containing resin cement and zirconia. The SBS values of air-abraded specimens or those treated with the fractional CO2 laser at 10 W/10 mJ, although were significantly greater than that achieved by the controls, did not reach the threshold limit required for successful bonding in the clinical conditions. The present study proposed fractional CO2 laser as a suitable strategy for surface treatment of oxidebased ceramics, which can provide bond strength values remarkably greater than that of the conventional techniques of zirconia surface treatment. This method may be extremely useful in dental restorations with limited or no mechanical retention in the preparation design, which rely heavily on bonding interface.
The limitation of this study was that it did not evaluate bond strength values after artificial aging for example by exposing the specimens to thermocycling or long term water storage. Therefore, the results of this study should be carefully extrapolated to the clinical conditions. The present investigation also did not evaluate the combined effect of fractional CO2 laser and MDP containing primer on SBS of zirconia copings. Further long-term studies are suggested to determine SBS values of laser treated zirconia in the clinical situation.
Conclusions
Under the conditions used in this study
Irradiation from a fractional CO2 laser at either 10 W/14 mJ or 20 W/10 mJ was the most effective strategy for enhancing bond strength of the resin cement to zirconia, and thus it could be recommended as a suitable alternative to conventional methods of zirconia surface treatment.
The application of a universal primer containing MDP (Monobond plus), without any additional surface preparation, provided sufficient adhesion between the luting cement and zirconia.
The failure mode was mostly adhesive with no significant difference among the study groups, indicating the lack of relationship between bond strength and failure mode.
Acknowledgements
The authors would like to thank the research chancellor of Mashhad University of Medical Sciences for the financial support of this project (grant number 910845). The results presented in this paper have been taken from a student thesis (thesis number 2641).
Conflict of interest: The authors deny any conflict of interest.
References
- 1: Gargari M, Gloria F, Napoli E, Pujia AM. (2010). Zirconia: cementation of prosthetic restorations. Literature review. Oral Implantol (Rome) 3(4):25-29. [PMC free article] [PubMed] [Google Scholar]
- 2: Kern M. (2015). Bonding to oxide ceramics-Laboratory testing versus clinical outcome. Dent Mater 31(1):8-14. [DOI] [PubMed] [Google Scholar]
- 3: Papia E, Larsson C, du Toit M, Vult von Steyern P. (2014). Bonding between oxide ceramics and adhesive cement systems: a systematic review. J Biomed Mater Res B Appl Biomater 102(2):395-413. [DOI] [PubMed] [Google Scholar]
- 4: Ahrari F, Poosti M, Motahari P. (2012). Enamel resistance to demineralization following Er:YAG laser etching for bonding orthodontic brackets. Dent Res J (Isfahan) 9(4):472-477. [PMC free article] [PubMed] [Google Scholar]
- 5: Ahrari F, Akbari M, Akbari J, Dabiri G. (2013). Enamel surface roughness after debonding of orthodontic brackets and various clean-up techniques. J Dent (Tehran) 10(1):82-93. [PMC free article] [PubMed] [Google Scholar]
- 6: Ahrari F, Basafa M, Fekrazad R, Mokarram M, Akbari M. (2012). The efficacy of Er,Cr:YSGG laser in reconditioning of metallic orthodontic brackets. Photomed Laser Surg 30(1):41-46. [DOI] [PubMed] [Google Scholar]
- 7: Ahrari F, Fekrazad R, Kalhori KA, Ramtin M. (2013). Reconditioning of ceramic orthodontic brackets with an Er,Cr:YSGG laser. Lasers Med Sci 28(1):223-228. [DOI] [PubMed] [Google Scholar]
