Abstract
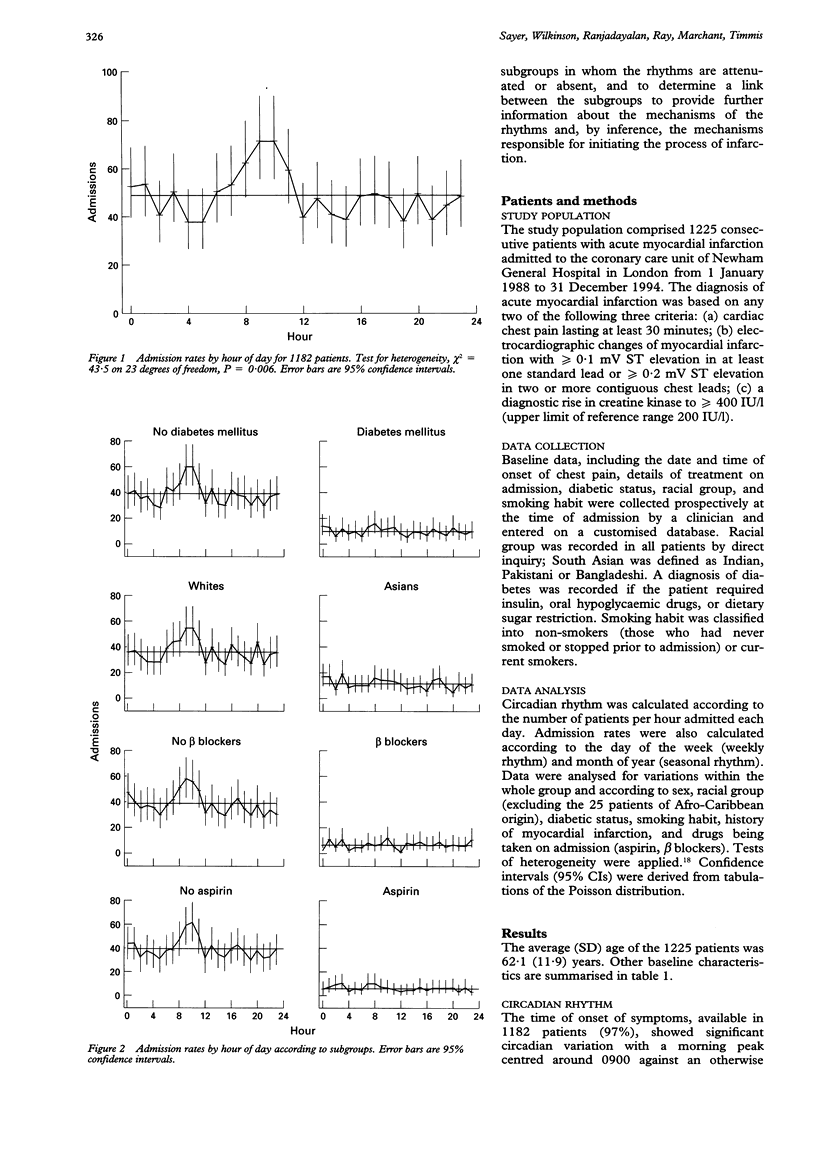
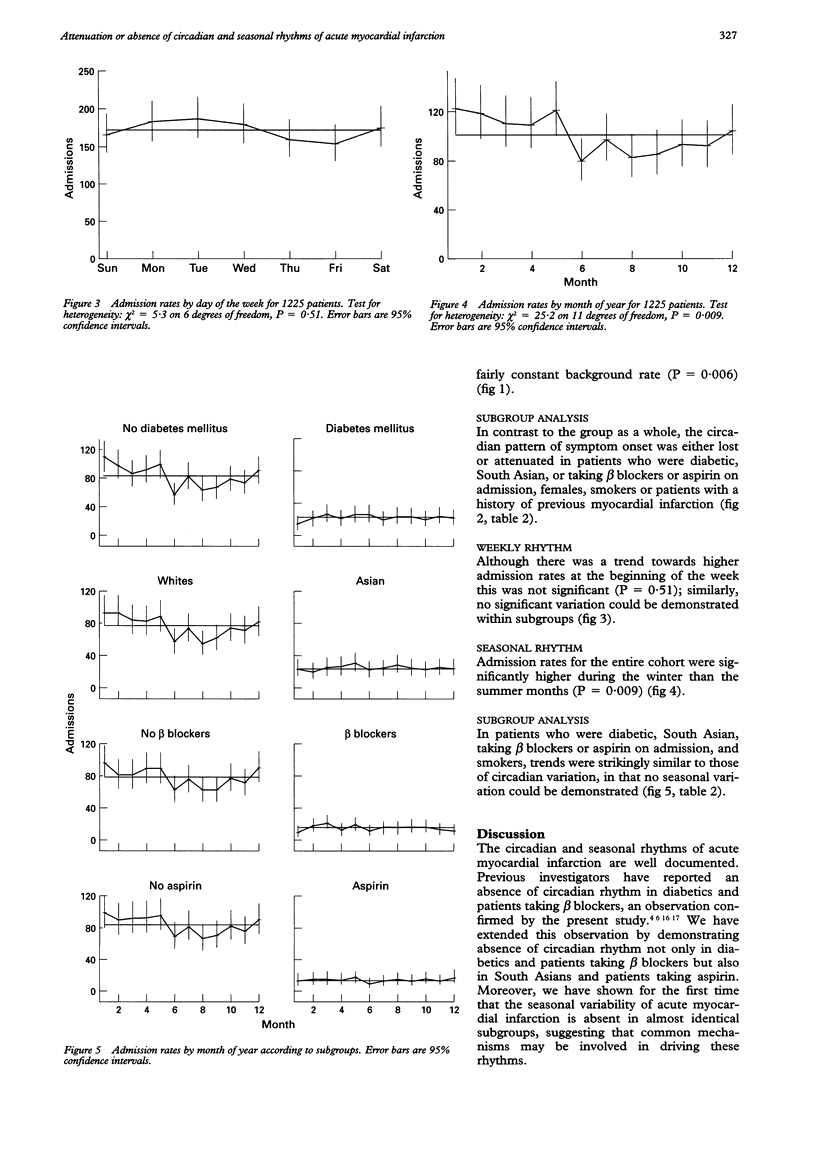
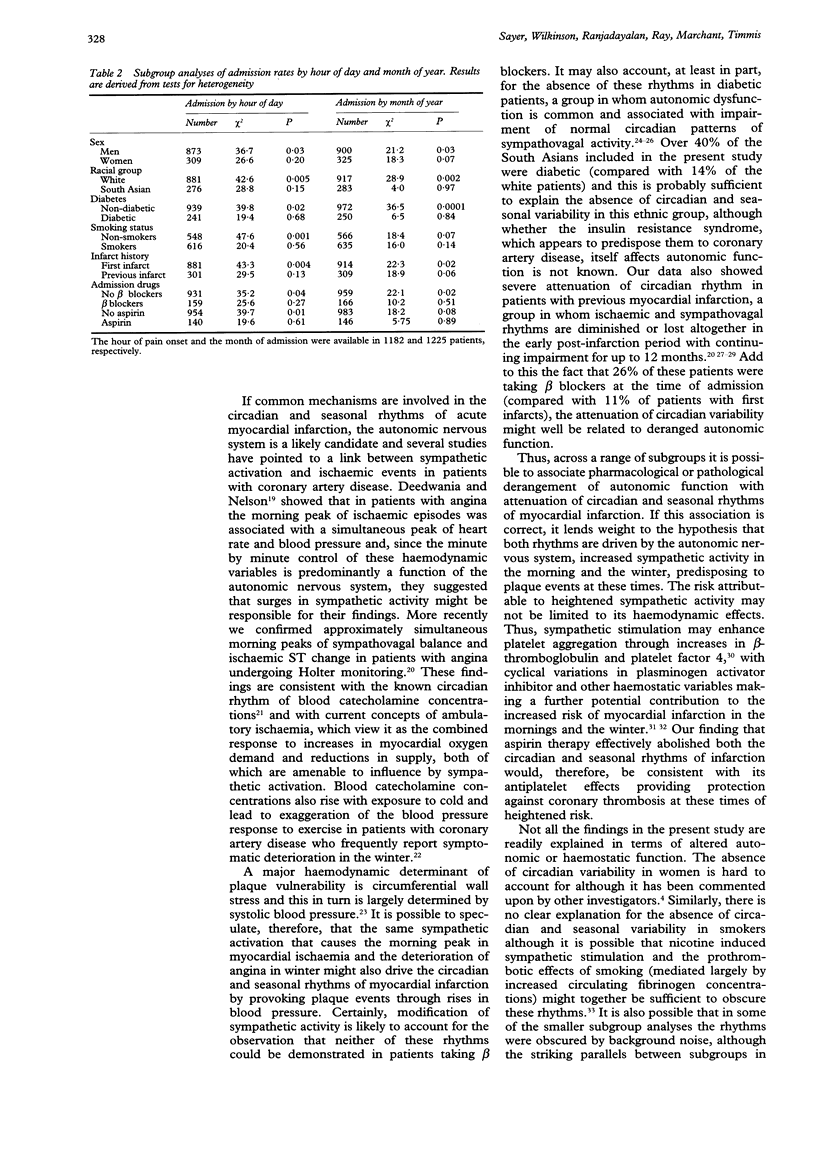
OBJECTIVES: To examine the circadian, seasonal, and weekly rhythms of acute myocardial infarction, and to identify subgroups in whom the rhythms are attenuated or absent to provide further information about the mechanisms of the rhythms and the processes responsible for triggering plaque events. DESIGN AND SETTING: Prospective, observational study in a general hospital. PATIENTS AND METHODS: 1225 consecutive patients admitted to a coronary care unit with acute myocardial infarction were studied. Admission rates were calculated according to the hour of the day (circadian rhythm), day of the week (weekly rhythm), and month of year (seasonal rhythm). The data were analysed for variations within the whole group and within subgroups. RESULTS: A weekly rhythm of acute myocardial infarction could not be demonstrated but there was a trend towards higher admission rates at the beginning of the week. However, the time of onset of symptoms showed significant circadian variation for the group as a whole, peaking in the morning (P = 0.006), against an otherwise fairly constant background rate. Subgroup analysis showed complete absence of the circadian rhythm in patients who were diabetic, South Asian, or taking beta blockers or aspirin on admission. Significant seasonal variation in admission rates was also demonstrated for the group as a whole with a winter peak and a summer trough (P = 0.009). Again, no seasonal rhythm could be demonstrated in patients who were diabetic, South Asian, or taking beta blockers or aspirin on admission. CONCLUSIONS: The absence of circadian and seasonal rhythms of acute myocardial infarction in almost identical subgroups suggests that common mechanisms are involved in driving these rhythms. The autonomic nervous system is a likely candidate because the rhythms were absent in patients taking beta blockers as well as in patients in whom derangement of autonomic function commonly occurs.
