Abstract
Although the Family Health History (FHH) is the most cost-effective tool in the staratification of disense risk, it is not designed to collect information from non-biological family members (NBFM). Significant NBFM, defined as “fictive kin and othermothers,” tend to play a major role in the transmission of culture, health promotion, and decision-making; yet, their influence cannot be captured using the standard FHH. Participants attending the National Black Nurses Association (NBNA) 2012 genetic workshop were divided into groups to role-play FHH. All participants (N = 50) indicated difficulties with the standard FHH, ranking collection of sensitive data as the number 1 challenge. Consequently, a new symbol was developed with support from NBNA genetics workshop participants. Having such a symbol afforts an apportunity for inclusion of all NBFM to help guide risk-specific recommendations for disense management, prevention, and health promotion of common chronic diseases. This report will describe the process, presentation, and adoption of the symbol.
Keywords: community mothers, culture, epigenetics, family history, nurses
Introduction
A medical pedigree is a graphic presentation of a family’s health history and genetic relationships and it has been a pivotal tool in the practice of medical genetics for nearly a century (Bennett, 1999, 2000). With the mapping of the human genome and the increasing role of genetics in daily medical practice, recording and interpreting a pedigree should be a standard competency of all health professionals. ln 200 the U.S. Surgeon General announced the Family Health Initiative, a national campaign to promote the use of Family Health History (FHH) for disease pre and health promotion. The use of genetic information, particularly the FHH, has the potential to identify at-risk individuals and provide opportunities for education, prevention, and early diagnosis. In addition, FHH can lay the foundation for accurate risk perception and appropriately identify at-risk individuals for targeted, risk-reducing individual and community interventions (Guttmacher, Collins, & Carmona, 2004).
As the most cost-effective and commonly applied genetics/genomics tool in the stratification of disease risk at the community level (Yoon et al., 2002), the FHH has Jong been acknowledged as an important part of the medical examination and reflects the effects of genetic, environmental, and behavioral factors. It is a “low tech” powerful community health genomics tool that can predict risks and important risk factors fo a variety of disorders including coronary heart disease, cancer, and diabetes. More importantly, the understanding of personal risk factors provided by the FHH may benefit medically underserved populations who experience higher rates of morbidity and mortality associated with common chronic diseases (Bennett, French, Resta, & Doyle, 2008). Yet, the FHH is under-utilized by minority groups and few studies have examined the under-utilization of FHH among African-Americans or other ethnic populations. Given that most common complex diseases, such as diabetes and heart disease, disproportionately affect ethnic minorities and have both genetic and environmental components, community health interventions that utilize information from both risk factors promise to have higher impact. More importantly, the inclusion of knowledge from family members can guide risk-specific recommendations for disease management and prevention.
Prevention strategies for people with increased familial risk of common diseases could include lifestyle changes; more frequent screenings at earlier ages; and for those at highest risk, prophylactic procedures and surgeries (Scheuner, Yoon, & Khoury, 2004; Wattendorf & Hadley, 2005). However, the lack of involvement of family members in health promotion may hamper prevention strategies. Nonetheless, despite significant advances in understanding the human genome, the clinical utility of the genetic contribution to common chronic diseases has been limited in the current age of genomics (Grosse & Khoury, 2006). Moreover, the importance of FHH is becoming ever more apparent in risk stratification to develop personalized prevention strategies (Collins & McKusick, 2001). Although it is well documented that many common diseases such as diabetes, obesity, and cancer duster within ethnic families as a result of shared environment and genetics, the clinical utility of genetic contribution to common chronic diseases has been limited, especially among racially marginalized groups.
The African-American Family
There have been many attempts to define and conceptualize the family as a unit from multiple perspectives by numerous disciplines. Each discipline has its own point of reference for viewing the family and all have appreciation for the diversity of definitions. The narrow definition by the U.S. Census Bureau (two or more people living together and related by birth, marriage, or adoption) excludes extended families. However, for this report, we chose to use the definition from the 1981 White House Conference on Aging, “a family is a system of related and unrelated individuals integrated by pattern of social relationship and mutual help.”
