Considered one of the most intractable conflicts in history, hostilities between Palestine and Israel have been ongoing sporadically for 67 years and counting, since the formation of the Israeli state in 1948. The impact of a continuous state of war has left the Palestinian health system in a chronic state of disarray. Jimmy Carter, former American President declared,
The health situation in the Occupied Palestinian Territories shows the urgency of finding a political solution, as restraints and insecurities continue to undermine the creation of a health infrastructure able to address the dire public-health needs of Palestinians.1
One of the main constraints to the establishment of a functional healthcare system is a 708 kilometre long, 8 meters high wall, known as the “Separation Wall” (Figures 1 and 2).2 Deemed by successive Israeli governments to be a necessary protective mechanism for Israelis, the wall has led to the separation of the West Bank from Israel.3 Yet, despite suggestions to the contrary, the reality is that the barrier has had a devastating impact on 2.79 million people living in the West Bank and caused fragmentation of the region both physically and economically.4 Amongst other issues, the wall has contributed to the disruption of Palestinian access to land, livelihoods, education, water resources and has significantly inhibited freedom of movement across the West Bank.5 This in turn has generated deep seeded psychological and social harm to those living behind it.2 From a medical sense, the barrier acts as an obstacle to health, inhibiting the fundamental right of Palestinians to healthcare by restricting the movement of patients, doctors, ambulances and medications within the area.6 Importantly, it should be highlighted that the so-called “Separation Wall” is considered illegal under International Law.2&7
Fig 1.
Picture of the “Separation Wall” as taken from Abu Dis in the West Bank.
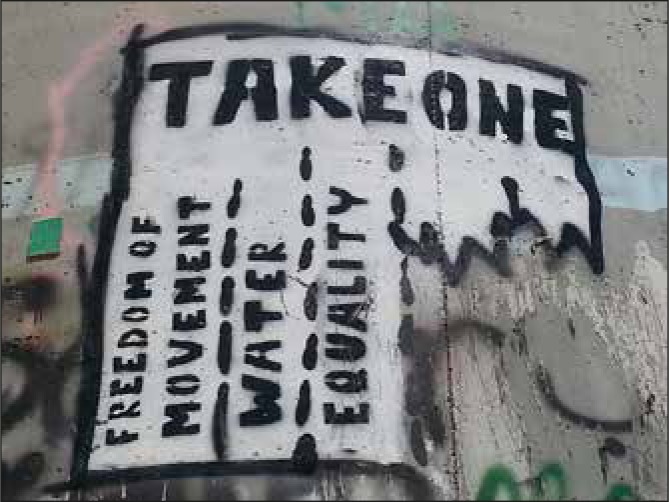
Fig 2.
Graffiti on the “Separation Wall” in Bethlehem, Palestine - highlighting issues as a result of the barrier.
Following the 1993 Oslo Peace Accords, the newly established Palestinian Authority (PA), functioning through the Ministry of Health (MOH), were given responsibility for the administration of health care in the region. Yet, the PA’s stewardship over health care administration is by-in large symbolic. The health care system remains subservient to Israel, with the Israeli state retaining ultimate control over healthcare budgets, border crossings, building permits and pharmaceutical import/exports.6 Consequently MOH hospitals are basic in comparison to hospitals within Israel and lacking many resources taken for granted in the UK, particularly those relating to imaging and specialist personnel. Doctors practising in the West Bank have limited opportunities for training and continued professional development due to imposed permit sanctions and accordingly, Palestine has 8 times fewer specialist doctors when compared with Israel.6
The physical implications of the path the wall has taken through the West Bank has resulted in the isolation of rural communities from health care amenities, leading to substandard local health care facilities, making “health” inaccessible to the most vulnerable in society.5 Costly travel expenses and lengthy journeys to hospital as a result of the wall hinders access for the impoverished, elderly and disabled. Consequently, there exists a heavy reliance on humanitarian aid organisations for healthcare however, limited communication between such agencies and the MOH fragments an already ailing infrastructure.
