Abstract
Trephination or trepanation is an intentional surgical procedure performed from the Stone Age. It looks like escaping a black evil from the head. This technique is still used for treatment of chronic subdural hematoma (SDH). Now, we know the origin, pathogenesis and natural history of this lesion. The author try to explore the history of trephination and modern discovery of chronic SDH. The author performed a detailed electronic search of PubMed. By the key word of chronic SDH, 2,593 articles were found without language restriction in May 2015. The author reviewed the fact and way, discovering the present knowledge on the chronic SDH. The first authentic report of chronic SDH was that of Wepfer in 1657. Chronic SDH was regarded as a stroke in 17th century. It was changed as an inflammatory disease in 19th century by Virchow, and became a traumatic lesion in 20th century. However, trauma is not necessary in many cases of chronic SDHs. The more important prerequisite is sufficient potential subdural space, degeneration of the brain. Modifying Virchow's description, chronic SDH is sometimes traumatic, but most often caused by severe degeneration of the brain. From Wepfer's first description, nearly 350 years passed to explore the origin, pathogenesis, and fate of chronic SDH. The nature of the black evil in the head of the Stone Age is uncovering by many authors riding the giant's shoulder. Chronic SDH should be categorized as a degenerative lesion instead of a traumatic lesion.
Keywords: Hematoma, subdural, chronic; Trephination; History; Craniocerebral trauma; Aging
Introduction
Trephination or trepanation is a surgical intervention where a hole is drilled, incised or scraped into the skull using simple surgical tools. Evidence for trephination occurs from prehistoric times from the Neolithic period onwards.4,40) Even in Korea, there was an article (http://www.koreadaily.com/news/read.asp?art_id=1490018#sthash.ZhOSqsN5.dpuf) of a woman's skull, which was trephined in the 6th century (Baekje kingdom). It was practiced starting in the late Paleolithic period and in virtually every part of the world.17) Remarkably, it is performed yet today in parts of Africa, South America, and Melanesia.4) Till 19th century, these openings had been thought to result from weapons, posthumous tampering, or accidental breakage. However, Broca had realized that some of the openings were actually caused by an intentional surgical procedure performed during the Neolithic period.7) Following these discoveries, thousands of such specimens have been discovered from many parts of the world: the United Kingdom, Denmark, Spain, Portugal, Poland, Germany, the Danube Basin, North Africa, Palestine, the Caucasus, all down the western coastline of the Americas and, especially, in Peru, where more than 10,000 specimens have been excavated.7) The number of perforations was usually one or two, however, it varied to seven or eleven.1,59)
Trephination was continued to medieval period through Greco-Roman from Iron, Bronze and Stone Age, all around the world.5,12,38,70) Not all holes in the skull were made by trephination. They may be congenital, developmental, or acquired (whether pathological e.g., due to inflammation, tumor or trauma, or surgical intervention e.g., trephining) lesions.26,56) Differentiation is not always possible, however, evidence of healing from the edge of holes clearly implies surgery in living human skull.26,56,64) The shapes of the holes depended on the technique and tools.4) Previous authors thought trephined skulls were relatively rare in the Far East and China, more trephined skulls have been found in this region than in the rest of the world combined.20,39)
Why they trephined the skull from the Neolithic time to Middle age? Since trephined skulls were found in all around the world, it is hard to develop in a certain area, then spread over. It is also hard to think that all trephination had the same purpose. The reasons for trephination and the instruments used for the procedure differ with time and from culture to culture.3,40) Trephination was performed as part of tribal or superstitious rituals. It was also used as a treatment for a head injury.71) Obvious fracture lines were found on many specimens, often coinciding with, or near, the site of the trephine defect.12,30) It may be used to treat disorders such as headaches, epilepsy, hydrocephalus and mental disorders. Hippocrates recommend trephination for patients with fissured fractures, bone contusion with or without associated fracture, and head injuries with associated bone contusion with or without fracture. He also described surgical technique of trephination with caution.42,50)
Surprisingly, Inca surgeons achieved an average survival rate of 50 to 70% of their craniectomy patients, with little incidence of infection or other complications.40) The outcomes of trepanation in Papua New Guinea were good, in that 70% of patients were thought to survive in 19th century, contrasting with a 75% mortality for cranial surgery in London in the 1870s.72,74) Surgeons of the ancient Peru executed postmortem trepanations on corpses as a means of better understanding cranial anatomy and improving techniques.30) Postmortem trepanations was used as an ancient hands-on workshop.
How they know the trepanations could save the life? It is impossible to prove the fact happen before prehistoric age without any writings, we can guess only. The Stone Age was a clan or a tribal society. The leader of those societies would be a man who was the strongest and the cleverest. The young leader became the aged with an aged brain. Brain atrophy representing the aged brain is an important pre-requisite for development of chronic subdural hematoma (SDH). Asymptomatic chronic SDH can be developed after a trivial injury. If the hematoma became enlarged, typical symptoms of increased intracranial pressure would appear. Shifting of the brain or compression of the motor cortex will brought hemiplegia with loss of consciousness, which make easy to fall. The aged leader with hemiplegia might fall down over a sharp stone, which made a natural trephination. The liquefied hematoma would drain out, which resolve the shifting and compression. The old leader recovered from coma and hemiplegia. It looks like a black evil leak out from the head of the leader.28) People of the Stone Age might think that the black evil in the head made the leader confused. They saw the evil escaping from the head through a hole made by trepanation (Figure 1).
