Abstract
Purpose
To determine the prevalence and causes of decreased visual acuity (VA)
Design
Population-based cross-sectional study.
Participants
Multi-ethnic sample of children 30 to 72 months of age identified in Los Angeles.
Methods
All eligible children underwent comprehensive ophthalmic evaluation including monocular VA testing, cover testing, cycloplegic autorefraction, fundus evaluation, and VA retesting with refractive correction. Decreased visual acuity was defined as presenting or best-measured VA worse than 20/50 in children aged 30 to 47 months and worse than 20/40 for children 48 months of age and older. The prevalence and causes of decreased VA were determined, for both presenting and best-measured VA, in the better seeing and the worse seeing eyes.
Main Outcome Measures
Prevalence and causes of decreased vision.
Results
Presenting VA was assessed in 1840 children and best-measured VA in 1886 children. Presenting VA was decreased in the worse eye of 4.2% of Asian and 3.6% of Non-Hispanic White (NHW) children. Close to one fourth of these cases had no identifiable etiology, and 81% of these resolved on retesting. Decreased presenting VA in the worse eye with an identifiable ophthalmic etiology was present in 3.4% of Asian and 2.6% of NHW children. Decreased presenting VA attributable to simple refractive error (myopia ≥0.5 diopters [D]; hyperopia ≥3.0 D; astigmatism ≥2.0 D or ≥1.5 D for children >36 months of age) was present in the worse eye of 2.3% of Asian children and 1.4% of NHW children, and in the better eye of 0.5% of Asian children and 0.3% of NHW children. Decreased best-measured VA attributable to a cause was present in the worse eye of 1.2% of both Asian children and NHW children, and in the better eye of 0.2% of Asian and 0.3% of NHW children. Amblyopia related to refractive error was the most common cause, and ten times as common as ocular disease. Severe VI was rare.
Conclusion
Seventy percent of all decreased VA in Asian and NHW preschool children, and over 90% of decreased VA with an identifiable cause, is related to refractive error - either uncorrected refractive error or amblyopia due to refractive error.
Keywords: Prevalence, visual impairment, Asian, White, preschool children
Recently, the Multi-Ethnic Pediatric Eye Disease Study (MEPEDS)1 and the Baltimore Pediatric Eye Disease Study (BPEDS)2 published the findings of the first population-based studies on the prevalence and causes of visual impairment (VI) in children under 6 years of age in the United States. Uncorrected refractive error was a major underlying cause of presenting VI, and also of VI due to amblyopia, which persisted after refractive correction. To date, data have been reported in samples of African-American (MEPEDS and BPEDS), Hispanic (MEPEDS only) and Non-Hispanic White (BPEDS only) children. This report details the findings of the MEPEDS for Non-Hispanic White and Asian children.
Methods
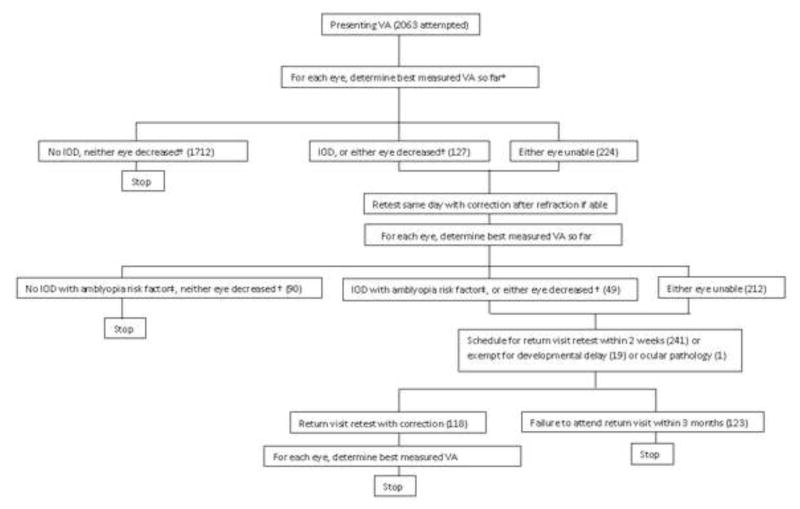
Details of the methods are published in an accompanying paper 3, 4. The visual acuity (VA) testing protocol 1,7 (summarized in Figure 1) was as follows: Presenting single-surround HOTV VA5, 6 was tested with correction, if worn, in children aged ≥30 months. A subsample of children also underwent quality control (QC) retesting of presenting VA. Taking the best result obtained so far for each eye, if VA was decreased in either eye (<20/50, or <20/40 in children ≥48 months of age) or there was a 2-line interocular difference (IOD) with VA ≤20/32 in the worse eye, VA was retested with correction after cycloplegic refraction. Taking the best result obtained so far for each eye, if VA was still decreased or untestable, or there was an IOD with an amblyopia risk factor, a return visit retest with correction was scheduled. “Presenting VA” refers to the first test performed, and does not include results from QC retesting. The “best-measured” VA for each eye was the best of all test results recorded for that eye.
