Abstract
Maximum contaminant levels created by the U.S. Environmental Protection Agency under the Safe Drinking Water Act do not apply to private wells. Rather, the onus is on individual households to undertake regular water testing. Several barriers exist to testing and treating water from private wells, including a lack of awareness about both well water as a potential source of contaminants and government-recommended water testing schedules; a health literacy level that may not be sufficient to interpret complex environmental health messages; the inconvenience of water testing; the financial costs of testing and treatment; and a myriad of available treatment options. The existence of these barriers is problematic because well water can be a source of hazardous contaminants. This article describes an initiative—undertaken by the Tuftonboro (New Hampshire) Conservation Commission, with support from state agencies and a research program at Dartmouth College—to increase water testing rates in a rural region with a relatively high number of wells. The project prompted more water tests at the state laboratory in one day than in the prior six years. This suggests that community-driven, collaborative efforts to overcome practical barriers could be successful at raising testing rates and ultimately improving public health.
Introduction
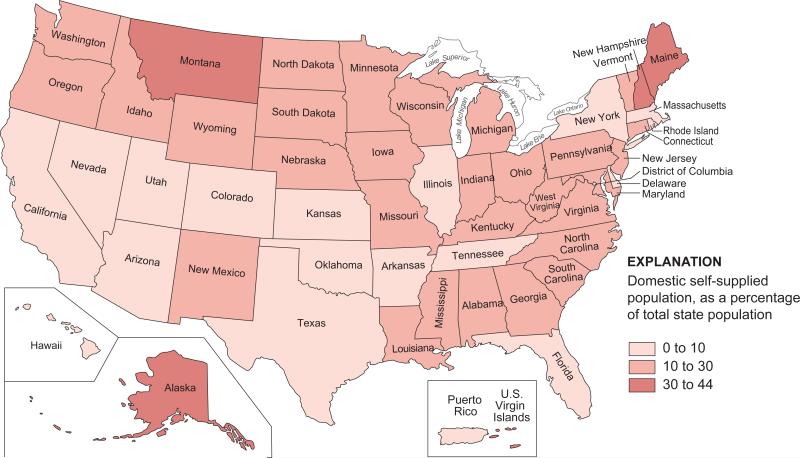
Approximately one-sixth of U.S. households obtain drinking water from a private well (Kenny et al., 2009). In New Hampshire, more than 40% of the population obtains household water from an unregulated well (Figure 1) (Kenny et al., 2009). Under the Safe Drinking Water Act (SDWA), the U.S. Environmental Protection Agency (U.S. EPA) regulates public drinking water supplies by establishing maximum contaminant levels (MCLs) and delegating enforcement to states and tribes to ensure water systems conform with the MCLs (Levine, 2012; Tiemann, 2010). The SDWA defines a contaminant as “any physical, chemical, biological, or radiological substance or matter in water.” Private well water is not tested for compliance with MCLs unless it (1) provides piped water for human consumption to at least 15 service connections (community water systems) or (2) regularly serves at least 25 of the same people for 60 days a year (nontransient, non-community water systems) (Tiemann, 2010; U.S. Environmental Protection Agency [U.S. EPA], 2012a). Therefore, households with wells are responsible for regular water testing to detect contaminants and for applying treatment when necessary.
FIGURE 1.
Percentage of Total State Population With a Self-Supplied Domestic Water Source
Potential Human Health Effects of Drinking Water From Private Wells
Untreated water from private wells can be a source of unsafe levels of contaminants (Table 1) (Charrios, 2010; Committee on Environmental Health & Committee on Infectious Diseases [CEHCID], 2009; Walker, Shaw, & Benson, 2006). Ingestion of contaminated water can cause both acute and chronic illness and certain contaminants are particularly hazardous to fetuses, infants, and children (Brender et al., 2013; CEHCID, 2009; Dangleben, Skibola, & Smith, 2013; Farzan, Karagas, & Chen, 2013; Hexemer et al., 2008; Hilborn et al., 2013; Naujokas et al., 2013; Rahman et al., 2010; Reynolds, Mena, & Gerba, 2008; Smith & Steinmaus, 2009). Bacteria, viruses, and parasites cause gastrointestinal illnesses; contaminants, such as radon, arsenic, chromium, and trichloroethylene are carcinogenic; and studies associate consumption of nitrates with a host of health effects and abnormal fetal development (Ward et al., 2005). Few studies have explored complex mixtures of contaminants and their additive or synergistic effects on health (Ryker & Small, 2008).
TABLE 1.
Sources, Human Health Benchmarks, and Possible Health Effects of Contaminants Potentially Present in New Hampshire Domestic Well Watera
| Contaminant | Source | Human Health Benchmark | Possible Health Effects | |
|---|---|---|---|---|
| Value | Typeb | |||
| Arsenic | Erosion of natural deposits; runoff from historic pesticide or insecticide application; industrial waste | 0.01 mg/L | MCL | Increased risk of several cancers; circulatory problems; endocrine disruption |
| E. coli; Legionella; Giardia; Cryptosporidium | Human and animal fecal waste; some are naturally present | Goal = zero; No more than 5.0% samples total coliform positive in a month |
Gastrointestinal illness (diarrhea, vomiting, cramps); Legionnaires' disease | |
| Fluoride | Naturally in water in a few parts of the U.S. | 4.0 mg/L | MCL | Dental fluorosis at high doses; increased risk of bone fractures |
| Lead | Corrosion of household plumbing; erosion of natural deposits | 0.015 mg/L | U.S. EPA action level | Children: developmental delays; possible deficits in attention span and learning abilities Adults: kidney problems; high blood pressure |
| Manganese | Soil; aquifers; gasoline | 0.05 mg/L | Secondary MCL | Neurological effects; manganism; some evidence that shower inhalation can cause toxicity |
| Nitrate | Fertilizer use; manure; sewage and septic-system effluent; aquifer materials | 10 mg/L | MCL | Neural tube defects; central nervous system defects; oral cleft defects; musculoskeletal defects; congenital heart defects; methemoglobinemia; possible promoter of carcinogenesis |
| Nitrite | 1 mg/L | |||
| Radon | Radioactive decay of uranium in aquifer; building materials | 2000 pCi/L | NH DES action level | Increased risk of lung cancer for radon in air; increase in risk of stomach cancer for ingested radon |
| Uranium | Aquifers | 0.03 mg/L | MCL | Increased risk of cancer; kidney toxicity |
| Volatile organics and pesticides (e.g., MtBE) | Dry cleaning and gasoline; leaking storage tanks and pipelines; gasoline spills; air deposition; unidentified sources | 0.013 mg/L | NH DES HBSL for MtBE | Compound-specific effects |
Modified and adapted from DeSimone, Hamilton, & Gillom, 2009 and AAP Committee on Environmental Health and Committee on Infectious Diseases, 2009.