FIGURE 1. People of the Stone Age might think that the black evil escaped from the head through a hole made by trepanation.
Modern History of Chronic SDH
D'Errico and German10) described that the first authentic report of chronic SDH was that of Johannes Wepfer in 1657. He found a large blood-filled cyst beneath the dura on a patient who died after an "apoplectic stroke". Ninety years later, Morgagni reported a similar finding on a patient who died of an "apoplectic" attack. At that time, this condition was regarded as an apoplectic stroke. In 1817, Houssard described the nature of this condition as the clot and its enveloping membranes. Bayle ascribed the pathophysiology of chronic SDH to 'chronic rebleeding' in 1826. However, until 1857, histology and etiology of this lesion remained obscure. Two hundred years after the Wepfer's report, Virchow described the histology of the membranes and explained their formation. He recognized that hematoma durae matris sometimes was traumatic, but he believed that this lesion was most often caused by chronic inflammation (pachymeningitis chronica hemorrhagica) of the dura with extravasation of blood into the subdural space and formation of a film of fibrin over the inner surface of the dura.10,66) Virchow's hypothesis became widely accepted notion over 50 years.75) Successful neurosurgical treatment of chronic subdural hematoma was first reported by Hulke in 1883,75) however, this lesion was regarded as an inflammatory disease in a textbook published in 1911.49) Trauma got attention as a possible cause of this lesion from late 19th and early 20th century.75) In 1914, Trotter69) emphasized the traumatic etiology. Following Putnam and Cushing's report55) in 1925, this lesion has generally been called chronic SDH instead of pachymeningitis hemorrhagica interna. SDH was regarded as a stroke in 17th century, changed as an inflammatory disease in 19th century, and became a traumatic lesion in 20th century. Although the cause of chronic SDH was revealed as trauma, this lesion has still many unrevealed secrets. At first, doctors thought that missed or asymptomatic acute SDHs will be the source of chronic SDH. There was no clear explanation for the latent interval between head injury and onset of symptoms. In 1826, Bayle suggested the chronic rebleeding as a pathogenesis.80) In 1925, Putnam and Cushing55) thought that recurrent hemorrhage caused progressive enlargement of the hematoma. However in 1932, Gardner15) proposed that expansion of an original subdural clot occurred through osmotic attraction of cerebrospinal fluid (CSF) by blood within the semipermeable hematoma neomembranes. Although oncotic pressure theory86) and effusion theory16) were proposed in 1934 and 1955 respectively, osmotic pressure theory was a general opinion for about 40 years.57) Weir76,77) discarded osmotic and oncotic pressure theories comparing the osmolality and oncotic pressure of SDH fluid, venous blood, and CSF in 1971 and 1980. However, Weir could not explain the mechanism of hematoma enlargement by himself.
Attempts to produce chronic SDH in experimental animals were usually failed.9) Injecting blood into the subdural space of mice or dogs was a reasonable method. However, small amount of blood would absorbed, while too much blood killed the animal. In 1972, Watanabe et al.73) could produce a clinical form of chronic SDH by inoculating a clot of blood mixed with CSF. However, Apfelbaum et al.2) failed to prove that CSF was essential to produce chronic SDH. Till the end of 20th century, we could not develop any experimental model demonstrating progressive enlargement of chronic SDH, except a similar pathology of liquefied hematoma enveloped with neomembrane.9)
Meanwhile, attempts to explore the nature of chronic SDH was continued by studying the structure of the neomembrane and content of the hematoma.24,25) In 1975, Sato and Suzuki60) found repeated microhemorrhage from the capillaries of the outer membrane. They reported that repeated microhemorrhage was responsible to the enlargement of chronic SDH.60) Markwalder41) supported that the mechanism of hematoma enlargement was repeated microhemorrhage from the membrane of chronic SDH by reviewing the literature in 1981. Markwalder's review of rebleeding theory was widely accepted. However, asymptomatic acute SDHs were suspected as the origin of chronic SDH till 1985.8) Till the end of 20th century, there were controversies on the origin and natural history of this lesion.37)