Full text
PDF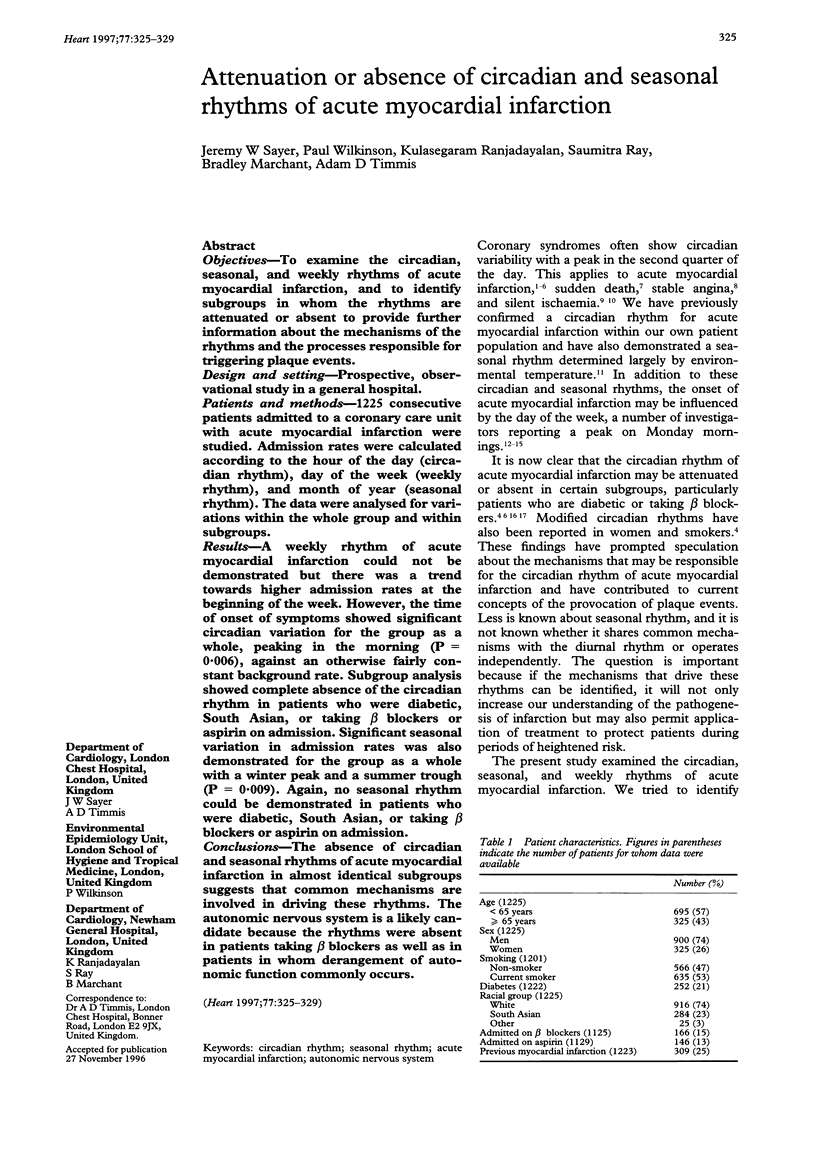
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andreotti F., Davies G. J., Hackett D. R., Khan M. I., De Bart A. C., Aber V. R., Maseri A., Kluft C. Major circadian fluctuations in fibrinolytic factors and possible relevance to time of onset of myocardial infarction, sudden cardiac death and stroke. Am J Cardiol. 1988 Sep 15;62(9):635–637. doi: 10.1016/0002-9149(88)90669-8. [DOI] [PubMed] [Google Scholar]
- Benowitz N. L. Drug therapy. Pharmacologic aspects of cigarette smoking and nicotine addition. N Engl J Med. 1988 Nov 17;319(20):1318–1330. doi: 10.1056/NEJM198811173192005. [DOI] [PubMed] [Google Scholar]
- Bernardi L., Ricordi L., Lazzari P., Soldá P., Calciati A., Ferrari M. R., Vandea I., Finardi G., Fratino P. Impaired circadian modulation of sympathovagal activity in diabetes. A possible explanation for altered temporal onset of cardiovascular disease. Circulation. 1992 Nov;86(5):1443–1452. doi: 10.1161/01.cir.86.5.1443. [DOI] [PubMed] [Google Scholar]
- Bigger J. T., Jr, Fleiss J. L., Rolnitzky L. M., Steinman R. C., Schneider W. J. Time course of recovery of heart period variability after myocardial infarction. J Am Coll Cardiol. 1991 Dec;18(7):1643–1649. doi: 10.1016/0735-1097(91)90497-w. [DOI] [PubMed] [Google Scholar]
- Bridges A. B., McLaren M., Scott N. A., Pringle T. H., McNeill G. P., Belch J. J. Circadian variation of tissue plasminogen activator and its inhibitor, von Willebrand factor antigen, and prostacyclin stimulating factor in men with ischaemic heart disease. Br Heart J. 1993 Feb;69(2):121–124. doi: 10.1136/hrt.69.