MCL = maximum contaminant level; U.S. EPA = U.S. Environmental Protection Agency; NH DES = New Hampshire
Department of Environmental Services; HBSL = health-based screening level.
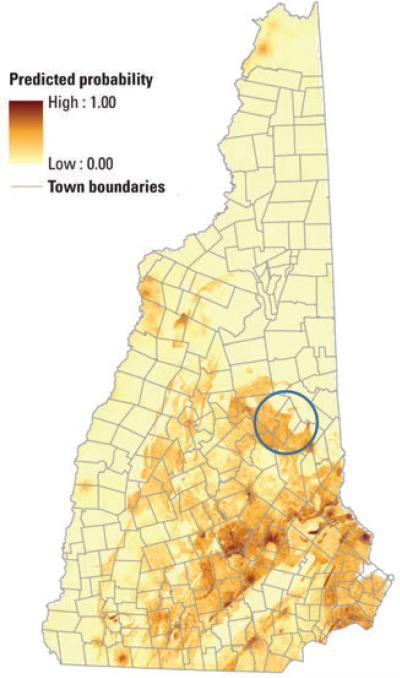
In New Hampshire wells, several contaminants are found at levels of concern, including arsenic, radon, and uranium. Low levels of arsenic are likely in nearly 40% of New Hampshire's groundwater (Figure 2) (Ayotte, Cahillaine, Hayes, & Robinson, 2012). Public health officials estimate that approximately one in five New Hampshire wells has arsenic in excess of the U.S. EPA MCL of 0.01 mg/L (Montgomery, Ayotte, Carroll, & Hamlin, 2003). Arsenic is a concern due to both its status as a class 1 carcinogen (Anders et al., 2004) and its place atop of the 2011 Priority List of Hazardous Substances published by the Agency for Toxic Substances and Disease Registry, which is a ranking of substances based on a combination of their frequency, toxicity, and potential for human exposure at Superfund sites (Agency for Toxic Substances and Disease Registry, 2011). The major concern of ingesting inorganic arsenic is cancer, but dermatological, developmental, neurological, respiratory, cardiovascular, immunological, and endocrine effects are also evident (Hughes, Beck, Chen, Lewis, & Thomas, 2011; Martinez, Vucic, Becker-Santos, Gil, & Lam, 2011; Naujokas et al., 2013; Nuckols et al., 2011; Parvez et al., 2013; Rahman et al., 2010). Evidence is growing that links prenatal and early-life exposure to arsenic with long-term health implications (Farzan et al, 2013) and deleterious effects on the immune system (Dangleben et al., 2013).
FIGURE 2.
Probability of Arsenic Concentration in Groundwater From Bedrock Aquifers in New Hampshire Exceeding 0.01 mg/L
As estimated from a U.S. Geological Survey model. Tuftonboro is located inside the blue circle. Adapted from Ayotte et al., 2012.
Radon is also commonly present in New Hampshire well water. Approximately 50%–60% of all private drilled wells in New Hampshire produce water with radon concentrations between 300 and 4,000 picocuries per liter (pCi/L) (New Hampshire Department of Environmental Services, 2009). Although the ingestion risk of radon is smaller than the risk associated with inhalation, drinking water with radon increases the risk of developing stomach cancer (Catelinois et al., 2006; Hopke et al., 2000). Of the estimated 168 cancer deaths per year due to radon in drinking water, 11% of the deaths are from stomach cancer caused by ingestion (National Research Council, 1999; U.S. EPA, 2012b). Furthermore, radon in water vaporizes during normal usage and contributes to the overall level of radon in indoor air (Collman, Loomis, & Sandler, 1991).
A small number of New Hampshire wells contain uranium above the U.S. EPA MCL (0.03 mg/L). Possible biological effects of drinking uranium above 0.03 mg/L over a long period include vitamin D and iron homeostasis, bone volume decrease and healing interference, and adverse effects on the kidneys (Canu, Laurent, Pires, Laurier, & Dublineau, 2011). Lower levels of uranium in drinking water have also been associated with high blood pressure (Frisbie, Mitchell, & Sarkar, 2013).
Communicating With Households About Private Wells
Encouraging citizens to monitor their homes is a formidable task (Doyle et al., 1990) and studies indicate that a significant proportion of households are unaware of the need for regular water quality testing (Novokowski, Beatty, Conboy, & Lebedin, 2006). For example, in a rural area of Canada, only 8% of survey respondents had tested their well water at a frequency that met the recommended testing schedule and 20% of households that had tested did not know which tests were performed (Jones et al., 2006). Another study in two rural U.S. counties found that a quarter of respondents with wells had never thought about taking precautions to limit their children's exposure to contaminants, and only one-third of respondents had ever previously tested their water (Postma, Butterfield, Odom-Maryon, Hill, & Butterfield, 2011). At least one study concluded that education, income, age, and homeowner status are all significantly associated with water testing rates (Jones et al., 2005). Treatment rates are also low; a survey in a rural county in Nevada where the media reported extensively about arsenic in drinking water found that only 38% of residents applied treatment (Walker et al., 2006).