Origin of Chronic SDH and Relations of Traumatic Subdural Lesions
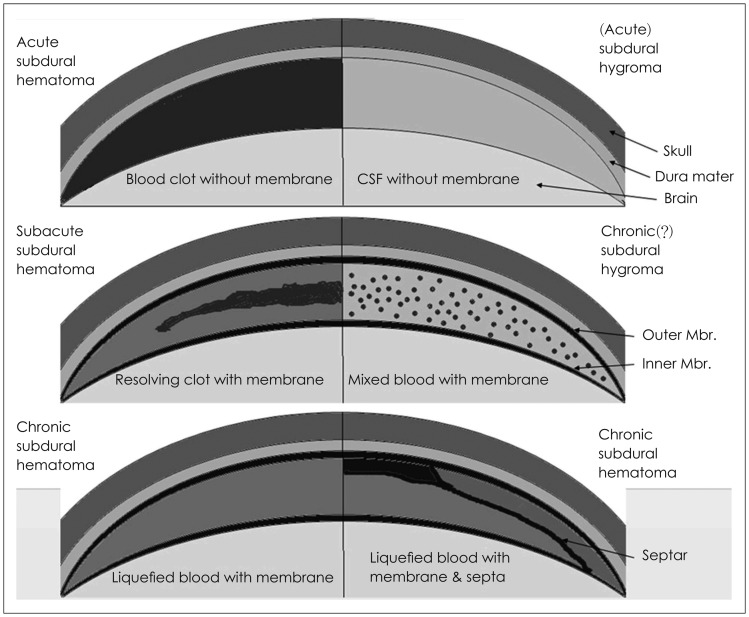
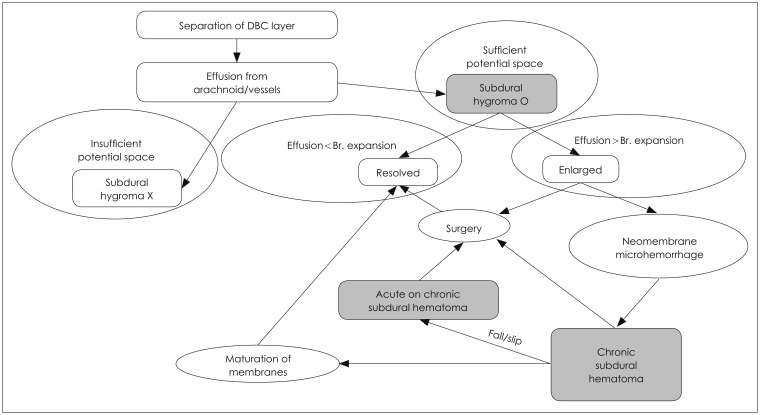
There are three kinds of traumatic subdural lesions; acute SDH, chronic SDH, and subdural hygroma (SDG).35) They are related to trauma and take place in the subdural space. However, they have clearly different characteristics. Acute SDH is a clot without a membrane, while chronic SDH is a liquefied hematoma with neomembranes. SDG is an accumulation of clear or xanthochromic CSF in the subdural space (Figure 2). Endtz13) reported that the first description on the SDG was made by Schwencke in 1733. However, nobody concerned on this lesion over a hundred years. Oka et al.48) reported that Payr presented the first four cases of meningitis serosa traumatica in 1916, while Mayo and Richter reported subdural hydroma and duramater hygroma in 1894 and 1899, respectively.85) Naffziger45) proposed a ball valve mechanism for production of SDG in 1924. This flap hypothesis was hard to observe and impossible to explain the low incidence in the young people, while they were more frequently injured.63) SDG after head injuries became a common lesion after development of computed tomographic scan in 1971. Diagnosis of this lesion became easy and accurate. Although a lot of studies were reported on traumatic SDG after 1980s, the pathogenesis, symptoms, diagnostic criteria, and natural history of this lesion remained obscure. In 1994, we reported a study on the pathogenesis and fate of traumatic SDG (Figure 3).34) To develop SDG, there should be a sufficient potential subdural space and separation of the dural border cell (DBC) layer. The later alone is impossible to develop SDG, if there is no enough space. Separation of the DBC layer is usually made by trauma,34,35) however, it can occur after any surgery opening the skull, dehydration, artificial brain shrinkage, or excessive CSF drainage.11,58) SDG actually occurred at both ends of life, before 5 years or after 50 years, where the potential subdural space was enough.34,48) Age distribution of SDG is the same as that of chronic SDH, which implies pre-requisite of these two lesions is identical. The subdural fluid of SDG is made from CSF78) by effusion.18,22,35,78) Most SDG resolve when the brain expansion or absorption exceeds effusion.32) However, when the brain remains shrunken or effusion exceeds absorption, it will be changed into chronic SDH by the following mechanism. Immediately after the separation, the DBC layer begins proliferation.14,19,61,83) Fibroblast appeared within 24 hours makes visible outer membrane within a week, and inner membrane around three weeks. These neomembrane envelops the subdural space. In-growth of new vessels will follow, especially along the outer membrane, then bleeding from these vessels occurs.21) These unresolved SDGs become chronic SDHs by repeated microhemorrhage from the neomembrane. Such a transformation from SDG to chronic SDH was first reported by Yamada et al.81) in 1979. In 1987, Ohno et al.47) reported nearly 50% of patients with a SDG developed a chronic SDH. They suggested that a chronic SDH usually developed as a consequence of a traumatic SDG. There were numerous reports observing such transformation.6,23,27,29,34,35,44,46,47,51,52,67,68,79,82) Such a transformation or development of a new subdural lesion depends on the interaction of the pre-morbid status, the dynamics of absorption-expansion and maturation of the neomembrane.31) In 2000, we could confirm that the unresolved SDG is the precursor of chronic SDH.33)
FIGURE 2. Pathological characteristics of subdural lesions. Modified from Lee KS. Natural history of chronic subdural haematoma. Brain Inj 18:351-358, 2004.31) Copyright 2004 by the Taylor & Francis. Reprinted with permission. CSF: cerebrospinal fluid, Mbr.: membrane.
FIGURE 3. Development of subdural hygroma and fate of chronic subdural hematoma. Modified from Lee KS, Bae WK, Park YT, Yun IG. The pathogenesis and fate of traumatic subdural hygroma. Br J Neurosurg 8:551-558, 1994.34) Copyright 1994 by the Taylor & Francis. Reprinted with permission. DBC: dural border cell, Br.: brain.