The impact of military occupation and the need for permits to pass through Israeli checkpoints generates additional access issues. At present there are more than 500 blockades, checkpoints and roadblocks affecting the freedom of movement within the West Bank.8 Palestinian patients must apply for permits to enter Israel for medical services not provided in the West Bank, namely oncological treatments. It is commonplace to suffer protracted delays in receiving a permit or to have an application declined. A World Health Organisation report released in 2013 stated, patients referred to Israel from the West Bank had permits denied in 17% of cases with no reason cited in one third of applications.9 Perhaps even more worryingly, statistics from the Palestinian Red Crescent Society (PRCS), the main ambulance supplier in the West Bank, reported 93% of its ambulance transfers with acutely unwell passengers experiencing “time consuming delays” of 10 minutes or longer at checkpoints due to Israeli security protocols.9 When taken together, this presents a bleak picture of Palestinian access to healthcare.
In February 2015, my husband and I took the decision to move to Bethlehem where I took up positions with two NGOs providing health care in the West Bank through mobile clinics. I work with the Palestinian organisation, Palestinian Medical Relief Society, Bethlehem (PMRS) 2-3 days a week and the Israeli organisation, Physicians for Human Rights (PHR) on a Saturday (Figures 3 and 4). PMRS have many branches in the region, each working locally whilst PHR provides services throughout the West Bank. Mobile clinics are used as a means of delivering free of charge primary level health care within communities where such facilities do not exist. These clinics have target areas, specifically those areas with the greatest restrictions on mobility and rural communities. Correspondingly these areas tend to be those with the highest levels of poverty and are more likely to be surrounded by settlements.10
Figure 3.
Typical facilities in a PHR mobile clinic visiting Azzun, Palestine.
Figure 4.
The author at a PHR mobile clinic in Azzun, Palestine.
The two organisations function differently and, as a volunteer present distinct challenges. Attending a PHR clinic can have logistical difficulties. I must travel a mere 8km to the meeting point in Jerusalem, yet navigating the “Separation Wall” has obvious access issues. What would be a 10 minute bus journey in Belfast can take over 1 hour, allowing for security checks though the “Beit Jala” checkpoint. PHR provide a clinic conducted solely by volunteers of Palestinian, Israeli and international backgrounds comprising physicians, nurses, allied health professionals, translators, pharmacists and alternative therapists. The variety of specialist physicians alters weekly. This group differs greatly from my colleagues at PMRS, a small cohort of 7 Palestinians (3 doctors, a nurse, a lab technician, a pharmacist, a driver) and myself. Our PHR delegation meet and travel in a convoy of 2 buses to the clinics. The director of the mobile clinic coordinates with local villages in need of health care and prioritises where the clinic will travel, attending a different town each week. More often than not, the clinics are based in the Northern regions of the West Bank as many towns here are completely isolated due to the “Separation Wall”.
PHR clinics are held within school buildings thus there are no formal examination areas and issues with privacy and confidentiality ensue. Patient numbers are large and space a premium. As a result two physicians may be required to practice within the same room, sometimes even sharing a translator. PMRS differs inasmuch as the clinics attend the same villages each week but the communities they serve experience extreme levels of poverty (Figure 5). The clinics are located in structures which lack windows, doors, heating and water and there remains little by way of examination areas or privacy. As expected, services at both clinics are basic and whilst an ultrasound machine is available for gynaecological exams from a medical perspective it is considered exceptional if a urine dipstix or ECG machine is available. It has thus become necessary to travel with my own equipment where possible, particularly a blood pressure cuff and glucometer.
Figure 5.
A PMRS clinic facility in an impoverished town on the outskirts of Bethlehem.
My role in both organisations involves working as a general internal physician or “Batini” in Arabic. Despite this I tend to review patients from a variety of other specialities, from orthopaedics to paediatrics. The clinic lasts 4-5 hours or until all the patients are seen. PMRS clinics, for many of the reasons listed above, regrettably do not have the same level of specialist physicians. Their clinics are comprised of one gynaecologist and two “general practitioners”. These doctors, like many Palestinian doctors have completed a 1 year internship, equivalent of the Foundation Programme in the UK, however many have been unable to enter into Residency Programmes given the restrictions on work permits by Israel and the lack of such programmes in the West Bank. The lack of training afforded to my colleagues in PMRS has on occasion become evident. This is not the case with highly trained Israeli physicians and frequently I have felt that teaching sessions between the two groups would achieve a greater long term benefit for the Palestinian health care system than just “bridging the health gap” on a weekly basis.
