Abstract
Background:
New technologies, instruments, and surgical techniques are necessary to help the clinician ensure the best result and satisfy the patient's expectations, and surgical microscope has been thoroughly demonstrated as a useful tool. A clinical study was carried out to compare 2 different types of root coverage procedures using periodontal microsurgical procedure.
Materials and Methods:
Forty patients were selected and divided into Group A and Group B. Group A subjects were treated with subepithelial connective tissue graft (CTG) whereas Group B subjects were treated using a resorbable collagen membrane. The procedures were performed with the help of an operating microscope using 250 mm objective lens and ×6 magnification.
Results:
A comparison between baseline, 1, 3, and 12 months have been done between groups among all parameters. It has been noticed that the root coverage was better in Group A subjects at all time. At 12 months, Group A showed 81.42% coverage where in Group B it was 70.08%. Similarly, increase in the width of keratinized gingiva and attached gingiva were more in Group A.
Conclusions:
The present study showed that use of microsurgical instrument helped to deliver precise incision, better visual acuity, and improved illumination which facilitate to gain a better final outcome. Root coverage was better in the patients using CTG.
Keywords: Collagen membrane, connective tissue graft, gingival recession, operating microscope
INTRODUCTION
Gingival recession is the denudation of cementum with the migration of epithelial attachment in the direction of root apex.[1] Gingival recession as a clinical entity has been described and documented since last century. While considering the elimination of these defects, two criteria should be considered, the esthetic aspects and the functional aspects. The former being the main concern of the patient and later being the main concern of the clinician and hence all attempt should be made to consider both while doing root coverage procedure.[2] The goal of the treatment is to restore the tissue margin to the cementoenamel junction (CEJ) and to create a normal gingival sulcus with a functional attachment.[3]
New technologies, instruments, and surgical techniques are therefore necessary to help the clinician ensure the best result and satisfy the patient's expectations. The surgical microscope has been thoroughly demonstrated as a useful tool in the other field, but use in periodontal surgery is scarcely documented. When maximum precision is required in performing surgery to satisfy particular esthetic demand, a surgical microscope that enhances complete visualization of the operative field represents a useful tool.[4]
The aim of this clinical study was to compare of management of gingival recession using subepithelial connective tissue graft (SCTG) and collagen membrane by microsurgical technique. In addition to the root coverage achieved various other parameters which were compared that were reduction in vertical gingival recession, reduction in horizontal gingival recession, gain in clinical attachment level (CAL), reduction in probing depth (PD), increase in attached gingiva (AG), increase in width of keratinized gingiva (KG), plaque index (PI), gingival index (GI), and improvement in patient sensitivity. All the parameters were compared at pre- and 12 months post-operatively.
MATERIALS AND METHODS
Patient selection
A total of 40 patients aged between 20 and 50 years (mean age 34) who reported to Department of Dental Surgery of the hospital were selected for this study. All these patients were having localized gingival recession with an inadequate width of AG in the maxillary or mandibular anterior region. All these patients were explained about the treatment planning and the surgical procedure. The main selection criteria were used for the selection of patients were Millers Class I and Class II localized gingival recession with <2 mm KG, intact papillae to the mesial and distal aspect of the involved tooth, no clinical mobility, free of any restoration or caries, no traumatic occlusion. Pregnant females, chronic smokers, and tooth with severe malpositioning were excluded from the study.
The study was approved by the Institutional Ethics Committee. Informed consent was taken prior to the study from each subject.
Surgical procedures
The subjects were divided into two groups Group A and Group B. Group A subjects were treated with the use of an SCTG and coronally repositioned flap whereas Group B subjects were treated using a resorbable collagen membrane and coronally repositioned flap.
A single operator performed all these surgical procedure and followed up all the cases. Identical clinical parameters were used for both these technique, and the same were recorded in a clinical data sheet which was specially designed for this study. All the surgical procedures were performed with the help of an operating microscope using 250 mm objective lens and ×6 magnification. In addition to standard surgical instruments, microsurgical instruments were used to perform the surgery. For guided tissue regeneration (GTR) technique lyophilized natural resorbable collagen membrane with 25 mm × 25 mm × 0.2 mm dimension was used.