Patients with chronic SDH are prone to fall or slip down.36) If they slip, even though the injury itself is trivial, it may tear the cortical bridge veins or fragile vessels in the neomembrane.53) Repeated trauma may cause acute bleeding, which would make a lump or a layer of hyperdensity within hypo- or isodense hematoma. Like the repeated microhemorrhages from the outer membrane, repeated trauma may cause acute bleeding over the chronic SDH as a mechanism of hematoma enlargement.36,62) Sometimes repeated trivial trauma may cause a subdural hygroma, which became a chronic SDH.53) Although the ages of the SDHs were different, such a chronic-on-chronic SDH may produce the mixed density. Such multiple episodes of trivial trauma are hard to remember.53)
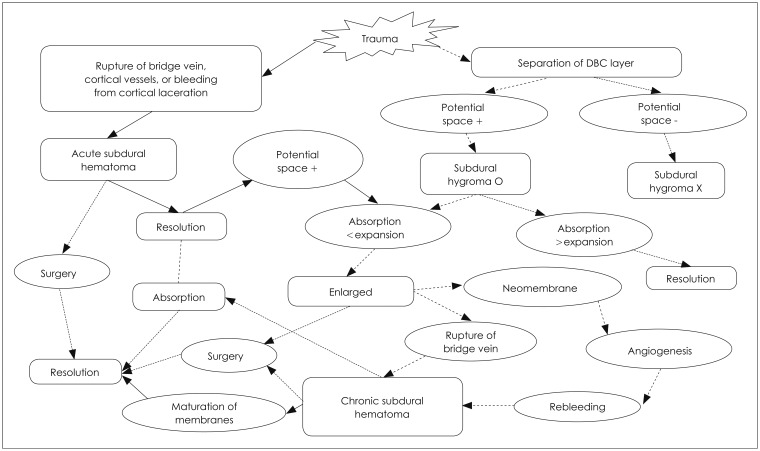
Although the acute SDH is the worst traumatic mass lesion, this lesion may become a chronic SDH if there is a sufficient potential subdural space or the amount of blood is small (Figure 4).84) The acute SDH was enveloped by a new membrane with time. The clot became liquefied by fibrinolytic activity. Neovascularization of the neomembrane results fragile and permeable vessels, which is easy to bleed. Repeated microhemorrhage is responsible to the enlargement of chronic SDH. Chronic SDH is not a static lesion, but an ever-changing lesion.31) Any forces to shrink the brain can be the precipitating factors, while the opposite forces to expand the brain will be the inhibiting factors.31) The initial thin neomembrane becomes matured, organized or even calcified with time.31) Chronic SDHs enlarge when rebleeding exceeds absorption and they become symptomatic. Symptoms of the chronic SDH depend on the pressure and the reserving capacity of the cranial cavity.31) A few chronic SDHs may resolve spontaneously.54) When the neomembrane is matured, the neocapillary becomes no longer fragile.31) If absorption or brain expansion exceeds rebleeding, the hematoma will disappear.31) Maturation of the neomembrane and stabilization of the neovasculature eventually bring about spontaneous resolution.31,65)
FIGURE 4. Origin and relations of subdural lesions. Modified from Lee KS, Bae WK, Park YT, Yun IG. The pathogenesis and fate of traumatic subdural hygroma. Br J Neurosurg 8:551-558, 1994.34) Copyright 1994 by the Taylor & Francis. Reprinted with permission. DBC: dural border cell, Br.: brain.
The origin of a chronic SDH is multiple. It can be developed spontaneously, or changed from a SDG or an acute SDH. Although trauma may separate the DBC layer, a significant number of chronic SDHs, often more than a half of cases, lacks any history of trauma.43,53) A more important prerequisite is sufficient potential subdural space that is aging, degeneration of the brain. At this time, we should answer whether this lesion is a traumatic lesion or a degenerative lesion? Modifying Virchow's description, chronic SDH is sometimes traumatic, but most often caused by severe degeneration of the brain.
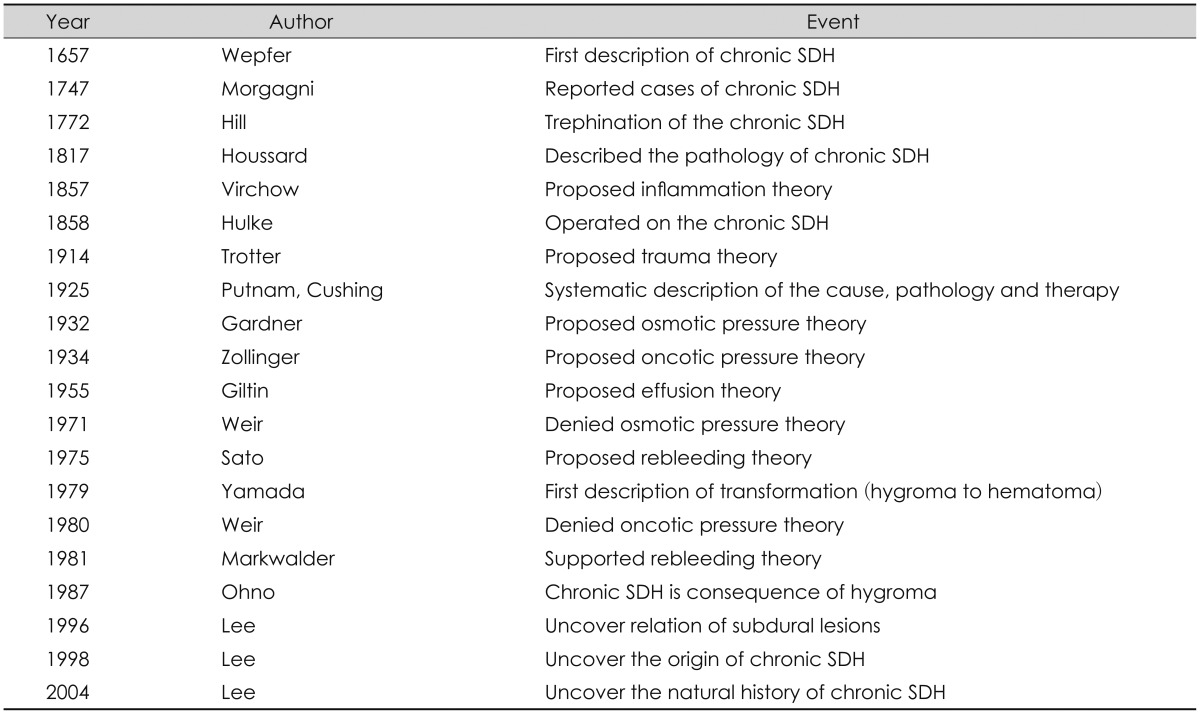
From Wepfer's first description in 1657, nearly 350 years passed to explore the origin, pathogenesis, and fate of chronic SDH (Table 1). The cause of SDG was uncovered in 1994. Relations of traumatic subdural lesions and the origin of this lesion was uncovered in 1996 and 1998, respectively. The nature of the black evil in the head of the Stone Age is uncovering by authors riding the giant's shoulder.