Figure 1.
Visual acuity testing protocol.
VA: visual acuity. IOD: inter-ocular difference in visual acuity. *Factoring in results of quality control retest, performed in a subset of children >=36 months under same conditions as presenting VA test (with child’s own glasses if worn): for the first exam of the day for each examiner, and for children with VA worse than 20/32 in either eye, if a second examiner was available. † IOD is defined as inter-ocular VA difference >=2 lines with 20/32 or worse in the worse eye. Decreased VA is defined as worse than 20/50 at any age, or worse than 20/40 if >=48 months of age. ‡ See Methods for definitions of amblyopia risk factors.
Definition of Decreased Visual Acuity
Decreased VA was defined for both presenting and best-measured vision as VA worse than 20/50 in children aged 30 to 47 months and worse than 20/40 for children 48 months of age and older.
Definitions of Visual Impairment
Visual impairment (VI) and etiologies of presenting and best-measured VI were defined as previously described by the MEPEDS 1: VI was defined as decreased VA (<20/50, or <20/40 in children ≥48 months of age) in the presence of an identifiable ophthalmic etiology. Decreased presenting VA had an identifiable ophthalmic etiology if one of the following two conditions was met: (1) VA normalized with retesting (“resolving”), in the presence of visually significant uncorrected refractive error (spherical equivalent (SE) myopia of −0.5 diopters (D) or more, SE hyperopia of 3.0 D or more, or astigmatism of any axis of 2.0 D or more if 30–36 months old, or 1.5 D or more for children > 36 months of age); (2) VA did not normalize with retesting (“non-resolving”), in the presence of an identifiable ophthalmic etiology for decreased best-measured VA.
Causes of Visual Impairment
Decreased best-measured VA was considered to have an identifiable ophthalmic etiology, and classified as VI, if one of the following was identified: (1) ocular disease (normal vision precluded by the presence of an anterior segment abnormality, fundus abnormality or nystagmus); (2) amblyopia (see below); (3) probable amblyopia (see below); (4) probable refractive error (visually significant refractive error at presentation, unable to complete retest with correction). Unilateral amblyopia was a 2-line IOD in best-measured VA, with one or more of the following risk factors: strabismus; anisometropia (≥1.00 D SE anisohyperopia, ≥3.00 D SE anisomyopia, or ≥1.50 D anisoastigmatism); or visual axis obstruction. Bilateral amblyopia was defined as bilateral decreased best-measured VA (<20/50, or <20/40 in children ≥48 months of age) with bilateral visual axis obstruction or bilateral ametropia (≥4.00 D SE hyperopia, ≥6.00 D SE myopia, or ≥2.50 D astigmatism). Probable amblyopia was diagnosed in cases that almost met the definition of bilateral amblyopia due to bilateral ametropia: specifically, when VA in one eye was one line short of meeting the criteria and refractive error criteria were met, or when refractive error in one eye was 0.25 D short of meeting the criteria and VA criteria were met.
Statistical Analysis
The analysis cohort for presenting VA was defined as all children able to complete presenting VA measurements in both eyes. For best-measured VA it was defined as all children able to complete VA measurements in both eyes by the end of the retesting protocol. Prevalence was calculated as the ratio of the number of individuals with VI to the total number evaluated. Fisher’s exact test was used for comparison of proportions between groups. Confidence intervals (CI) reported for proportions are exact binomial 95% confidence intervals. All analyses employed a 0.05 significance level.
Results
Of 3039 Asian and Non-Hispanic White children examined (52% male), 2063 (1018 Asian, 1045 Non-Hispanic White) were ≥30 months of age. Of these, 912 Asian children (90%) were able to perform VA testing for both eyes on the first attempt, as were 927 Non-Hispanic White children (89%). One additional Non-Hispanic White child with unmeasurable VA (worse than 20/800) in one eye due to ocular disease was also considered testable in both eyes for the purposes of analysis. These 1840 children constitute the analysis cohort for presenting VA. An additional 27 Asian children and 19 Non-Hispanic White children who were unable to perform VA testing at presentation were able to complete testing in both eyes by the end of the retesting protocol (Figure 1). Thus, best-measured VA was analyzed in 939 Asian (92%) and 947 Non-Hispanic White children (91%). Among these, cycloplegic eyedrops were refused by 97 (10.3%) Asian and 111 (11.7%) Non-Hispanic White participants. Of children with presenting VA measurements, 2.2% wore refractive correction at the time of presentation.