- 8: Dehghani M, Ahrari F. (2014). The effect of surface treatment with Er: YAG laser on shear bond strength of orthodontic brackets to fiber-reinforced composite. J Clin Exp Dent 6(4):e379-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9: Shahabi M, Ahrari F, Mohamadipour H, Moosavi H. (2014) Microleakage and shear bond strength of orthodontc brackets bonded to hypomineralized enamel following different surface preparations. J Clin Exp Dent 6(2):e110-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10: Spohr AM, Borges GA, Junior LH, Mota EG, Oshima HM. (2008). Surface modification of In- Ceram Zirconia ceramic by Nd:YAG laser, Rocatec system, or aluminum oxide sandblasting and its bond strength to a resin cement. Photomed Laser Surg 26(3):203-208. [DOI] [PubMed] [Google Scholar]
- 11: Usumez A, Hamdemirci N, Koroglu BY, et al. (2013). Bond strength of resin cement to zirconia ceramic with different surface treatments. Lasers Med Sci 28(1):259-266. [DOI] [PubMed] [Google Scholar]
- 12: Rocca JP, Fornaini C, Brulat-Bouchard N, Seif SB, Darque-Ceretti E. (2014). CO2 and Nd: YAP laser interaction with lithium disilicate and Zirconia dental ceramics: A preliminary study. Optics & Laser Technology 57: 216-223. [Google Scholar]
- 13: Lin Y, Song X, Chen Y, Zhu Q, Zhang W. (2013). Effect of Er:YAG laser irradiation on bonding property of zirconia ceramics to resin cement. Photomed Laser Surg 31(12):619-625. [DOI] [PubMed] [Google Scholar]
- 14: Akhavan Zanjani V, Ahmadi H, Nateghifard A, et al. (2014). Effect of different laser surface treatment on microshear bond strength between zirconia ceramic and resin cement. J Investig Clin Dent 6(4):294-300. [DOI] [PubMed] [Google Scholar]
- 15: Kasraei S, Rezaei-Soufi L, Heidari B, Vafaee F. (2014). Bond strength of resin cement to CO2 and Er:YAG laser-treated zirconia ceramic. Restor Dent Endod 39(4):296-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16: Pakfetrat A, Falaki F, Ahrari F, Bidad S. (2014). Removal of refractory erosive-atrophic lichen planus by the CO2 laser. Oral Health Dent Manag 13(3):595-599. [PubMed] [Google Scholar]
- 17: Ahrari F, Heravi F, Fekrazad R, Farzanegan F, Nakhaei S. (2012). Does ultra-pulse CO(2) laser reduce the risk of enamel damage during debonding of ceramic brackets? Lasers Med Sci 27(3):567-574. [DOI] [PubMed] [Google Scholar]
- 18: Ahrari F, Heravi F, Hosseini M. (2013). CO2 laser conditioning of porcelain surfaces for bonding metal orthodontic brackets. Lasers Med Sci 28(4):1091-1097. [DOI] [PubMed] [Google Scholar]
- 19: Akin H, Ozkurt Z, Kirmali O, Kazazoglu E, Ozdemir AK. (2011). Shear bond strength of resin cement to zirconia ceramic after aluminum oxide sandblasting and various laser treatments. Photomed Laser Surg 29(12):797-802. [DOI] [PubMed] [Google Scholar]
- 20: Paranhos MP, Burnett LH, Jr., Magne P. (2011). Effect Of Nd:YAG laser and CO2 laser treatment on the resin bond strength to zirconia ceramic. Quintessence Int 42(1):79-89. [PubMed] [Google Scholar]
- 21: Ural C, Kulunk T, Kulunk S, Kurt M. (2010). The effect of laser treatment on bonding between zirconia ceramic surface and resin cement. Acta Odontol Scand 68(6):354-359. [DOI] [PubMed] [Google Scholar]
- 22: Huzaira M, Anderson R, Sink K, Manstein D. (2003). Intradermal focusing of near-infrared optical pulses: A new approach for non-ablative laser therapy. Lasers Surg Med 15:66. [Google Scholar]
- 23: Geronemus RG. (2006). Fractional photothermolysis: current and future applications. Lasers Surg Med 38(3):169-176. [DOI] [PubMed] [Google Scholar]
- 24: Hantash BM, Bedi VP, Chan KF, Zachary CB. (2007). Ex vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med 39(2):87-95. [DOI] [PubMed] [Google Scholar]
- 25: Rahman Z, Alam M, Dover J. (2006). Fractional laser treatment for pigmentation and texture improvement. Skin Therapy Lett 11(9): 7-11. [PubMed] [Google Scholar]
