Abstract
Air pollution has been an on-going research focus due to its detrimental impact on human health. However, its specific effects on asthma prevalence in different age groups, genders and races are not well understood. Thus, the present study was designed to examine the association between selected air pollutants and asthma prevalence in different population groups during 2010 in the eastern part of Texas, USA.The pollutants considered were particulate matter (PM2.5 with an aerodynamic diameter less than 2.5 micrometers) and surface ozone. The population groups were categorized based on age, gender, and race. County-wise asthma hospital discharge data for different age, gender, and racial groups were obtained from Texas Asthma Control Program, Office of Surveillance, Evaluation and Research, Texas Department of State Health Services. The annual means of the air pollutants were obtained from the United States Environmental Protection Agency (U.S. EPA)’s air quality system data mart program. Pearson correlation analyzes were conducted to examine the relationship between the annual mean concentrations of pollutants and asthma discharge rates (ADR) for different age groups, genders, and races. The results reveal that there is no significant association or relationship between ADR and exposure of air pollutants (PM2.5, and O3). The study results showed a positive correlation between PM2.5 and ADR and a negative correlation between ADR and ozone in most of the cases. These correlations were not statistically significant, and can be better explained by considering the local weather conditions. The research findings facilitate identification of hotspots for controlling the most affected populations from further environmental exposure to air pollution, and for preventing or reducing the health impacts.
Keywords: air pollution, asthma, age, gender, race, Texas, USA
1. Introduction
Air pollution is one of the major environmental threats to urban populations [1]. It can be traced back to the industrialization-urbanization era started in the 19th century. Air pollution has been reported to cause adverse health impacts on people of all races, ages, and genders in every country including the USA. The past studies revealed that exposure to air pollution has more serious health effects such as reduced life expectancy, increased daily mortality and hospital admissions, birth outcomes, and asthma [2] than previously thought. Künzli et al. estimated that 40,000 deaths annually or 6% of total mortality amongst adults aged 30+years were due to ambient air pollution in Austria, Switzerland, and France [3]. In another study, Valent et al., reported that some 13,000 deaths annually of infants (ages 0–4) were attributed to outdoor air pollution [4], making it a second environmental burden of disease only to physical injuries across Europe. Over the last two decades, many epidemiologic studies have confirmed the positive association between air pollution and mortality [5,6,7,8,9,10]. To analyze these effects, air pollution epidemiology studies with useful assessment techniques have been implemented to detect the small increase in risk due to increase in the background pollution level. Additionally, the studies have consistently showed that exposure to common air pollutants is linked to many adverse health outcomes including respiratory (chronic obstructive pulmonary disease), asthma, and lung cancer [11,12,13,14,15,16] and cardiovascular diseases [12,17,18,19,20,21].
Airborne pollutants influence the symptoms of asthma in patients [22,23,24]. Asthma is a burden, not only in developing countries, but also in developed countries, with significant impacts on public health and economics. As per the 2011 National Health Survey Data of United States, asthma is identified as one of the most prevalent chronic diseases among U.S. children. A total of 10.5 million (14%) U.S. children have been diagnosed with asthma [25]. Asthma is a serious and sometimes life-threatening chronic respiratory disease that affects almost 25 million Americans and costs the nation $56 billion per year [26]. In 2009, 3.3 deaths per 100,000 people were attributed to asthma, and 1.9 million asthma-related emergency department visits were recorded [27,28]. Asthma prevalence increased from 7.3% in 2001 to 8.4% in 2010 [29]. It was also revealed that children may be more susceptible to ambient air pollution than adults [30,31], and are disproportionately affected by asthma, as evidenced by higher asthma hospitalization rates for persons under age 18 [32]. These adverse health outcomes have been shown to be similar in both economically developing and developed countries [33].
Many specific epidemiologic studies have found that short-term exposure of ozone leads to adverse health effects ranging from mild respiratory function impairment to increased mortality [10,34,35,36,37]. It is also confirmed in many studies that short-term ambient ozone exposures increases the asthma emergency department (ED) visits [38,39,40,41,42] and hospitalizations [43,44,45], particularly during the warm season when ozone concentrations are higher [46,47]. Further, many epidemiologic studies have been conducted on the association between exposure to ozone with asthma exacerbations in children [48,49,50,51], but results have not always been consistent. Thus, many questions regarding the effects of air pollution remain unanswered, and overall, these effects have not been adequately quantified. Furthermore, the differences in health effects due to air pollution exposure on different races, age groups, and genders are not properly established. In various studies, results have varied widely, particularly for effects between racial groups, genders, and age groups. According to Zeka et al., the impacts of air pollution was similar among races while others found significant differences for Whites and Hispanics [52], but not African Americans [53], or for African Americans but not for other races or ethnic groups [54]. Few other researchers have found the greater risk for African Americans from air pollution [55]. The evidence of significant adverse effects of air pollution on public health has led to more stringent air quality norms in many countries including the USA.
Though, current research indicates relationship between social-demographic characteristics (e.g., age, race, etc.) and disease [56], the underlying reasons for disparities in disease have not fully elucidated. Additionally, it is known that asthma attacks are triggered by multiple criteria pollutants, namely particulate matter (PM), ozone (O3), sulfur dioxide (SO2), nitrogen dioxide (NO2), and carbon monoxide (CO) [18,20,57,58,59]. However, the specific effects of these air pollutants on asthma prevalence in different age groups, genders, and races are not well understood. Thus, the aim of the present study was to examine the association between selected air pollutants (PM2.5 and ground-level ozone), and asthma prevalence in different population groups (based on age, gender, and race) residing in eastern part of Texas, USA using geospatial techniques.Due to an insufficient number of spatial data on other criteria air pollutants monitored in the region, the present study focused only on PM2.5 and ground-level ozone.