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deedwania P. C., Nelson J. R. Pathophysiology of silent myocardial ischemia during daily life. Hemodynamic evaluation by simultaneous electrocardiographic and blood pressure monitoring. Circulation. 1990 Oct;82(4):1296–1304. doi: 10.1161/01.cir.82.4.1296. [DOI] [PubMed] [Google Scholar]
- Fava S., Azzopardi J., Muscat H. A., Fenech F. F. Absence of circadian variation in the onset of acute myocardial infarction in diabetic subjects. Br Heart J. 1995 Oct;74(4):370–372. doi: 10.1136/hrt.74.4.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnecchi-Ruscone T., Piccaluga E., Guzzetti S., Contini M., Montano N., Nicolis E. Morning and Monday: critical periods for the onset of acute myocardial infarction. The GISSI 2 Study experience. Eur Heart J. 1994 Jul;15(7):882–887. doi: 10.1093/oxfordjournals.eurheartj.a060605. [DOI] [PubMed] [Google Scholar]
- Goldberg R. J., Brady P., Muller J. E., Chen Z. Y., de Groot M., Zonneveld P., Dalen J. E. Time of onset of symptoms of acute myocardial infarction. Am J Cardiol. 1990 Jul 15;66(2):140–144. doi: 10.1016/0002-9149(90)90577-n. [DOI] [PubMed] [Google Scholar]
- Hjalmarson A., Gilpin E. A., Nicod P., Dittrich H., Henning H., Engler R., Blacky A. R., Smith S. C., Jr, Ricou F., Ross J., Jr Differing circadian patterns of symptom onset in subgroups of patients with acute myocardial infarction. Circulation. 1989 Aug;80(2):267–275. doi: 10.1161/01.cir.80.2.267. [DOI] [PubMed] [Google Scholar]
- Kawahara J., Sano H., Fukuzaki H., Saito K., Hirouchi H. Acute effects of exposure to cold on blood pressure, platelet function and sympathetic nervous activity in humans. Am J Hypertens. 1989 Sep;2(9):724–726. doi: 10.1093/ajh/2.9.724. [DOI] [PubMed] [Google Scholar]