Preoperative preparation
Strict oral hygiene instructions were given to all individuals. Phases I therapy was carried out, and the patients were kept under observation for a period of 1 month prior to the surgical procedure. Patients, who could not maintain adequate plaque control, were excluded from this study. Preoperative photographs, routine blood, and urine investigation, Intraoral periapical radiograph of the involved tooth were taken prior to the surgery. All the measurements were taken by using same William's graduated periodontal probe and the measurement were recorded to the nearest 0.5 mm.
Group A: Subepithelial connective tissue graft technique
A local anesthetic solution containing 2% lignocaine with 1:80,000 adrenaline was administered at the surgical site. The case shown here was having 6 mm clinical attachment loss [Figure 1]. Horizontal and vertical incisions were given on either side of the recession site, and sulcular incision along the sulcus was given to reflect the flap.[5] The partial thickness flap was dissected carefully leaving the bone covered with periosteum and connective tissue as advocated by Langer and Langer.
Figure 1.
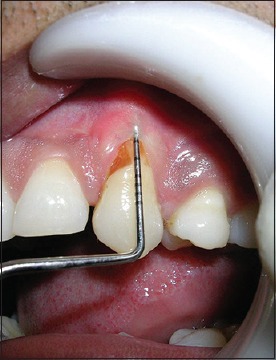
Preoperative Group A (6 mm)
Tension on the flap was relieved by a periosteal releasing incision as recommended by Harris.[6] The exposed root surface was thoroughly planned and kept free of any plaque. The measurement of the recipient bed was taken using the Williams graduated probe in both vertical as well as horizontal direction. The same measurement was used as a guideline while procuring the graft from the palate. The interdental papillae were de-epithelized. Adequate care was taken not to remove the papillae while doing this procedure. Moist gauze was placed on recipient bed to achieve homeostasis before the placement of the graft.
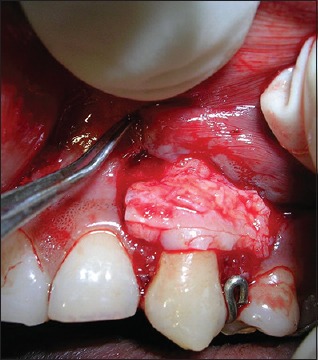
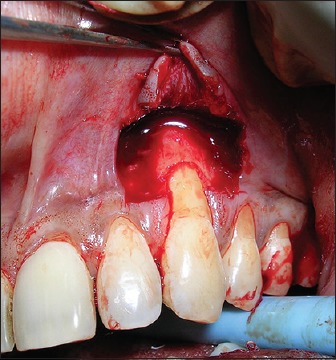
The connective tissue graft (CTG) was procured from the palate. Liu and Weisgold[7] type I–A incision was used for harvesting graft [Figure 2]. The donor area was sutured protected with the help of a prefabricated acrylic palatal stent. The graft was checked for its size, transferred to the recipient bed and sutured to the donor bed with 6–0 Vicryl suture [Figure 3]. The partial thickness flap was repositioned coronally to cover as much of the graft as possible and stabilized with 6–0 polypropylene suture. No attempt was made to completely cover the graft as this would create tension in the flap. A Coe-Pak dressing was given over the graft.
Figure 2.

Procurement of connective tissue graft
Figure 3.
Placement of connective tissue graft
Group B: Collagen membrane technique
The case shown here was having 7 mm clinical attachment loss [Figure 4]. Full thickness flap was raised up to the mucogingival junction and partial thickness flap apical to as recommended by Pini Prato et al.[8] [Figure 5]. The exposed root surface was thoroughly planned, contoured and the curvature was reduced with air rotor with an adequate amount of air-water spray. A template was used as a guideline for trimming the collagen membrane initially. The coronal end of the membrane was placed just apical to the CEJ. It was then stabilized with 6–0 Vicryl suture. A sling suture was placed at the level of CEJ and two lateral sutures at the apical portion of the membrane [Figure 6]. The mucoperiosteal flap was repositioned coronally to cover the entire membrane and stabilized using 6–0 polypropylene and lateral sutures. The periodontal pack was not given postsurgically in Group B subjects.