Presenting visual acuity
Presenting VA was decreased in the worse eye of 4.2% of Asian children (38/912) and 3.6% of Non-Hispanic White children (33/928), and in the better eye of 0.9% of Asian children (8/912) and 1.0% of Non-Hispanic White children (9/928). For the worse eye, 82% of decreased presenting VA in Asian children (31/38) and 73% in Non-Hispanic White children (24/33) was attributable to an identifiable ophthalmic etiology and thus classified as VI. For the better eye, 88% of decreased presenting VA in Asian children (7/8) and 78% in Non-Hispanic White children (7/9) was attributable to an identifiable ophthalmic etiology and thus classified as VI. Decreased VA without an identifiable ophthalmic etiology is discussed further below.
VI at presentation was seen in the worse eye of 3.4% of Asian children (31/912) and 2.6% of Non-Hispanic White children (24/928), and in the better eye of 0.8% of Asian children (7/912) and 0.8% of Non-Hispanic White children (7/928) (Table 1). There was no significant difference in VI prevalence between Asian and Non-Hispanic White children for either the worse eye (p=0.34) or the better eye (p>0.99). There was no significant difference in VI prevalence between children <48 months, and children 48 months of age and older, for either the worse eye (p=0.15) or the better eye (p=0.40). Pooling presenting VA results from all children, 58% (32/55) of worse eye VI cases had presenting VA better than 20/80, as did 57% (8/14) of better eye VI cases (Table 2, available at http://aaojournal.org).
Table 1.
Prevalence of presenting visual impairment (decreased visual acuity with an ophthalmic etiology) stratified by age group, ethnicity and type of visual impairment.
| Type of Visual impairment | Asian | Non-Hispanic White | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Age (months) | Age (months) | |||||||||
|
| ||||||||||
| 30–35 (n=71) | 36–47 (n=243) | 48–59 (n=282) | 60–72 (n=316) | Total (n=912) | 30–35 (n=77) | 36–47 (n=258) | 48–59 (n=267) | 60–72 (n=326) | Total (n=928) | |
|
Worse eye, stratified by resolution with retesting protocol:*
n (% of age group) (95% CI**)
| ||||||||||
|
Non-resolving
|
0 | 4 (1.6) | 6 (2.1) | 0 | 10 (1.1) | 0 | 3 (1.2) | 3 (1.1) | 5 (1.5) | 11 (1.2) |
|
Resolving, with refractive error
|
2 (2.8) | 2 (0.8) | 9 (3.2) | 8 (2.5) | 21 (2.3) | 0 | 3 (1.2) | 7 (2.6) | 3 (0.9) | 13 (1.4) |
| Total | 2 (2.8) (0.3–9.8) |
6 (2.5) (0.9–5.3) |
15 (5.3) (3.0–8.6) |
8 (2.5) (1.1–4.9) |
31 (3.4) (2.3–4.8) |
0 | 6 (2.3) (0.9–5.0) |
10 (3.7) (1.8–6.8) |
8 (2.5) (1.1–4.8) |
24 (2.6) (1.7–3.8) |
|
| ||||||||||
|
Better eye, stratified by resolution with retesting protocol: n (% of age group) (95% CI)
| ||||||||||
|
Non-resolving
|
0 | 0 | 2 (0.7) | 0 | 2 (0.2) | 0 | 1 (0.4) | 1 (0.4) | 2 (0.6) | 4 (0.4) |
|
Resolving, with refractive error
|
0 | 1 (0.4) | 1 (0.4) | 3 (0.9) | 5 (0.5) | 0 | 1 (0.4) | 0 | 2 (0.6) | 3 (0.3) |
| Total | 0 | 1 (0.4) (0.0–2.3) |
3 (1.1) (0.2–3.1) |
3 (0.9) (0.2–2.8) |
7 (0.8) (0.3–1.6) |
0 | 2 (0.8) (0.1–2.8) |
1 (0.4) (0.0–2.1) |
4 (1.2) (0.3–3.1) |
7 (0.8) (0.3–1.6) |
Non-resolving: visual impairment by best measured as well as presenting visual acuity. Resolving, with refractive error: resolved during retesting protocol (Figure 1), with significant uncorrected refractive error at presentation: spherical equivalent (SE) hyperopia 3.0 diopters (D) or more, SE myopia 0.5 D or more, astigmatism 2.0 D or more at any age, or astigmatism 1.5 D or more for children >36 months of age.
CI: confidence interval (Exact 95% binomial confidence interval; calculated for total visual impairment in each age category).
