Abstract
Rationale
Excessive weight gain during pregnancy is a major determinant of later life obesity among both Black and Latina women and their offspring. However, psychosocial determinants of this risk, including everyday discrimination, and potential moderators of such effects remain unexplored.
Objective
We examined the influence of discrimination, a culturally relevant stressor, on odds of gaining weight beyond Institute of Medicine recommendations during pregnancy. Whether the effect was moderated by race/ethnicity, age, or depressive symptoms was also examined.
Method
Participants were 413 Black and Latina pregnant young women, ages 14-21 years. Experience with discrimination and all moderators were assessed in the second trimester. Last weight recorded in the third trimester was abstracted from medical records and used to determine excessive weight gain.
Results
Ever experiencing discrimination was associated with a 71% increase in the odds of excessive weight gain. The effect of discrimination was primarily present among women who attributed this treatment to membership in a historically oppressed group (e.g., ethnic minority, female) or to membership in other stigmatized groups (e.g., overweight). The effect of ever experiencing discrimination was not moderated by race/ethnicity or age but was moderated by depressive symptoms. Supporting the perspective of the environmental affordances model, discrimination strongly predicted excessive weight gain when women were low in depressive symptoms but had no effect when women were high in depressive symptoms. The moderating role of depressive symptoms was equivalent for Black and Latina women.
Conclusion
Results highlight the role of discrimination in perpetuating weight-related health disparities and suggest opportunities for improving health outcomes among young pregnant women.
Keywords: discrimination, weight gain, pregnancy, adolescents, young women, Black, Latina
Overweight and obesity are serious threats to health worldwide. Almost 70% of adults and one-third of children and adolescents in the United States (U.S.) are overweight or obese, with a body mass index (BMI) of 25–29.9 or ≥ 30 kg/m2, respectively (Ogden, Carroll, Kit, & Flegal, 2014). Women of color have been disproportionally affected by this epidemic. The prevalence of overweight and obesity among Black and Latina women is 82.1% and 76.2%, respectively, 17% and 12% higher than the prevalence among White women (Ogden et al., 2014). Elevated rates of overweight and obesity among Black and Latina women are evident in adolescence and continue to climb into adulthood (Ogden et al., 2014).
The majority of women gain weight beyond medical recommendations during pregnancy (Caulfield, Witter, & Stoltzfus, 1996; Gould Rothberg, Magriples, Kershaw, Rising, & Ickovics, 2011; Wells, Schwalberg, Noonan, & Gabor, 2006). Excessive pregnancy weight gain, in turn, increases risk for obesity in subsequent years among both mother and child due to increased postpartum weight retention and large for gestational age babies, respectively (Amorim, Rossner, Neovius, Lourenco, & Linne, 2007; Frederick, Williams, Sales, Martin, & Killien, 2008; Gould Rothberg et al., 2011; Magriples, Kershaw, Rising, Westdahl, & Ickovics, 2009; Oken, Rifas-Shiman, Field, Frazier, & Gillman, 2008). The literature examining differences in weight gain by race/ethnicity is mixed, with some studies indicating that Black women are particularly likely to exceed recommendations relative to White women (Wells et al., 2006). Latinas are consistently less likely to exceed recommendations than Black and White women (Gould Rothberg et al., 2011; Wells et al., 2006). However, they remain an important group to study in the context of pregnancy weight gain given their increased risk for obesity in later life.
A growing body of research indicates that experiencing everyday discrimination, characterized by ongoing day-to-day experiences of being treated differently than others, is associated with increased waist circumference and abdominal fat over time, and ultimately increased weight (Cozier, Wise, Palmer, & Rosenberg, 2009; Hickson et al., 2012; Hunte, 2011; Lewis, Kravitz, Janssen, & Powell, 2011). The effect of discrimination on weight-related outcomes persists whether attributed to race/ethnicity (Cozier et al., 2009) or not attributed to any specific factor (Lewis et al., 2011). However, null effects have also been observed (Hunte & Williams, 2009; Vines et al., 2007), suggesting the need to continue evaluating conditions under which discrimination affects weight-related outcomes.
Discrimination is believed to affect health outcomes because, as a chronic stressor (Mays, Cochran, & Barnes, 2007), it impairs the sympathetic nervous system and alters hypothalamic-pituitary-adrenal axis (HPA-axis) reactivity to and recovery following exposure to a stressor (Bjorntorp, 2001). In the context of weight gain, the stress hormone cortisol, which is released by the HPA-axis in response to stress, can influence both overeating and the accumulation of abdominal fat (Bjorntorp, 2001; Epel, Lapidus, McEwen, & Brownell, 2001). Everyday discrimination has been shown to affect levels of cortisol during pregnancy (Thayer & Kuzawa, 2015), suggesting one potential pathway through which discrimination may contribute to excess pregnancy weight gain and future obesity among women. However, the association between discrimination and pregnancy weight gain has not been examined in previous research.
Demographic factors, including race/ethnicity and age, may moderate the relationship between discrimination and pregnancy weight gain. Following the arguments that Black individuals have a different history of oppression in the U.S. and that Latinos are more likely to be immigrants and therefore may be less sensitized to detecting the subtle indications of prejudice that are common in day-to-day life, racial discrimination in particular has been found to more strongly affect Black relative to Latino individuals (Gee, Ryan, Laflamme, & Holt, 2006). Yet, other research has observed no differences by race/ethnicity in the influence of discrimination due to any cause on health (Earnshaw et al., 2013; Lewis et al., 2013). Similarly, age may alter the relationship between discrimination and health. Early adolescence may be a critical period during which discrimination and stigma strongly influence initiation of maladaptive behaviors (Gibbons et al., 2007; Reid, Dovidio, Ballester, & Johnson, 2014). On the other hand, the “weathering” hypothesis indicates that experiences with discrimination accumulate, strongly impacting older adults’ health (Geronimus, Hicken, Keene, & Bound, 2006). Thus, it is unclear whether and in what direction race/ethnicity and age might affect the relationship between discrimination and weight gain.