Historical (Pre-Slavery) Evidence of Fictive Kinship Ties Among Black Americans
The classic work by Guttman (1976) notes considerable evidence for the practice of establishing fictive kinship ties and status among African-Americans. Persons from various West African cultures viewed kinship as the normal idiom of social relations. For example, parents and other adults taught children to address older persons who were unrelated to them by either blood or marriage as “Aunt” or “Uncle.” Many enslaved Africans replaced their absent extended family with “fictive kin,” from the same ethnic or national community to perform the role of absent family members. In fact, kinship obligations were extended beyond customary adult-child relationships to encompass both unrelated adults and unrelated children within slave communities. In some instances, family systems consisted entirely of non-blood members, with share points of view and belief systems, and others a combination that influenced lifestyle risk behaviors of the blood members. These fictive kin relationships functioned to integrate adults into informal supportive networks that surpassed formal kin obligations conventionally prescribed by blood or marriage. Moreover, the practice of informal adoption of enslaved children speaks to the salience of fictive kinship relations (Guttman, 1976).
Purpose of the Study
A growing body of research has documented the existence of extensive kinship networks within African-American and other ethnic communities as well as the importance of these networks as sources of informal social support (Guttman, 1976). Guttman (1976) noted that fictive kin relationships are an integral component of these networks, and indeed, extending kinship status to friend relationships is a means to expand one’s social network. Many of the rights and statuses usually associated with kinship are accorded to participants in these relationships. However, with the designation of fictive kin status comes both respect and responsibility and fictive kin are expected to participate in the duties and decisions of the extended family. Despite the importance of fictive kin ties in the maintenance and functioning of the extended family networks of African-Americans, little is known about fictive kin generally, and quantitative evidence to examine the impact of fictive kin on decision-making and health promotion is lacking. The current study, the first of its kind, seeks to describe the process, presentation, and adoption of a cultural symbol for inclusion of non-biological family members in the FHH.
Fictive Kin and Othennothers
Briefly defined, fictive kinship involves the extension of kinship obligations and relationships to individuals specifically not otherwise included in the kinship universe. Development of the fictive family structure among African-Americans resulted as a survival adaptation and does not conform to what is considered the ideal nuclear structure (Billingsley, 1968, 1992). Some of the cultural distinctiveness of African-American families may extend back to pre-slavery when enslaved Africans brought cultural patterns such as extended families to the United States. This family structure dynamic is the inclusion of fictive kin as socially and emotionally significant entities within the African-American family structure. Moreover, fictive ties are as important as, or more important than, comparable relationships created by blood, marriage, or adoption. Fictive relationships serve to broaden mutual support networks, create a sense of community, and enhance social control. Today fictive kin persists as a form of extended kin for pooling resources, extending familial networks, and extending social support among many ethnically marginalized families.
Othermothers and Extended Families
Similar to fictive kin, the institution of othermothers was a common practice in African-American communities. The term connotes functioning within the parameters of a biological maternal figure by a female individual with no biological ties to the family unit. Individuals indoctrinated as kin in this way become part of an extended family network, with expectations of obligation equal to those of blood-relatives (Chatters, Taylor, & Jayakody, 1994; Taylor, Chatters, Woodward, & Brown, 2013). In “Black Women and Motherhood,” Collins (2000) describes othermothers as women, including mothers, who provide care for children who are not biologically their own. Othermothering could manifest as providing a meal, essentially adopting the child, or simply supplying guidance. Collins further explains othermothers as women who hold the family infrastructure together or provide unity within the family by virtues of caring, ethics, teaching, and community services. Othermothers can be sisters, aunts, neighbors, grandmothers, cousins, or any other woman who steps in to relieve the stress of intimate mother-daughter relationships. More importantly these othermothers should not be ignored when trying to complete a FHH or advocate health promotion.
Re-Framing the Language
Non-biological family members, such as fictive kinship and othermothers, have been shown to play a central role in the transmission of health beliefs, health behaviors, and decision-making processes regarding health prevention, promotion, and intervention of their fellow kinsmen. Hall (2008) documented the importance of fictive kin to maintaining psychological health among African-American children of alcoholics. Among Samoan women, non-kin support was associated with positive lifestyle behaviors like engaging in exercise and weight loss strategies (Levy-Storms & Lubben, 2006). Kinship was an important factor in the creation and retention of family integrity among African-Americans during slavery and even though families may have been broken up in their initial transport to America, the enslaved Africans would ultimately forge kinship ties to others in blood and unrelated Africans.
In re-framing the discussion around African-Americans, we chose to use the cultural-variant perspective because it allowed us to view the African-American family as unique, functional, and to focus on family configuration that is based on needs for resources (Cain, 2005). It is important to note that the need for pooled resources is a deleterious consequence of social events such as involuntary immigration and enslavement, the informal adoption of slave-parented children, poverty, education, and economic inequality. These events created a need for an expansion of the family structure beyond mere social networking. The culturant variant view challenges the deficit model often used in research about the African-American family. In fact, it allowed us to view the function of the family unit differently in that all families do not seek or need a nuclear configuration of living (Guttman, 1976).