2. Study Area
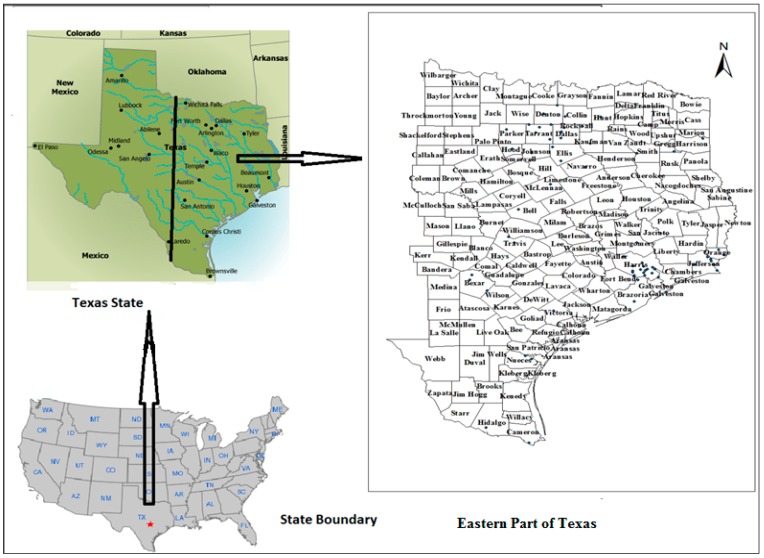
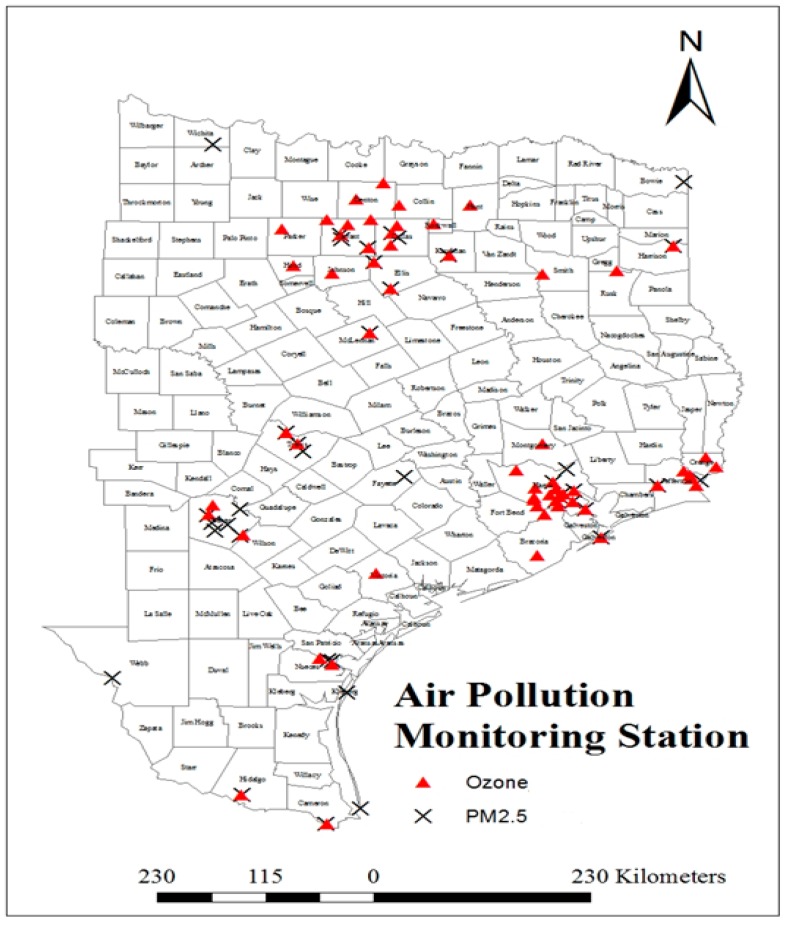
The eastern part of Texas State, USA (shown in the Figure 1) was selected for the proposed study. Due to the inexistence of a sufficient number of air pollution monitoring stations in the western part of the state, only eastern part was considered for the study. Texas State is located in the west-south-central region of the United States. The extent of longitude and latitude of the state are 93°31′ W to 106°38′ W and 25°50′ N to 36°30′ N, respectively. Texas is the second most populous (25,145,561), and 29th most densely populated (37.2 inhabitants per square kilometer of land area) state of the 50 United States [60]. Texas covers 696,241 square kilometers of land area and ranks as the 2nd state by size [61]. In general, the climate in Texas varies widely, from arid in the west tohumidin the east. There is significant variation in the geography from one region to another of the state. There are coastal regions, mountains, deserts and wide-open plains. In coastal regions, the weather is neither particularly hot in the summer nor particularly cold during the winter. East Texas has a humid subtropical climate typical of the southeast, occasionally interrupted by intrusions of cold air from the north.
Figure 1.
Study area map.
3. Data
3.1. Asthma Data
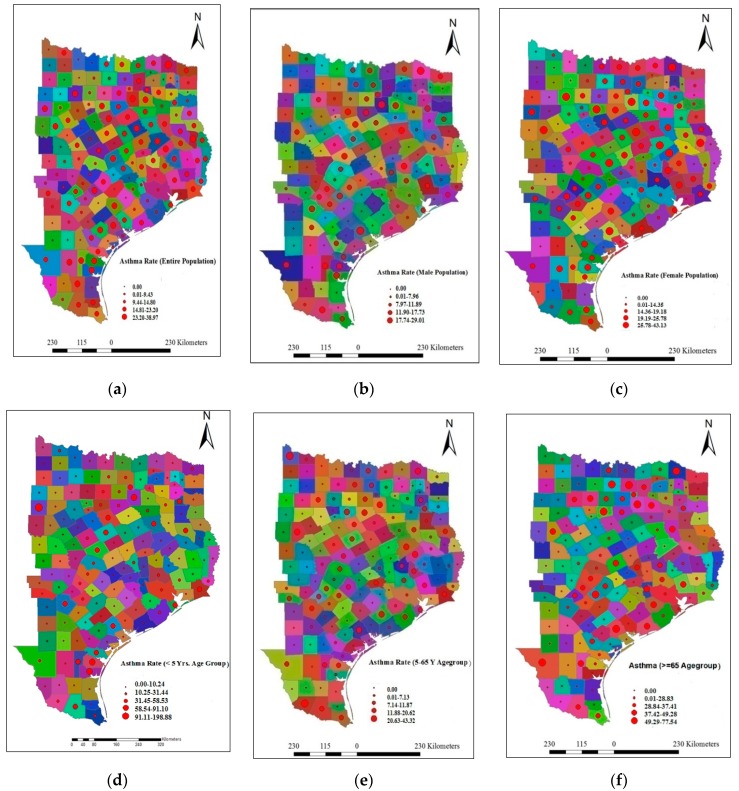
The proposed study conducted using a full year of asthma data from January 2010 to December 2010. The asthma hospital discharge numbers for different population groups (age-wise, gender-wise, and race-wise) were obtained through a personal request to Texas Asthma Control Program, Office of Surveillance, Evaluation and Research, Texas Department of State Health Services [62]. The asthma hospital discharge numbers were diagnosed as per the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code 493 [63]. The county-wise estimated population data were also obtained from the same office for determining the asthma rate. Asthma discharge rate (ADR) represents the number of asthma-related hospital discharges per 10,000 people for a specified period. The counties with less than 12 asthma hospital discharge cases were not reported and, thus the asthma discharge rate was considered to be zero. The county-wise asthma rate for different races (Black, White, Hispanic), age groups (<5 year, 5–65 year, and >65 year), and genders (Male, and Female) are represented in Figure 2. The reason for selecting these age groups was based on the availability of asthma data that were collected by the Texas Department of State Health Services according to these age groups.
Figure 2.
County-wise asthma rates in eastern part of Texas State (a) Entire Population; (b) Male Population; (c) Female Population; (d) <5 Year Age Group; (e) 5–65 Year Age Group; (f) >65 Age Group; (g) White Population; (h) Black Population; (i) Hispanic Population.
The data shown in Figure 2 indicate that the maximum ADR for entire population group was 38.97; whereas, the ADR values for the male and female population groups were 29.01 and 43.13 respectively in 2010. The ADR values for the three age groups (<5 year, 5–65 year, and >65 year) were 198.88, 43.32, and 77.54, respectively. Similarly, the ADR values for White, Black, and Hispanic population group were recorded as 35.81, 285.01, and 51.78, respectively. Thus, the data clearly indicate that the asthma rate was higher for the female population group in comparison to the male population group. Similarly, age-wise asthma rate indicate that children are more affected than the middle-aged and older population groups. Additionally, the data confirms that Hispanic population group are more vulnerable than the White and Black population groups.
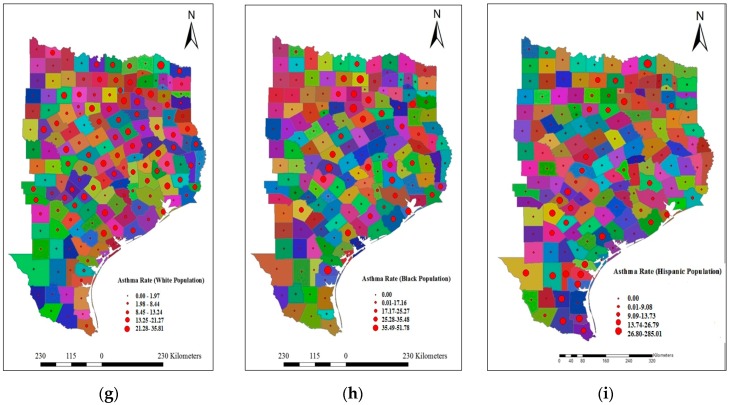
The quarterly asthma discharge rate data were also calculated for seasonal study. The entire year was divided into four quarters (first quarter (Q1): January to March; second quarter (Q2): April to June; third quarter (Q3): July to September; and fourth quarter: October to December). The reason for selecting the quarters for this study was based on the fact that the asthma data was available on quarterly basis. The maximum ADR of different races (Black, White, Hispanic), age groups (<5 year, 5–65 year, and >65 year), and gender (Male, and Female) in different quarters of 2010 are represented in Figure 3. It clearly indicates that the ADR was found to be relatively high in the first quarter (Q1) for most of the groups. The ADR was found to be lowest in the third quarter (Q3) for most of the groups except the Hispanic population group. The descriptive statistics of quarterly average ADR are presented in Table 1.