Presenting visual acuity: visual impairment from uncorrected refractive error
Presenting VI was stratified according to whether or not VA normalized with retesting (Table 1). Two thirds of worse eye cases in Asian children and about half of those in Non-Hispanic White children (68% and 54%, respectively) resolved and were associated with a pre-specified level of visually significant uncorrected refractive error (see Methods) (“Resolving, with refractive error”, Table 1). Of better-eye cases, 71% in Asian children and 43% in Non-Hispanic White children resolved and were associated with significant refractive error. The remaining cases did not resolve over the course of retesting, and were associated with a variety of other identifiable ophthalmic etiologies (“Not resolving”, Table 1). These etiologies are discussed below in the context of best-measured VA.
The prevalence of worse eye VI at presentation attributed to refractive error was 2.3% in Asian children (21/912), and 1.4% in Non-Hispanic White children (13/928); this difference was not significant (p=0.17). The overall prevalence of better eye VI at presentation attributed to refractive error was 0.5% in Asian children (5/912), and 0.3% in Non-Hispanic White children (3/928) (p=0.50). The type of refractive error associated with cases of resolving VI tended to differ according to race/ethnicity (Table 3, available at http://aaojournal.org). Among Asian children with resolving worse eye VI, 67% were myopic, compared to 31% for Non-Hispanic White children. SE hyperopia was present in only 19% of Asian children with resolving VI, compared to 46% of Non-Hispanic White children. However, these differences were not statistically significant (p=0.08 and p=0.13, respectively).
Among all children with resolving worse-eye VI associated with refractive error, 9 (26%) had QC testing, and 5 of these resolved with QC testing alone, prior to refractive correction; by extrapolation, around half of all refractive error-associated resolving VI might have resolved due to retesting, regardless of refractive correction.
Best-measured visual acuity
Best-measured VA was decreased in the worse eye of 1.4% of Asian children (13/939) and 1.5% of Non-Hispanic White children (14/947), and in the better eye of 0.3% of Asian children (3/939) and 0.4% of Non-Hispanic White children (4/947). For the worse eye, 85% of decreased best-measured VA in Asian children (11/13) and 86% in Non-Hispanic White children (12/14) was attributable to an identifiable ophthalmic etiology and thus classified as VI. For the better eye, 67% of decreased best-measured VA in Asian children (2/3) and 75% in Non-Hispanic White children (3/4) was attributable to an identifiable ophthalmic etiology and thus classified as VI.
VI according to best-measured VA was seen in the worse eye of 1.2% of Asian children (11/939) and 1.3% of Non-Hispanic White children (12/947) (Table 4). It was seen in the better eye of 0.2% of Asian children (2/939) and 0.3% of Non-Hispanic White children (3/947) (Table 4). There were no significant differences between Asian and Non-Hispanic White children (p>0.99). There was no significant difference in VI prevalence between children <48 months, and children 48 months of age and older, for either the worse eye (p=0.83) or the better eye (p=0.66). Pooling best-measured VA results from all children, 14 of the 23 cases (61%) of worse eye VI had best-measured VA better than 20/80, as did 4 of 5 cases (80%) of better eye VI (Table 5, available at http://aaojournal.org).
Table 4.
Cause-specific prevalence of best-measured visual impairment (decreased visual acuity with an ophthalmic etiology) stratified by age and ethnic group.
| Asian | Non-Hispanic White | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Age in months | 30–35 (n=84) | 36–47 (n=254) | 48–59 (n=283) | 60–72 (n=318) | Total (n=939) | 30–35 (n=87) | 36–47 (n=266) | 48–59 (n=267) | 60–72 (n=327) | Total (n=947) |
|
Worse eye, stratified by etiology:*
n (% of age group) (95% CI**)
| ||||||||||
|
Ocular disease
|
0 | 0 | 0 | 0 | 0 | 0 | 1 (0.4) | 0 | 1 (0.3) | 2 (0.2) |
|
Amblyopia
|
0 | 4 (1.6) | 5 (1.8) | 0 | 9 (1.0) | 0 | 2 (0.8) | 3 (1.1) | 4 (1.2) | 9 (1.0) |
|
Prob. Amblyopia
|
0 | 1 (0.4) | 1 (0.4) | 0 | 2 (0.2) | 0 | 0 | 0 | 0 | 0 |
|
Prob. Refr. Error
|
0 | 0 | 0 | 0 | 0 | 0 | 1 (0.4) | 0 | 0 | 1 (0.1) |