Hazard perception is another challenge. No time pressure exists to complete the testing and treatment process and certain contaminants found in well water possess characteristics that lead people to accept the risks associated with drinking well water (Covello, 2008). People may dismiss the risks associated with drinking water because of the following risk characteristics, which have also been identified as reasons people fail to address radon in indoor air (Doyle et al., 1990):
The objective probability of the health risk is often below the level at which people understand and respond appropriately;
Often no perceptual cues or reminders exist to alert people to the presence of the risk (e.g., arsenic is colorless, odorless, and tasteless in water);
Contaminants in well water are often of geological origin, so no villain exists to whom the household can easily assign blame or responsibility;
People's experience with the risk is generally benign in the sense that many have lived in their homes years without experiencing any easily attributable health effect;
The effect of the risk is far removed from the initial exposure (e.g., arsenic-induced cancer takes many years to develop);
Deaths due to contaminant consumption are not dramatic, occur singly, and are impossible to unequivocally relate to consumption; and
The risk is not the same for everyone but varies in complex ways depending on several dimensions (e.g., location, soil type, well structure).
Additional commonly reported obstacles to water testing and treatment rates include inconvenience, economic costs, inability to interpret test results, and uncertainty over the reliability of treatment companies or performance of systems (Jones et al., 2006; Kreutzwiser, de Loe, & Imgrund, 2010; Kreutzwiser et al., 2011; Montgomery et al., 2003). Self-installation treatment systems are available, but they have startup and maintenance costs, require skills to install, and are typically contaminant specific. Finally, water quality information and test results contain complex terms, labels, and numbers with various confounding units; thus, we suspect that health literacy levels are also an understudied contributor to low treatment rates. Health literacy is “the degree to which individuals have the capacity to obtain, process, and understand basic health information . . . needed to make appropriate health decisions (Ratzan & Parker, 2000),” and it refers to “... understanding and using information to make health decisions (Peerson & Saunders, 2009).” It includes the ability to use quantitative information (Berkman, Davis, & McCormack, 2010). Almost 9 out of 10 U.S. adults have difficulty applying everyday health information (Kutner, Greenberg, Jin, & Paulsen, 2006).
Recent research suggests public health officials must design interventions and materials to address these barriers. In Waterloo, Canada, removing the barriers of cost and inconvenience approximately doubled the background testing rate (Hexemer et al., 2008). A thorough analysis identified complacency and inconvenience as the most significant barriers and confirmed that household knowledge and better information alone were weak bases for predicting higher testing rates (Imgrund, Kreutzwiser, & de Loe, 2011).
Community-Level Interventions and Behavior Change
Community-based participatory research and other forms of community-engaged research encourage involvement of communities in the formation of research and solutions (Brown et al., 2012; O'Fallon & Dearry, 2002). Researchers and communities increasingly report that partnership-driven, community-level interventions are successful in promoting healthy behaviors (Brown et al., 2012; Downs et al., 2010). Partnership-driven efforts build social capital, empower households, and help develop locally appropriate management strategies (Arnold & Fernandez-Gimenez, 2007; Berkes, 2009; Downs et al., 2010). Findings suggest target populations may ignore messages when community leaders do not sufficiently participate in the design of interventions; thus, communication may not clarify the public health hazard and has the potential to expand the gap between perceived and actual risk. High levels of public disinterest and apathy have been reported in many “technocratic” approaches (Covello, 2008; Doyle et al., 1991; Slovic, 1987).
Participatory testing and reporting refers to an approach that enables community members to participate in meaningful and empowering ways in the testing activity and reporting of results (Downs et al., 2010). The work described here was “participatory” in that 1) a local group of volunteers consulted an academic research program and state agency to conceive, design, and implement a water testing program; and 2) the volunteers led an effort to report the results to local leaders and the community with support from the other partners.
Methods
Partnership to Increase Well Water Testing Rates in Tuftonboro, New Hampshire
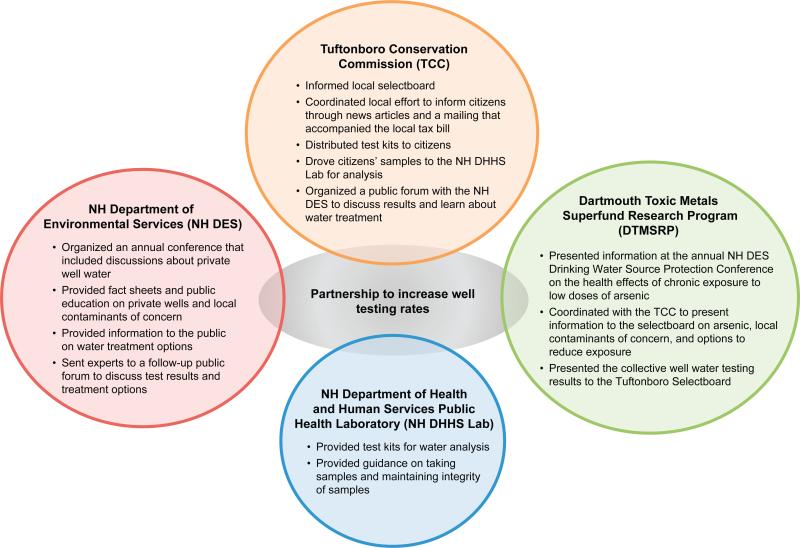
In 2012, the Tuftonboro Conservation Commission (TCC) initiated an effort to inform local residents about the potential health effects of well water. TCC began by inviting the Dartmouth Toxic Metals Superfund Research Program (DTMSRP) to present to the Tuftonboro Selectboard (Figure 3). A member of DTMSRP presented information about the health effects of contaminants in well water and provided information about protective actions. The selectboard responded with support for an informational campaign. TCC subsequently planned a well water testing service for residents in order to make testing accessible and reduce its overall inconvenience.