Recognizing the Need
There is a need for systematic collection of vital social-environmental data from non-blood kinships as they can influence epigenetics of disease. In a classic work by Watts-Jones (1997), she described two key family composition (functional, biological) structures of the African-American family dynamic relationship that carry great importance when gathering information for health promotion and decision-making.
Functional
Watts-Jones (1997) noted that functional relationships existed among both biological and non-biological members. She noted that functional kinship consisted of non-biological family members, such as an adopted child, and incorporated selected individuals into a biological or legally appointed family.
Biological
Similarly, the functional role of biological members was based on a true genetic or blood connection. For example, a biological grandmother may function as a mother to her abandoned grandchild. Although the FHH is structured to produce a narrative health profile of several generations of blood-relatives that enables health professionals to link chronic conditions that run in biologically linked families, it is not designed to capture pertinent information from functional kinship and/or functional biological members. In fact, the standardization symbols in the FHH pedigree schematic do not give recognition to the culturally sensitive role of non-biological members when gathering information from the proband.
Without recognition of the non-biological influence of the othermothers and fictive kin, pertinent risk evidence for the links between disease risk and the environment may well be inhibited (Feero, Bigley, Brinner, & Family Health History Multi-Stakeholder Workgroup of the American Health Information, 2008). These exclusions could compromise data sensitivity and specificity that could weaken the capacity of the assessment tool to link multifactorial diseases and environment (Feero et al., 2008; Reid, Walter, Brisbane, & Emery, 2009). More importantly, population specific usability issues related to obtaining a FHH from African-American families have been identified as a challenge when constructing a FHH regarding non-biological family members.
Link between Non-Biological Family and Disease
Fictive kin and othermothers have long been revered in African-American communities. Although not related via a biological basis, they have long fulfilled the role of kinship, resulting in imparting family culture, structure, patterns, shared environment, common health behaviors, food habits, genetic susceptibilities, and information. The capture of data on environmentally influenced potential risk traits becomes increasingly significant for populations in which behavior nuances resulting from cultural differences contribute to the health and well being of its family members. Symbols that capture the effect of culturally influenced alternative family structures, such as the fictive kinship bonds, on environmental practices that have an effect on the manifestation of multifactorial diseases have yet to be developed. To this end, we proposed the adoption of a symbol that will capture information from non-biological family members known as “fictive kin” and “othermothers.”
Creating a symbol that is sensitive to the dynamics of African-American family style provides an inclusive approach to gathering genetic/genomic information and decision-making from all family members. This article describes the process of identifying, post development and acceptance, of a symbol that represents non-biological contributions to the development of common diseases and health promotion.
Methodology
The National Black Nurses Association (NBNA) is a profesional nursing organization organized on 1971 and currently represents over 150,00 African-American nurses. Each year the organization hosts an annual conference in different cities within the United States. Annual Institutes on Diabetes, Women’s Health, and Cancer are held and revered by the membership. In 2006, the first Genetics/Genomics Institute was held with financial support from Vence Bonham, Senior Advisor to the National Institutes of Health/National Huwan Genetics Research Institute (NIH-NHGHl) and support from the NBNA leadership. Attendance ranged from 45 to over 100 participants. Although a pre- and post-test were not administered to the participants, the conference evaluation documented continued support fo the institute.
Descriptive Analysis
This report will describe some key features of data collection from 2008 to 2012 and provide a simple summary from a sub-sample of nurses attending the genetic workshops. More importantly, we present information regarding the development and acceptance of a symbol to capture the influence of non-biological family members.
Data Collection Phase 1
In 2008, a pilot survey was administered to the Board of Directors to evaluate the interest and knowledge of genetics and genomics among African-American nurses. This was the first survey administered to minority nurses regarding genetic/genomics. Survey results revealed that 96% (N = 74) believed that family pedigree could help identify at-risk African-American families. Over 50% (n = 43/74) believed that Family Health History could be used as a tool to teach patients about the significance of genetics and disease prevention. Further, the majority believed that the current method of gathering information about health and social relationships from non-biological family members was inadequate (Spruill, Coleman, & Collins-McNeil, 2009
Data Collection Analysis Phase 2
Data were collected and analyzed from a convenience sample of 384 nurses (N = 384) attending the 2009 annual conference in Las Vegas, Nevada. The sample consisted of practicing and retired registered nurses and licensed vocational-practical nurses of African heritage from the United States, the Eastern Caribbean, and Africa. Overall, the results mirrored the findings from 2008 survey data from the NBNA leadership. Over 90% (n = 346/384) reported that family pedigree could help identify at-risk African-American families, and the majority believed that the current method to gather information about health and social relationships was inadequate (Powell-Young & Spruill, 2013).