Depression and other mood disorders have primarily been considered as outcomes of discrimination (Pascoe & Smart Richman, 2009), or as potential confounders or mediators of the influence of discrimination on health (Earnshaw et al., 2013; Gibbons, Gerrard, Cleveland, Wills, & Brody, 2004; Lewis, Cogburn, & Williams, 2015). However, the moderating role of depression has also been examined. Chae et al. (2012) found that history of a mood disorder heightened the effect of discrimination on cardiovascular disease risk. On the other hand, the environmental affordances model (Mezuk et al., 2013) has demonstrated a tradeoff, whereby discrimination may affect either mental or physical health but not necessarily both. Specifically, Black women who smoke, use substances, and/or are obese (an indicator of unhealthy eating) have a lower likelihood of developing depression in response to chronic stress than women who engage in none of these practices (Boardman & Alexander, 2011; Jackson, Knight, & Rafferty, 2010; Mezuk et al., 2010). This model draws on research demonstrating that each of these behaviors reduces the experience of stress. Consuming unhealthy foods, for example, dampens HPA-axis response to stress (Dallman, 2010; Foster et al., 2009; Pecoraro, Reyes, Gomez, Bhargava, & Dallman, 2004). Likewise, although cigarettes and alcohol both activate the HPA-axis, they also act on the dopamine system, producing feelings of calm and relaxation and dampening the body’s response to stressful events (Koob et al., 1998; Pierce & Kumaresan, 2006). Black women may prefer unhealthy eating as the most gender- and socially-appropriate physical means for coping with stress (Giscombe, 2005; Jackson et al., 2010), especially while pregnant. This research has viewed obesity as an indicator of coping with stress in a manner that either protects against or masks the effects of stress on depression. Likewise, the presence of heightened depressive symptoms may be seen as an indicator of coping with stress in a manner that limits its effects on obesity and excess weight gain. Discrimination may therefore have less effect on weight gain among women with heightened depressive symptoms. Thus, as with race/ethnicity and age, there are conflicting views regarding whether depression may exacerbate or dampen the effect of discrimination on weight.
The present research sought to make a novel contribution to the literature by prospectively examining the relationship between everyday discrimination and weight gain during pregnancy, a contributing factor to later life obesity, among Black and Latina young women. Because these young women are likely to be exposed to discrimination on the basis of a number of different characteristics (e.g. race/ethnicity, language, income level, etc.) we examined discrimination due to any cause, rather than specifically due to race/ethnicity. We predicted that reports of discrimination in the second trimester of pregnancy would be associated with excessive weight gain in the third trimester, over and above important covariates. Given mixed results in previous research, we explored whether the influence of discrimination was moderated by race/ethnicity, age, and depressive symptoms.
Method
Procedures
Data were drawn from the control condition of a randomized controlled trial testing the efficacy of group prenatal care versus standard individual prenatal care (Ickovics et al., 2015). Fourteen study sites in New York City were randomized. The present analysis reports data from the seven sites randomized to standard prenatal care. Young women receiving prenatal care at a study site between 2008 and 2011 were invited to participate. Inclusion in the study required that the woman was 14–21 years old, no more than 24 weeks gestation, not considered high-risk (e.g., HIV positive), willing to be randomized, and comfortable speaking English or Spanish.
Structured interviews were completed in English or Spanish using Audio-Handheld Assisted Personal Interview, allowing participants to simultaneously listen to and read questions, then enter their responses on a handheld computer. Participants received $20 for participation in each interview. All self-report data used in the present analysis were taken from interviews conducted at study enrollment in the second trimester, between 14 and 24 weeks gestation. Procedures were approved by the Institutional Review Boards at Yale University, the Clinical Directors Network, and each study site.
Participants
In all, 624 young women from the clinical study sites were randomized to the control condition. Women were excluded from the present analysis if they were not Black or Latina (n = 37), were missing medical record data (n = 56) or information on the baby’s date of birth (n = 21), did not have their weight assessed at the study site during the third trimester (n = 48), were carrying twins (n = 6), or did not provide complete data on examined variables (n = 49), resulting in a sample of 413 women. Women who were not Black or Latina were excluded because the small sample size did not allow for consideration of other races or ethnicities. Exclusion from analyses was unrelated to study variables, including discrimination (χ2(1, N = 622) = 0.03, p = .86), pre-pregnancy BMI (t (587) = −0.92, p = .36), and race/ethnicity (χ2(1, N = 587) = 0.001, p = .97).
Measures
Excessive weight gain
The Institute of Medicine (IOM; 2009) has provided guidelines for weight gain during pregnancy based on a woman’s pre-pregnancy BMI. A maximum weight gain of 40 pounds is recommended for underweight women (BMI < 18.5 kg/m2), with 35, 25, and 20 pounds recommended for normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese women (BMI > 30.0 kg/m2), respectively. Women are advised to gain no more than 4.4 pounds during the first trimester and 1.32, 1.13, .76, or 0.58 pounds per week, depending on their pre-pregnancy BMI group.
Pre-pregnancy BMI was calculated from self-reported pre-pregnancy weight and height in the second trimester. The final weight assessed during the third trimester of pregnancy, the date of the final weight assessment, and gestational age at birth were abstracted from medical records. Weight gain was calculated by subtracting pre-pregnancy weight from final third trimester weight. Gestational age when the final weight was assessed was back-calculated from gestational age at birth. Maximum recommended weight gain was calculated for each woman from IOM guidelines (2009), accounting for each woman’s BMI group and gestational age at final weight assessment. Weight gain was categorized as excessive if it exceeded the maximum recommended.
Discrimination
Discrimination was assessed with a 10-item version of the Everyday Discrimination Scale (Williams, Yan, Jackson, & Anderson, 1997). Participants indicated on a 1 (never) to 4 (often) scale how often in their day-to-day lives they experienced discrimination (e.g., are “treated with less courtesy than other people”); items did not reference race/ethnicity, gender, etc., as the cause of discrimination. This measure of discrimination has been frequently employed in previous research examining weight outcomes (Cozier et al., 2009; Hickson et al., 2012; Hunte, 2011; Lewis et al., 2011). The items were initially summed to form a scale score. However, responses were skewed such that few individuals “sometimes” or often “experienced” discrimination. We explored forming categories of none, low, moderate, or high exposure (Chae et al., 2008) but still observed limited exposure at the moderate (n = 34) and high levels (n = 2). Moreover, there was no evidence of a dose-response relationship between excessive weight gain and either the fully continuous or the graded categorical measures of discrimination. Consistent with previous research, we ultimately dichotomized the scale into never experienced (0) versus had ever experienced (1) discrimination (Hunte & Williams, 2009; Schulz et al., 2006).