FIGURE 3.
Partners Involved in a Pilot Project to Increase Well Testing Rates in Tuftonboro, New Hampshire
Table 2 outlines the timeline of the water testing campaign in 2012. In short, TCC contacted the New Hampshire Department of Health and Human Services Public Health Laboratory (NH DHHS Lab) to obtain water testing kits for distribution to residents. TCC disseminated and publicized information about well water and notified the community about dates TCC would distribute testing kits. After collecting samples, forms, and money, a volunteer delivered the time-sensitive samples to the NH DHHS Lab, which was a 70-minute drive (140 minutes round trip). The volunteer ensured correct transfer of test forms and samples, and TCC coordinated the delivery of results to residents. Residents were provided the option to choose a basic analysis, a standard analysis, a radiological analysis, or individual contaminants. Results were subsequently delivered to residents, and personally identifiable information was removed so the collective results could be presented to the selectboard by a member of DTMSRP. Finally, TCC organized a well water forum in collaboration with the New Hampshire Department of Environmental Services (NH DES) to answer residents’ questions about results and treatment. In total, TCC estimated it spent more than 100 man-hours organizing the campaign in 2012. TCC repeated the process in 2013.
TABLE 2.
Timeline of Partnership and Events
| Month in 2012 | Eventa |
|---|---|
| May | Three TCC members attend the NH DES Drinking Water Source Protection Workshop. Dr. Josh Hamilton of DTMSRP presents information on the potential health effects of arsenic in New Hampshire well water. |
| TCC researches the issue of contaminants in well water and presents the information at the next TCC meeting. TCC agrees to approach the Tuftonboro Selectboard about organizing a public information program. | |
| A member of the DTMSRP presents information to the Tuftonboro Selectboard about the potential health effects of common contaminants, a regulatory overview, and information about other local ordinances. The Tuftonboro Selectboard responds with support for an informational campaign. TCC meets to discuss a plan of action. | |
| TCC contacts several water testing labs to determine the cost of testing and service options. | |
| June | A member of TCC continues to attend selectboard meetings to report progress, receive formal approval, and to ensure the proposed project was covered by the local media. |
| TCC produces two articles about arsenic and other pollutants found in New Hampshire wells and the potential health effects. The articles appear in the town newsletter and a local paper. A reporter from the paper also publishes an article about a resident who had discovered an extremely high level of arsenic in their water. | |
| TCC announces plans to offer a water testing service and produces posters and a supplemental instruction sheet for residents. TCC also posts notices at three post offices and the library. | |
| July | TCC distributes water testing kits at the town transfer station. Members of the TCC set up displays that include handouts from DTMSRP and NH DES. TCC makes three trips to the NH DHHS Lab to pick up test kits because demand exceeds estimations. |
| In shifts, members of TCC collect water samples at the town transfer station. TCC checks residents' paperwork and collects money for the cost of water tests. The samples are properly bagged and refrigerated. The next morning two members deliver the samples to the state lab and help technicians organize the samples. | |
| August | As residents receive water test results from the state lab, several members help people interpret reports or refer people to NH DES for technical assistance. |
| September | TCC begins planning a public forum for residents to include information about interpreting water test results and treatment options. |
| TCC prepares a notice to be included with tax bills and a press release to advertise the Well Water Forum. | |
| October | The first collection event in 2012 prompts 122 water samples. A member of DTMSRP presents the collective results of the water tests. |
| November | NH DES and TCC hold a Well Water Forum where testing and treatment specialists present information on interpreting water tests and respond to questions about water treatment. |
| TCC distributes, collects, and delivers additional test kits to the NH DHHS Lab. |
TCC = Tuftonboro Conservation Commission; NH DES = New Hampshire Department of Environmental Services; DTMSRP = Dartmouth Toxic Metals Superfund Research Program; NH DHHS = New Hampshire Department of Health and Human Services.
Community and Partners Involved
TCC
TCC is composed of four year-round volunteer residents. Conservation commissions are composed of volunteers who work to study and protect local natural resources. Three members planned and carried out the water testing events, extending the mission of TCC to protect residents from the consequences of contaminants in well water. Tuftonboro is located in Carroll County, New Hampshire. Carroll County has fewer than 50,000 people and Tuftonboro has approximately 2,500, with the number of residents markedly increasing during the summer months. Tuftonboro is a summer vacation spot on the north shore of Lake Winnipesaukee, with a marina and many lakeside homes and rental cottages.
DTMSRP
DTMSRP is a research program funded by the National Institute of Environmental Health Sciences. A focus of the program is to investigate the health effects of arsenic in well water, and informing residents about arsenic in well water has been a priority of DTMSRP since its inception. The Research Translation and Community Engagement Cores maintain a Web site with frequently asked questions and water testing information. The Research Translation Core created a 10-minute movie, In Small Doses: Arsenic, about arsenic in wells. The cores frequently organize public events to promote water testing, and they have a prominent role in the coordination of the New Hampshire Arsenic Consortium, which is an annual meeting of regional professionals to share information on arsenic in well water.
NH DES
NH DES produces drinking water fact sheets, provides technical assistance about testing and treatment to residents, and conducts outreach to promote testing and treatment. Private well installation and related construction standards are administered by the New Hampshire Water Well Board. The board along with NH DES is primarily responsible for licensing well and pump contractors, maintaining well construction records, and adopting and enforcing standards for the construction of wells and the installation of pumps. NH DES recommends private well users test their water annually for bacteria and nitrates, and every three to five years for a suite of other contaminants. The agency also maintains a list of accredited labs that provide services locally.