- Kono T., Morita H., Nishina T., Fujita M., Hirota Y., Kawamura K., Fujiwara A. Circadian variations of onset of acute myocardial infarction and efficacy of thrombolytic therapy. J Am Coll Cardiol. 1996 Mar 15;27(4):774–778. doi: 10.1016/0735-1097(95)00552-8. [DOI] [PubMed] [Google Scholar]
- Lombardi F., Sandrone G., Pernpruner S., Sala R., Garimoldi M., Cerutti S., Baselli G., Pagani M., Malliani A. Heart rate variability as an index of sympathovagal interaction after acute myocardial infarction. Am J Cardiol. 1987 Dec 1;60(16):1239–1245. doi: 10.1016/0002-9149(87)90601-1. [DOI] [PubMed] [Google Scholar]
- Marchant B., Donaldson G., Mridha K., Scarborough M., Timmis A. D. Mechanisms of cold intolerance in patients with angina. J Am Coll Cardiol. 1994 Mar 1;23(3):630–636. doi: 10.1016/0735-1097(94)90747-1. [DOI] [PubMed] [Google Scholar]
- Marchant B., Ranjadayalan K., Stevenson R., Wilkinson P., Timmis A. D. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: the influence of environmental temperature. Br Heart J. 1993 May;69(5):385–387. doi: 10.1136/hrt.69.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchant B., Stevenson R., Vaishnav S., Wilkinson P., Ranjadayalan K., Timmis A. D. Influence of the autonomic nervous system on circadian patterns of myocardial ischaemia: comparison of stable angina with the early postinfarction period. Br Heart J. 1994 Apr;71(4):329–333. doi: 10.1136/hrt.71.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchant B., Umachandran V., Stevenson R., Kopelman P. G., Timmis A. D. Silent myocardial ischemia: role of subclinical neuropathy in patients with and without diabetes. J Am Coll Cardiol. 1993 Nov 1;22(5):1433–1437. doi: 10.1016/0735-1097(93)90554-e. [DOI] [PubMed] [Google Scholar]