TABLE 1. Chronicle on the modern discovery of chronic subdural hematoma.
SDH: subdural hematoma
Footnotes
The author has no financial conflicts of interest.
References
- 1.Andrushko VA, Verano JW. Prehistoric trepanation in the Cuzco region of Peru: a view into an ancient Andean practice. Am J Phys Anthropol. 2008;137:4–13. doi: 10.1002/ajpa.20836. [DOI] [PubMed] [Google Scholar]
- 2.Apfelbaum RI, Guthkelch AN, Shulman K. Experimental production of subdural hematomas. J Neurosurg. 1974;40:336–346. doi: 10.3171/jns.1974.40.3.0336. [DOI] [PubMed] [Google Scholar]
- 3.Bereczki Z, Marcsik A. Trephined skulls from ancient populations in Hungary. Acta Medica Lithuanica. 2005;12:65–69. [Google Scholar]
- 4.Campillo D. Neurosurgical pathology in prehistory. Acta Neurochir (Wien) 1984;70:275–290. doi: 10.1007/BF01406656. [DOI] [PubMed] [Google Scholar]
- 5.Capasso L, Michetti E, Pierfelice L, D'Anastasio R. Neurosurgery 7000 years ago in central Italy. Lancet. 2002;359:2206. doi: 10.1016/S0140-6736(02)09084-0. [DOI] [PubMed] [Google Scholar]
- 6.Cha KH, Kim CH, Lee HK, Moon JG, Cho TG. The Clinical Course of Subdural Hygroma with Head Injury. Korean J Neurotrauma. 2013;9:125–130. [Google Scholar]
- 7.Clower WT, Finger S. Discovering trepanation: the contribution of Paul Broca. Neurosurgery. 2001;49:1417–1425. discussion 1425-1426. doi: 10.1097/00006123-200112000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Cooper PR. Traumatic intracranial hematomas. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. vol 2. New York: McGraw-Hill; pp. 1657–1661.pp. 1985 [Google Scholar]
- 9.D'Abbondanza JA, Loch Macdonald R. Experimental models of chronic subdural hematoma. Neurol Res. 2014;36:176–188. doi: 10.1179/1743132813Y.0000000279. [DOI] [PubMed] [Google Scholar]
- 10.D'Errico AP, German WJ. Chronic Subdural Hematoma. Yale J Biol Med. 1930;3:11–20. [PMC free article] [PubMed] [Google Scholar]
- 11.Dierckx RA, Bruyland M, Nuyens Z, Stadnik T, Solheid C, Ebinger G. Non-traumatic subdural hygroma. Acta Neurol Belg. 1989;89:352–357. [PubMed] [Google Scholar]
- 12.Ellis H. The Cambridge illustrated history of surgery. Cambridge: Cambridge University Press; 2009. [Google Scholar]
- 13.Endtz LJ. Post-traumatic hygroma in the eighteenth century: described by Thomas Schwencke. Surg Neurol. 1978;10:305–307. [PubMed] [Google Scholar]
- 14.Friede RL, Schachenmayr W. The origin ofsubdural neomembranes. II. Fine structural of neomembranes. Am J Pathol. 1978;92:69–84. [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner WJ. Traumatic subdural hematoma with particular reference to the latent interval. Arch Neurol Psychiatry. 1932;27:847–858. [Google Scholar]
- 16.Gitlin D. Pathogenesis of subdural collections of fluid. Pediatrics. 1955;16:345–352. [PubMed] [Google Scholar]
- 17.Gross CG. A hole in the head. Neuroscientist. 1999;5:263–269. [Google Scholar]
- 18.Haines DE. On the question of a subdural space. Anat Rec. 1991;230:3–21. doi: 10.1002/ar.1092300103. [DOI] [PubMed] [Google Scholar]
- 19.Haines DE, Harkey HL, al-Mefty O. The "subdural" space: a new look at an outdated concept. Neurosurgery. 1993;32:111–120. doi: 10.1227/00006123-199301000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Han K, Chen X. The archaeological evidence of trepanation in early China. Indo-Pac Prehist Assoc Bull. 2007;27:22–27. [Google Scholar]
- 21.Hasegawa M, Yamashima T, Yamashita J, Suzuki M, Shimada S. Traumatic subdural hygroma: pathology and meningeal enhancement on magnetic resonance imaging. Neurosurgery. 1992;31:580–585. doi: 10.1227/00006123-199209000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Hoff J, Bates E, Barnes B, Glickman M, Margolis T. Traumatic subdural hygroma. J Trauma. 1973;13:870–876. [PubMed] [Google Scholar]
- 23.Ishibashi A, Yokokura Y, Miyagi J. Clinical analysis of nineteen patients with traumatic subdural hygromas. Kurume Med J. 1994;41:81–85. doi: 10.2739/kurumemedj.41.81. [DOI] [PubMed] [Google Scholar]
- 24.Ito H, Komai T, Yamamoto S. Fibrinolytic enzyme in the lining walls of chronic subdural hematoma. J Neurosurg. 1978;48:197–200. doi: 10.3171/jns.1978.48.2.0197. [DOI] [PubMed] [Google Scholar]
