Abstract
One of the most important hoof diseases is laminitis. Yet, the pathology of laminitis is not fully understood. Different bacterial toxins, e.g. endotoxins or exotoxins, seem to play an important role. Additionally, ingestion of mycotoxins, toxic secondary metabolites of fungi, might contribute to the onset of laminitis. In this respect, fumonsins are of special interest since horses are regarded as species most susceptible to this group of mycotoxins. The aim of our study was to investigate the influence of fumonisin B1 (FB1) on primary isolated epidermal and dermal hoof cells, as well as on the lamellar tissue integrity and sphingolipid metabolism of hoof explants in vitro. There was no effect of FB1 at any concentration on dermal or epidermal cells. However, FB1 significantly reduced the separation force of explants after 24 h of incubation. The Sa/So ratio was significantly increased in supernatants of explants incubated with FB1 (2.5–10 µg/mL) after 24 h. Observed effects on Sa/So ratio were linked to significantly increased sphinganine concentrations. Our study showed that FB1 impairs the sphingolipid metabolism of explants and reduces lamellar integrity at non-cytotoxic concentrations. FB1 might, therefore, affect hoof health. Further in vitro and in vivo studies are necessary to elucidate the effects of FB1 on the equine hoof in more detail.
Keywords: horses, fumonisin, hoof explants, laminitis, Sa/So ratio
1. Introduction
Hoof related diseases are a common cause of lameness in horses [1]. One of those diseases is laminitis, which causes severe damage of the lamellar tissue and detachment of the pedal bone. The pathology of laminitis is yet not fully understood and bacterial toxins, such as endotoxins [2,3] or exotoxins [4,5], are discussed to play an important role. In addition, ingestion of mycotoxins, toxic secondary metabolites of fungi, might contribute to the onset of laminitis. For example, ergovaline, a mycotoxin produced by endophyte-infected fescues, negatively affects hoof health in vitro [6] and in vivo [7,8] by vasoconstriction. Unfortunately, no information on the effects of other mycotoxins on the equine hoof is available.
In this respect, fumonisins might be of special interest since horses are regarded as a species most susceptible to these mycotoxins. Fumonisins are a group of mycotoxins mainly produced by Fusarium spp., such as F. verticillioides and F. proliferatum. Among different analogues identified so far, fumonisin B1 (FB1) is the most relevant, considering prevalence and toxicity [9]. FB1 is a frequent contaminant of corn, wheat, barley, oats, and hay and can be detected in more than 90% of commercial horse feeds [10]. Hence, horses are at high risk to ingest FB1 and to suffer from its effects. Due to its structural similarity to the sphingoid bases sphinganine (Sa) and sphingosine (So), FB1 inhibits the de novo ceramide synthesis and, thereby, alters the sphingolipid metabolism. As a consequence, FB1 induces a broad range of adverse health effects, including liver and kidney toxicity. In horses, FB1 causes a specific disease called equine leukoencephalomalacia (ELEM) [11], which is characterized by neurological symptoms (e.g., circling, head pressing, ataxia), hepatotoxicity, and leads to irreversible damage of the brain [12,13,14]. Furthermore, an increase of the sphinganine to sphingosine (Sa/So) ratio was observed in serum. As these changes occurred prior to alterations of liver enzymes, the Sa/So ratio might be an early biomarker for FB1 exposure in horses [15,16], indicating impaired ceramide biosynthesis. As ceramides are important parts of the equine hoof tissue, fumonisins might also affect equine hoof health. One report [17] already described a significant difference in total ceramide content of claws of healthy cows and cows with subclinical laminitis.
Still, effects of FB1 on equine hoof health have not been investigated so far. Thus, the aim of our study was to assess the cytotoxic effects of FB1 on primary isolated epidermal and dermal hoof cells. Furthermore, the impact of increasing FB1 concentrations on the lamellar tissue integrity and sphingolipid metabolism was evaluated in vitro. This study will provide first results on the effects of FB1 on primary hoof cells and hoof tissue in vitro and its potential role in hoof related diseases.