- Mulcahy D., Keegan J., Crean P., Quyyumi A., Shapiro L., Wright C., Fox K. Silent myocardial ischaemia in chronic stable angina: a study of its frequency and characteristics in 150 patients. Br Heart J. 1988 Nov;60(5):417–423. doi: 10.1136/hrt.60.5.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller J. E., Stone P. H., Turi Z. G., Rutherford J. D., Czeisler C. A., Parker C., Poole W. K., Passamani E., Roberts R., Robertson T. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985 Nov 21;313(21):1315–1322. doi: 10.1056/NEJM198511213132103. [DOI] [PubMed] [Google Scholar]
- Richardson P. D., Davies M. J., Born G. V. Influence of plaque configuration and stress distribution on fissuring of coronary atherosclerotic plaques. Lancet. 1989 Oct 21;2(8669):941–944. doi: 10.1016/s0140-6736(89)90953-7. [DOI] [PubMed] [Google Scholar]
- Rocco M. B., Barry J., Campbell S., Nabel E., Cook E. F., Goldman L., Selwyn A. P. Circadian variation of transient myocardial ischemia in patients with coronary artery disease. Circulation. 1987 Feb;75(2):395–400. doi: 10.1161/01.cir.75.2.395. [DOI] [PubMed] [Google Scholar]
- Tanaka T., Fujita M., Fudo T., Tamaki S., Nohara R., Sasayama S. Modification of the circadian variation of symptom onset of acute myocardial infarction in diabetes mellitus. Coron Artery Dis. 1995 Mar;6(3):241–244. [PubMed] [Google Scholar]
- Taylor C. R., Hodge E. M., White D. A. Circadian rhythm of angina: similarity to circadian rhythms of myocardial infarction, ischemic ST segment depression, and sudden cardiac death. The Amlodipine Angina Study Group. Am Heart J. 1989 Nov;118(5 Pt 2):1098–1099. doi: 10.1016/0002-8703(89)90833-8. [DOI] [PubMed] [Google Scholar]
- Thompson D. R., Blandford R. L., Sutton T. W., Marchant P. R. Time of onset of chest pain in acute myocardial infarction. Int J Cardiol. 1985 Feb;7(2):139–148. doi: 10.1016/0167-5273(85)90354-7. [DOI] [PubMed] [Google Scholar]