Figure 3.
Quarterly maximum asthma discharge rate (ADR) in different groups.
Table 1.
Descriptive statistics of pollutants and asthma discharge rate in four quarters.
| Items | Minimum | Maximum | Mean | Standard Deviation | Minimum | Maximum | Mean | Standard Deviation |
|---|---|---|---|---|---|---|---|---|
| First Quarter of 2010 (Q1) | Second Quarter of 2010 (Q2) | |||||||
| ADR * | 0 | 10.89 | 1.92 | 2.40 | 0 | 10.11 | 1.21 | 1.80 |
| PM2.5 ** | 5.5 | 11.7 | 8.3 | 1.42 | 6.8 | 13.2 | 10.5 | 1.30 |
| Ozone *** | 30.2 | 42.5 | 37.0 | 2.64 | 33.3 | 49.7 | 42.2 | 3.85 |
| Third Quarter of 2010 (Q3) | Fourth Quarter of 2010 (Q4) | |||||||
| ADR | 0 | 5.46 | 0.75 | 1.27 | 0 | 10.89 | 1.35 | 1.97 |
| PM2.5 | 8.7 | 14.6 | 11.0 | 1.24 | 6.1 | 11.3 | 9.1 | 1.26 |
| Ozone | 25.8 | 49.8 | 38.4 | 5.50 | 31.9 | 42.8 | 38.3 | 2.28 |
* ADR is number of asthma-related hospital discharges per 10,000 populations for a specified period of time; ** PM2.5 values represented in µg/m3; *** Ozone values represented in ppb.
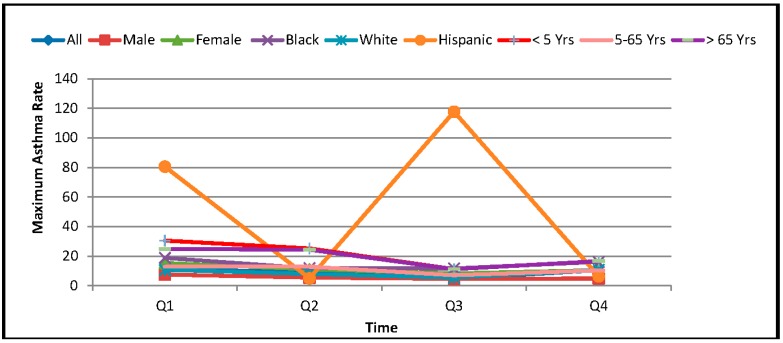
3.2. Air Pollution Data
The present study used the concentrations of two criteria air pollutant parameters (PM2.5, and O3) for the analyses. Air pollution data routinely collected by U.S. EPA’s Air Quality System (AQS) at 99 U.S. EPA administered monitoring stations (forty for PM2.5, and fifty-nine for Ozone) located in different counties of the eastern part of Texas for the year 2010 were used for the study. The air pollution data used in this study were taken from the United States Environmental Protection Agency (U.S. EPA) air quality system data mart [64]. The spatial locations of monitoring stations are represented in Figure 4. The characteristics of the raw data collected from the website are daily average (24 h) concentrations of PM2.5, and daily maximum 8 hours average concentrations of ozone. The daily data for each monitoring station were used for determination of quarterly average and annual average concentrations.
Figure 4.
Air pollution monitoring stations in Eastern part of Taxas State.
3.2.1. Statistical Analyses of Air Pollution Data
The descriptive spatial statistics of the two pollutants (PM2.5 and Ozone) are represented in Table 1. In 2010, the minimum quarterly average concentrations of PM2.5 in four quarters were 5.5 μg/m3, 6.8 μg/m3, 8.7 μg/m3, and 6.1 μg/m3, respectively. In each quarter, the minimum values were observed in the Wichita County except in the third quarter. In the third quarter, the minimum quarterly average concentration was observed in Fayette County. In the same duration, the maximum quarterly average concentrations of PM2.5 were 11.7 μg/m3, 13.2 μg/m3, 14.6 μg/m3, and 11.3 μg/m3, respectively in 1st, 2nd, 3rd, and 4th quarters. The maximum values were observed in the Harris County in each quarter except the third one. In the third quarter, the maximum concentration was observed in Bowie County.The means of the quarterly average concentrations in four quarters of 2010 were found to be 8.3 μg/m3, 10.5 μg/m3, 11 μg/m3, and 9.1 μg/m3, respectively.
Similarly, in the year 2010, the minimum quarterly average concentrations of ozone in four quarters were 30.2 ppb, 33.3 ppb, 25.8 ppb, and 31.9 ppb. These values were observed in the counties of Harris, Hidalgo, Cameron and Harris respectively in 1st, 2nd, 3rd, and 4th quarters.The maximums of quarterly average concentrations of O3 in four quarters of 2010 were 42.5 ppb, 49.7 ppb, 49.8 ppb, and 42.8 ppb, respectively. These values were observed in the counties of Orange, Denton, Denton, and Smith respectively in 1st, 2nd, 3rd, and 4th quarters.The mean spatial concentrations in four quarters of 2010 were 37 ppb, 42.2 ppb, 38.4 ppb, and 38.3 ppb, respectively.
The quarterly average data clearly indicate that the mean PM2.5 concentration level was highest in third quarter. The mean concentration level of PM2.5 was found to be slightly higher than the mean concentration of PM2.5 in the second quarter, and was significantly higher than the mean PM2.5 concentrations in first and fourth quarters. Similarly, the mean ozone concentration level was found to be highest in the second quarter.
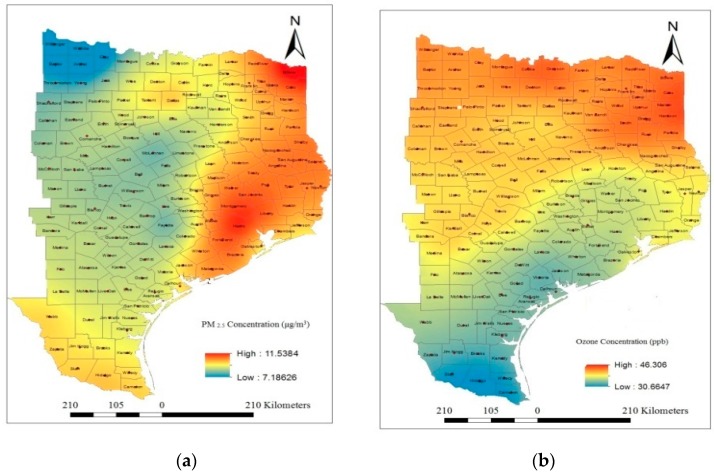
3.2.2. Spatial Analysis of Air Pollution Data
The spatial locations of each of the selected monitoring stations along with the pollutant concentrations were fed into the GIS system. Interpolation of air pollution data between monitoring stations can be done using geostatistical techniques, such as kriging in its various forms [65] rather than using more complex and empirically based models. Though, there are various types of kriging techniques (ordinary kriging, simple kriging, indicator kriging, universal kriging, and co-kriging) for spatial mapping, the present study used ordinary kriging method for spatial analysis of PM2.5 and ozone concentration. The software used for the analysis is Geostatistical Analyst Extension module of ArcGIS version 10.2 [66]. In ordinary kriging interpolation method, a smooth surface is estimated from irregularly spaced data points based on the assumptions that the spatial variation in the feature (O3, and PM2.5) is homogeneous over the study area. The method interpolates the point data obtained for various monitoring stations in the study area to predict the concentration in each grid cell over a spatial domain. Figure 5a,b depicts the spatial patterns of annual average concentrations of PM2.5 and O3, respectively, during 2010. A stable type variogram model was used for the prediction of air pollution concentrations at the un-sampled location. The cross-validation results of the model predictions are shown in Table 2. For the cross validation test, the values of mean error (ME), root mean square error (RMSE), average standard error (ASR), mean square error (MSE), and root mean square standardized error (RMSSE) estimated to ascertain the performance of the developed models. A detailed description of the model is provided in the “Geostatistics for Environmental Scientists” book [67].