NH DHHS Lab
The NH DHHS Lab provides analytical testing services of water, wastes, hazardous materials, soils, and other chemical matrices for all state agencies and citizens. The NH DHHS Lab's mission is to meet clients’ needs and requirements, comply with all applicable quality assurance and quality control objectives, and comply with current applicable government standards and regulations. Its policy is to assist clients in understanding and interpreting the relevance of their test results by providing educational material and personal communication.
Results
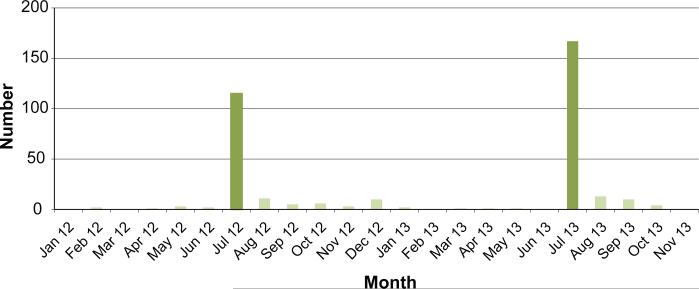
In total, TCC collected and delivered 285 water samples to the NH DHHS Lab in July 2012 and July 2013 (Figure 4), which was more than triple the number of water samples tested at the same lab in the previous six years (the NH DHHS Lab tested just 83 water samples from Tuftonboro from 2006 to 2012). After the first sample collection event in 2012, the TCC delivered 122 water samples in July and then 37 other samples prompted by follow-up publicity and a Well Water Forum led by NH DES. In 2013, TCC collected and delivered a total of 163 water samples after the sample collection event and then 27 in the following months. Alarmingly, 28% of water samples exceeded the arsenic MCL and 23% were positive for total coliform bacteria. Of the 79 samples that underwent a radiological analysis, 24 water samples (34%) had greater than 2,000 pCi/L of radon, which is the NH DES recommended action level. The combined results are summarized in Table 3.
FIGURE 4.
Number of Well Water Samples Processed by the New Hampshire Department of Health and Human Services Lab from Tuftonboro, Melvin Village, and Mirror Lake in Each Month of 2012–2013
The Tuftonboro Conservation Commission held community water testing events in July 2012 and July 2013. Over the previous six-year period, the state lab processed a total of 83 samples from these three communities.
TABLE 3.
Tuftonboro Area Homeowner Survey, June 2012 and June 2013
| Parameter | Samples | Limit Typea | Limit Value | # Above Limit | % |
|---|---|---|---|---|---|
| Total coliform bacteria | 258 | MCL | 0 cts/100/mLb | 61 | 23.64 |
| Noncoliform counts | 258 | >200 cts/100/mL | 40 | 15.50 | |
| E. coli bacteria | 258 | MCL | 0 cts/100/mL | 14 | 5.43 |
| Analytical gross alpha | 8 | MCL | 15 pCi/L | 0 | 0.00 |
| Arsenic | 275 | MCL | 0.01 mg/L | 77 | 28.00 |
| Chloride | 246 | SMCL | 250 mg/L | 4 | 1.63 |
| Copper | 237 | SMCL | 1.0 mg/L | 1 | 0.42 |
| Copper-stagnant | 232 | SMCL | 1.0 mg/L | 22 | 9.48 |
| Fluoride | 240 | MCL | 4.0 mg/L | 10 | 4.17 |
| Fluoride SMCL | 240 | SMCL | 2.0 mg/L | 33 | 13.75 |
| Hardness | 237 | 250 mg/L | 0 | 0.00 | |
| Iron | 237 | SMCL | 0.3 mg/L | 17 | 7.17 |
| Lead | 237 | AL | 0.015 mg/L | 1 | 0.42 |
| Lead-stagnant | 232 | AL | 0.015 mg/L | 23 | 9.91 |
| Manganese | 237 | SMCL | 0.05 mg/L | 20 | 8.44 |
| Nitrate | 246 | MCL | 10 mg/L | 21 | 8.54 |
| Nitrite | 246 | MCL | 1 mg/L | 0 | 0.00 |
| Radon | 79 | 2000 pCi/L | 24 | 30.38 | |
| Sodium | 237 | SMCL | 250 mg/L | 1 | 0.42 |
| Uranium | 237 | MCL | .030 mg/L | 0 | 0.00 |
| pH | 237 | pH <6.5 | 37 | 15.61 | |
| 237 | pH >8.5 | 8 | 3.38 | ||
| Volatile organic compounds | 3 | MCL | varies with compound | 0 | 0.00 |
| Alkalinity | 2 | 0 | 0.00 |
MCL = maximum contaminant level for public water systems; SMCL= secondary maximum contaminant level for public water systems; AL= action level for public water systems.
PRESENT is unacceptable.
Discussion
We consider the participatory water testing program designed and implemented by TCC to be successful. The program raised awareness about the potential hazards of well water among local community leaders and empowered many residents to test their water. The reporting of results also sprouted other community-led testing initiatives in New Hampshire. Elements that contributed to the success of the program included the following:
Targeted messages. TCC used local media to significantly raise public awareness, and the efforts to promote the water testing service were well timed.
Support from the town selectboard. TCC worked together with the town select-board, keeping the town leaders informed about its actions, and the selectboard supported the TCC's testing service by providing reimbursement to the TCC member who transported the water samples to the NH DHHS Lab. Members of TCC attended selectboard meetings each month to report on progress leading up to the events. The meeting minutes are published and read by town residents.
Persistence. TCC volunteered a substantial amount of time over the course of two years to plan, inform citizens, and hold events.