Participants were asked about genetic conditions manifested as chronic diseases within their families and survey results indicated the following: diabetes mellitus (64.8%), kidney disease (31.5%), cancer (31.8%), Alzheimer’s (25.3%), and mental retardation (22.7%). In spite of the desire that new treahnent strategies would emerge from disparities that disproportionately affect African-Americans, research indicated that African-Americans were not well represented in health-related research, especially in genetic research studies. Nurses from the 2009 NBNA study cited concerns for discrimination and mistrust with researchers as a viable reason for lack of participation. However, 84% (n = 323/384) of the sample felt strongly that African-Americans should participate in genetic and genomic research, as the benefits outweigh their concerns (Powell-Young & Spruill, 2013).
In 2010, the National Coalition of Ethnic Minority Organizations (NCEMNA) in collaboration with the National Institutes of Health, the National Cancer Institute (NCI), the Center for Cancer Research, and the National Human Genome Research Institute (NHGRI) embarked on an initiative to determine the interest of minority nursing organizations with respect to genomic topics and how ethnic minority nurses’ utilized genetic/genomic core concepts in their practice. The survey was administered online with 389 respondents (N = 389) and were included in the data analysis. Participant characteristics of the four participating organizations included: the Asian American/ Pacific Islander Nurses Association, Inc., the Philippine Nurses Association of America, Inc., the Nationnal Black Nurses Association, Inc., and the National Association of Hispanic Nurses. Of the sample, the majority 74% (n = 288/389) had completed a family history for themselves and 51% (n = 198/389) had completed a family history for a family member. Ninety-five percent indicated that the use of family history could identify at-risk families. However, half of the respondents (50%) reported fair to poor knowledge related to genetics of common diseases. When asked about the value of nurses being educated regarding how to complete a family history, 98% of the respondents believed it was either very important or somewhat important. Only 35% (n = 136/389) of the respondents reported taking a genetics course since licensure and 81% (n = 315/389) would attend training if offered at their annual conferences (Coleman et al., 2014). During that same year, the authors introduced the symbol and explained it at the genetics workshop conducted at the NBNA conference.
Data Results Phase 3
The following year (2011), the authors recruited a subset of 50 African-American nurses (N = 50) who had previously attended the NBNA genetic institute to define and rank issues that would influence gathering perceived sensitive genetic information from African-American clients. Workshop convenors (IS, BC) provided an explanation and purpose for the session. Participants were encouraged to ask questions and allowed time to provide a verbal consent. All participants were given verbal instruction on how to complete a three-generation FHH and participated in role-playing. The nurses were divided into 5 groups of 10, and within each group, participants were further divided into 5 teams of 2. Case studies that included fictive kin and othermothers were then provided. Each pair consisted of a nurse role-playing as an interviewer and a patient who had a non-biological family member. The interviewer was expected to conduct a standard FHH that incorporated an important non-biological family member. Once the exercise was completed, the group reassembled to provide feedback. Participants reported on the most influential impediments to obtaining a FHH within the African-American population and ranked them according to importance (See Table 1).
Table 1.
Ranking of Items
| Rank | Prioritized Themes | Ranked as Important in Gathering Genetic/Genomic Information from AA Families |
|---|---|---|
| 1 | Characteristics of African-American families (“Fictive Kin”) “Othermothers” not captured in current pedigree nomenclature |
50/50 |
| 2 | Providers need to acknowledge the feeling of “altruism” among AA families when promoting their health and the health of other family members |
50/50 |
| 3 | Unexpected parenting information can be a barrier | 30/50 |
| 4 | Privacy issues, and confidentiality were of grave concerns | 30/50 |
Nurses who role-played as an interviewer spoke of the difficulty of using the standard FHH form to elicit information relating to important non-biological family members. For example, during the role-play, when asked about the illness of her biological mother, one participant stated, “I was not raised by my biological mother.” Another stated, “My cousin mom raised me and my cousins and we are all brothers and sisters.” The interviewers shared that they really did not know how to incorporate this knowledge into the standard FHH pedigree and felt a sense of frustration. The concept of creating a symbol as a strategy to support inclusivity of the cultural differences of African-American families was discussed and supported by the group. The highest ranked items (lack of inclusion fo non-biological family members) among others are listed in Table 1.