If participants reported ever experiencing any form of discrimination, a follow-up question assessed participants’ primary attribution for these experiences. Participants who identified race/ethnicity, language, gender, income, or sexual orientation as the primary reason for this treatment were classified as having attributed differential treatment to membership in a group that has historically experienced group-based oppression. Individuals who attributed differential treatment to non-group based identities indicated age, physical appearance, or “other” as reasons for this treatment or chose not to select a reason.
Moderators
All moderators were assessed during the second trimester. Women self-reported their current age and race/ethnicity as Latina or Black, non-Latina. Depressive symptoms were assessed with 15 items from the affect-only component of the Center for Epidemiologic Studies - Depression Scale (CES-D; Radloff, 1977). Consistent with previous research on pregnant women (Westdahl et al., 2007), five somatic items from the full scale that may reflect symptoms of either depression or pregnancy were not assessed (e.g., poor appetite, restless sleep). Participants indicated how often in the previous week they felt “depressed” or “lonely” on a 0 (less than 1 day) to 3 (5–7 days) scale. Items were summed to form a scale score ranging from 0 to 44 (Cronbach’s α = .86).
Covariates
All analyses controlled for variables that have been linked to pregnancy weight gain or discrimination in previous research. Covariates included race/ethnicity, age, depressive symptomatology, pre-pregnancy BMI, gestational age when the final weight was assessed, number of births >20 weeks gestation (i.e., parity: 0 versus 1+), and nativity (U.S. born versus not) (Casanueva, Labastida, Sanz, & Morales-Carmona, 2000; Caulfield et al., 1996; Gee et al., 2006; Gould Rothberg et al., 2011). Parity and nativity status were assessed via self-report in the second trimester.
Data Analysis
All analyses were conducted in SPSS 22.0. Descriptive statistics were run to characterize the sample on all covariates and total weight gain. T-tests were conducted to compare women who had appropriate versus excessive weight gain. We examined the extent to which total weight gain (final weight – pre-pregnancy weight) among participants was correlated within study sites. There was little evidence of clustering in weight gain (Intra-class correlation=.002, design effect= 1.18), therefore, we used standard logistic regression to examine the association of discrimination with excessive weight gain. Mean (M) differences between those who did versus did not experience discrimination were examined for each moderator. Moderators were tested in three separate logistic regressions. Everyday discrimination and moderators were mean centered prior to forming interaction terms (Aiken & West, 1991). Significant interactions were probed within categories for dichotomous variables or at one standard deviation (SD) above and below the mean for continuous moderators.
Results
Sample Characteristics
Participants averaged 18.56 years of age (SD = 1.70). Sixty-six percent identified as Latina, 34% as Black. Mean pre-pregnancy BMI was 24.08 (SD = 5.66); 18% were overweight, and 15% were obese. Women averaged 18.69 weeks gestation (SD = 3.50) in the second trimester and 38.09 weeks gestation (SD = 2.37) at their final third trimester weight assessment. In all, 54% had weight gain that exceeded recommendations. On average, women who exceeded weight recommendations did so by 15.04 pounds (SD = 13.16); 79% were five or more pounds beyond recommendations. Overall, 78% (n = 320) of women had experienced discrimination. Among these women, 39% (n = 125) attributed their experiences to a group-based identity. Race/ethnicity (n = 73) and language (n = 20) were most often selected as reasons for discrimination, followed by income (n = 15), gender (n = 10), and sexual orientation (n = 7). Women who did not attribute discrimination to group membership (n = 195), most commonly selected “other” (n = 102), followed by age (n = 52) and physical appearance (n = 28). Thirteen participants chose not to indicate a reason for discrimination.
Demographic comparisons of participants who had appropriate versus excessive weight gain are given in Table 1. Women with excessive weight gain had higher pre-pregnancy BMIs and were 0.78 weeks, or 5.46 days, further along in pregnancy. Notably, women who exceeded recommendations gained, on average, double that of women with appropriate weight gain. Black and Latina women were equally likely to exceed weight recommendations.
Table 1.
Sample Characteristics Stratified by Weight Gain Status
| Weight Gain Status Based on Institute of Medicine Guidelines |
|||
|---|---|---|---|
| Demographics | Appropriate (n = 189) |
Excessive (n = 224) |
p-value |
| Race/ethnicity, N (%) | |||
| Black | 67 (47.5%) | 74 (52.5%) | .61 |
| Latina | 122 (44.9%) | 150 (55.1%) | |
| Age, M (SD) | 18.40 (1.75) | 18.70 (1.66) | .08 |
| Nativity status, N (%) | |||
| U.S. born | 133 (44.0%) | 169 (56.0%) | .25 |
| Foreign born | 56 (50.5%) | 55 (49.5%) | |
| Pre-pregnancy BMI, M (SD) | 22.85 (6.56) | 25.12 (5.73) | .001 |
| Gestational age at final weight assessment (weeks), M (SD) |
37.67 (2.62) | 38.45 (2.08) | .001 |
| Parity, N (%) a | |||
| 0 | 155 (44.7%) | 192 (55.3%) | .31 |
| 1+ | 34 (51.5%) | 32 (48.5%) | |
| Depressive symptoms, M (SD) | 11.79 (8.58) | 12.18 (8.77) | .65 |
| Total weight gain (pounds), M (SD) | 21.02 (9.59) | 43.50 (13.59) | .001 |
Notes. M=Mean. SD=Standard deviation. BMI= body mass index (kg/m2).
Parity: 0 = no births >20 weeks gestation; +1 = 1 or more birth >20 weeks gestation.
Main Effect of Everyday Discrimination
Everyday discrimination was not related to pre-pregnancy weight or BMI (ps > .16). However, having experienced discrimination in the second trimester predicted greater odds of excessive weight gain in the third trimester (p = .04). As indicated in Table 2, ever experiencing discrimination was associated with a 71% increase in the odds of excessive weight gain. A sensitivity analysis indicated that excluding individuals who were within one pound of the weight recommendation (n = 24) did not alter the magnitude of the effect (Odds ratio [OR] = 1.70, p = .05). Among the covariates, gestational age at final weight assessment and BMI were the only significant predictors of excessive weight gain. Depressive symptoms were not associated with excessive weight gain.
Table 2.