Figure 4.

Preoperative Group B (7 mm)
Figure 5.
Recipient bed with intact papillae
Figure 6.
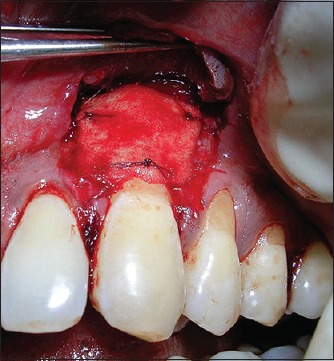
Stabilization of membrane with coronal and lateral sutures
Postoperative data collection
Patients of both groups were recalled frequently for a check-up. The postoperative measurements were recorded at 1 month (except probing), 3 months, and 12 months, respectively. The measurements were recorded in the specific case data sheet and necessary photographs were taken. At the end of 1 year, CTG case showed 1 mm CAL [Figure 7] and 1 mm in collagen group [Figure 8].
Figure 7.

Twelve months postoperative - Group A (1 mm)
Figure 8.

Twelve months postoperative - Group B (1 mm)
Statistical analysis
Various clinical recordings obtained had analyzed with proper statistical analysis. Paired t-test was carried out for comparing parameters within the group, and unpaired t-test was carried out for comparison between the groups. Mann–Whitney test was carried out to do the statistical analysis for patient comfort index.
RESULTS
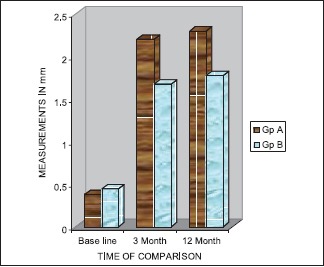
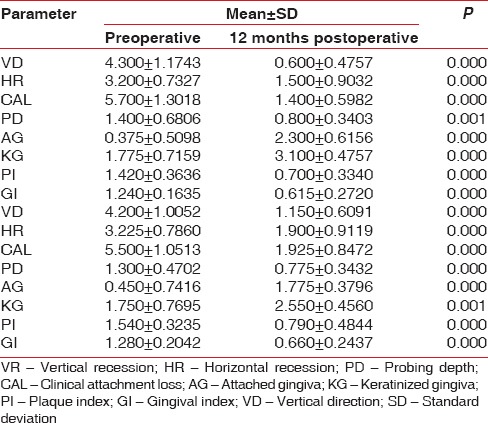
The mean vertical gingival recession in Group A subjects was 4.3 (±1.17) while Group B patients was 4.2 (±1.1). Mean reduction in gingival recession in Group A 12 months postoperatively was 0.6 (±0.48) and in Group B was 1.15 (±0.61), respectively. The reduction in recession in both groups were statistically highly significant (P = 0.000). Similarly, an intergroup comparison of vertical gingival recession at 12 months was clinically insignificant with a P = 0.003. A comparison between baseline to 1, 3, and 12 months have been done between groups to assess the percentage of gingival recession coverage. It has been noticed that the coverage was better in Group A subjects at all time. At 12 months, Group A showed coverage of 81.42% where in Group B it was 70.08% which was statistically significant (P = 0.001) [Graph 1]. Three cases in Group A had 100% root coverage whereas 1 case showed the same in Group B cases. Mean CAL was reduced from 5.7 (±1.30) to 0.60 (±1.4) at the end of 12 months in CTG group, and same in GTR group was 5.5 (±1.05)–0.60 (±1.4). In the intergroup comparison showed statistically significant results at 12 months (P > 0.029). The difference between AG changes was statistically significant [Graph 2]. In CTG Group preoperative mean value of 0.38 was increased to 2.3 (±0.62) whereas in GTR group the preoperative mean value of 0.45 (±0.11) increased to 2.2 (±0.49). The intergroup comparison showed statistically insignificant increase at 12 months with the P = 0.002. Similarly, KG showed a statistical increase in both group but better result with CTG group. At the end of 12 months, in Group A subjects width KG increased from 1.78 (±0.72) to 3.1 (±0.47) while in Group B patients it was from of 1.75 (±0.77) to 2.5 (±0.46). Both results were statistically significant (P = 0.000 and 0.001, respectively). Both procedures showed a reduction in the PD, PI, GI, and improvement in sensitivity clinically, but the observations were statistically insignificant [Table 1].