Dedicated and compassionate volunteers. Informed members of TCC provided individual assistance to residents on what tests to select, how to draw the samples, and what payment to make.
The actions of TCC addressed factors that have previously been found to influence testing behavior. First, TCC likely changed local attitudes through a public information campaign focused on providing facts and stories about local residents who were dealing with contamination. The publicity may have boosted household knowledge and altered a common misperception that unsafe water must taste or smell abnormally. Second, TCC learned that the inconvenience of water testing may be an important structural constraint, especially in rural regions. TCC made water testing more accessible for people by distributing test kits, driving samples to the lab, and reducing the overall effort needed to obtain and interpret results. This reinforces previous findings that merely providing the public with information is not sufficient to ensure that decisions are consistent with the actual level of risk (Imgrund et al., 2011; Madajewicz et al., 2007; Walker, Shaw, & Benson, 2006).
The overall effectiveness of the program in reducing exposure is difficult to evaluate because we did not measure the rate of treatment and did not formally follow up with households about whether they acted on the test results. This limits our ability to analyze how people interpreted water test results and whether the information they received was actionable. Future programs should contain a mechanism to measure treatment rates, since water testing alone does not reduce exposure to contaminated water. Comments from TCC emphasized the need for clear and simple instructions with test kits and the need for water test results to highlight elevated levels of particular contaminants. We are also unable to definitively state that the water testing program increased the background water testing rate in Tuftonboro because private laboratories in New Hampshire do not release data on the number of samples tested at their facilities. It is possible a significant number of people used private lab services, which could mean 1) more people tested prior to the efforts of TCC, or 2) the number of water tests prompted by the TCC is higher, which would result in a smaller or larger increase of the background water testing rate, respectively.
Conclusion
Water from private wells is largely unmonitored and private well users are often unaware of the potential presence of contaminants. In the absence of protective laws, convincing households to follow recommended testing schedules is necessary to protect public health. Participatory programs that reduce the barriers to testing and treatment can help certain communities increase the likelihood of protective behaviors. The pilot program described here was successful in raising local awareness and prompting residents to test their water. Further programs and research should explore the other testing and treatment constraints.
Acknowledgements
DTMSRP is supported by funds from National Institute of Health Grant Number P42ES07373. The authors are solely responsible for this content; it does not represent the official views of the National Institute of Environmental Health Sciences or the National Institutes of Health.
Contributor Information
Michael P. Paul, Toxic Metals Superfund Research Program, The Audrey and Theodor Geisel School of Medicine at Dartmouth.
Pierce Rigrod, New Hampshire Department of Environmental Services.
Steve Wingate, Tuftonboro Conservation Commission.
Mark E. Borsuk, Thayer School of Engineering, Dartmouth College.
References
- Agency for Toxic Substances and Disease Registry The ATSDR 2011 substance priority list. 2011 Retrieved from http://www.atsdr.cdc.gov/spl/
- Anders WM, Bull RJ, Cantor KP, Chakraborti D, Chen C, DeAngelo AB, DeMarini DM, Ferreccio C, Fukushima S, Gebel TW, Mazumder DN, Karagas MR, Kogevinas M, Komulainen H, Le Curieux F, Meharg A, Ng JC, Nieuwenhuijsen MJ, Olin S, Pereira M, Rahman M, Roberson JA, the Working Group on the Evaluation of Carcinogenic Risks to Humans . Some drinking-water disinfectants and contaminats, including arsenic. Vol. 84. World Health Organization; Geneva: 2004. [Google Scholar]
- Arnold JS, Fernandez-Gimenez M. Building social capital through participatory research: An analysis of collaboration on Tohono O'odham tribal rangelands in Arizona. Society and Natural Resources: An International Journal. 2007;20(6):481–495. [Google Scholar]
- Ayotte JD, Cahillaine M, Hayes L, Robinson KW. Estimated probability of arsenic in groundwater from bedrock aquifers in New Hampshire, 2011. 2012 Retrieved from http://pubs.usgs.gov/sir/2012/5156/
- Berkes F. Evolution of co-management: Role of knowledge generation, bridging organizations, and social learning. Journal of Environmental Management. 2009;90(5):1692–1702. doi: 10.1016/j.jenvman.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Davis TC, McCormack L. Health literacy: What is it? Journal of Health Communication: International Perspectives. 2010;15(Suppl. 2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- Brender JD, Weyer PJ, Romitti PA, Mohanty BP, Shinde MU, Vuong AM, Sharkey JR, Dwivedi D, Horel SA, Kantamneni J, Huber JC, Jr., Zheng Q, Werler MM, Kelley KE, Griesenbeck JS, Zhan FB, Langlois PH, Suarez L, Canfield MA, the National Birth Defects Prevention Study Prenatal nitrate intake from drinking water and selected birth defects in offspring of participants in the national birth defects prevention study. Environmental Health Perspectives. 2013;121(9):1083–1089. doi: 10.1289/ehp.1206249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown P, Brody JG, Morello-Frosch R, Tovar J, Zota AR, Rudel RA. Measuring the success of community science: The northern California household exposure study. Environmental Health Perspectives. 2012;120(3):326–331. doi: 10.1289/ehp.1103734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canu IG, Laurent O, Pires N, Laurier D, Dublineau I. Health effects of naturally radioactive water ingestion: The need for enhanced studies. Environmental Health Perspectives. 2011;119(12):1676–1680. doi: 10.1289/ehp.1003224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catelinois O, Rogel A, Laurier D, Billon S, Herman D, Verger P, Tirmarche M. Lung cancer attributed to indoor radon exposure in France: Impact of the risk models and uncertainty analysis. Environmental Health Perspectives. 2006;114(9):1361–1366. doi: 10.1289/ehp.9070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charrios JWA. Private drinking water supplies: Challenges for public health. Canadian Medical Association Journal. 2010;182(10):1061–1064. doi: 10.1503/cmaj.090956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collman GW, Loomis DP, Sandler DP. Childhood cancer mortality and radon concentrations in drinking water in North Carolina. British Journal of Cancer. 1991;63(4):626–629. doi: 10.1038/bjc.1991.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Environmental Health, & Committee on Infectious Diseases Technical report: Drinking water from private wells and risks to children. Pediatrics. 2009;123(6):e1123–e1137. doi: 10.1542/peds.2009-0752. [DOI] [PubMed] [Google Scholar]
- Covello VT. Risk communication: Principles, tools, and techniques. Global Health Technical Briefs. 2008 Retrieved from http://www.popline.org/node/201150.