Lack of health insurance is a barrier to healthcare for many. Patients attend clinics for serious ailments only to ascertain if the required investigations are either inaccessible or impractical from a financial perspective. As a physician I have learnt to streamline my investigations, doing only what is absolutely necessary, be that the most basic investigation or that with the greatest diagnostic yield. Given the issues with access to health care, some patients present in the later stages of their illness or with florid clinical signs. Regrettably I have seen children with significant chronic kidney disease, adults with disseminated cancers and have diagnosed conditions including acromegaly, ankylosing spondylitis and Behcet’s disease.
Moreover, there is a limited selection of medications available for Palestinian patients compared with those living in Israel. Despite the high prevalence of type 2 diabetes, patients may only be treated with metformin or gliclazide prior to commencement of insulin. This is in stark contrast to myriad medications available in the UK. Whilst insulin is available, it is not free, which in turn creates obstacles when attempting to adequately treat patients. As such I have had to make alterations to my prescribing practices, suggesting herbal remedies such as ginger or cinnamon that have been proven to reduce blood glucose levels in conjunction with health education.11, 12 Familiarising myself with brand names and learning to simply make do with the available medications has been an additional challenge. I have become adept at converting between drug subtypes, be that a beta blocker or a steroid, ensuring an equivalent dosage to allow for ongoing administration when the patient’s “brand” has no longer been available. A situation I have never found myself in before.
“Inshallah” is a phrase heard commonly at clinics, translated it means “God willing”. At times, patients place their health “in God’s hands” accepting the outcome as predetermined. This ultimately contributes to a fatalistic acceptance of disease and death. Nevertheless, there remains a belief that there is a tablet for all ills and a doctor may be deemed incompetent if a prescription is not administered.13 In my time spent working here I have noted that a spectrum of preference exists with injections favoured over liquids or tablets, coloured pills preferred over uncoloured, and larger pills over smaller ones.13 Unquestionably this has led to patients on excessive volumes of medications, high levels of antibiotic use and patients prescribed treatments with no proven merit.
Behavioural risk factors such as tobacco and argila smoking, unhealthy diets and physical inactivity contribute greatly to ill-health.14 Non communicable diseases have significant prevalence in Palestine and formed the majority of my clinical work. In spite of the high levels of smoking however, the prevalence of patients with chronic obstructive pulmonary disease at mobile clinics has been low. Unfortunately, the same cannot be said for lung cancer, particularly in male patients. Amongst many of the patients I have met, smoking is considered part of manhood and a symbol of generosity.15 As a rite of passage, a father often gives their son their first cigarette, from age 11. Equally, I have been offered cigarettes as a gesture of thanks at clinics. Arab culture does not support the idea that many practices deemed ‘risky’ by the West have any bearing on health outcomes.15 Consequently, such cultural views mean the concepts of preventative medicine, health education and health promotion are non-existent in Palestine.
In fact, the first campaign of its kind entitled POSIT has only been planned for 2015, comprising a “bottom up approach” aimed at education of patients through primary health care and reinforced by widespread media coverage, although I remain dubious about the impact this will have in Palestine.16
The ongoing conflict, high levels of violence and a continued threat to people’s safety has, understandably, resulted in high levels of psychological stress.17, 18 That being said, when patients present at clinics they report their symptoms in terms of physical complaints rather than emotional or psychological symptoms. Adults frequently report generalised weakness, headache or palpitations whilst children have high rates of insomnia, bedwetting and night terrors. Moreover I have witnessed increased levels of disorders where one would identify “stress” as a risk factor, namely irritable bowel syndrome, migraine and gastritis. It has been suggested that in Arab culture, mental health problems are seen to be a punishment from God or an evil spirit from the devil.15 Patients are reluctant to openly discuss symptoms deemed to be psychological in nature, to accept psychiatric medication or seek formal psychiatric help due to the stigma associated with such a diagnosis. Families tend to conceal the fact that a member has a psychiatric illness for fear, amongst other things, that their daughters’ prospects for marriage will be jeopardised.15 The social stigma of mental health was most evident to me when the PMRS provided a clinic in an elderly care facility. I was astounded to find that patients with mental health problems, specifically schizophrenia, and elderly patients were nursed alongside each other. Of great concern is the fact that staff receive no training in the care of psychiatric patients and were expected to tend to patients whose ages ranged from 28 to 103.