- 25.Ito H, Yamamoto S, Komai T, Mizukoshi H. Role of local hyperfibrinolysis in the etiology of chronic subdural hematoma. J Neurosurg. 1976;45:26–31. doi: 10.3171/jns.1976.45.1.0026. [DOI] [PubMed] [Google Scholar]
- 26.Kaufman MH, Whitaker D, McTavish J. Differential diagnosis of holes in the calvarium: application of modern clinical data to palaeopathology. J Archaeol Sci. 1997;24:193–218. [Google Scholar]
- 27.Kawano N, Endo M, Saito M, Yada K. [Origin of the capsule of a chronic subdural hematoma--an electron microscopy study] No Shinkei Geka. 1988;16:747–752. [PubMed] [Google Scholar]
- 28.Kim DJ. The appeal of holes in the head. In: Whitelaw WA, editor. The Proceedings of the 13th annual history of medicine days. Calgary, CA: Faculty of Medicine; University of Calgary; 2004. pp. 17–24. [Google Scholar]
- 29.Koizumi H, Fukamachi A, Wakao T, Tasaki T, Nagaseki Y, Yanai Y. [Traumatic subdural hygromas in adults--on the possibility of development of chronic subdural hematoma (author's transl)] Neurol Med Chir (Tokyo) 1981;21:397–406. [PubMed] [Google Scholar]
- 30.Kurin DS. Trepanation in South-Central Peru during the early late intermediate period (ca. AD 1000-1250) Am J Phys Anthropol. 2013;152:484–494. doi: 10.1002/ajpa.22383. [DOI] [PubMed] [Google Scholar]
- 31.Lee KS. Natural history of chronic subdural haematoma. Brain Inj. 2004;18:351–358. doi: 10.1080/02699050310001645801. [DOI] [PubMed] [Google Scholar]
- 32.Lee KS. The pathogenesis and clinical significance of traumatic subdural hygroma. Brain Inj. 1998;12:595–603. doi: 10.1080/026990598122359. [DOI] [PubMed] [Google Scholar]
- 33.Lee KS, Bae WK, Bae HG, Yun IG. The fate of traumatic subdural hygroma in serial computed tomographic scans. J Korean Med Sci. 2000;15:560–568. doi: 10.3346/jkms.2000.15.5.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee KS, Bae WK, Park YT, Yun IG. The pathogenesis and fate of traumatic subdural hygroma. Br J Neurosurg. 1994;8:551–558. doi: 10.3109/02688699409002947. [DOI] [PubMed] [Google Scholar]
- 35.Lee KS, Doh JW, Bae HG, Yun IG. Relations among traumatic subdural lesions. J Korean Med Sci. 1996;11:55–63. doi: 10.3346/jkms.1996.11.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee KS, Shim JJ, Yoon SM, Doh JW, Yun IG, Bae HG. Acute-on-chronic subdural hematoma: not uncommon events. J Korean Neurosurg Soc. 2011;50:512–516. doi: 10.3340/jkns.2011.50.6.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liau LM, Bergsneider M, Becker DP. Pathology and pathophysiology of head injury. In: Youmans JR, editor. Neurological surgery. ed 4. Vol 3. Philadelphia: Saunders; 1996. pp. 1549–1594. [Google Scholar]
- 38.López B, Caro L, Pardiñas AF. Evidence of trepanations in a medieval population (13th-14th century) of northern Spain (Gormaz, Soria) Anthropol Sci. 2011;119:247–257. [Google Scholar]
- 39.Lv X, Li Z, Li Y. Prehistoric skull trepanation in China. World Neurosurg. 2013;80:897–899. doi: 10.1016/j.wneu.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 40.Marino R, Jr, Gonzales-Portillo M. Preconquest Peruvian neurosurgeons: a study of Inca and pre-Columbian trephination and the art of medicine in ancient Peru. Neurosurgery. 2000;47:940–950. doi: 10.1097/00006123-200010000-00028. [DOI] [PubMed] [Google Scholar]
- 41.Markwalder TM. Chronic subdural hematomas: a review. J Neurosurg. 1981;54:637–645. doi: 10.3171/jns.1981.54.5.0637. [DOI] [PubMed] [Google Scholar]
- 42.Missios S. Hippocrates, Galen, and the uses of trepanation in the ancient classical world. Neurosurg Focus. 2007;23:E11. doi: 10.3171/foc.2007.23.1.11. [DOI] [PubMed] [Google Scholar]
- 43.Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo) 2001;41:371–381. doi: 10.2176/nmc.41.371. [DOI] [PubMed] [Google Scholar]
- 44.Murata K. Chronic subdural hematoma may be preceded by persistent traumatic subdural effusion. Neurol Med Chir (Tokyo) 1993;33:691–696. doi: 10.2176/nmc.33.691. [DOI] [PubMed] [Google Scholar]
- 45.Naffziger HC. Subdural fluid accumulations following head injury. J Am Med Assoc. 1924;82:1751–1752. [Google Scholar]