- Dangleben NL, Skibola CF, Smith MT. Arsenic immunotoxicity: A review. Environmental Health. 2013;12(73):1–15. doi: 10.1186/1476-069X-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs TJ, Ross L, Mucciarone D, Calvache M-C, Taylor O, Goble R. Participatory testing and reporting in an environmental-justice community of Worcester, Massachusetts: A pilot project. Environmental Health. 2010;9(34) doi: 10.1186/1476-069X-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle JK, McClelland GH, Schulze WD, Elliott SR, Russell GW. Protective responses to household risk: A case study of radon mitigation. Risk Analysis. 1991;11(1):121–134. [Google Scholar]
- Doyle JK, McClelland GH, Schulze WD, Locke PA, Elliott SR, Russell GW, Moyad A. Risk Communication and Economic Research Series. U.S. Environmental Protection Agency; Washington, DC: 1990. An evaluation of strategies for promoting effective radon mitigation. [Google Scholar]
- Farzan SF, Karagas MR, Chen Y. In utero and early life arsenic exposure in relation to long-term health and disease. Toxicology and Applied Pharmacology. 2013;272(2):384–390. doi: 10.1016/j.taap.2013.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisbie SH, Mitchell EJ, Sarkar B. World health organization increases its drinking-water guideline for uranium. Environmental Science: Processes & Impacts. 2013;15(10):1817–1823. doi: 10.1039/c3em00381g. [DOI] [PubMed] [Google Scholar]
- Hexemer AM, Pintar K, Bird TM, Zentner SE, Garcia HP, Pollari F. An investigation of bacteriological and chemical water quality and the barriers to private well water sampling in a southwestern Ontario community. Journal of Water and Health. 2008;6(4):521–525. doi: 10.2166/wh.2008.070. [DOI] [PubMed] [Google Scholar]
- Hilborn ED, Wade TJ, Hicks L, Garrison L, Carpenter J, Adam E, Mull B, Yoder JS, Roberts VA, Gargano JW. Surveillance for waterborne disease outbreaks associated with drinking water and other nonrecreational water—United States, 2009–2010. Morbidity and Mortality Weekly Report. 2013;62(35):714–720. [PMC free article] [PubMed] [Google Scholar]
- Hopke PK, Borak TB, Doull J, Cleaver JE, Eckerman KF, Gundersen LCS, Harley NH, Hess CT, Kinner NE, Kopecky KJ, McKone TE, Sextro RG, Simon SL. Health risks due to radon in drinking water. Environmental Science & Technology. 2000;34(6):921–926. [Google Scholar]
- Hughes MF, Beck BD, Chen Y, Lewis AS, Thomas DJ. Arsenic exposure and toxicology: A historical perspective. Toxicological Sciences. 2011;123(2):305–332. doi: 10.1093/toxsci/kfr184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imgrund K, Kreutzwiser R, de Loe R. Influences on the water testing behaviors of private well owners. Journal of Water and Health. 2011;9(2):241–252. doi: 10.2166/wh.2011.139. [DOI] [PubMed] [Google Scholar]
- Jones AQ, Dewey CE, Dore K, Majowicz SE, McEwen SA, David W-T, Eric M, Carr DJ, Henson SJ. Public perceptions of drinking water: A postal survey of residents with private water supplies. BMC Public Health. 2006;6(94):1–11. doi: 10.1186/1471-2458-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AQ, Dewey CE, Dore K, Majowicz SE, McEwen SA, Waltner-Toews D, Henson SJ, Mathews E. Public perception of drinking water from private water supplies: Focus group analyses. BMC Public Health. 2005;5(129) doi: 10.1186/1471-2458-5-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny JF, Barber NL, Hutson SS, Linsey KS, Lovelace JK, Maupin MA. Estimated use of water in the United States in 2005. U.S. Geological Survey; Washington, DC: 2009. [Google Scholar]
- Kreutzwiser R, de Loe R, Imgrund K. Out of sight, out of mind: Private well stewardship in Ontario. Water Policy and Governance Group, University of Waterloo; Waterloo, ON: 2010. [Google Scholar]
- Kreutzwiser R, de Loe R, Imgrund K, Conboy MJ, Simpson H, Plummer R. Understanding stewardship behavior: Factors facilitating and constraining private water well stewardship. Journal of Environmental Management. 2011;92(4):1104–1114. doi: 10.1016/j.jenvman.2010.11.017. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America's adults: Results from the 2003 national assessment of adult literacy. U.S. Department of Education; Washington, DC: 2006. [Google Scholar]
- Levine RL. The need for congressional action to finance arsenic reductions in drinking water. Journal of Environmental Health. 2012;75(4):20–25. [PubMed] [Google Scholar]
- Madajewicz M, Pfaff A, van Green A, Graziano J, Hussein I, Momotaj H, Sylvi R, Ahsan H. Can information alone change behavior? Response to arsenic contamination of groundwater in Bangladesh. Journal of Development Economics. 2007;84(2):731–754. [Google Scholar]
- Martinez VD, Vucic EA, Becker-Santos DD, Gil L, Lam WL. Arsenic exposure and the induction of human cancers. Journal of Toxicology. 2011;2011:1–13. doi: 10.1155/2011/431287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery DL, Ayotte JD, Carroll PR, Hamlin P. Arsenic concentrations in private bedrock wells in southeastern New Hampshire (USGS Fact Sheet 051-03) U.S. Geological Survey; 2003. Retrieved from http://pubs.usgs.gov/fs/fs-051-03/ [Google Scholar]
- National Research Council . Health effects of exposure to radon: Beir VI. National Academies Press; Washington, DC: 1999. [PubMed] [Google Scholar]
- Naujokas MF, Anderson B, Ahsan H, Aposhian HV, Graziano JH, Thompson C, Suk WA. The broad scope of health effects from chronic arsenic exposure: Update on a worldwide public health problem. Environmental Health Perspectives. 2013;121(3):295–302. doi: 10.1289/ehp.1205875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Hampshire Department of Environmental Services Radon in air and water: An overview for the homeowner. 2009 Retrieved from http://des.nh.gov/organization/commissioner/pip/factsheets/dwgb/documents/dwgb-3-12.pdf.