Graph 1.

% of coverage
Graph 2.
Width of attached gingiva
Table 1.
Pre- and 12 months post-clinical measurements
DISCUSSION
Gingival recession coverage procedures have become an important part of periodontal therapy. Root sensitivity, root caries, and gingival margin discrepancies can be eliminated with these procedures. Patient's desire for improved esthetics has also increased its popularity. It is important to recognize the objectives of root coverage. Rubenstein et al.[9] described that densely organized well-collagenated zones of AG serve as a physical barrier to the inflammatory spread to the nearby bone and effectively dissipate muscular and frenal pull and remain in health with normal function.
The result of this study shows that both CTG and GTR resulted in statically significant coverage of recession, the gain in CAL, increases in the amount of keratinized as well as AG. However, the clinical outcome was better in the CTG group than GTR group. The result showed Group A achieved better gingival recession coverage at 3 and 12 months postoperatively which were statistically significant (P = 0.03 and 0.003, respectively). The result of the present study was in agreement with the study conducted by Harris[10] Trombelli et al.[11] and Elizabeth et al.[12]
Various reasons could explain this difference in the outcome of these two techniques. The double blood supplies seem to be enough to nourish the entire graft and its successful outcome of CTG in the Group A subjects.[5] The possible reasons for unsatisfactory results for GTR procedure are the incidence of membrane exposure, size and shape of the defect, tension in the overlying flap, thin marginal tissue, and postoperative mechanical trauma due to noncompliance of patient to the instructions.[2] Trauma to the flap during dissection, the extent of flap undermining, positioning, and suturing of the flap and inadequate tissue integration of the membrane can affect the postsurgical tissue shrinkage that could lead to exposure of the membrane.
Percentage of root coverage achieved was assessed between the groups. A highly significant difference was achieved between Group A and Group B at the end of 12 months with the values of 81.42% and 70.08%, respectively with the P = 0.01. In this study, SCTG procedure gave a better root coverage than GTR procedures [Graph 1]. This is in agreement with the previous studies carried out by other workers.[13,14]
The result showed clinical improvements in SCTG group over GTR group for reducing the width of recession, and this was in agreement with the result seen in the study by Dimitris and Trombelli.[13] However, it is not in agreement with the observations made by Wang et al.[14] and Müller et al.[15] The gain of CAL from baseline to 12 months was statistically significant in Group A when compared with Group B with a P = 0.29. Even though there was no statistical difference in CAL between 3 and 12 months among both groups, there was a gain clinically. The possible explanation for this is the phenomenon of creeping attachment. In this study, this difference seems to have taken place principally by this mechanism. Similar observations were made by Bell et al.[16] and Matter and Cimasoni.[17]
As most of the cases treated exhibit minimal pocket depths, it was difficult to establish the extent of any possible influence in this study. However, in all cases pocket depths remained the same or were reduced after treatment. Comparison between the groups showed no difference between SCTG and GTR with regard to reduction in PD at any point of time.
One of the most important objectives of mucogingival surgery is to increase the width of AG. The comparison among the group clearly showed a highly significant increase in the width of KG in CTG group at 3 and 12 months postoperatively [Graph 2]. The study is in agreement with the results of similar kind of study in the past.
Subjective evaluation was done pre- and post-operatively for tooth sensitivity which revealed that none of the patients had severe postoperative sensitivity following surgery. Most patients had marked a reduction in root sensitivity. An intercomparison between the two groups suggest that both procedures could reduce the sensitivity markedly.