Effects of Discrimination, Covariates, and Interactions on Excessive Weight Gain
| Predictors | B [95% CI] | Adjusted Odds Ratio [95% CI] |
Chi-square |
|---|---|---|---|
| Discrimination (never vs. ever) | 0.54 [0.03, 1.05] | 1.71 [1.03, 2.85] | 4.31* |
| Race/ethnicity | 0.12 [−0.33, 0.57] | 1.13 [0.72, 1.77] | 0.30 |
| Age | 0.10 [−0.02, 0.23] | 1.11 [0.98, 1.26] | 2.57 |
| Depressive symptoms | 0.00 [−0.02, 0.03] | 1.00 [0.98, 1.03] | 0.01 |
| Body mass index | 0.08 [0.04, 0.12] | 1.08 [1.04, 1.13] | 14.53*** |
| Gestational age | 0.14 [0.05, 0.23] | 1.15 [1.05, 1.26] | 9.28** |
| Parity | −0.40 [−0.99, 0.19] | 0.67 [0.37, 1.21] | 1.78 |
| Nativity | −0.42 [−0.89, 0.06] | 0.66 [0.41, 1.06] | 2.96 |
| Interactions | |||
| Discrimination × Race/ethnicity | −0.57 [−1.71, 0.59] | 0.57 [0.18, 1.81] | 0.92 |
| Discrimination × Age | −0.14 [−0.45, 0.18] | 0.87 [0.64, 1.20] | 0.70 |
| Discrimination × Depressive symptoms | −0.08 [−0.15, 0.00] | 0.93 [0.86, 1.00] | 3.87* |
| Discrimination × Depressive symptoms × Race/ethnicity | −0.08 [−0.24, 0.09] | 0.93 [0.79, 1.09] | 0.82 |
Notes. Interactions were examined in separate logistic regression models. B= unstandardized coefficient. CI= confidence interval.
p ≤ .05
p ≤ .01
p ≤ .001.
We conducted a post-hoc analysis to examine whether the effect of discrimination depended on whether participants attributed this treatment to a group-based identity or to some other cause. The variables capturing ever experiencing discrimination and attributions for discrimination were used to create two dummy codes. Individuals who never experienced discrimination (23%), the base group, were compared first with individuals who experienced discrimination but did not attribute it to a group-based identity (non-group-based discrimination; 47%) and second, with individuals who attributed discrimination to race/ethnicity, language, gender, income, or sexual orientation (group-based discrimination; 30%). These dummy codes were examined as predictors in logistic regression models in place of the dichotomous measure of discrimination. As shown in Table 3, results indicated that group-based discrimination was associated with a 94% increase in the odds of excessive weight gain (p = .03). Non-group-based discrimination was only marginally associated with greater odds of excessive weight gain (p = .10).
Table 3.
Effects of Group-based, Non-group-based, Attributed, and Unattributed Discrimination on Excessive Weight Gain
| B [95% CI] | Adjusted Odds Ratio [95% CI] |
Chi-square | |
|---|---|---|---|
| Group-based discrimination | 0.66 [0.07, 1.25] | 1.94 [1.08, 3.50] | 4.88* |
| Non-group-based discrimination | 0.46 [−0.08, 1.00] | 1.58 [0.92, 2.72] | 2.75 |
| Attributed discrimination | 0.64 [0.10, 1.18] | 1.89 [1.10, 3.26] | 5.30* |
| Unattributed discrimination | 0.38 [−0.21, 0.97] | 1.46 [0.81, 2.63] | 1.59 |
Notes. Group-based and non-group-based discrimination were examined in a single analysis, and attributed and unattributed discrimination in a separate analysis. Ethnicity, age, depressive symptoms, body mass index, gestational age, parity, and nativity were included as covariates in both analyses. B= unstandardized coefficient. CI= confidence interval.
p ≤ .05.
As age and weight may also be a basis for discrimination (Puhl & Brownell, 2001; Rosenthal et al., 2014), a sensitivity analysis further examined whether the effect observed for group-based discrimination extended to other stigmatized identities. Dummy codes included those who attributed discrimination to a group identity, age, or physical appearance in a single category (attributed discrimination; 49%). Individuals who never experienced discrimination (23%), the base group, and individuals who experienced discrimination but selected “other” or chose not to select an attribution (unattributed discrimination; 28%) formed the other categories. Consistent with the results for group-based discrimination, attributed discrimination was associated with an 89% increase in the odds of excessive weight gain (p = .02) (see Table 3). Unattributed discrimination did not increase risk of excessive weight gain (p = .21). Taken together, these analyses support that the main effect of never versus ever experiencing discrimination primarily reflects discrimination due to membership in historically oppressed and other stigmatized groups, rather than general unfair treatment.
Potential Moderators: Race/ethnicity, Age, and Depressive Symptoms
Moderators were examined with respect to the dichotomous measure of never versus ever experiencing discrimination. Analyses examining moderators of group-based and non-group-based discrimination were largely consistent with the results reported below. Regarding mean differences in discrimination as a function of the moderators, Black women (86%) were more likely to report experiencing discrimination than Latina women (73%) (χ2 [1, N = 413] = 8.52, p < .01). In addition, women who reported experiencing discrimination had higher concurrent depressive symptomatology (M = 13.04) than those who did not (M = 8.43) (t [208.17] = −5.55, p <.001). However, age did not vary across experiences with discrimination (p = .28).