- 46.Naganuma H, Fukamachi A, Kawakami M, Misumi S, Nakajima H, Wakao T. Spontaneous resolution of chronic subdural hematomas. Neurosurgery. 1986;19:794–798. doi: 10.1227/00006123-198611000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Ohno K, Suzuki R, Masaoka H, Matsushima Y, Inaba Y, Monma S. Chronic subdural haematoma preceded by persistent traumatic subdural fluid collection. J Neurol Neurosurg Psychiatry. 1987;50:1694–1697. doi: 10.1136/jnnp.50.12.1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oka H, Motomochi M, Suzuki Y, Ando K. Subdural hygroma after head injury. A review of 26 cases. Acta Neurochir (Wien) 1972. 1972;26:265–273. doi: 10.1007/BF01407072. [DOI] [PubMed] [Google Scholar]
- 49.Oppenheim H. Textbook of nervous diseases for physicians and students. ed 5. New York: Otto Schulze and Company; 1911. [Google Scholar]
- 50.Panourias IG, Skiadas PK, Sakas DE, Marketos SG. Hippocrates: a pioneer in the treatment of head injuries. Neurosurgery. 2005;57:181–189. discussion 181-189. doi: 10.1227/01.neu.0000163416.66374.48. [DOI] [PubMed] [Google Scholar]
- 51.Park CK, Choi KH, Kim MC, Kang JK, Choi CR. Spontaneous evolution of posttraumatic subdural hygroma into chronic subdural haematoma. Acta Neurochir (Wien) 1994;127:41–47. doi: 10.1007/BF01808545. [DOI] [PubMed] [Google Scholar]
- 52.Park HB, Lee CR, Kim SC. Chronic subdural hematoma superimposed on posttraumatic subdural hygroma: a report of three cases. J Korean Neurosurg Soc. 1990;19:126–130. [Google Scholar]
- 53.Park HR, Lee KS, Shim JJ, Yoon SM, Bae HG, Doh JW. Multiple Densities of the Chronic Subdural Hematoma in CT Scans. J Korean Neurosurg Soc. 2013;54:38–41. doi: 10.3340/jkns.2013.54.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parlato C, Guarracino A, Moraci A. Spontaneous resolution of chronic subdural hematoma. Surg Neurol. 2000;53:312–315. discussion 315-317. doi: 10.1016/s0090-3019(00)00200-7. [DOI] [PubMed] [Google Scholar]
- 55.Putnam TJ, Cushing H. Chronic subdural hematoma: its pathology, its relation to pachymeningitis hemorrhagica, and its surgical treatment. Arch Surg. 1925;11:329–393. [Google Scholar]
- 56.Quatrehomme G, Işcan MY. Postmortem skeletal lesions. Forensic Sci Int. 1997;89:155–165. doi: 10.1016/s0379-0738(97)00113-8. [DOI] [PubMed] [Google Scholar]
- 57.Rabe EF, Flynn RE, Dodge PR. A study of subdural effusions in an infant. With particular reference to the mechanisms of their persistence. Neurology. 1962;12:79–92. doi: 10.1212/wnl.12.2.79. [DOI] [PubMed] [Google Scholar]
- 58.Rosen HM, Simeone FA. Spontaneous subdural hygromas: a complication following craniofacial surgery. Ann Plast Surg. 1987;18:245–247. doi: 10.1097/00000637-198703000-00012. [DOI] [PubMed] [Google Scholar]
- 59.Sankhyan AR, Weber GHJ. Evidence of surgery in Ancient India: trepanation at Burzahom (Kashmir) over 4000 years ago. Int J Osteoarchaeol. 2001;11:375–380. [Google Scholar]
- 60.Sato S, Suzuki J. Ultrastructural observations of the capsule of chronic subdural hematoma in various clinical stages. J Neurosurg. 1975;43:569–578. doi: 10.3171/jns.1975.43.5.0569. [DOI] [PubMed] [Google Scholar]
- 61.Schachenmayr W, Friede RL. The origin of subdural neomembranes. I. Fine structure of the dura-arachnoid interface in man. Am J Pathol. 1978;92:53–68. [PMC free article] [PubMed] [Google Scholar]
- 62.Seo DH, Lee KS, Shim JJ, Yoon SM. Multiple episodes of hemorrhage identified in MRI of chronic subdural hematomas. Korean J Neurotrauma. 2014;10:22–25. doi: 10.13004/kjnt.2014.10.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sohn IT, Lee KS, Doh JW, Bae HG, Yun IG, Byun BJ. A prospective study on the incidence, patterns and premorbid conditions of traumatic subdural hygroma. J Korean Neurosurg Soc. 1997;26:87–93. [Google Scholar]
- 64.Stone JL, Miles ML. Skull trepanation among the early Indians of Canada and the United States. Neurosurgery. 1990;26:1015–1019. discussion 1019-1020. doi: 10.1097/00006123-199006000-00016. [DOI] [PubMed] [Google Scholar]
- 65.Sun TF, Boet R, Poon WS. Non-surgical primary treatment of chronic subdural haematoma: preliminary results of using dexamethasone. Br J Neurosurg. 2005;19:327–333. doi: 10.1080/02688690500305332. [DOI] [PubMed] [Google Scholar]
- 66.Taarnhoj P. Chronic subdural hematoma; historical review and analysis of 60 cases. Cleve Clin Q. 1955;22:150–156. doi: 10.3949/ccjm.22.4.150. [DOI] [PubMed] [Google Scholar]