Practicing medicine in Palestine has provided an invaluable opportunity to learn about medicine and healthcare in another culture. I faced challenges relating to cultural matters I previously had no experience with, most notably during Ramadan. Aside from having to alter my prescribing to accommodate periods of fasting, the prolonged duration of fasts created a specific set of presenting complaints, namely duodenal ulcers, duodenitis and syncope. I have been fascinated by the impact culture has, not only on a patient’s perception of health but in contributing towards ill health. Vitamin D deficiency is prominent in the female population, attributed to wearing of the hijab.19 Moreover the prevalence of congenital heart disease is above the UK average, related to the sizeable prevalence of consanguinity in the region.20 Poverty in Palestine is extreme, both in terms of the widespread nature of the problem and the levels of social deprivation people endure. I found this to be extremely upsetting. Many women and children present to the clinics thin and malnourished with deficiencies in B12, folate and iron due to their inadequate diets or conflictingly, present with obesity and nutrient deficiencies as food which is cheap is unfortunately higher in fat.
Working as an outsider, particularly as a female in a patriarchal culture, has been problematic on occasion. To work effectively in the rural communities required a level of trust to be established between myself and the patients. This required me to act as an observer to the local Palestinian doctors during my first PMRS clinics, allowing time for patients to become accustomed to my presence. Nonetheless occasionally men would not allow me to examine them physically due to their cultural beliefs; a challenging situation that necessitated alternatives to be carefully and sensitively negotiated so as to please all parties. I can think of one example when the patient was examined fully clothed whilst my male interpreter placed the stethoscope. On the other hand, some of my new habits generated as a result of my time here are more amusing, like my caffeine addiction. Coffee is used as a way to do business, to chat and as a sign of hospitality.21 Coffee was provided frequently during clinics by grateful patients as a gesture of thanks and participating in these coffee drinking rituals helped generate rapport. Similarly the use of a little arabic, even if horribly mispronounced was helpful in creating trust, putting a patient at ease and bridging the inevitable gap created through a translator.
Working with the mobile clinics in Palestine has been a privilege and an insightful experience both culturally and emotionally. The process has at times been difficult and often I felt the clinics to be an emotional rollercoaster. Feelings of immense frustration at being unable to contribute enough are all too familiar. The resilience of the Palestinian doctors working in such challenging circumstances has been truly humbling, and it is clear that ultimately the main challenge to the sustainability and long term improvement of the Palestinian health system is the ongoing conflict.
REFERENCES
- 1.Carter J. Peace and health in the occupied Palestinian territory. Lancet. 2009;373(9666):783–4. doi: 10.1016/S0140-6736(09)60106-9. [DOI] [PubMed] [Google Scholar]
- 2.Parry N. Is it a fence? Is it a wall? No, it’s a Separation Barrier. The Electronic Intifada [Internet] 2003 Aug; [about 4 p.] Available from: https://electronicintifada.net/content/it-fence-it-wall-no-its-separation-barrier/4715 Last accessed November 2015. [Google Scholar]
- 3.Bard M. West Bank Security: background and overview. The Jewish Virtual Library. [Internet]. Updated April 2015. Available from: http://www.jewishvirtuallibrary.org/jsource/Peace/fence.html Last accessed November 2015. Last accessed November 2015. [Google Scholar]
- 4.National Statistical Monitoring System. State of Palestine. Palestinian Central Bureau of Statistics. Ramallah, Palestine: Palestinian Ministerial Cabinet; 2015. Available from: http://www.pcbs.gov.ps/site/881/default.aspx#Population Last accessed November 2015. [Google Scholar]
- 5.Palestinian National Authority. The impact of annexation and expansion wall on the Palestinian environment. Ramallah, Palestine: Palestinian National Authority; 2010. Available from: http://www.lacs.ps/documentsShow.aspx?ATT_ID=6057 Last accessed November 2015. [Google Scholar]
- 6.Efrat M. Divide and conquer: inequality in health. Ramallah, Palestine: Physicians for Human Rights Israel; 2015. Available from: http://www.scribd.com/doc/256771352/Divide-Conquer-Inequality-in-Health-PHR-Israel Last accessed November 2015. [Google Scholar]
- 7.International Court of Justice. [Internet] Legal consequences of the construction of a wall in the Occupied Palestinian territory: Press release 2004/28. The Hague, Netherlands: 2004. Available from: http://www.icj-cij.org/docket/index.php?pr=71&code=mwp&p1=3&p2=4&p3=6. Last accessed November 2015.