Postsurgical discomfort was more in Group A subjects due to the creation of a second surgical site. Common discomfort reported were bleeding from the donor area, developed sloughing of the flap in the donor area may be due to excessive thinning of the superficial flap. Adequate care was taken for the cases to avoid such complication. As per Reiser et al. the ideal area for the donor procurement is the premolar area and not extending beyond the distal aspect of the first molar.[18] This protocol was strictly followed to the entire Group A subjects. GTR membrane can become partially exposed become contaminated and form a pathway for infection which may jeopardize the healing resulting unfavorable result as reported by Selvig et al.[19] Two cases reported with exposure of the coronal portion of the membrane which was trimmed and the area was irrigated with saline. These patients were instructed to give more emphasis on home care plaque control methods.
All the surgical procedures were performed using an operating microscope using ×6 with a 250 mm objective lens [Figure 9]. The key of microsurgery is precise control of gingiva.[20] The improved visual acuity and use of microsurgical instruments provided a new scope to the field of periodontal plastic surgery. The present study showed that use of microsurgical instrument definitely improves the outcome of surgery. The result of this study is in agreement with the study by Burkhardt and Lang[21] and Francetti et al.[22] Operating microscope offers three distinct advantages to the periodontists. They are illumination, magnification, and increased precision in the delivery of surgical skill which is known as a triad of microsurgery.
Figure 9.

Ergonomics of microsurgery
Only very few studies have carried out in past using operating microscope for gingival recession coverage. Hence to get a reliable and conclusive report regarding the advantage of periodontal microsurgery, more number of studies with long-term follow-up is required to be carried out. The smaller sample size and short follow-up period are the major limitations of the present study. Therefore, it would be desirable to carry out a study with a larger sample size and a longer follow-up. No attempt was made to compare the histological healing pattern between the groups. However, histological studies are suggested which determine the type of attachment and healing following the SCTG and GTR procedure using collagen membrane.
CONCLUSIONS
Analyzing the observations made at the end of 12 months follow-up, it is summarized that:
Both techniques produced a predictable and satisfactory result as per esthetics and coverage of denuded roots was concerned. However, the clinical outcome is appeared to be better with SCTG technique. SCTG technique achieved a better result in gingival recession coverage and gained in CAL
At 12 months increase in width of AG and KG were more in SCTG group
Insignificant differences in reduction in PD, improvement in sensitivity, PI and GI were observed between two groups.
Microsurgical procedure helped to deliver precise incision, better visual acuity, and better illumination which facilitate to gain a better final outcome in both techniques.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Stoner JE, Mazdyasna S. Gingival recession in the lower incisor region of 15-year-old subjects. J Periodontol. 1980;51:74–6. doi: 10.1902/jop.1980.51.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Al-Hamdan K, Eber R, Sarment D, Kowalski C, Wang HL. Guided tissue regeneration-based root coverage: Meta-analysis. J Periodontol. 2003;74:1520–33. doi: 10.1902/jop.2003.74.10.1520. [DOI] [PubMed] [Google Scholar]
- 3.Miller PD., Jr Regenerative and reconstructive periodontal plastic surgery. Mucogingival surgery. Dent Clin North Am. 1988;32:287–306. [PubMed] [Google Scholar]
- 4.Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein RL. Microsurgical treatment of gingival recession: A controlled clinical study. Int J Periodontics Restorative Dent. 2005;25:181–8. [PubMed] [Google Scholar]