Figure 5.
Spatial distribution of air pollutants (a) PM2.5; (b) O3.
Table 2.
Prediction Errors of Variogram Model.
| Parameter | Type of Variogram Model | ME | RMSE | ASE | MSE | RMSSE |
|---|---|---|---|---|---|---|
| PM2.5 | Stable | 0.099 | 0.75 | 0.85 | 0.06 | 0.88 |
| Ozone | Stable | −0.090 | 1.40 | 1.63 | −0.03 | 0.99 |
ME: Mean Error; RMS: Root Mean Square Error; ASE: Average Standard Error; MSE: Mean Standard Error; RMSSE: Root Mean Square Standardized Error.
4. Results and Discussion
In recent years, geospatial technology has become increasingly popular in environmental studies. It helps to estimate the individual air pollution via interpolation, and thus minimizing the chances of ecological bias characterized to information loss because of a real data aggregation [68,69,70,71,72,73]. It also helps in deriving the association between the multivariate data. Since the last decade, GIS-based pollution mapping using various interpolation techniques (inverse distance weighted, kriging, and land use regression modeling) has been explored by many researchers for epidemiological studies [74,75,76,77]. Most of the researchers have interpolated mainly the criteria pollutants like PM2.5, ozone, SO2, and NO2 for spatial mapping to determine the exposure level. Asthma data collected from all around the world indicate an increasing trend of asthma morbidity and mortality despite the availability of effective symptomatic treatment. Thus, the problem of asthma has drawn much attention globally. The literature shows that most of the researchers used time-series analyses [41,42,46,78,79,80,81,82,83,84,85,86,87,88,89,90] for understanding the association between air quality and asthma prevalence rather geospatial techniques [74,75,76,77]. In the present study, we demonstrate the application of GIS for analyzing the association between air pollution exposure and ADR, and to visualize major threat areas in the form of maps. The spatial data of two pollutants (PM2.5 and ozone) and asthma discharge rate (ADR) in the selected study area were analyzed to understand the association between air pollution and ADR. The association between air pollution exposure and ADR was quantified using the correlation analyses. These are explained in the next section.
Correlation Analyses
Cross Correlation Analyses
The study sought to investigate the association between air pollution exposure and asthma rate for different races (Black, White, and Hispanic), age groups (<5 years, 5–65 years, and >65 years), and genders (Male and Female). Pearson correlation analyses were carried out using the point data represented at the centroid point of each county to understand the association. The concentrations of PM2.5 and O3 at the centroid point of each county were extracted from the spatial maps as shown in Figure 5a,b respectively. These data were further used in correlation analyses between air pollution level and ADR for different population groups. The ADR at the centroid point of each county is considered to be the same as determined for the individual county.Since, the total numbers of counties in the study area are 157; the numbers of point data derived for the correlation analysis are also 157. The Pearson two-tailed correlation analyses were carried out using SPSS software version 21. The cross-correlation analyses results are presented in Table 3 and indicate that there is a significant variation in correlation coefficient between air pollutants with different populations groups. Though, the results showed a positive association between PM2.5 and ADR in each case; the correlations were not statistically significant in most of the cases. Ozone levels showed a negative correlation with asthma rate in most cases. The results also clearly indicate that PM2.5 is negatively correlated with the ozone concentration, and hence, it is bound to show a reverse correlation coefficient of ADR with PM2.5 and ozone. That is, the result does not mean that ozone concentration reduces the asthma cases. It rather shows that the asthma prevalence is mainly dominated by PM2.5 concentrations in the study area.
Table 3.
Correlation analysesresults of annual average data.
| Items | Pearson Correlations Coefficients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PM2.5 | Ozone | AR_All | AR_Black | AR_White | AR_Hispanic | AR_Male | AR_Female | AR_LT_5Y | AR_5–65Y | AR_GT_65Y | |
| PM2.5 | 1 | ||||||||||
| Ozone | −0.100 | 1 | |||||||||
| AR_All | 0.244 ** | −0.095 | 1 | ||||||||
| AR_Black | 0.148 | 0.082 | 0.214 ** | 1 | |||||||
| AR_White | 0.181 * | 0.222 ** | 0.733 ** | 0.258 ** | 1 | ||||||
| AR_Hispanic | 0.039 | −0.003 | 0.134 | 0.065 | −0.061 | 1 | |||||
| AR_Male | 0.156 | −0.007 | 0.617 ** | 0.477 ** | 0.562 ** | 0.210 ** | 1 | ||||
| AR_Female | 0.205 ** | 0.003 | 0.858 ** | 0.306 ** | 0.767 ** | 0.122 | 0.655 ** | 1 | |||
| AR_LT_5Y | 0.086 | −0.037 | 0.048 | 0.132 | −0.021 | 0.018 | 0.149 | 0.066 | 1 | ||
| AR_5-65Y | 0.111 | −0.081 | 0.399 ** | 0.361 ** | 0.401 ** | 0.038 | 0.550 ** | 0.497 ** | 0.074 | 1 | |
| AR_GT_65Y | 0.130 | −0.022 | 0.499 ** | 0.482 ** | 0.529 ** | 0.157 * | 0.755 ** | 0.624 ** | 0.071 | 0.461 ** | 1 |
Note: AR_All—Asthma rate for entire population group; AR_Black—Asthma rate for Black population group; AR_White—Asthma rate for White population group; AR_Hispanic—Asthma rate for Hispanic population group; AR_Male—Asthma rate for Male population group; AR_Female—Asthma rate for Female population group; AR_LT_5Y—Asthma rate for less than 5 years agegroup population; AR_LT_5–65Y—Asthma rate for 5–65 years age group population; AR_GT_65Y—Asthma rate for less greater than 65 years age group population; ** Correlation is significant at the 0.01 level (2-tailed); * Correlation is significant at the 0.05 level (2-tailed).
The study also investigated the association between air pollution exposure level and ADR on a quarterly basis to understand the seasonal effects. The results are represented in Table 4. The results reveal that there is no significant association or relationship between ADR and exposure of air pollutants (PM2.5, and O3). Though, the results showed a positive correlation between PM2.5 and ADR and a negative correlation between ADR and ozone in most of the cases. These correlations were not statistically significant, and can be better explained after considering the local weather conditions.
Table 4.