| Total† | 0 | 5 (2.0) (0.6–4.5) |
6 (2.1) (0.8–4.6) |
0 |
11 (1.2) (0.6–2.1) |
0 | 4 (1.5) (0.4–3.8) |
3 (1.1) (0.2–3.3) |
5 (1.5) (0.5–3.5) |
12 (1.3) (0.7–2.2) |
|
| ||||||||||
|
Better eye, stratified by etiology: n (% of age group) (95% CI)
| ||||||||||
|
Ocular disease
|
0 | 0 | 0 | 0 | 0 | 0 | 1 (0.4) | 0 | 0 | 1 (0.1) |
|
Amblyopia
|
0 | 0 | 1 (0.4) | 0 | 1 (0.1) | 0 | 0 | 1 (0.4) | 1 (0.3) | 2 (0.2) |
|
Prob. Amblyopia
|
0 | 0 | 1 (0.4) | 0 | 1 (0.1) | 0 | 0 | 0 | 0 | 0 |
|
Prob. Refr. Error
|
0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total† | 0 | 0 | 2 (0.7) (0.1–2.5) |
0 |
2 (0.2) (0.0–0.8) |
0 | 1 (0.4) (0.0–2.1) |
1 (0.4) (0.0–2.1) |
1 (0.3) (0.0–1.7) |
3 (0.3) (0.1–0.9) |
Amblyopia: unilateral or bilateral amblyopia sufficient to cause visual impairment; note that this does not include milder cases of unilateral amblyopia in which the worse eye does not meet the definition of visual impairment. Prob. amblyopia: probable bilateral amblyopia; one line of acuity in one eye or 0.25 diopters in one eye short of bilateral amblyopia criteria. Prob. Refr. Error: probable refractive error; significant refractive error at presentation, not testable on retest.
CI: confidence interval (exact 95% binomial confidence interval; calculated for total visual impairment in each age category).
Numbers differ from Table 1 “not resolving” due to children untestable at presentation, and cases of better eye at presentation becoming worse eye for best measured acuity.
Causes of visual impairment
The causes of VI according to best-measured VA are shown in Table 4. All but one case was attributable to ocular disease or probable or definite amblyopia. One Non-Hispanic White child had decreased best-measured VA in one eye with significant uncorrected refractive error at presentation without ocular disease or amblyopia, and did not complete any VA retest with correction; the VI was attributed to probable refractive error. Excluding this child, 1.2% of Non-Hispanic White children (11/940) had VI in the worse eye due to ocular disease or to definite or probable amblyopia.
Structural eye anomalies or nystagmus (“ocular disease”, Table 4) causing bilateral VI were seen in only 1 Non-Hispanic White child with a history of retinopathy of prematurity. One additional Non-Hispanic White child had unilateral VI from ocular disease (optic atrophy). The overall prevalence of VI from ocular disease was 0.1% (2/1886) for the worse eye and 0.05% (1/1886) for the better eye. No additional cases of ocular disease likely to cause bilateral VI were identified after reviewing the records for all children 30–72 months of age who were excluded from analysis because of inability to perform VA testing.
Amblyopia was the most common cause of VI in the worse-seeing eye. Most of the children diagnosed with amblyopia as the cause of VI (14/18; 78%) had at least one retest of VA with refractive correction, at the time of the original visit or on a return visit retest without cycloplegia; the exceptions were 3 children with strabismic amblyopia, and one child with >3.0 D of uncorrected anisohyperopia. Ten of the 18 amblyopic children (56%) also completed an uncyclopleged retest with refractive correction. Amblyopia caused VI in the worse eye of 1.0% (9/939) of Asian children, one of whom had bilateral VI from bilateral ametropic amblyopia. An additional 0.2% of Asian children had probable bilateral amblyopia from bilateral ametropia. Amblyopia caused VI in the worse eye of 1.0% of Non-Hispanic White children (9/947); 2 of these children had bilateral VI from bilateral ametropic amblyopia.
VI in the worse eye caused by amblyopia or probable amblyopia was 10 times more common than that caused by ocular disease. For the better eye, VI caused by amblyopia or probable amblyopia was 4 times more common than that caused by ocular disease. The types of amblyopia and probable amblyopia causing VI are detailed in Table 6. VI from unilateral amblyopia was caused mostly (75% of cases) by hyperopic anisometropia or esotropia associated with high hyperopia. Of all cases of amblyopia or probable amblyopia causing VI in the worse eye, 85% (17/20) were attributable to refractive error or refractive error-related esotropia. Of these 17 children, only 18% already wore refractive correction (one Non-Hispanic White child and 2 Asian children).
Table 6.