- 67.Taguchi Y, Nakamura N, Sato J, Hasegawa Y. [Pathogenesis of chronic subdural hematoma. Sequential study with computerized tomography (author's transl)] Neurol Med Chir (Tokyo) 1982;22:276–282. doi: 10.2176/nmc.22.276. [DOI] [PubMed] [Google Scholar]
- 68.Takahashi Y, Mikami J, Sato H, Takeda S, Matsuoka T, Ito K, et al. [Analysis of chronic subdural hematoma based on CT (Part 2). Symptoms and CT findings (author's transl)] Neurol Med Chir (Tokyo) 1982;22:395–401. doi: 10.2176/nmc.22.395. [DOI] [PubMed] [Google Scholar]
- 69.Trotter W. Chronic subdural hæmorrhage of traumatic origin, and its relation to pachymeningitis hæmorrhagica interna. Br J Surg. 1914;2:271–291. [Google Scholar]
- 70.Tullo E. Trepanation and Roman medicine: a comparison of osteoarchaeological remains, material culture and written texts. J R Coll Physicians Edinb. 2010;40:165–171. doi: 10.4997/jrcpe.2010.215. [DOI] [PubMed] [Google Scholar]
- 71.Velasco-Suarez M, Bautista Martinez J, Garcia Oliveros R, Weinstein PR. Archaeological origins of cranial surgery: trephination in Mexico. Neurosurgery. 1992;31:313–318. discussion 318-319. doi: 10.1227/00006123-199208000-00017. [DOI] [PubMed] [Google Scholar]
- 72.Verano JW. Trepanation in prehistoric South America: geographic and temporal trends over 2000 years. In: Arnott R, Finger S, Smith CUM, editors. Trepanation: history, discovery, theory. Leiden: Swets & Zeitlinger; 2003. pp. 223–236. [Google Scholar]
- 73.Watanabe S, Shimada H, Ishii S. Production of clinical form of chronic subdural hematoma in experimental animals. J Neurosurg. 1972;37:552–561. doi: 10.3171/jns.1972.37.5.0552. [DOI] [PubMed] [Google Scholar]
- 74.Watters DA. Skull trepanation in the Bismarck archipelago. P N G Med J. 2007;50:20–24. [PubMed] [Google Scholar]
- 75.Weigel R, Krauss JK, Schmiedek P. Concepts of neurosurgical management of chronic subdural haematoma: historical perspectives. Br J Neurosurg. 2004;18:8–18. doi: 10.1080/02688690410001660418. [DOI] [PubMed] [Google Scholar]
- 76.Weir B. Oncotic pressure of subdural fluids. J Neurosurg. 1980;53:512–515. doi: 10.3171/jns.1980.53.4.0512. [DOI] [PubMed] [Google Scholar]
- 77.Weir B. The osmolality of subdural hematoma fluid. J Neurosurg. 1971;34:528–533. doi: 10.3171/jns.1971.34.4.0528. [DOI] [PubMed] [Google Scholar]
- 78.Wetterling T, Demierre B, Rama B, Nekic M. Protein analysis of subdural hygroma fluid. Acta Neurochir (Wien) 1988;91:79–82. doi: 10.1007/BF01400533. [DOI] [PubMed] [Google Scholar]
- 79.Whang K, Hu C, Hong SK, Kim HJ, Han YP, Pyen JS. Clinical analysis of chronic subdural hematoma originated from traumatic subdural hygroma. J Korean Neurosurg Soc. 1993;22:898–904. [Google Scholar]
- 80.Wilberger JE. Pathophysiology of evolution and recurrence of chronic subdural hematoma. Neurosurg Clin N Am. 2000;11:435–438. [PubMed] [Google Scholar]
- 81.Yamada H, Nihei H, Watanabe T, Shibui S, Murata S. [Chronic subdural hematoma occurring consequently to the posttraumatic subdural hygroma--on the pathogenesis of the chronic subdural hematoma (author's transl)] No To Shinkei. 1979;31:115–121. [PubMed] [Google Scholar]
- 82.Yamada H, Watanabe T, Murata S, Shibui S, Nihei H, Kohno T, et al. Developmental process of chronic subdural collections of fluid based on CT scan findings. Surg Neurol. 1980;13:441–448. [PubMed] [Google Scholar]
- 83.Yamashima T, Yamamoto S. Clinicopathological classification of chronic subdural hematoma. Zentralbl Neurochir. 1985;46:304–314. [PubMed] [Google Scholar]
- 84.Yoon JW, Park IS, Park H, Kang DH, Park KB, Lee CH, et al. A study of the progression from acute subdural hematoma to chronic stage requiring surgical treatment. Korean J Neurotrauma. 2013;9:74–80. [Google Scholar]
- 85.Zanini MA, de Lima Resende LA, de Souza Faleiros AT, Gabarra RC. Traumatic subdural hygromas: proposed pathogenesis based classification. J Trauma. 2008;64:705–713. doi: 10.1097/TA.0b013e3180485cfc. [DOI] [PubMed] [Google Scholar]
- 86.Zollinger R, Gross RE. Traumatic subdural hematoma: an explanation of the late onset of pressure symptoms. J Am Med Assoc. 1934;103:245–249. [Google Scholar]