Correlation analyses results of quarterly data.
| Items | First Quarter (Q1) | Second Quarter (Q2) | Third Quarter (Q3) | Fourth Quarter (Q4) | ||||
|---|---|---|---|---|---|---|---|---|
| PM2.5 | Ozone | PM2.5 | Ozone | PM2.5 | Ozone | PM2.5 | Ozone | |
| AR_All | 0.104 | 0.099 | 0.125 | 0.057 | 0.116 | −0.009 | 0.053 | 0.108 |
| AR_Black | 0.012 | 0.073 | 0.142 | −0.023 | 0.054 | −0.135 | 0.032 | 0.026 |
| AR_White | 0.108 | 0.063 | 0.083 | 0.031 | 0.041 | 0.001 | 0.039 | 0.063 |
| AR_Hispanic | 0.177 * | −0.042 | 0.014 | 0.151 | 0.147 | 0.119 | 0.004 | 0.018 |
| AR_Male | 0.050 | −0.027 | 0.038 | 0.137 | 0.088 | 0.033 | −0.045 | −0.072 |
| AR_Female | 0.031 | 0.001 | 0.146 | −0.253 ** | 0.075 | 0.072 | 0.090 | 0.092 |
| AR_LT_5Y | −0.051 | 0.086 | 0.070 | −0.063 | −0.021 | −0.103 | 0.004 | 0.041 |
| AR_5–65Y | −0.055 | −0.054 | 0.157 | −0.162 * | 0.004 | −0.144 | 0.173 * | −0.109 |
| AR_GT_65Y | 0.077 | −0.012 | 0.115 | −0.027 | 0.024 | −0.088 | 0.104 | −0.120 |
** Correlation is significant at the 0.01 level (2-tailed); * Correlation is significant at the 0.05 level (2-tailed).
Autocorrelation Analyses
Autocorrelation analyses were carried out to investigate the spatial association between quarterly averages of ADR in different population groups, and conducted in similar ways as cross-correlation analyses. The correlation results for different population groups are presented in Table 5. The correlation analyses results for asthma discharge rate (ADR) clearly indicate that the correlation coefficients among different quarters are statistically significant at 1 percent significance level for each group except Hispanic population. This indicates that the occurrences of asthma cases in different seasons for each group except Hispanic are spatially consistent in nature.
Table 5.
Autocorrelation analyses results.
| Entire Population Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||||||
| Q1 | 1 | ||||||||
| Q2 | 0.684 ** | 1 | |||||||
| Q3 | 0.568 ** | 0.606 ** | 1 | ||||||
| Q4 | 0.657 ** | 0.781 ** | 0.503 ** | 1 | |||||
| Female Population Group | Male Population Group | ||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Q1 | 1 | Q1 | 1 | ||||||
| Q2 | 0.587 ** | 1 | Q2 | 0.773 ** | 1 | ||||
| Q3 | 0.622 ** | 0.742 ** | 1 | Q3 | 0.707 ** | 0.775 ** | 1 | ||
| Q4 | 0.547 ** | 0.610 ** | 0.591 ** | 1 | Q4 | 0.755 ** | 0.713 ** | 0.749 ** | 1 |
| Black Population Group | White Population Group | ||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Q1 | 1 | Q1 | 1 | ||||||
| Q2 | 0.678 ** | 1 | Q2 | 0.613 ** | 1 | ||||
| Q3 | 0.674 ** | 0.667 ** | 1 | Q3 | 0.583 ** | 0.749 ** | 1 | ||
| Q4 | 0.921 ** | 0.722 ** | 0.757 ** | 1 | Q4 | 0.701 ** | 0.489 ** | 0.435 ** | 1 |
| Hispanic Population Group | <5 Years Age Group | ||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Q1 | 1 | Q1 | 1 | ||||||
| Q2 | 0.155 | 1 | Q2 | 0.804 ** | 1 | ||||
| Q3 | 0.968 ** | 0.034 | 1 | Q3 | 0.662 ** | 0.636 ** | 1 | ||
| Q4 | 0.186 * | 0.701 ** | 0.044 | 1 | Q4 | 0.753 ** | 0.620 ** | 0.752 ** | 1 |
| 5–65 Years Age Group | ≥ 65 Years Age Group | ||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Q1 | 1 | Q1 | 1 | ||||||
| Q2 | 0.685 ** | 1 | Q2 | 0.587 ** | 1 | ||||
| Q3 | 0.643 ** | 0.879 ** | 1 | Q3 | 0.714 ** | 0.763 ** | 1 | ||
| Q4 | 0.614 ** | 0.805 ** | 0.815 ** | 1 | Q4 | 0.773 ** | 0.725 ** | 0.837 ** | 1 |
** Correlation is significant at the 0.01 level (2-tailed); * Correlation is significant at the 0.05 level (2-tailed).
5. Limitations of the Study
Although the GIS technology facilitated the research implementation faster and easier, lack of spatial detail and spatial consistency between data sets impeded their full utility. For better and more conclusive results, GIS-based studies need the availability of uniformly distributed pollution and health data. Some data problems and data limitations are encountered with the integration of health data in GIS. Primarily, the interpolation analyses give better pollution level prediction for uniformly distributed spatial data in the study area. However, the pollution monitoring stations in Texas State was not uniformly distributed, and this may lead to some errors in prediction level. Furthermore, there is no state-wide reporting on asthma and, therefore, no centralized asthma database. People suffering from asthma may be seen by a private doctor or may not be seen by any health care provider. This type of cases may not be listed in the asthma database. Again, counties with less than 12 asthma cases are not reported. In addition to above, the asthma data available does not consider the movement of people from one county to another. This study used annual and quarterly average level of pollutants at a particular location as the population's exposure level, but the workplace may not be located in the same county, and this could be biased about an individual’s exposure estimation, which could influence the results. The present study explores the associationsbetween air pollution (PM2.5 and ozone)and does not determine causality. There are many environmental variables, including air pollution and some meteorological variables which can influence the prevalence or incidence rate of asthma. Thus, there is a future need for an integrated assessment to evaluate the combined effects of air pollutants and climatic factors on disease rates.
6. Conclusions
The study results indicated significant variations in the correlation coefficients between asthma rate and air pollution exposure among different age groups, genders, and races in the residents of East Texas, USA. Furthermore, PM2.5 always showed a positive effect in triggering the asthma rate, whereas, the association between ozone and asthma rate did not show a uniform trend. This finding does not mean that ozone reduces the asthma cases, but can be better explained by the fact that asthma prevalence is mainly dominated by PM2.5 concentrations in the study area. Auto-correlation results indicated that the occurrences of asthma cases in different seasons for each group except Hispanics, were spatially consistent in nature.That is, few hotspots exist in the study area, where asthma prevalence is more frequent irrespective of seasons. Thus, steps should be taken to protect the most affected populations from further environmental exposure to air pollution, and to control, prevent or reduce the health impacts.
Acknowledgments
Authors are thankful to U.S. EPA for providing the air pollution data available on the website for public use, and to Texas Department of State Health Services for providing the quarterly county wise asthma data. The supports from the Department of Science and Technology, New Delhi Grant No. SR/FTP/17/2012 and National Institutes of Health (NIMHD-RCMI Grant No. G12MD007581) are also acknowledged.
Author Contributions
Amit K. Gorai led the design of the study and analysis of results, and drafted the manuscript. Francis Tuluri helped in preparing the draft of the manuscript. Paul B. Tchounwou provided the critical comments on the draft manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Cohen A.J., Anderson H.R., Ostra B., Dev Pandey K., Krzyzanowski M., Kunzli N., Guschmidt K., Pope A., Romieu I., Samet J.M., et al. The Global burden of disease due to outdoor air pollution. J. Toxicol. Environ. Health A. 2005;68:1–7. doi: 10.1080/15287390590936166. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Study 2010. [(accessed on 18 December 2015)]. Available online: http://www. thelancet.com/themed/global-burden-of-disease.