Refractive error/ocular disease associated with type of amblyopia causing visual impairment, stratified by ethnicity.
| Unilateral amblyopia | Bilateral amblyopia (definite or probable) | |||
|---|---|---|---|---|
| Asian | Non-Hispanic White | Asian | Non-Hispanic White | |
| Myopia | 0 | 1* | 0 | 0 |
| Hyperopia | 5 | 4 | 2** | 1 |
| Astigmatism | 0 | 0 | 1 | 1 |
| Esotropia† | 3** | 1 | - | - |
| Exotropia | 1 | 1 | - | - |
| Total (n) | 9 | 7 | 3 | 2 |
This child, with unilateral amblyopia attributed to >4.5 diopters of anisomyopia, also had intermittent esotropia.
One Asian child with hyperopia and esotropia met both unilateral (strabismic) and bilateral amblyopia criteria, and is included in both categories.
Three of 4 esotropic children with unilateral strabismic amblyopia were hyperopic (≥ 4.5 diopters bilaterally).
There were only 2 children (0.1% of the sample) with best-measured VA in the worse eye poorer than 20/200 (one with amblyopia and one with retinopathy of prematurity). Only one child (the child with retinopathy of prematurity) met the World Health Organization (WHO) definition8 of “severe VI,”9 i.e., VA worse than 20/200 bilaterally; this child was also the only child who met the WHO definition of “any visual impairment,” i.e., better-eye VA worse than 20/60 (herein, 20/63).
The proportion of all presenting decreased VA in the worse eye having no identifiable ophthalmic etiology (not classified as VI) was 23% overall, and highest in the youngest age group; 60%, 29%, 11% and 24% of decreased presenting VA was unexplained by examination findings for children aged 30–35, 36–47, 48–59 and 60–72 months, respectively. Pooling all ages, 0.8% of Asian children and 1.0% of Non-Hispanic White children tested had decreased presenting VA in the worse eye without an identifiable etiology. These cases were stratified according to whether or not VA normalized with retesting; 81% (13/16) resolved, and of the remaining 3 children, 2 were not cooperative with attempted retesting.
Discussion
Visual impairment due to ocular disease, unilateral or bilateral amblyopia, or probable bilateral ametropic amblyopia, was seen in the worse eye of 1.2% of Asian and Non-Hispanic White children, and in the better eye of 0.2% to 0.3% of Asian and Non-Hispanic White children. In addition, correctable presenting VI associated with unmet need for refractive correction was seen in the worse eye of 2.3% of Asian children and 1.4% of Non-Hispanic White children, and in the better eye of 0.5% of Asian children and 0.3% of Non-Hispanic White children. There were no significant differences between races/ethnicities.
Considering the combined impact of presenting VI due to uncorrected refractive error, and the proportion of best-corrected VI that is attributable to refractive error-related amblyopia or strabismic amblyopia from refractive esotropia, over 90% of all presenting VI was ultimately attributable to refractive error. Considering all decreased VA, including both VI and decreased VA that did not have an identifiable cause (and which usually resolved with retesting), 70% of cases of decreased VA were ultimately attributable to refractive error.
As previously reported for other population-based samples of preschool children in the United States,1, 2 as well as in a study of mostly Asian and Caucasian preschool children in Australia,10 VI from ocular disease was rare, present in the worse eye of only 0.1% of children. Most VI that was not immediately correctable with spectacles was from definite amblyopia or probable amblyopia, consistent with previous reports.1, 2, 10–12 Similar to our previous findings in other racial/ethnic groups, 85% of amblyopia cases were directly or indirectly attributable to underlying refractive error. Hyperopia was the most frequent root cause in both racial/ethnic groups. Unfortunately, fewer than 1 in 5 of these amblyopic children needing refractive correction was receiving treatment with glasses. There are a variety of potential reasons for this, including both failure to detect the problem by standard screening, and failure to obtain recommended follow-up care if a problem was identified on screening. The low rate of appropriate treatment for these treatable conditions highlights the need for improved early detection, referral and treatment of amblyopia and amblyogenic conditions, particularly those associated with refractive error.
VI in the worse eye from definite amblyopia was seen in 1.0% of both Asian and Non-Hispanic White children. It should be noted that this is lower than the overall prevalence of amblyopia, because milder cases of unilateral amblyopia, in which the worse eye does not meet the criteria for VI, are not included. The rates of VI from definite amblyopia in Asian and Non-Hispanic White children are similar to those reported for similar racial/ethnic groups from population-based studies in other countries: in urban centers in India and China, the Refractive Error Study in Children (RESC) 13 reported VI in the worse eye from amblyopia in 0.6% and 0.9% of children respectively, 14 and in an Australian study of 6 year old children (66% white, 15% Asian), amblyopia caused worse-eye VI in 0.9% of children.12 More recently, the Sydney Pediatric Eye Disease study10 reported visual impairment in the worse eye from definite or probable amblyopia in a population of mostly Caucasian and Asian children to be 1.7%, somewhat higher than the overall prevalence (Asian and Non-Hispanic White) of 1.1% for definite or probable amblyopia in the present study. The difference in findings may be related to the fact that in the Sydney study, unlike the present study, those with a history of amblyopia or amblyopia treatment were included in the definition of amblyopia.