- 8.The Israeli Information Center for Human Rights in the Occupied Territories. B’Tselem [Internet] 2011. Restriction of movement: checkpoints, physical obstructions, and forbidden roads. updated 2015. Available from: http://www.btselem.org/freedom_of_movement/checkpoints_and_forbidden_roads Last accessed November 2015. [Google Scholar]
- 9.The World Health Organisation. Cairo, Egypt: The World Health Organisation. 2014. The right to health - crossing barriers to access health in the occupied Palestinian territory; pp. 21–3. Available from: http://www.emro.who.int/images/stories/palestine/documents/WHO_-_RTH_crossing_barriers_to_access_health.pdf?ua=1 Last accessed November 2015. [Google Scholar]
- 10.Palestinian Central Bureau of Statistics (PCBS) and the World Bank. Seeing is believing; poverty in the Palestinian territories. Washington: The World Bank; 2014. pp. 29–30. Available from: http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2014/03/14/000333037_20140314125844/Rendered/PDF/860380WP0P12860rty0in0Palestine0web.pdf Last accessed November 2015. [Google Scholar]
- 11.Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care. 2003;26(12):3215–8. doi: 10.2337/diacare.26.12.3215. [DOI] [PubMed] [Google Scholar]
- 12.Daily JW, Yang M, Kim DS, Park S. Efficacy of ginger for treating Type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Ethnic Food. 2015;2(1):36–43. [Google Scholar]
- 13.Lipson JG, Meleis AI. Issues in health care of Middle Eastern patients. West J Med. 1983;139(6):854–61. [PMC free article] [PubMed] [Google Scholar]
- 14.Brosnahan T. Nargile(Turkish water pipe) Turkey Travel Planner. 2015 Available from: http://www.turkeytravelplanner.com/details/Tobacco/nargile.html Last accessed November 2015. [Google Scholar]
- 15.Hammad A, Kysia R, Rabah R, Hassoun R, Connelly M. Guide to Arab culture: health care delivery to the Arab American Community. Dearborn, Michigan: ACCESS Community Health Center Health Research Unit; 1999. Available from: http://www.naama.com/pdf/arab-american-culture-health-care.pdf Last accessed November 2015. [Google Scholar]
- 16.Directorate General of the Development Cooperation, Ministry of Foreign Affairs and International Cooperation. Strengthening the primaryhealth care system in Palestine. Sheikh Jarrah, Jerusalem: Department of Primary Health Care and Public Health Palestinian Ministry of Health; 2014. Available from: http://www.itcoop-jer.org/sites/default/files/booklet_POSIT_20_1_2015_FINAL.pdf Last accessed November 2015. [Google Scholar]
- 17.Punamaki R. Stress among Palestinian woman under military occupation; women’s appraisal of stressors, their coping modes, and their mental health. Int J Psychol. 1986;21(1-4):445–62. [Google Scholar]
- 18.Espié E, Gaboulaud V, Baubet T, Casas G, Mouchenik Y, Yun O, et al. Trauma related psychological disorders amongst Palestinian children and adults in Gaza and West Bank, 2005-2008. Int J Ment Health Syst. 2009;3(1):21. doi: 10.1186/1752-4458-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batieha A, Khader Y, Jaddou H, Hyassat D, Batieha Z, Khateeb M, et al. Vitamin D status in Jordan: dress style and gender discrepancies. Ann Nutr Metab. 2011;58(1):10–8. doi: 10.1159/000323097. [DOI] [PubMed] [Google Scholar]
- 20.Tayebi N, Yazdani K, Naghshin N. The prevalence of congenital malformations and its correlation with consanguineous marriages. Oman Med J. 2010;25(1):37–40. doi: 10.5001/omj.2010.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Browne BC, McBride RS. Politically sensitive encounters: ethnography, access and the benefits of “hanging out”. Qual Sociol Rev. 2015;11(1):33–48. [Google Scholar]