Eliciting sensitive genetic information can be problematic in families and even more so within African-American families because of mistrust of the medical community, concerns with violations and misuse of privacy, and “outside” sharing of confidential family issues. Creating a symbol that is sensitive to the dynamics of African-American families while providing an inclusive approach to gathering perceived sensitive genetic material seemed beneficial. The new symbol was researched and designed by the authors to capture the unique pattern and cultural influences of non-biological kinship. Notably, there was overwhelming support for the symbol, but time constraints limited the discussion to fully evaluate the utility of the symbol within the groups. However, there was consensus among the participants that the authors should continue to work with the symbol and provide follow up at subsequent NBNA sponsored genetic workshops.
Symbol
The symbol was adapted from Ejagham people of Nigeria and consists of two round circles representing family unity, shared decision-making, and health promotion. Double lines that signify inclusion of non-biological family members connect the half circle. Placed above and below the double lines is a symbol to denote gender. The Square represents the male gender and a Circle represents the female gender (Figure 1). Further work is planned to test the impact of the symbol among African-American clinicians during the 2014 ProGene genetic workshop. Moreover, the authors believe that the use of the symbol may have utility for gathering sensitive genetic and genomic information from other populations. Such assumptions do require further testing in populations other than African-Americans, which is not the focus of this report (See Figure 1).
Figure 1.
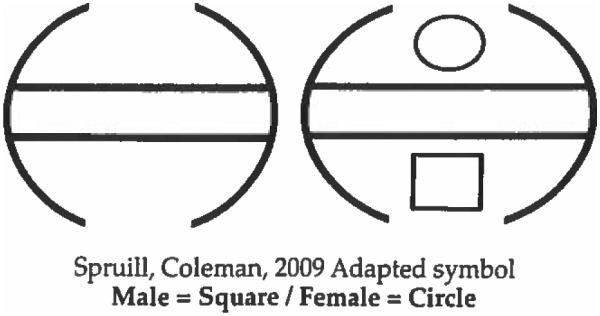
UNITY-Ejagham People of Nigeria (left) Adapted for African-American Family Pedigree (right)
Important Next Steps
The overall goal is to present and investigate the utility of the symbol to other ethnic groups and the ultimate goal is to make recommendations for inclusion of a symbol that represents non-biological family members to the Pedigree Standardization Task Force of the National Society of Genetic Counselors.
Discussion
Symbols used to gather information from a genetic pedigree that captures the effect of culturally influenced family structures from non-biological family members on decision-making and health promotion have yet to be developed. This report provides a summary of the NBNA investigators’ attempt to provide a cultural symbol to capture health and social data from important non-biological family members. This is important because genomics research is making significant contributions to the understanding of the biology and treatment of several human diseases. With varying degrees of success, genomics has also contributed to the development of new diagnostic tools and prevention strategies in the public health settings (Burke et al., 2010).
A high proportion of diseases with significant public health impact occur due to the interplay between the genetic and genomics of environmental factors. In this regard, conducting genomics research on diseases with strong environmental determinants is useful not only to identify genetic causes but also to improve public health approaches that aim to modify environmental risk factors (Burke et al., 2010). Genomics research may contribute to the latter by presenting evidence fo stratifying targeted populations by levels of genetic risk. More importantly, this approach has the potential to refine disease prevention strategies and treatments to specific populations more effectively (Khoury, Davis, Gwinn, Lindegren, & Yoon, 2005). Moreover, given that most common complex diseases have both genetic and environmental components, community health interventions that utilize information from both risk factors promise to have higher impact (Khoury et al., 2005). Therefore, inclusivity of all family members is important due to environmental factors and shared learned behaviors among family members.
Environmental factors, such as culture and lifestyle behavior choices, have been shown to increase the risk for common complex diseases among family members (Centers for Disease Control and Prevention of Genetics and Disease Prevention,2000; Olden & White,2005). Clearly, it is well documented that many common diseases such as diabetes, obesity, and cancer cluster within families as a result of a shared environment and genetics (Korf, 2013). Common diseases that result from complex interactions among shared genetics and familial-influenced environmental characteristics are labeled multifactorial inheritance (Nussbaum, Mcinnes, & Willard, 2007; Peiper & Strayer, 2014). Understanding the multifactorial inheritance of these common diseases does not include the influence from non-biological family members, and some researchers suggest the need for an expanded role of the FHH. This expanded role would help to detect, diagnose, and predict multifactorial patterns associated with common diseases (Brock, Allen, Keiser, & Langlois, 2010; Doerr & Teng, 2012; Valdez, Yoon, Qureshi, Green, & Khoury, 2010; Wattendorf & Hadley, 2005).