- 3.Künzli N., Kaiser R., Medina S., Studnicka M., Chanel O., Filliger P., Herry M., Horak F., Jr., Puybonnieux-Texier V., Quénel P., et al. Public-health impact of outdoor and traffic-related air pollution: A European assessment. Lancet. 2000;356:795–801. doi: 10.1016/S0140-6736(00)02653-2. [DOI] [PubMed] [Google Scholar]
- 4.Valent F., Little D., Bertollini R., Nemer L., Barbone F., Tamburlini G. Burden of disease attributable to selected environmental factors and injury among children and adolescents in Europe. Lancet. 2003;363:2032–2039. doi: 10.1016/S0140-6736(04)16452-0. [DOI] [PubMed] [Google Scholar]
- 5.Levy J.I., Hammitt J.K., Spengler J.D. Estimating the mortality impacts of particulate matter: What can be learned from between-study variability? Environ. Health Perspect. 2000;108:109–117. doi: 10.1289/ehp.00108109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carey I.M., Atkinson R.W., Kent A.J., van Staa T., Cook D.G., Anderson H.R. Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am. J. Respir. Crit. Care Med. 2013;187:1226–1233. doi: 10.1164/rccm.201210-1758OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodman P.G., Dockery D.W., Clancy L. Cause-specific mortality and the extended effects of particulate pollution and temperature exposure. Environ. Health Perspect. 2004;112:179–185. doi: 10.1289/ehp.6451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz J. The effects of particulate air pollution on daily deaths: A multi-city case-crossover analysis. Occup. Environ. Med. 2004;61:956–961. doi: 10.1136/oem.2003.008250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Analitis A., Katsouyanni K., Dimakopoulou K., Samoli E., Nikoloulopoulos A.K., Petasakis Y., Touloumi G., Schwartz J., Anderson H.R., Cambra K., et al. Short-term effects of ambient particles on cardiovascular and respiratory mortality. Epidemiology. 2006;17:230–233. doi: 10.1097/01.ede.0000199439.57655.6b. [DOI] [PubMed] [Google Scholar]
- 10.Choi M., Curriero F.C., Johantgen M., Mills M.E., Sattler B., Lipscomb J. Association between ozone and emergency department visits: An ecological study. Int. J. Environ. Health Res. 2011;21:201–221. doi: 10.1080/09603123.2010.533366. [DOI] [PubMed] [Google Scholar]
- 11.Bild D.E., Bluemke D.A., Burke G.L., Detrano R., Diez Roux A.V., Folsom A.R., Greenland P., Jacob D.R., Jr., Kronmal R., Liu K., et al. Multi-Ethnic Study of Atherosclerosis: Objectives and design. Am. J. Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 12.Chen H., Goldberg M.S., Villeneuve P.J. A systematic review of the relation between long-term exposure to ambient air pollution and chronic diseases. Rev. Environ. Health. 2008;23:243–297. doi: 10.1515/reveh.2008.23.4.243. [DOI] [PubMed] [Google Scholar]
- 13.Szpiro A.A., Sampson P.D., Lumley T., Adar S.D., Kaufman J.D. Predicting intra-urban variation in air pollution concentrations with complex spatio-temporal dependencies. Environmetrics. 2009;21:606–631. doi: 10.1002/env.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen M.A., Adar S.D., Allen R.W., Avol E., Curl C.L., Gould T., Hardie D., Ho A., Kinney P., Larson T.V., et al. Approach to estimating participant pollutant exposures in the Multi-Ethnic Study ofAtherosclerosis and Air Pollution (Mesa Air) Environ. Sci. Technol. 2009;43:4687–4693. doi: 10.1021/es8030837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sampson P.D., Szpiro A.A., Sheppard L., Lindstom J., Kaufman J.D. Pragmatic estimation of a spatio-temporal air quality model with irregular monitoring data. Atmos. Environ. 2011;45:6593–6606. doi: 10.1016/j.atmosenv.2011.04.073. [DOI] [Google Scholar]
- 16.Kaufman J.D., Adar S.D., Allen R.W., Barr R.G., Budoff M.J., Burke G.L., Casillas A.M., Cohen M.A., Curl C.L., Daviglus M.L., et al. Prospective study of particulate air pollution exposures, subclinical atherosclerosis, and clinical cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis and Air Pollution (Mesa Air) Am. J. Epidemiol. 2012;176:825–837. doi: 10.1093/aje/kws169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pope C.A., III, Burnett R.T., Thurston G.D., Thun M.J., Calle E.E., Krewski D., Godleski J.J. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109:71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Environmental Protection Agency Integrated Science Assessment for Particulate Matter. [(accessed on 13 December 2014)];2009 Dec; Available online: http://www.epa.gov/ncea/pdfs/partmatt/Dec2009/PM_ISA_full.pdf. [PubMed]
- 19.Miller K.A., Siscovick D.S., Sheppard L., Shepherd K., Sullivan J.H., Anderson G.L., Kaufman J.D. Longterm exposure to air pollution and incidence of cardiovascular events in women. New Engl. J. Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Environmental Protection Agency Air Quality Criteria for Ozone and Related Photochemical Oxidants. [(accessed on 13 December 2014)];2006 Feb; Available online: http://oaspub.epa.gov/eims/eimscomm.getfile?p_download_id=456384.
- 21.Brook R.D., Rajagopalan S., Pope C.A., III, Brook J.R., Bhatnagar A., Diez-Roux A.V., Holguin F., Hong Y., Luepker R.V., Mittleman M.A., et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 22.Delfino R.J., Coate B.D., Zeiger R.S., Seltzer J.M., Street D.H., Koutrakis P. Daily asthma severity in relation to personal ozone exposures and outdoor fungal spores. Am. J. Respir. Crit. Care Med. 1996;154:633–641. doi: 10.1164/ajrccm.154.3.8810598. [DOI] [PubMed] [Google Scholar]
- 23.Delfino R.J., Zeiger R.S., Seltzer J.M., Street D.H., Matteucci R.M., Anderson P.R., Koutrakis P. The effect of outdoor fungal spore concentrations on daily asthma severity. Environ. Health Perspect. 1997;105:622–635. doi: 10.1289/ehp.97105622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorai A.K., Tuluri F., Tchounwou P.B. A GIS based approach for assessing the Association between Air Pollution and Asthma in New York State, USA. Int. J. Environ. Res. Publ. Health. 2014;11:4845–4869. doi: 10.3390/ijerph110504845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC National Health Interview Survey Data 2011. [(accessed on 20 October 2014)]; Available online: http://www.cdc.gov/nchs/nhis.htm.
- 26.Barnett S.B., Nurmagambetov T.A. Costs of asthma in the United States: 2002–2007. J. Allergy Clin.Immunol. 2011;127:145–152. doi: 10.1016/j.jaci.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Health Data Interactive In Center for Disease Control and Prevention and National Center for Health Statistic, Online Server. Public Reports. Mortality and Life Expectancy. Mortality by Underlying Cause, Ages 18+ 2009. 2009. [(accessed on 18 December 2015)]. Available online: http://205.207.175.93/hdi/ReportFolders/ReportFolders.aspx.
- 28.National Center for Environmental Health: Asthma’s Impacton the Nation. In Center for Disease Control and Prevention. [(accessed on 18 December 2015)];2012 Available online: http://www.cdc.gov/asthma/impacts_nation/AsthmaFactSheet.pdf.