- 26: Turker SB, Ozcan M, Mandali G, et al. (2013). Bond strength and stability of 3 luting systems on a zirconia- dentin complex. Gen Dent 61(7):e10-13. [PubMed] [Google Scholar]
- 27: Cavalcanti AN, Foxton RM, Watson TF, et al. (2009). Bond strength of resin cements to a zirconia ceramic with different surface treatments. Oper Dent 34(3):280-287. [DOI] [PubMed] [Google Scholar]
- 28: Ersu B, Yuzugullu B, Ruya Yazici A, Canay S. (2009). Surface roughness and bond strengths of glass-infiltrated alumina-ceramics prepared using various surface treatments. J Dent 37(11):848-856. [DOI] [PubMed] [Google Scholar]
- 29: Monaco C, Cardelli P, Scotti R, Valandro LF. (2011). Pilot evaluation of four experimental conditioning treatments to improve the bond strength between resin cement and Y-TZP ceramic. J Prosthodont 20(2):97-100. [DOI] [PubMed] [Google Scholar]
- 30: Zhang Y, Lawn BR, Rekow ED, Thompson VP. (2004). Effect of sandblasting on the long-term performance of dental ceramics. J Biomed Mater Res B Appl Biomater 71(2):381-386. [DOI] [PubMed] [Google Scholar]
- 31: Wolfart M, Lehmann F, Wolfart S, Kern M. (2007). Durability of the resin bond strength to zirconia ceramic after using different surface conditioning methods. Dent Mater 23(1):45-50. [DOI] [PubMed] [Google Scholar]
- 32: Foxton RM, Cavalcanti AN, Nakajima M, et al. (2011). Durability of resin cement bond to aluminium oxide and zirconia ceramics after air abrasion and laser treatment. J Prosthodont 20(2):84-92. [DOI] [PubMed] [Google Scholar]
- 33: Attia A, Lehmann F, Kern M. (2011). Influence of surface conditioning and cleaning methods on resin bonding to zirconia ceramic. Dent Mater 27(3):207-213. [DOI] [PubMed] [Google Scholar]
- 34: Yi YA, Ahn JS, Park YJ, et al. (2015). The Effect of Sandblasting and Different Primers on Shear Bond Strength Between Yttria-tetragonal Zirconia Polycrystal Ceramic and a Self-adhesive Resin Cement. Oper Dent 40(1):63-71. [DOI] [PubMed] [Google Scholar]
- 35: Sanohkan S, Kukiattrakoon B, Larpboonphol N, et al. (2013). The effect of various primers on shear bond strength of zirconia ceramic and resin composite. J Conserv Dent 16(6):499-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36: Kern M, Barloi A, Yang B. (2009). Surface conditioning influences zirconia ceramic bonding. J Dent Res 88(9):817-822. [DOI] [PubMed] [Google Scholar]
- 37: Lehmann F, Kern M. (2009). Durability of resin bonding to zirconia ceramic using different primers. J Adhes Dent 11(6):479-483. [DOI] [PubMed] [Google Scholar]
- 38: Roman-Rodriguez JL, Fons-Font A, Amigo-Borras V, et al. (2013). Bond strength of selected composite resin-cements to zirconium-oxide ceramic. Med Oral Patol Oral Cir Bucal 18(1):e115-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39: Shin YJ, Shin Y, Yi YA, et al. (2014). Evaluation of the shear bond strength of resin cement to Y-TZP ceramic after different surface treatments. Scanning 36(5):479-486. [DOI] [PubMed] [Google Scholar]
- 40: Yang B, Barloi A, Kern M. (2010). Influence of airabrasion on zirconia ceramic bonding using an adhesive composite resin. Dent Mater 26(1):44-50. [DOI] [PubMed] [Google Scholar]
- 41: Zandparsa R, Talua NA, Finkelman MD, Schaus SE. (2014). An in vitro comparison of shear bond strength of zirconia to enamel using different surface treatments. J Prosthodont 23(2):117-123. [DOI] [PubMed] [Google Scholar]
- 42: Ahrari F, Poosti M, Akbari M, Sadri K. (2012). Early versus delayed rebonding of orthodontic brackets. Prog Orthod 13(1): 17-22. [DOI] [PubMed] [Google Scholar]
- 43: Nour El-din AK, Miller BH, Griggs JA, Wakefield C. (2006). Immediate bonding to bleached enamel. Oper Dent 31(1): 106-114. [DOI] [PubMed] [Google Scholar]