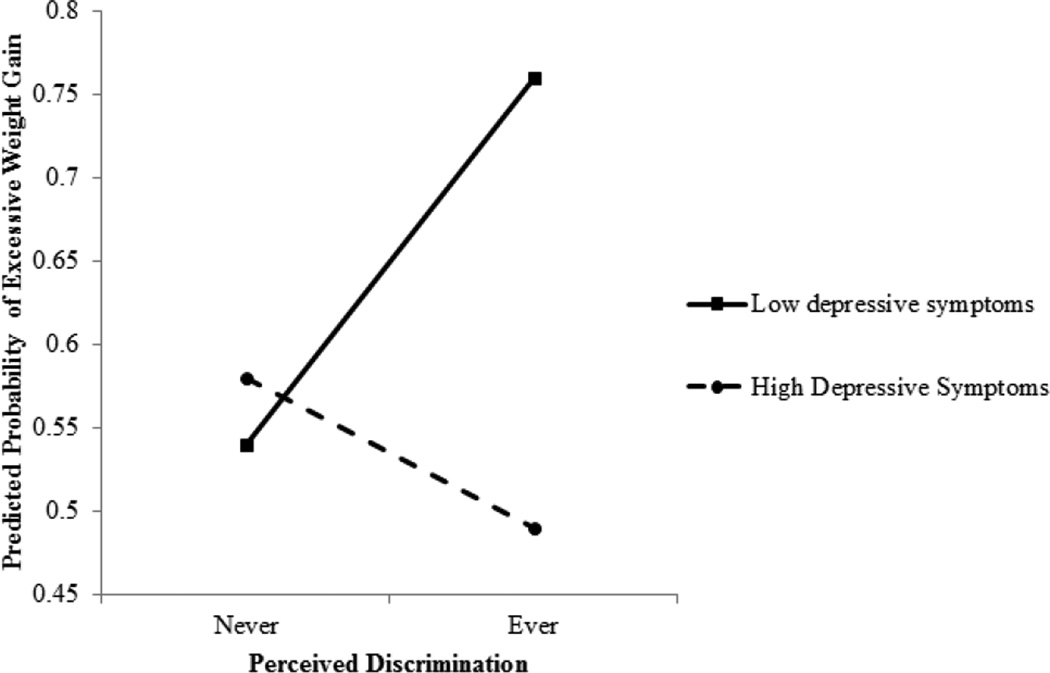
Although the simple slopes suggested that the influence of discrimination on excessive weight gain was stronger for Black women (B = 0.97, p = .06) than Latina women (B = 0.40, p = .18), the discrimination by race/ethnicity interaction was not significant (p = .34) (Table 2). Likewise, age did not moderate the relationship between discrimination and excessive weight gain (p = .40). The influence of discrimination on excessive weight gain was, however, moderated by depressive symptoms (p = .05) (Table 2). Simple effects, shown in Figure 1, were examined at one SD above and below the mean of depressive symptoms, reflecting scores of 21 and 3, respectively. High values of depressive symptomatology were well above 16, the typical cut-point on the CES-D for defining individuals as at high risk for depression (Radloff, 1977).
Figure 1.
Simple effects for the relationship of discrimination to probability of excessive weight gain at high and low levels of depressive symptoms. Simple effects were probed at 1 standard deviation above and below the mean of depressive symptoms, respectivley.
Consistent with the environmental affordances model (Mezuk et al., 2013), when depressive symptoms were high, there was no effect of discrimination on excessive weight gain (B = −0.36, 95% confidence interval [CI]: −1.41, 0.68; χ2 = 0.46, p = .50). However, when depressive symptoms were low, discrimination strongly affected excessive weight gain (B = 0.98, 95% CI: 0.31, 1.65; χ2 = 8.13, p < .01). Reports of ever experiencing discrimination were associated with a 165% increase in the odds of excessive weight gain among women who were low in depressive symptoms. As shown in Figure 1, women who had low levels of depressive symptoms and experienced discrimination had a 76% chance of exceeding weight recommendations. All other women had approximately a 50% chance of exceeding weight recommendations.
Previous research documenting this tradeoff between mental and physical health in the influence of discrimination has focused on Black but not Latina women (e.g., Jackson et al., 2010). Therefore, we conducted a post-hoc analysis to examine whether the interaction between discrimination and depressive symptoms varied as a function of race/ethnicity. The nonsignificant three-way interaction between discrimination, depressive symptoms, and race/ethnicity (p = .39) indicated that the moderating role of depressive symptoms was equivalent for Black and Latina women (Table 2). The simple slopes further supported that there was no effect of discrimination among Black women (B = 0.73, p = .45) or Latina women (B = −0.75 p = .26) when depressive symptoms were high. However, an effect of discrimination emerged when depressive symptoms were low for both Black (B = 1.14, p = .08) and Latina (B = 0.95, p = .02) women. Thus, among women of both races/ethnicities, ever experiencing discrimination predicted excessive weight gain primarily when depressive symptoms were low.
Discussion
To our knowledge, this study is the first to examine and find associations of discrimination with the likelihood of exceeding recommendations for weight gain during pregnancy. Although young women who exceeded recommendations were just 5.46 days further along in pregnancy, they gained 22 pounds more on average than women who stayed within recommendations. This is problematic because research suggests that women who exceed weight recommendations during pregnancy experience significant difficulty in returning to their pre-pregnancy weight postpartum, putting them at risk for overweight and obesity throughout adulthood (Gould Rothberg et al., 2011).
Our post-hoc analysis supported that the main effect of never versus ever experiencing discrimination was more so the result of discrimination due to membership in historically oppressed and other stigmatized groups, rather than attributions of differential treatment to other causes. Previous research has discussed the benefits and drawbacks of different approaches to assessing discrimination (Shariff-Marco et al., 2011; Williams & Mohammed, 2009). Assessing discrimination without reference to a specific identity can be beneficial because it yields the highest level of reported exposure to discrimination (Shariff-Marco et al., 2011). Further, it remains unclear whether one approach is more accurate than the other options for assessing discrimination (Lewis et al., 2015). Nonetheless, our results are consistent with previous research demonstrating that increased experiences with discrimination, whether assessed with respect to a specific identity or not, appear to negatively impact weight-related outcomes (Cozier et al., 2009; Lewis et al., 2011).
It is noteworthy that discrimination was not associated with women’s pre-pregnancy weight or BMI. Associations have been observed between cross-sectional but not longitudinal assessments of stress and weight among adolescents (van Jaarsveld, Fidler, Steptoe, Boniface, & Wardle, 2009). Further, although adolescents do cope with stress by eating high fat foods and engaging in emotional eating (Cartwright et al., 2003; Nguyen-Rodriguez, Chou, Unger, & Spruijt-Metz, 2008), these eating practices do not consistently differentiate between normal- and over-weight adolescents (e.g., Nguyen-Rodriguez et al., 2008). Only a few studies have examined the relationship between stress and weight among adolescents (Wardle, Chida, Gibson, Whitaker, & Steptoe, 2011). It therefore remains unclear whether discrimination is more likely to manifest in behaviors like substance use and unprotected sex among adolescents, requiring a critical life event like pregnancy to differentially influence weight. This issue highlights the need for more comprehensive theorizing regarding for which individuals discrimination is likely to impact which outcomes.
Discrimination was concurrently associated with second trimester depressive symptoms. However, given the lack of a relationship between depressive symptoms and excessive weight gain, depressive symptoms did not mediate the effect of discrimination on excessive weight gain. Rather, depressive symptoms moderated the relationship between discrimination and weight gain, with an effect of discrimination evident at low but not high levels of depressive symptoms. Both Black and Latina women were primarily influenced by discrimination when depressive symptoms were low. From the perspective of the environmental affordances model (Mezuk et al., 2013), this might be expected given similarly high rates of obesity, modest rates of depression, and comparable social environments among Black and Latino individuals (Cottrell & Neuberg, 2005; Dunlop, Song, Lyons, Manheim, & Chang, 2003; Ogden et al., 2014).