Typically structured to produce a narrative health profile from several generations of blood-relatives, the FHH enables health professionals to link chronic conditions that run in biologically link families. Because there is little item standardization for the PHH, some questionnaires may not contain elements that generate pertinent risk evidence for the links between disease risk and the environment (Feero et al., 2008). These exclusions could compromise data sensitivity and specificity that could weaken the capacity of the assessment tool to link multifactorial diseases (Feero et al., 2008; Reid et al., 2009). Furthermore, the illustration and interpretation of unique non-blood kinships have been identified as a challenge when constructing a FHH. In fact, the nomenclature and symbology fo adoption and marital status pedigree standardization does not easily lend it to address the complexities of non-biological ties or culturally influenced environmental factors that may influence multifactorial disease risk (Bennett et al., 2008; Bennett et al., 1995).
Symbols that capture the effect of fictive kinship bonds on environmental practices and manifestation of multifactorial diseases have yet to be developed. Cultural anthropologists have recorded family systems that exist among diverse ancestral groups (Guttm 1976). The capture of data on environmentally influenced potential risk traits becomes increasingly significant for populations where behavior nuances resulting from cultural differences contribute to the health and wellbeing of its members.
Implications
It is important to remember that development of the fictive family structure among African-Americans resulted as a survival adaptation and does not conform to what is considered the ideal nuclear structure (Billingsley, 1968, 1992). The importance of non-biological fictive kin to African-Americans must be noted when gathering sensitive information during the family history taking. Furthermore, centrality of fictive kinship within the African-American community complicates the investigation of consanguinity.
To this end, the interviewer must navigate an often-uncharted pathway of real and perceived family members to achieve a level of sophistication about the broad diversity of family structure. It is not uncommon for the members of the family to collude in a narrative that is an intricate mix of biological relationships and deeply intimate emotional relationships. We recommend that language reflect and honor family designations as described by the proband. For example, if a particular proband describes a non-biological fictive kin as “Auntie,” then the interviewer needs to use the same terms. In addition, when symbolizing this family relationship through graphs or charts, there needs to be a symbol that recognizes and/or captures the fictive kin. The authors believe that the symbol presented in this paper provides a viable option for capturing the importance of non-biological kin when gathering family history from African-Americans.
Conclusions
As a clinical resource, genetic risk assessment instruments that adequately and consistently address familial and environmental risk factors for common diseases are scarce. The availability of genetic risk assessment methods that aid prevention and early detection modeling for common diseases could positively impact clinical decision making, clinical outcomes, and personalization of healthcare from primary care through genetics-based specialty services. Many barriers exist to the accurate and complete collection and application of the FHH, especialy as it relates to non-biological family members. For example, population-specific usability issues related to the FHH have been identified. Most notably with the FHH there is the need for systematic generation of vital social and environmental data from non-biological family members. The increasing disparities of common diseases among specific populations substantiate the need for uncomplicated instruments that nursing and other health professionals can utilize to evaluate multifactorial (genetics, behavioral, and environmental) susceptibility in the practice setting. Policy statements from the American Nurses Association and competency guidelines disseminated by key health organizations such as the NBNA can provide plausibility for the usefulness of the FHH in the clinical arena beyond identification of inheritance risks, to the identification and contribution of non-biological family members in decision-making.
As an organization, we recommend regular and continued review of the FHH to determine if additional symbols are needed to accommodate changes in clinical practice. More importantly, to ensure that the symbols continue to meet the needs of health professionals and researchers as well as adhere to evolving ethical, family style, and privacy standards. All health professionals should be made aware of the clinical utility of using a common symbol to represent non-biological kinship in clinical practice and publication. Our task as a national health advocacy organization is to first access the utility of the symbols among the membership and to make appropriate recommendations to the Pedigree Standardization Task Force (PSTF), the Pedigree Standardization Work Group (PSWG) of the National Society of Genetic Counselors (NSGC).
Acknowledgements
Research reported in this article was supported by the following: (1) National Institute of Diabetes and Digestive and Kidney Disease (NIDDK/Diversity Supplement, R01-DK084350). (2) Dr. Coleman is supported in part by the National Center for Advancing Translational Sciences (NCATS), through NIH Grant Number UL1TR000124. (3) Dr. Magwood is supported in part by the National Institute for Nursing Research (NINR/NIH- 5KOINR013195). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to thank the leadership and membership of the NBNA for their unwavering support and acknowledge the contribution Dr. Sandra Millon Underwood for the 2012 Pre-Genetics Institute.