- 29.Akinbami L.J., Moorman J.E., Bailey C., Zahran H.S., King M., Johnson C.A., Liu X. Trends in Asthma Prevalence, Health Care Use, and Mortality in the United States, 2001–2010. [(accessed on 18 December 2015)];NCHS Data Brief. 2012 94. Available online: http://www.cdc.gov/nchs/data/databriefs/db94.pdf. [PubMed]
- 30.American Academy of Pediatrics Committee on Environmental Health Ambient air pollution: Health hazards to children. Pediatrics. 2004;114:1699–1707. doi: 10.1542/peds.2004-2166. [DOI] [PubMed] [Google Scholar]
- 31.Trasande L., Thurston G.D. The role of air pollution in asthma and other pediatric morbidities. J. Allergy Clin. Immunol. 2005;115:689–699. doi: 10.1016/j.jaci.2005.01.056. [DOI] [PubMed] [Google Scholar]
- 32.Moorman J.E., Rudd R.A., Johnson C.A., King M., Minor P., Bailey C., Scalia M.R., Lara J., Akinbami L.J. National surveillance for asthma–United States, 1980–2004. MMWR Surveill. Summ. 2007;56:1–54. [PubMed] [Google Scholar]
- 33.Schwartz J., Zanobetti A. Using meta-smoothing to estimate dose-response trends across multiple studies, with application to air pollution and daily death. Epidemiology. 2000;11:666–672. doi: 10.1097/00001648-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Gold D.R., Damokosh A.I., Pope C.A., Dockery D.W., McDonnell W.F., Serrano P., Retama A., Castillejos M. Particulate and ozone pollutant effects on the respiratory function of children in southwest Mexico City. Epidemiology. 1999;10:8–16. doi: 10.1097/00001648-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Bell M.L., McDermott A., Zeger S.L., Samet J.M., Dominici F. Ozone and short-term mortality in 95 US urban communities, 1987–2000. JAMA. 2004;292:2372–2378. doi: 10.1001/jama.292.19.2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filleul L., Cassadou S., Medina S., Fabres P., Lefranc A., Eilstein D., le Tertre A., Pascal L., Chardon B., Blanchard M., et al. The relation between temperature, ozone, and mortality in nine French cities during the heat wave of 2003. Environ. Health Perspect. 2006;114:1344–1347. doi: 10.1289/ehp.8328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halonen J.I., Lanki T., Tiittanen P., Niemi J.V., Loh M., Pekkanen J. Ozone and cause-specific cardiorespiratory morbidity and mortality. J. Epidemiol. Community Health. 2010;64:814–820. doi: 10.1136/jech.2009.087106. [DOI] [PubMed] [Google Scholar]
- 38.Cassino C., Ito K., Bader I., Ciotoli C., Thurston G., Reibman J. Cigarette smoking andozone-associated emergency department use for asthma by adults in New York City. Am. J. Respir. Crit. Care Med. 1999;159:1773–1779. doi: 10.1164/ajrccm.159.6.9809042. [DOI] [PubMed] [Google Scholar]
- 39.Jaffe D.H., Singer M.E., Rimm A.A. Air pollution and emergency department visits for asthma among Ohio medicaid recipients, 1991–1996. Environ. Res. 2003;91:21–28. doi: 10.1016/S0013-9351(02)00004-X. [DOI] [PubMed] [Google Scholar]
- 40.Peel J.L., Tolbert P.E., Klein M., Metzger K.B., Flanders W.D., Todd K., Mulholland J.A., Ryan P.B., Frumkin H. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16:164–174. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- 41.Wilson A.M., Wake C.P., Kelly T., Salloway J.C. Air pollution, weather, and respiratory emergency room visits in two northern New England cities: An ecological time-series study. Environ. Res. 2005;97:312–321. doi: 10.1016/j.envres.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Stieb D.M., Szyszkowicz M., Rowe B.H., Leech J.A. Air pollution and emergency department visits for cardiac and respiratory conditions: A multi-city time-series analysis. Environ. Health. 2009;8 doi: 10.1186/1476-069X-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thurston G.D., Ito K., Hayes C.G., Bates D.V., Lippmann M. Respiratory hospital admissions and summertime haze air pollution in Toronto, Ontario: Consideration of the role of acid aerosols. Environ. Res. 1994;65:271–290. doi: 10.1006/enrs.1994.1037. [DOI] [PubMed] [Google Scholar]
- 44.Anderson W., Prescott G.J., Packham S., Mullins J., Brookes M., Seaton A. Asthma admissions and thunderstorms: A study of pollen, fungal spores, rainfall, and ozone. QJM. 2001;94:429–433. doi: 10.1093/qjmed/94.8.429. [DOI] [PubMed] [Google Scholar]
- 45.Lee J.T., Cho Y.S., Son J.Y. Relationship between ambient ozone concentrations and daily hospital admissions for childhood asthma/atopic dermatitis in two cities of Korea during 2004–2005. Int. J. Environ. Health Res. 2010;20:1–11. doi: 10.1080/09603120903254033. [DOI] [PubMed] [Google Scholar]
- 46.Ito K., Thurston G.D., Silverman R.A. Characterization of PM2.5, gaseous pollutants, and meteorological interactions in the context of time-series health effects models. J. Expo. Sci. Environ. Epidemiol. 2007;17(Suppl. 2):S45–S60. doi: 10.1038/sj.jes.7500627. [DOI] [PubMed] [Google Scholar]
- 47.Strickland M.J., Darrow L.A., Klein M., Flanders W.D., Sarnat J.A., Waller L.A., Sarnat S.E., Mulholland J.A., Tolbert P.E. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am. J. Respir. Crit. Care Med. 2010;182:307–316. doi: 10.1164/rccm.200908-1201OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akinbami L.J., Lynch C.D., Parker J.D., Woodruff T.J. The association between childhood asthma prevalence and monitored air pollutants in metropolitan areas, United States, 2001–2004. Environ. Res. 2010;110:294–301. doi: 10.1016/j.envres.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 49.Silverman R.A., Ito K. Age-related association of fine particles and ozone with severe acute asthma in New York City. J. Allergy Clin. Immunol. 2010;125:367–373. doi: 10.1016/j.jaci.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 50.Dong G.H., Chen T., Liu M.M., Wang D., Ma Y.N., Ren W.H., Lee Y.L., Zhao Y.D., He Q.C. Gender differences and effect of air pollution on asthma in children with and without allergic predisposition: Northeast Chinese children health study. PLoS ONE. 2011;6 doi: 10.1371/journal.pone.0022470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Samoli E., Nastos P.T., Paliatsos A.G., Katsouyanni K., Priftis K.N. Acute effects of air pollution on pediatric asthma exacerbation: Evidence of association and effect modification. Environ. Res. 2011;111:418–424. doi: 10.1016/j.envres.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 52.Zeka A., Zanobetti A., Schwartz J. Individual-level modifiers of the effects of particulate matter on daily mortality. Am. J. Epidemiol. 2006;163:849–859. doi: 10.1093/aje/kwj116. [DOI] [PubMed] [Google Scholar]
- 53.Ostro B., Feng W.Y., Broadwin R., Malig B., Green S., Lipsett M. The impact of components of fine particulate matter on cardiovascular mortality in susceptible subpopulations. Occup. Environ. Med. 2008;65:750–756. doi: 10.1136/oem.2007.036673. [DOI] [PubMed] [Google Scholar]
- 54.Bell M.L., Dominici F. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US Communities. Am. J. Epidemiol. 2008;167:986–997. doi: 10.1093/aje/kwm396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Apelberg B.J., Buckley T.J., White R.H. Socioeconomic and racial disparities in cancer risk from air toxics in Maryland. Environ. Health Perspect. 2005;113:693–699. doi: 10.1289/ehp.7609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tian J., Wilson J.G., Zhan F.B. Female breast cancer mortality clusters within racial groups in the United States. Health Place. 2010;16:209–218. doi: 10.1016/j.healthplace.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 57.U.S. Environmental Protection Agency, 2007 Integrated Review Plan for the Primary National Ambient Air Quality Standard for Nitrogen Dioxide. [(accessed on 18 December 2015)]; Available online: http://www.epa.gov/ttn/naaqs/standards/nox/data/20070823_nox_review_plan_final.pdf.
- 58.U.S. Environmental Protection Agency, 2012 U.S. Federal Register: Secondary National Ambient Air Quality Standards for Oxides of Nitrogen and Sulfur. [(accessed on 18 December 2015)]; Available online: http://www.gpo.gov/fdsys/pkg/FR-2012-04-03/pdf/2012-7679.pdf.
- 59.Schildcrout J.S., Sheppard L., Lumley T., Slaughter J.C., Koenig J.Q., Shapiro G.G. Ambient air pollution and asthma exacerbations in children: An eight city analysis. Am. J. Epidemiol. 2006;64:505–517. doi: 10.1093/aje/kwj225. [DOI] [PubMed] [Google Scholar]
- 60.U.S. Census Bureau, Resident Population Data—2010 Census. [(accessed on 13 December 2013)]; Available online: http://www.census.gov/2010census/
- 61.U.S. Census Bureau, State Area Measurement. [(accessed on 13 December 2013)]; Available online: http://www.census.gov/geo/reference/state-area.html.