These results support the broader perspective of the environmental affordances model, indicating that there may be tradeoffs in the way that individuals manage chronic stress (Jackson et al., 2010). As research based on the model has assessed the presence of depression and obesity rather than coping strategies that may lead to these outcomes (Boardman & Alexander, 2011; Jackson et al., 2010; Mezuk et al., 2010), additional research is needed to verify actual use of coping strategies that differentially impact mental versus physical heath. Nonetheless, results support that coping with discrimination in a way that impacts mental health may channel the effects of stress away from mechanisms that impact weight gain and vice versa. As a result, treating weight gain or depressive symptoms directly may lead to rebounds in the alternative outcome. Instead, techniques that address the physiological response to discrimination are likely to be most effective long-term.
Black women were more likely to report discrimination than Latina women, potentially due to differences in the history and nature of discrimination directed at these groups (Gee et al., 2006). This may also reflect differences in Blacks’ and Latinas’ residential environments. Although residential segregation has been linked to a number of negative health outcomes (Williams & Collins, 2001), living in a segregated neighborhood that exists within a cluster of other similarly segregated neighborhoods, an “ethnic enclave,” may actually protect residents from experiencing discrimination (Bell, Zimmerman, Almgren, Mayer, & Huebner, 2006). Nonetheless, it is unclear in the present sample whether neighborhood composition explains Black-Latino differences in experiences with discrimination.
Although the simple slopes suggested that the effect of discrimination on weight gain may be more so evident among Black women than among Latina women, the discrimination by race/ethnicity interaction was not significant. Certainly, power is low for detecting small to moderate sized interactions, especially when measures are not perfectly reliable (Aiken & West, 1991). In light of the “Hispanic/Latino paradox” (Franzini, Ribble, & Keddie, 2001), it is plausible that discrimination may more strongly influence the health outcomes of Black individuals. Yet, we also noted an effect of discrimination among Latina women with low but not high depressive symptoms. It therefore does not appear that Latinas’ pregnancy weight gain is universally unrelated to their experiences with discrimination. The circumstances under which these relationships are detectable among Black versus Latina individuals may be highly nuanced. Research that is sufficiently powered to detect discrimination by race/ethnicity interactions is needed to allow us to more definitively gauge to what extent discrimination differentially influences the outcomes of individuals of different races or ethnicities.
Similarly, age did not moderate the relationship between discrimination and weight gain. Reports of discrimination also did not vary by age. The lack of a difference in reports of discrimination by age is somewhat surprising given that young women, relative to adolescents, potentially had more opportunities for contact with stigmatizing institutions, including pre-pregnancy healthcare and work environments. However, previous research has documented that preadolescents report experiencing discrimination (Simons et al., 2002) and these early experiences may be particularly critical for shaping coping behavior (Gibbons et al., 2007). Experiences with discrimination have also been shown to vary in late but not early pregnancy as a function of age (Rosenthal et al., 2014). Thus, in the absence of additional visible marks of stigma (i.e., being a pregnant adolescent), the likelihood of experiencing discrimination may primarily be a function of race/ethnicity rather than age.
Where these young women were likely to have encountered discrimination remains an open question. Given their mean age of 18, many of them had likely spent a substantial amount of time in the school system. Black and Latino students in New York City have reported being treated differently than students of other ethnicities by teachers, and these experiences increase over the course of high school (Greene, Way, & Pahl, 2006; Rosenbloom & Way, 2004). These students also reported experiencing discrimination in interactions with police and shopkeepers (Rosenbloom & Way, 2004). The present study enrolled young women during their 18th week of pregnancy, on average. As the first prenatal visit typically occurs between weeks eight and 10, these women may also have experienced discrimination in interactions with doctors as a result of being ethnic minority, primarily unwed, pregnant adolescents. Experiences with discrimination have been documented among Latino and Black adults seeking general healthcare, as well as among ethnic minority women seeking reproductive healthcare (Gee et al., 2006; Malat & Hamilton, 2006; Thorburn & Bogart, 2005). Thus, there are a number of settings in which the women in the present sample could have experienced discrimination.
Although medical interactions may communicate discrimination, pregnancy is an ideal time for medical professionals who have regular contact with pregnant patients to implement interventions that aim to reduce the impact of discrimination. For example, a brief task in which individuals affirm their self-worth by writing about important values (e.g., relationships with family and friends) has been show to buffer the effects of discrimination by preventing increases in cortisol and epinephrine in response to stressors (Creswell et al., 2005; Sherman, Bunyan, Creswell, & Jaremka, 2009). Indeed, self-affirmation interventions have had long-term positive effects on minority youth across a number of domains (Sherman, 2013), including in the context of weight loss (Cook et al., 2014).
Strengths and Limitations
The primary limitation of the present study is that some of our predictors and outcomes, such as pre-pregnancy weight, are subject to self-report bias. However, research suggests fairly accurate reporting of pre-pregnancy weight (Gould Rothberg et al., 2011; Park et al., 2011). In addition, results may not extend to non-pregnant adolescent samples, where the effects of discrimination may manifest differently. Despite these limitations, the prospective study design is a strength, which allowed for greater causal inference. Moreover, we are unaware of previous research that has demonstrated an association of discrimination to pregnancy weight gain, highlighting an avenue for limiting the effect of discrimination on long-term health outcomes.
Conclusion
Our results suggest pregnancy weight gain as a pathway through which discrimination may contribute to disparities in obesity among women. Results also highlight the complex interplay between mental and physical health in manifestation of the effects of discrimination. Strategies that aim to reduce the likelihood of encountering discrimination and that alter young pregnant women’s physiological response to discrimination may potentially have far reaching consequences for both mother and child.
Research Highlights.
Excess pregnancy weight gain increases risk of obesity among mothers and children.
We examined whether discrimination predicted excess pregnancy weight gain.
Experience with discrimination increased odds of third trimester excess weight gain.
The effect was moderated by depressive symptoms but not by ethnicity or age.
Discrimination predicted excess weight gain only when depressive symptoms were low.