- 5.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 6.Harris RJ. The connective tissue and partial thickness double pedicle graft: A predictable method of obtaining root coverage. J Periodontol. 1992;63:477–86. doi: 10.1902/jop.1992.63.5.477. [DOI] [PubMed] [Google Scholar]
- 7.Liu CL, Weisgold AS. Connective tissue graft: A classification for incision design from the palatal site and clinical case reports. Int J Periodontics Restorative Dent. 2002;22:373–9. [PubMed] [Google Scholar]
- 8.Pini Prato G, Tinti C, Vincenzi G, Magnani C, Cortellini P, Clauser C. Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recession. J Periodontol. 1992;63:919–28. doi: 10.1902/jop.1992.63.11.919. [DOI] [PubMed] [Google Scholar]
- 9.Rubenstein HS, Ruben MP, Levy C, Peiser S. Evidence for successful acceptance of irradiated free gingival allografts in dogs. J Periodontol. 1975;46:195–208. doi: 10.1902/jop.1975.46.4.195. [DOI] [PubMed] [Google Scholar]
- 10.Harris RJ. A comparison of 2 root coverages techniques: GTR with a bioresorbable matrix style membrane versus a connective tissue graft combined with a coronally positioned pedicle graft without vertical incisions. Results of a series of consecutive cases. J Periodontol. 1998;69:1426–34. doi: 10.1902/jop.1998.69.12.1426. [DOI] [PubMed] [Google Scholar]
- 11.Trombelli L, Scabbia A, Tatakis DN, Calura G. Subpedicle connective tissue graft versus guided tissue regeneration with bioabsorbable membrane in the treatment of human gingival recession defects. J Periodontol. 1998;69:1271–7. doi: 10.1902/jop.1998.69.11.1271. [DOI] [PubMed] [Google Scholar]
- 12.Elizabeth PR, Rosemary AC, Carlos R, Eros SC, Gilberto G, Elcio M. Treatment of gingival recession: Comparative study between subepithelial connective tissue graft and guided tissue regeneration. J Periodontol. 2000;71:1441–7. doi: 10.1902/jop.2000.71.9.1441. [DOI] [PubMed] [Google Scholar]
- 13.Tatakis DN, Trombelli L. Gingival recession treatment: Guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. J Periodontol. 2000;71:299–307. doi: 10.1902/jop.2000.71.2.299. [DOI] [PubMed] [Google Scholar]
- 14.Wang HL, Bunyaratavej P, Labadie M, Shyr Y, MacNeil RL. Comparison of 2 clinical techniques for treatment of gingival recession. J Periodontol. 2001;72:1301–11. doi: 10.1902/jop.2001.72.10.1301. [DOI] [PubMed] [Google Scholar]
- 15.Müller HP, Eger T, Schorb A. Gingival dimensions after root coverage with free connective tissue grafts. J Clin Periodontol. 1998;25:424–30. doi: 10.1111/j.1600-051x.1998.tb02466.x. [DOI] [PubMed] [Google Scholar]
- 16.Bell LA, Thomas AG, Jerry JG, Billy MP. The presence of creeping attachment in human gingiva. J Periodontol. 1978;49:513–8. doi: 10.1902/jop.1978.49.10.513. [DOI] [PubMed] [Google Scholar]
- 17.Matter J, Cimasoni G. Creeping attachment after free gingival grafts. J Periodontol. 1976;47:574–9. doi: 10.1902/jop.1976.47.10.574. [DOI] [PubMed] [Google Scholar]
- 18.Reiser GM, Bruno JF, Mahan PE, Larkin LH. The subepithelial connective tissue graft palatal donor site: Anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 1996;16:130–7. [PubMed] [Google Scholar]
- 19.Selvig KA, Nilveus RE, Fitzmorris L, Kersten B, Khorsandi SS. Scanning electron microscopic observations of cell populations and bacterial contamination of membranes used for guided periodontal tissue regeneration in humans. J Periodontol. 1990;61:515–20. doi: 10.1902/jop.1990.61.8.515. [DOI] [PubMed] [Google Scholar]
- 20.Tibbetts LS, Shanelec D. Periodontal microsurgery. Dent Clin North Am. 1998;42:339–59. [PubMed] [Google Scholar]
- 21.Burkhardt R, Lang NP. Coverage of localized gingival recessions: Comparison of micro-and macrosurgical techniques. J Clin Periodontol. 2005;32:287–93. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 22.Francetti L, Del Fabbro M, Weinstein RL. Periodontal microsurgery. Reported 16 cases consecutively treated by the free rotated papilla autograft technique combined with the coronally advanced flap. Int J Periodontics Restorative Dent. 2005;25:181–8. [PubMed] [Google Scholar]