In addition to causing amblyopia, unmet need for refractive correction was associated with correctable VI in the worse eye in 2.3% of Asian and 1.4% of Non-Hispanic White children. Myopia tended to be more common in Asian children, but the differences were not significant. Robaei et al, though using a lower threshold for significant refractive error than MEPEDS, found similar results in 6- to 7-year-old Australian children: refractive error caused decreased worse-eye presenting VA in 2.0% of children. RESC data from 5–15 year-old Asian children in urban centers in India and China show a much higher rate of presenting VI with refractive error than in our Asian children, 7.3% and nearly 30% in India and China respectively.14 However, this is presumably due in large part to the older age of children in the RESC study, because of the age-related rise in myopia prevalence that is seen with increasing age in school-age children.
A majority of the children with VI had relatively mild VI, with VA better than 20/80. It should be noted that in some of these cases of mild VI attributable to refractive error, such as uncorrected low myopia, in which near VA would be expected to be normal, the VI may have relatively little impact on daily visual function.
Profound VI in preschool children was rare, as previously observed in the MEPEDS and other studies.1, 2, 12 Only one child had bilateral best-measured VA worse than 20/200 from an identifiable ophthalmic cause, and one additional child had best-measured VI worse than 20/200 in one eye. It should be noted that profound bilateral VI in multiply-disabled children could be underrepresented in MEPEDS if these children were less likely to participate.
As previously observed,1, 15 testability impacts the assessment of VA in young children. In the youngest age group, 60% of decreased presenting VA in the worse eye had no identifiable ophthalmic etiology. Retesting resulted in resolution of the apparent deficit in most cases. The issue of testability also impacts estimates of the prevalence of VI from refractive error, since a non-negligible proportion of presenting VI that resolves with refractive correction might be attributable to poor test performance with improvement on retesting, rather than to the refractive error itself. 1
Comparing our findings to those of the BPEDS for the same racial/ethnic group, our results for Non-Hispanic White children are very similar: the overall prevalence of decreased presenting VA (with or without an identified etiology) in Non-Hispanic White children was 3.6% and 3.5%, in the MEPEDS and BPEDS respectively, for the worse eye, and 1.0% and 1.2% for the better eye.2
Comparing our findings for different racial/ethnic groups within the MEPEDS, the pattern of observations for Non-Hispanic White and Asian children is very similar to that in Hispanic and African-American children, with most best-measured VI being caused by refractive error-related amblyopia. The prevalence of VI in the worse eye from definite amblyopia in African-American children in the MEPEDS was 1%, and in Hispanic children it was 1.4%.1 Neither prevalence is significantly different from that in either Asian or Non-Hispanic White children (p>0.36). On the other hand, higher prevalence of presenting refractive-error related VI was seen in both African-American (4.3% in the worse eye) and Hispanic (5.3%) children than in either Asian (p<0.01) or Non-Hispanic White children (p<0.0001). These differences may be related in part to racial/ethnic differences in refractive error prevalence; for example, the prevalence of astigmatism was observed to be lower in Non-Hispanic White children than in Hispanic and African-American children in the MEPEDS and BPEDS,16–18 and Asian children in the MEPEDS also have a lower prevalence of astigmatism4. Furthermore, access to early refractive correction may differ among racial/ethnic groups; in African-American and Hispanic children, only 1.6% of children presented wearing refractive correction, compared to 2.2% in the present report. In addition, the prevalence of unexplained decreased VA was higher in the earlier report (2.7% to 3.4%) than the 0.8% to 1.0% reported here (p<0.004), suggesting some testability differences between populations. For example, in the current report, children with a given level of refractive error may have been less likely to meet the pre-defined threshold for decreased VA.
Strengths of this study include the population-based study design, highly standardized protocol, retesting of children with refractive correction to confirm cases of suspected amblyopia, and large sample size. However, the findings reported here may not be generalizable to children in other racial/ethnic groups, or to children with different levels of access to health care.
In conclusion, Asian and Non-Hispanic White preschool children in California have a largely unmet burden of need for refractive correction, causing both easily correctable visual impairment and a more challenging burden of amblyopia. Seventy percent of all cases of decreased VA, and over 90% of all cases with an identifiable etiology, are ultimately attributable to refractive error. This reflects the need for improved early detection and treatment of significant refractive errors in preschool children.
Supplementary Material
Acknowledgments
Support: Supported by the National Eye Institute, National Institutes of Health, Bethesda, MD (grant nos. EY14472 and EY03040), and an unrestricted grant from the Research to Prevent Blindness, New York, NY. Dr. Varma is a Research to Prevent Blindness Sybil B. Harrington Scholar.