- Novokowski K, Beatty B, Conboy MJ, Lebedin J. Water well sustainability in Ontario. 2006 Retrieved from http://www.greelycommunity.org/documents/Well%20Water%20Sustainability%20Jan%2006.pdf.
- Nuckols JR, Beane Freeman LE, Lubin JH, Airola MS, Baris D, Ayotte JD, Taylor A, Paulu C, Karagas MR, Colt J, Ward MH, Huang A-T, Bress W, Cherala S, Silverman DT, Cantor KP. Estimating water supply arsenic levels in the New England bladder cancer study. Environmental Health Perspectives. 2011;119(9):1279–1285. doi: 10.1289/ehp.1002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Fallon LR, Dearry A. Community-based participa-tory research as a tool to advance environmental health sciences. Environmental Health Perspectives. 2002;110(Suppl. 2):155–159. doi: 10.1289/ehp.02110s2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parvez F, Chen Y, Yunus M, Olopade C, Segers S, Slavkovich V, Argos M, Hasan R, Ahmed A, Islam T, Akter MM, Graziano JH, Ahsan H. Arsenic exposure and impaired lung function. Findings from a large population-based prospective cohort study. American Journal of Respiratory and Critical Care Medicine. 2013;188(7):813–819. doi: 10.1164/rccm.201212-2282OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peerson A, Saunders M. Health literacy revisited: What do we mean and why does it matter? Health Promotion International. 2009;24(3):285–296. doi: 10.1093/heapro/dap014. [DOI] [PubMed] [Google Scholar]
- Postma J, Butterfield PW, Odom-Maryon T, Hill W, Butterfield PG. Rural children's exposure to well water contaminants: Implications in light of the American Academy of Pediatrics’ recent policy statement. Journal of the American Academy of Nurse Practitioners. 2011;23(5):258–265. doi: 10.1111/j.1745-7599.2011.00609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Persson L-A, Barbro N, Arifeen SE, Ekstrom E-C, Smith AH, Vahter M. Arsenic exposure and risk of spontaneous abortion, stillbirth, and infant mortality. Epidemiology. 2010;21(6):797–804. doi: 10.1097/EDE.0b013e3181f56a0d. [DOI] [PubMed] [Google Scholar]
- Ratzan SC, Parker RM. Introduction. In: Seldon CR, Zorn M, Ratzan SC, Parker RM, editors. National library of medicine current bibliographies in medicine: Health literacy. National Institutes of Health, U.S. Department of Health and Human Services; Bethesda, MD: 2000. [Google Scholar]
- Reynolds KA, Mena KD, Gerba CP. Risk of water-borne illness via drinking water in the United States. Reviews of Environmental Contamination and Toxicology. 2008;192:117–158. doi: 10.1007/978-0-387-71724-1_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryker SJ, Small MJ. Combining occurrence and toxicity information to identify priorities for drinking-water mixture research. Risk Analysis. 2008;28(3):653–666. doi: 10.1111/j.1539-6924.2008.00985.x. [DOI] [PubMed] [Google Scholar]
- Safe Drinking Water Act of 1974. U.S. Environmental Protection Agency; 1974. pp. 93–523. § 300F. [Google Scholar]
- Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi: 10.1126/science.3563507. [DOI] [PubMed] [Google Scholar]
- Smith AH, Steinmaus CM. Health effects of arsenic and chromium in drinking water: Recent human findings. Annual Review of Public Health. 2009;30:107–122. doi: 10.1146/annurev.publhealth.031308.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiemann M. Safe drinking water act (SDWA): Selected regulatory and legislative issues. Congressional Research Service; Washington, DC: 2010. [Google Scholar]
- Environmental Protection Agency US. Public drinking water systems: Facts and figures. 2012a Retrieved from http://water.epa.gov/infrastructure/drinkingwater/pws/factoids.cfm.
- Environmental Protection Agency US. Proposed radon drinking water regulation. 2012b Retrieved from http://water.epa.gov/lawsregs/rulesregs/sdwa/radon/regulations.cfm.
- Walker M, Shaw WD, Benson M. Arsenic consumption and health risk perceptions in a rural western U.S. area. Journal of the American Water Resources Association. 2006;42(5):1363–1370. [Google Scholar]
- Ward MH, deKok TM, Levallois P, Brender J, Gulis G, Nolan BT, VanDerslice J. Workgroup report: Drinking-water nitrate and health–recent findings and research needs. Environmental Health Perspectives. 2005;113(11):1607–1614. doi: 10.1289/ehp.8043. [DOI] [PMC free article] [PubMed] [Google Scholar]