- 62.Texas State Department of Health, Public Health Information Group National Asthma Survey Report Data Obtained through Personal Request on March 2015
- 63.International Classification of Diseases (Ninth Revision, Clinical Modification) Department of Health and Human Services, Public Health Service, U.S.; Washington, DC, USA: 1988. [Google Scholar]
- 64.U.S. Environmental Protection Agency, Technology Transfer Network (TTN) Air Quality System (AQS) Data Mart. [(accessed on 15 December 2013)]; Available online: http://www.epa.gov/airdata/ad_rep_mon.html/
- 65.Oliver M.A., Webster R. Kriging: A method of interpolation for geographical information science. Int. J. Geogr. Inf. Sci. 1990;4:313–332. doi: 10.1080/02693799008941549. [DOI] [Google Scholar]
- 66.ESRI . Geostatistical Analyst Extension. ESRI Inc.; Redlands, CA, USA: 2001. Using analytic tools when generating surfaces. [Google Scholar]
- 67.Webster R., Oliver M.A. Geostatistics for Environmental Scientists (Statistics in Practice) John Wiley & Sons Ltd.; Chichester, UK: 2007. [Google Scholar]
- 68.Elliott P., Wartenberg D. Spatial epidemiology: Current approaches and future challenges. Environ. Health Persp. 2004;112:998–1006. doi: 10.1289/ehp.6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nuckols J.R., Ward M.H., Jarup L. Using geographic information systems for exposure assessment in environmental epidemiology studies. Environ. Health Persp. 2004;112:1007–1015. doi: 10.1289/ehp.6738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brauer M., Hoek G., van Vliet P., Meliefste K., Fischer P., Gehring U., Heinrich J., Cyrys J., Bellander T., Lewne M., et al. Estimating long-term average particulate air pollution concentrations: Application of traffic indicators and geographic information systems. Epidemiology. 2003;14:228–239. doi: 10.1097/01.EDE.0000041910.49046.9B. [DOI] [PubMed] [Google Scholar]
- 71.Cockings S., Dunn C.E., Bhopal R.S., Walker D.R. Users’ perspectives on epidemiological, GIS and point pattern approaches to analyzing environment and health data. Health Place. 2004;10:169–182. doi: 10.1016/j.healthplace.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 72.Gotway C., Young L.J. Combining incompatible spatial data. J. Am. Stat. Assoc. 2002;97:632–647. doi: 10.1198/016214502760047140. [DOI] [Google Scholar]
- 73.Scoggins A., Kjellstrom T., Fisher G., Connor J., Gimson N. Spatial analysis of annual air pollution exposure and mortality. Sci. Total Environ. 2004;321:71–85. doi: 10.1016/j.scitotenv.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 74.Jerrett M., Burnett R.T., Ma R., Pope C.A., 3rd, Krewski D., Newbold K.B., Thurston G., Shi Y., Finkelstein N., Calle E.E., et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology. 2005;16:727–736. doi: 10.1097/01.ede.0000181630.15826.7d. [DOI] [PubMed] [Google Scholar]
- 75.Gorai A.K., Tuluri F., Tchounwou P.B., Shaw N., Jain K.G. Establishing the association between quarterly/seasonal air pollution exposure and asthma using geospatial approach. Aerosol Air Qual. Res. 2015;15:1525–1544. doi: 10.4209/aaqr.2014.09.0218. [DOI] [Google Scholar]
- 76.Rashidi M., Ramesht M.H., Zohary M., Poursafa P., Kelishadi R., Rashidi Z., Rouzbahani R. Relation of air pollution with epidemiology of respiratory diseases in isfahan, Iran from 2005 to 2009. J. Res. Med.Sci. 2013;18:1074–1079. [PMC free article] [PubMed] [Google Scholar]
- 77.Le T.G., Ngo L., Mehta S., Do V.D., Thach T.Q., Vu X.D., Nguyen D.T., Cohen A. Effects of short-term exposure to air pollution on hospital admissions of young children for acute lower respiratory infections in Ho Chi Minh City, Vietnam. Res. Rep. Health Eff. Inst. 2012;169:5–72. [PubMed] [Google Scholar]
- 78.Gouveia N., Fletcher T. Time series analysis of air pollution and mortality: effects by cause, age and socioeconomic status. J. Epidemiol. Community Health. 2000;54:750–755. doi: 10.1136/jech.54.10.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kan H., Chen B., Zhao N., London S.J., Song G., Chen G., Zhang Y., Jiang L. A time-series study of ambient air pollution and daily mortality in Shanghai, China. Res. Rep. Health Eff. Inst. 2010;154:17–78. doi: 10.1097/00001648-200407000-00133. [DOI] [PubMed] [Google Scholar]
- 80.Thurston G.D. A critical review of PM10-mortality time-series studies. J. Expo. Anal. Environ. Epidemiol. 1996;6:3–21. [PubMed] [Google Scholar]
- 81.Touloumi G., Pocock S.J., Katsouyanni K., Trichopoulos D. Short-term effects of air pollution on daily mortality in Athens: A time-series analysis. Int. J. Epidemiol. 1994;23:957–967. doi: 10.1093/ije/23.5.957. [DOI] [PubMed] [Google Scholar]
- 82.Schwartz J., Dockery D.W. Particulate air pollution and daily mortality in Steubenville, Ohio. Am. J. Epidemiol. 1992;135:12–19. doi: 10.1093/oxfordjournals.aje.a116195. [DOI] [PubMed] [Google Scholar]
- 83.Sartor F., Snacken R., Demuth C., Walckiers D. Temperature, ambient ozone levels, and mortality during summer, 1994, in Belgium. Environ. Res. 1995;70:105–113. doi: 10.1006/enrs.1995.1054. [DOI] [PubMed] [Google Scholar]
- 84.Dockery D.W., Schwartz J., Spengler J.D. Air pollution and daily mortality: Associations with particulates and acid aerosols. Environ. Res. 1992;59:362–373. doi: 10.1016/S0013-9351(05)80042-8. [DOI] [PubMed] [Google Scholar]
- 85.Wordley J., Walters S., Ayres J.G. Short term variations in hospital admissions and mortality and particulate air pollution. Occup. Environ. Med. 1997;54:108–116. doi: 10.1136/oem.54.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Borja-Aburto V.H., Loomis D.P., Bangdiwala S.I., Shy C.M., Rascon-Pacheco R.A. Ozone, suspended particulates, and daily mortality in Mexico City. Am. J. Epidemiol. 1997;145:258–268. doi: 10.1093/oxfordjournals.aje.a009099. [DOI] [PubMed] [Google Scholar]
- 87.Ballester F., Corella D., Perez-Hoyos S., Hervás A. Air pollution and mortality in Valencia, Spain: A study using the APHEA methodology. J. Epidemiol. Community Health. 1996;50:527–533. doi: 10.1136/jech.50.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sunyer J., Castellsague J., Sáez M., Tobias A., Antó J.M. Air pollution and mortality in Barcelona. J. Epidemiol. Community Health. 1996;50:S76–S80. doi: 10.1136/jech.50.Suppl_1.s76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pope C.A., Schwartz J., Ransom M.R. Daily mortality and PM10 pollution in Utah Valley. Arch. Environ. Health. 1992;47:211–217. doi: 10.1080/00039896.1992.9938351. [DOI] [PubMed] [Google Scholar]
- 90.Schwartz J. What are people dying of on high air pollution days? Environ. Res. 1994;64:26–35. doi: 10.1006/enrs.1994.1004. [DOI] [PubMed] [Google Scholar]