References
- Bennett RL. The practical guide to the genetic family history. Wiley; New York: 1999. [Google Scholar]
- Bennett RL. Pedigree parables. Clinical Genetics. 2000;58(4):241–249. doi: 10.1034/j.1399-0004.2000.580401.x. [DOI] [PubMed] [Google Scholar]
- Bennett RL, French KS, Resta RG, Doyle DL. Standardized human pedigree nomenclature: Update and assessment of the recommendations of the National Society of Genetic Counselors. Journal of Genetic Counseling. 2008;17(5):424–433. doi: 10.1007/s10897-008-9169-9. doi:l0.1007/sl0897-008-9169-9. [DOI] [PubMed] [Google Scholar]
- Bennett RL, Steinhaus KA, Uhrich SB, O’Sullivan CK, Resta RG, Lochner-Doyle D, Hamanishi J. Recommendations for standardized human pedigree nomenclature. Journal of Genetic Counselling. 1995;4(4):267–279. doi: 10.1007/BF01408073. doi:l0.1007/BF01408073. [DOI] [PubMed] [Google Scholar]
- Billingsley A. Black families in white America. Prentice-Hall; Engle-wood Cliffs, NJ: 1968. [Google Scholar]
- Billingsley A. Climbing Jacob’s ladder: The enduring legacies of African-American families. Simon and Schuster; New York: 1992. [Google Scholar]
- Brock JA, Allen VM, Keiser K, Langlois S. Family history screening: Use of the three generation pedigree in clinical practice. Journal of Obstetrics and Gynaecology Canada. Journal d’Obstétrique et Gynecologie du Canada. 2010;32(7):663–672. doi: 10.1016/s1701-2163(16)34570-4. [DOI] [PubMed] [Google Scholar]
- Burke W, Burton H, Hall AE, Karmali M, Khoury MJ, Knoppers B, Ickworth Group Extending the reach of public health genomics: What should be the agenda for public health in an era of genome-based and “personalized” medicine? Genetics in Medicine. 2010;12(12):785–791. doi: 10.1097/GIM.0b013e3182011222. doi:l0.1097/GIM.Ob013e3182011222. [DOI] [PubMed] [Google Scholar]
- Cain DS, Combs-Orme T. Family structure effects on parenting stress and practices in the African American family. Journal of Sociology and Social Welfare. 2005;32(2):19–40. [Google Scholar]
- Centers for Disease Control and Prevention of Genetics and Disease Prevention Gene-Environment Interaction Fact Sheet. 2000 Retrieved from: http://www.cdc.gov/genomics/famhistory/famhist_2009-10_findings.htm.
- Chatters LM, Taylor RJ, Jayakody R. Fictive kinship relations in black extended families. Journal of Comparative Family Studies. 1994;24(3):297–312. [Google Scholar]
- Coleman B, Calzone KA, Jenkins J, Paniagua C, Rivera R, Hong 0S, Spruill I, Bonham V. Multi-ethnic minority nurses’ knowledge and practice of genetics and genomics. Journal of Nursing Scholarship. 2014;46(4):235–244. doi: 10.1111/jnu.12083. doi:l0.1111/jnu.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins FS, McKusick VA. lmplication of the human genome project for medical science. Journal of the American Medical Association. 2001;285(5):540–544. doi: 10.1001/jama.285.5.540. [DOI] [PubMed] [Google Scholar]
- Collins PH. Black woman and motherhood. In: Collins PH, editor. Black feminist thought: Knowledge, consciousness, and the politics of empowerment. 2nd Routledge; New York: 2000. [Google Scholar]
- Doerr M, Teng K. Family history: Still relevant in the genomics era. Cleveland Clinic Journal of Medicine. 2012;79(5):331–336. doi: 10.3949/ccjm.79a.11065. doi:10.3949/ccjm.79a.11065. [DOI] [PubMed] [Google Scholar]
- Feero WG, Bigley MB, Brinner KM, Family Health History Multi-Stakeholder Workgroup of the American Health Information Community New standards and enhanced utility for family health history information in the electronic health record: an update from the American Health Information Community’s Family Health History Multi-Stakeholder Workgroup. Journal of the American Medical Informatics Association. 2008;15(6):723–728. doi: 10.1197/jamia.M2793. doi:l0.1197/jamia.M2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse SD, Khoury MJ. What is the clinical utility of genetic testing? Genetics in Medicine. 2006;8(7):448–450. doi: 10.1097/01.gim.0000227935.26763.c6. doi:10.109701.gim.0000227935.26763.c6. [DOI] [PubMed] [Google Scholar]