The Multi-Ethnic Pediatric Eye Disease Study investigators would like to thank the following members of the National Eye Institute’s Data Monitoring and Oversight Committee for their substantial contributions through critical review and advice: Jonathan M. Holmes, MD (Chair), Eileen E. Birch, PhD, Karen J. Cruickshanks, PhD, Natalie Kurinij, PhD, Maureen G. Maguire, PhD, Joseph M. Miller, MD, MPH, Graham E. Quinn, MD, and Karla Zadnik, OD, PhD.
Footnotes
Conflicts of Interest: The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
This article contains online-only material. The following should appear online-only: Table 2, Table 3, Table 5 and Appendix 1.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Multi-Ethnic Pediatric Eye Disease Study (MEPEDS) Group. Prevalence and causes of visual impairment in African-American and Hispanic preschool children: the Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. 2009;116:1990–2000. doi: 10.1016/j.ophtha.2009.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman DS, Repka MX, Katz J, et al. Prevalence of decreased visual acuity among preschool-aged children in an American urban population: the Baltimore Pediatric Eye Disease Study, methods, and results. Ophthalmology. 2008;115:1786–95. doi: 10.1016/j.ophtha.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varma R, Deneen J, Cotter S, et al. Multi-Ethnic Pediatric Eye Disease Study Group. The Multi-Ethnic Pediatric Eye Disease Study: design and methods. Ophthalmic Epidemiol. 2006;13:253–62. doi: 10.1080/09286580600719055. [DOI] [PubMed] [Google Scholar]
- 4.Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of amblyopia or strabismus in Asian and non-Hispanic white preschool children: Multi-Ethnic Pediatric Eye Disease Study. Ophthalmology. doi: 10.1016/j.ophtha.2013.03.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 6.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group. The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 7.Cotter SA, Tarczy-Hornoch K, Wang Y, et al. Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity testability in African-American and Hispanic children: the Multi-Ethnic Pediatric Eye Disease Study. Am J Ophthalmol. 2007;144:663–7. doi: 10.1016/j.ajo.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The prevention of blindness. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1973;518:1–18. [PubMed] [Google Scholar]
- 9.Steinkuller PG, Du L, Gilbert C, et al. Childhood blindness. J AAPOS. 1999;3:26–32. doi: 10.1016/s1091-8531(99)70091-1. [DOI] [PubMed] [Google Scholar]
- 10.Pai AS, Wang JJ, Samarawickrama C, et al. Prevalence and risk factors for visual impairment in preschool children: the Sydney Paediatric Eye Disease Study. Ophthalmology. 2011;118:1495–500. doi: 10.1016/j.ophtha.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 11.Robaei D, Huynh SC, Kifley A, Mitchell P. Correctable and non-correctable visual impairment in a population-based sample of 12-year-old Australian children. Am J Ophthalmol. 2006;142:112–8. doi: 10.1016/j.ajo.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 12.Robaei D, Rose K, Ojaimi E, et al. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005;112:1275–82. doi: 10.1016/j.ophtha.2005.01.052. [DOI] [PubMed] [Google Scholar]
- 13.Negrel AD, Maul E, Pokharel GP, et al. Refractive Error Study in Children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol. 2000;129:421–6. doi: 10.1016/s0002-9394(99)00455-9. [DOI] [PubMed] [Google Scholar]
- 14.He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci. 2004;45:793–9. doi: 10.1167/iovs.03-1051. [DOI] [PubMed] [Google Scholar]
- 15.Pan Y, Tarczy-Hornoch K, Cotter SA, et al. Multi-Ethnic Pediatric Eye Disease Study Group. Visual acuity norms in pre-school children: the Multi-Ethnic Pediatric Eye Disease Study. Optom Vis Sci. 2009;86:607–12. doi: 10.1097/OPX.0b013e3181a76e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKean-Cowdin R, Varma R, Cotter SA, et al. Joint Writing Committee for the Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups. Risk factors for astigmatism in preschool children: the Multi-Ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease Studies. Ophthalmology. 2011;118:1974–81. doi: 10.1016/j.ophtha.2011.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fozailoff A, Tarczy-Hornoch K, Cotter S, et al. Writing Committee for the MEPEDS Study Group. Prevalence of astigmatism in 6- to 72-month-old African American and Hispanic children: the Multi-ethnic Pediatric Eye Disease Study. Ophthalmology. 2011;118:284–93. doi: 10.1016/j.ophtha.2010.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giordano L, Friedman DS, Repka MX, et al. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:739–46. doi: 10.1016/j.ophtha.2008.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.