Acknowledgments
We thank Marcy Boynton for assistance with statistical analyses. This research and preparation of this article was supported by National Institute of Mental Health grants R01MH074399, R01MH074394, and T32 MH20031.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Amorim AR, Rossner S, Neovius M, Lourenco PM, Linne Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity (Silver Spring) 2007;15:1278–1286. doi: 10.1038/oby.2007.149. [DOI] [PubMed] [Google Scholar]
- Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: A multilevel analysis of the role of racial residential segregation. Social Science & Medicine. 2006;63:3030–3045. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obesity Reviews. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Alexander KB. Stress trajectories, health behaviors, and the mental health of black and white young adults. Social Science & Medicine. 2011;72:1659–1666. doi: 10.1016/j.socscimed.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright M, Wardle J, Steggles N, Simon AE, Croker H, Jarvis MJ. Stress and dietary practices in adolescents. Health Psychology. 2003;22:362–369. doi: 10.1037/0278-6133.22.4.362. [DOI] [PubMed] [Google Scholar]
- Casanueva E, Labastida J, Sanz C, Morales-Carmona F. Depression and body fat deposition in Mexican pregnant adolescents. Archives of Medical Research. 2000;31:48–52. doi: 10.1016/s0188-4409(00)00041-2. [DOI] [PubMed] [Google Scholar]
- Caulfield LE, Witter FR, Stoltzfus RJ. Determinants of gestational weight gain outside the recommended ranges among black and white women. Obstetrics & Gynecology. 1996;87:760–766. doi: 10.1016/0029-7844(96)00023-3. [DOI] [PubMed] [Google Scholar]
- Chae DH, Nuru-Jeter AM, Lincoln KD, Arriola KRJ. Racial discrimination, mood disorders, and cardiovascular disease among black Americans. Annals of Epidemiology. 2012;22:104–111. doi: 10.1016/j.annepidem.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Takeuchi DT, Barbeau EM, Bennett GG, Lindsey J, Krieger N. Unfair treatment, racial/ethnic discrimination, ethnic identification, and smoking among Asian Americans in the National Latino and Asian American Study. American Journal of Public Health. 2008;98:485–492. doi: 10.2105/AJPH.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JE, Purdie-Vaughns V, Garcia J, Taborsky-Barba S, Tomassetti S, Davis E, Cohen GL. A values-affirmation intervention reduces body mass due to social identity threat. 2014 Manuscript submitted for publication. [Google Scholar]
- Cottrell CA, Neuberg SL. Different emotional reactions to different groups: A sociofunctional threat-based approach to “prejudice”. Journal of Personality and Social Psychology. 2005;88:770–789. doi: 10.1037/0022-3514.88.5.770. [DOI] [PubMed] [Google Scholar]
- Cozier YC, Wise LA, Palmer JR, Rosenberg L. Perceived racism in relation to weight change in the Black Women’s Health Study. Annals of Epidemiology. 2009;19:379–387. doi: 10.1016/j.annepidem.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Welch WT, Taylor SE, Sherman DK, Gruenewald TL, Mann T. Affirmation of personal values buffers neuroendocrine and psychological stress responses. Psychological Science. 2005;16:846–851. doi: 10.1111/j.1467-9280.2005.01624.x. [DOI] [PubMed] [Google Scholar]
- Dallman MF. Stress-induced obesity and the emotional nervous system. Trends in Endocrinology & Metabolism. 2010;21:159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop DD, Song J, Lyons JS, Manheim LM, Chang RW. Racial/ethnic differences in rates of depression among preretirement adults. American Journal of Public Health. 2003;93:1945–1952. doi: 10.2105/ajph.93.11.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Rosenthal L, Lewis JB, Stasko EC, Tobin JN, Lewis TT, Ickovics JR. Maternal experiences with everyday discrimination and infant birth weight: A test of mediators and moderators among young, urban women of color. Annals of Behavioral Medicine. 2013;45:13–23. doi: 10.1007/s12160-012-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- Foster MT, Warne JP, Ginsberg AB, Horneman HF, Pecoraro NC, Akana SF, Dallman MF. Palatable foods, stress, and energy stores sculpt corticotropin-releasing factor, adrenocorticotropin, and corticosterone concentrations after restraint. Endocrinology. 2009;150:2325–2333. doi: 10.1210/en.2008-1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethnicity & disease. 2001;11:496–518. [PubMed] [Google Scholar]
- Frederick IO, Williams MA, Sales AE, Martin DP, Killien M. Pre-pregnancy body mass index, gestational weight gain, and other maternal characteristics in relation to infant birth weight. Maternal and Child Health Journal. 2008;12:557–567. doi: 10.1007/s10995-007-0276-2. [DOI] [PubMed] [Google Scholar]
- Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: The added dimension of immigration. American Journal of Public Health. 2006;96:1821–1828. doi: 10.2105/AJPH.2005.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: A panel study. Journal of Personality and Social Psychology. 2004;86:517–529. doi: 10.1037/0022-3514.86.4.517. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Yeh H-C, Gerrard M, Cleveland MJ, Cutrona C, Simons RL, Brody GH. Early experience with racial discrimination and conduct disorder as predictors of subsequent drug use: A critical period hypothesis. Drug & Alcohol Dependence. 2007;88:S27–S37. doi: 10.1016/j.drugalcdep.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giscombe C. The association of race-related, gender-related, and generic stress with global distress and coping among African American women. Stony Brook, NY: State University of New York; 2005. (Unpublished doctoral dissertation) [Google Scholar]
- Gould Rothberg BE, Magriples U, Kershaw TS, Rising SS, Ickovics JR. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. American Journal of Obstetrics & Gynecology. 2011;204:1–11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: Patterns and psychological correlates. Developmental psychology. 2006;42:218. doi: 10.1037/0012-1649.42.2.218. [DOI] [PubMed] [Google Scholar]