- Guttmacher AE, Collins FS, Carmona RH. The family history—More important than ever. New England Journal of Medicine. 2004;351(22):2333–2336. doi: 10.1056/NEJMsb042979. doi:10.1056/NEJMsb042979. [DOI] [PubMed] [Google Scholar]
- Guttman HG. The black family in slavery and freedom. Random House; New York: 1976. pp. 226–228. 1750-1925. [Google Scholar]
- Hall JC. The impact of kin and fictive kin relationships on the mental health of black adult children of alcoholics. Health and Social Work. 2008;33(4):259–266. doi: 10.1093/hsw/33.4.259. [DOI] [PubMed] [Google Scholar]
- Khoury MJ, Davis R, Gwinn M, Lindegren ML, Yoon P. Do we need genomic research for the prevention of common diseases with environmental causes? American Journal of Epidemiology. 2005;161(9):799–805. doi: 10.1093/aje/kwi113. doi:l0.1093/aje/kwi113. [DOI] [PubMed] [Google Scholar]
- Korf BR, Irons MB, Irons MB. Multifactorial inheritance. In: Korf BR, editor. Human genetics and genomics. John Wiley & Sons, Ltd; New Jersey: 2013. pp. 87–99. [Google Scholar]
- Levy-Storms L, Lubben JE. Network composition and health behaviors among older Samoan women. fournal of Aging and Health. 2006;18(6):814–836. doi: 10.1177/0898264306293263. doi:l0.1177/0898264306293263. [DOI] [PubMed] [Google Scholar]
- Nussbaum RL, McInnes RR, Willard HF. Thompson & Thompson genetics in medicine. 7th Saunders Elsevier; Philadelphia: 2007. Genetics of common disorders with complex inheritance; pp. 151–176. [Google Scholar]
- Olden K, White SL. Health-related disparities: Influence of environmental factors. Medical Clinics of North America. 2005;89(4):721–738. doi: 10.1016/j.mcna.2005.02.001. doi:l0.1016/j.mcna.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Peiper S, Strayer DS. Developmental and genetic diseases. In: Rubin E, Reisner HM, editors. Essentials of Rubin’s pathology. Lippin-cott, Wilkins & Williams; Philadelphia: 2014. pp. 126–155. [Google Scholar]
- Powell-Young YM, Spruill IJ. Views of Black nurses toward genetic research and testing. Journal of Nursing Scholarship. 2013;45(2):151–159. doi: 10.1111/jnu.12015. doi:l0.1111/jnu.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid GT, Walter FM, Brisbane JM, Emery JD. Family history questionnaires designed for clinical use: A systematic review. Public Health Genomics. 2009;12(2):73–83. doi: 10.1159/000160667. doi:l0.1159/000160667. [DOI] [PubMed] [Google Scholar]
- Scheuner MT, Yoon PW, Khoury MJ. Contribution of Mendelian disorders to common chronic disease: Opportunities for recognition, intervention and prevention. American Journal of Medical Genetics. Part C: Seminars in Medical Genetics. 2004;125C(1):50–65. doi: 10.1002/ajmg.c.30008. doi:10.1002/ajmg.c.30008. [DOI] [PubMed] [Google Scholar]
- Spruill I, Coleman B, Collins-McNeil J. Knowledge, beliefs and practices of African-American nurses regarding genetics/genomics. Journal of National Black Nurses Association. 2009;20(2):20–24. [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Woodward AT, Brown E. Racial and ethnic differences in extended family, friendship, fictive kin and congregational informal support networks. Family Relations. 2013;62(4):609–624. doi: 10.1111/fare.12030. doi:10.1111/fare.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdez R, Yoon PW, Qureshi N, Green RF, Khoury MJ. Family history in public health practice: A genomic tool for disease prevention and health promotion. Annual Review of Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. doi:l0.1146/annurev.publhealth.012809.103621. [DOI] [PubMed] [Google Scholar]
- Wattendorf DJ, Hadley DW. Family history: The three-generation pedigree. American Family Physician. 2005;72(3):441–448. [PubMed] [Google Scholar]
- Watts-Jones D. Toward an African American genogram. Family Process. 1997;36(4):375–383. doi: 10.1111/j.1545-5300.1997.00375.x. [DOI] [PubMed] [Google Scholar]
- Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genetics in Medicine. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. doi:l0.109700125817-200207000-00009. [DOI] [PubMed] [Google Scholar]