- Thompson D. R., Pohl J. E., Sutton T. W. Acute myocardial infarction and day of the week. Am J Cardiol. 1992 Jan 15;69(3):266–267. doi: 10.1016/0002-9149(92)91318-x. [DOI] [PubMed] [Google Scholar]
- Thompson D. R., Sutton T. W., Jowett N. I., Pohl J. E. Circadian variation in the frequency of onset of chest pain in acute myocardial infarction. Br Heart J. 1991 Apr;65(4):177–178. doi: 10.1136/hrt.65.4.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turton M. B., Deegan T. Circadian variations of plasma catecholamine, cortisol and immunoreactive insulin concentrations in supine subjects. Clin Chim Acta. 1974 Sep 30;55(3):389–397. doi: 10.1016/0009-8981(74)90014-x. [DOI] [PubMed] [Google Scholar]
- Vaishnav S., Stevenson R., Marchant B., Lagi K., Ranjadayalan K., Timmis A. D. Relation between heart rate variability early after acute myocardial infarction and long-term mortality. Am J Cardiol. 1994 Apr 1;73(9):653–657. doi: 10.1016/0002-9149(94)90928-8. [DOI] [PubMed] [Google Scholar]
- Willich S. N., Levy D., Rocco M. B., Tofler G. H., Stone P. H., Muller J. E. Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population. Am J Cardiol. 1987 Oct 1;60(10):801–806. doi: 10.1016/0002-9149(87)91027-7. [DOI] [PubMed] [Google Scholar]
- Willich S. N., Linderer T., Wegscheider K., Leizorovicz A., Alamercery I., Schröder R. Increased morning incidence of myocardial infarction in the ISAM Study: absence with prior beta-adrenergic blockade. ISAM Study Group. Circulation. 1989 Oct;80(4):853–858. doi: 10.1161/01.cir.80.4.853. [DOI] [PubMed] [Google Scholar]
- Zarich S., Waxman S., Freeman R. T., Mittleman M., Hegarty P., Nesto R. W. Effect of autonomic nervous system dysfunction on the circadian pattern of myocardial ischemia in diabetes mellitus. J Am Coll Cardiol. 1994 Oct;24(4):956–962. doi: 10.1016/0735-1097(94)90855-9. [DOI] [PubMed] [Google Scholar]