- Hickson DA, Lewis TT, Liu J, Mount DL, Younge SN, Jenkins WC, Williams DR. The associations of multiple dimensions of discrimination and abdominal fat in African American adults: the Jackson Heart Study. Annals of Behavioral Medicine. 2012;43:4–14. doi: 10.1007/s12160-011-9334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunte HER. Association between perceived interpersonal everyday discrimination and waist circumference over a 9-year period in the Midlife Development in the United States cohort study. American Journal of Epidemiology. 2011;173:1232–1239. doi: 10.1093/aje/kwq463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunte HER, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. American Journal of Public Health. 2009;99:1285. doi: 10.2105/AJPH.2007.128090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics JR, Earnshaw V, Lewis JB, Kershaw TS, Magriples U, Stasko E, Tobin JN. Cluster randomized controlled trial of group prenatal care: Perinatal outcomes among adolescents in New York City health centers. American Journal of Public Health. 2015 doi: 10.2105/AJPH.2015.302960. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Roberts AJ, Schulteis G, Parsons LH, Heyser CJ, Hyytiä P, Weiss F. Neurocircuitry Targets in Ethanol Reward and Dependence. Alcoholism: Clinical and Experimental Research. 1998;22:3–9. [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual review of clinical psychology. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported experiences of discrimination and visceral fat in middle-aged African-American and Caucasian women. American Journal of Epidemiology. 2011;173:1223–1231. doi: 10.1093/aje/kwq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychology. 2013;32:810–819. doi: 10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magriples U, Kershaw TS, Rising SS, Westdahl C, Ickovics JR. The effects of obesity and weight gain in young women on obstetric outcomes. American Journal of Perinatology. 2009;26:365–371. doi: 10.1055/s-0028-1110088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malat J, Hamilton MA. Preference for same-race health care providers and perceptions of interpersonal discrimination in health care. Journal of Health and Social Behavior. 2006;47:173–187. doi: 10.1177/002214650604700206. [DOI] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Abdou CM, Hudson D, Kershaw KN, Rafferty JA, Lee H, Jackson JS. “White Box” epidemiology and the social neuroscience of health behaviors: The environmental affordances model. Society and Mental Health. 2013;3:79–95. doi: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, Lee H, Jackson JS. Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. American Journal of Epidemiology. 2010;172:1238–1249. doi: 10.1093/aje/kwq283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Rodriguez ST, Chou CP, Unger JB, Spruijt-Metz D. BMI as a moderator of perceived stress and emotional eating in adolescents. Eating Behaviors. 2008;9:238–246. doi: 10.1016/j.eatbeh.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E, Rifas-Shiman SL, Field AE, Frazier AL, Gillman MW. Maternal gestational weight gain and offspring weight in adolescence. Obstetrics & Gynecology. 2008;112:999–1006. doi: 10.1097/AOG.0b013e31818a5d50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Sappenfield WM, Bish C, Bensyl DM, Goodman D, Menges J. Reliability and validity of birth certificate prepregnancy weight and height among women enrolled in prenatal WIC program: Florida, 2005. Maternal and Child Health Journal. 2011;15:851–859. doi: 10.1007/s10995-009-0544-4. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychological bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic stress promotes palatable feeding, which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology. 2004;145:3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- Pierce RC, Kumaresan V. The mesolimbic dopamine system: The final common pathway for the reinforcing effect of drugs of abuse? Neuroscience & biobehavioral reviews. 2006;30:215–238. doi: 10.1016/j.neubiorev.2005.04.016. [DOI] [PubMed] [Google Scholar]
- Puhl R, Brownell KD. Bias, discrimination, and obesity. Obesity research. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, Johnson BT. HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine. 2014;103:118–125. doi: 10.1016/j.socscimed.2013.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbloom SR, Way N. Experiences of discrimination among African American, Asian American, and Latino adolescents in an urban high school. Youth & Society. 2004;35:420–451. [Google Scholar]
- Rosenthal L, Earnshaw VA, Lewis TT, Reid AE, Lewis JB, Stasko EC, Ickovics JR. Changes in experiences with discrimination across pregnancy and postpartum: Age differences and consequences for mental health. American Journal of Public Health. 2014:e1–e8. doi: 10.2105/AJPH.2014.301906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. American Journal of Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariff-Marco S, Breen N, Landrine H, Reeve BB, Krieger N, Gee GC, Alegría M. Measuring everyday racial/ethnic discrimination in health surveys. Du Bois Review: Social Science Research on Race. 2011;8:159–177. doi: 10.1017/S1742058X11000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman DK. Self-affirmation: Understanding the effects. Social and Personality Psychology Compass. 2013;7:834–845. [Google Scholar]
- Sherman DK, Bunyan DP, Creswell JD, Jaremka LM. Psychological vulnerability and stress: the effects of self-affirmation on sympathetic nervous system responses to naturalistic stressors. Health Psychology. 2009;28:554–562. doi: 10.1037/a0014663. [DOI] [PubMed] [Google Scholar]
- Simons RL, Murry V, McLoyd V, Lin K-H, Cutrona C, Conger RD. Discrimination, crime, ethnic identity, and parenting as correlates of depressive symptoms among African American children: A multilevel analysis. Development and Psychopathology. 2002;14:371–393. doi: 10.1017/s0954579402002109. [DOI] [PubMed] [Google Scholar]
- Thayer ZM, Kuzawa CW. Ethnic discrimination predicts poor self-rated health and cortisol in pregnancy: Insights from New Zealand. Social Science & Medicine. 2015;128:36–42. doi: 10.1016/j.socscimed.2015.01.003. doi: http://dx.doi.org/10.1016/j.socscimed.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Thorburn S, Bogart LM. African American women and family planning services: perceptions of discrimination. Women & health. 2005;42:23–39. doi: 10.1300/J013v42n01_02. [DOI] [PubMed] [Google Scholar]
- van Jaarsveld CHM, Fidler JA, Steptoe A, Boniface D, Wardle J. Perceived stress and weight gain in adolescence: A longitudinal analysis. Obesity. 2009;17:2155–2161. doi: 10.1038/oby.2009.183. [DOI] [PubMed] [Google Scholar]
- Vines AI, Baird DD, Stevens J, Hertz-Picciotto I, Light KC, McNeilly M. Associations of abdominal fat with perceived racism and passive emotional responses to racism in African American women. American Journal of Public Health. 2007;97:526–530. doi: 10.2105/AJPH.2005.080663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A. Stress and adiposity: A meta-analysis of longitudinal studies. Obesity. 2011;19:771–778. doi: 10.1038/oby.2010.241. [DOI] [PubMed] [Google Scholar]
- Wells CS, Schwalberg R, Noonan G, Gabor V. Factors influencing inadequate and excessive weight gain in pregnancy: Colorado, 2000-2002. Maternal and Child Health Journal. 2006;10:55–62. doi: 10.1007/s10995-005-0034-2. [DOI] [PubMed] [Google Scholar]
- Westdahl C, Milan S, Magriples U, Kershaw TS, Rising SS, Ickovics JR. Social support and social conflict as predictors of prenatal depression. Obstetrics & Gynecology. 2007;110:131–140. doi: 10.1097/01.AOG.0000265352.61822.1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public health reports. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of behavioral medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yan Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]