2. Results
2.1. Cytotoxicity of FB1 on Primary Hoof Cells
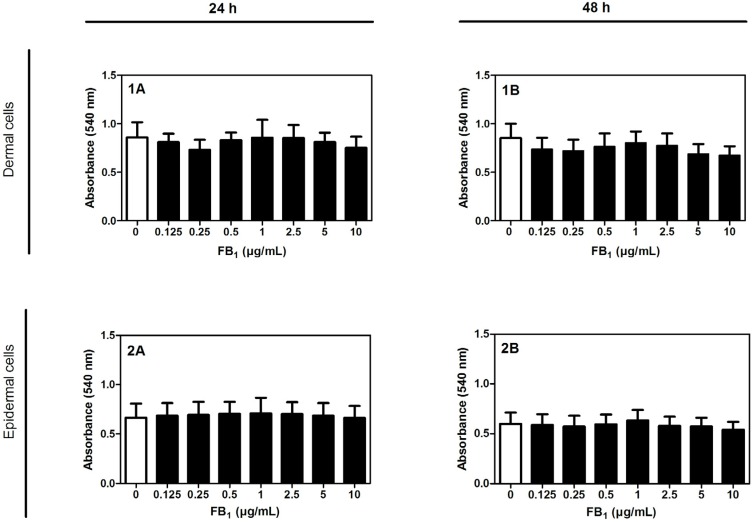
To ensure that used FB1 concentrations (0.125–10 µg/mL) do not have any cytotoxic effects, the neutral red viability assay was performed with primary hoof cells after 24 and 48 h of incubation. FB1 (0.125–10 µg/mL) had no cytotoxic effect on dermal or on epidermal cells after 24 h and 48 h, respectively (Figure 1).
Figure 1.
Absorbance values (540 nm) measured with the neutral red assay to evaluate the viability of dermal hoof cells (1) and epidermal hoof cells (2) incubated with different concentrations of FB1 (0–10 µg/mL) for (A) 24 h and (B) 48 h (n = 4). Error bars present standard deviation.
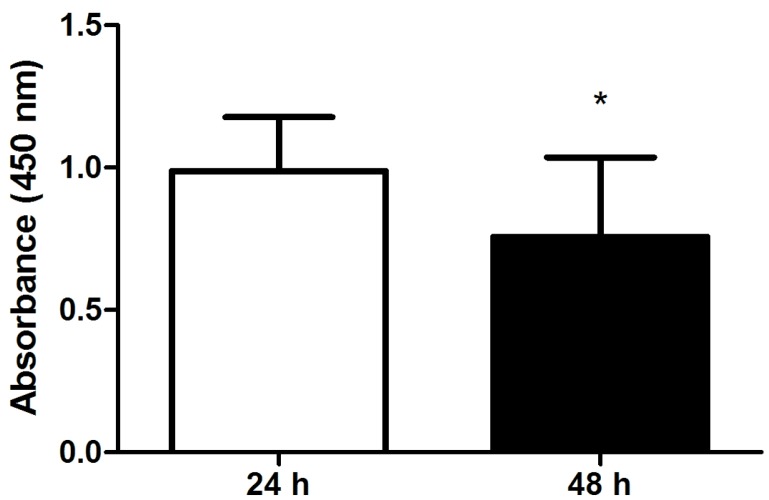
2.2. Viability and Separation Force of Control Hoof Explants
To assess a potential effect of incubation time on investigated parameters, viability (WST-1 assay) and separation force of explants incubated in medium for 24 h (n = 12 explants) or 48 h (n = 9 explants) were compared. Hoof explants incubated for 48 h showed a significantly decreased viability compared to explants incubated for 24 h (Figure 2).
Figure 2.
Absorbance values (450 nm) measured with the WST-1 assay to evaluate the viability of explants incubated with culture medium (control, no FB1 addition) for 24 h (n = 12) and 48 h (n = 9). Error bars present standard deviation. * p < 0.05.
There was no significant decrease of separation force of explants incubated for 48 h compared to explants incubated for 24 h (p = 0.1452).
2.3. Effect of FB1 on Separation Force
The effects of different FB1 concentrations (0–10 µg/mL) on hoof tissue integrity was tested. To this end, a force transducer was used to measure the force needed to separate the explants after incubation with FB1 for 24 h (n = 12 explants) and 48 h (n = 9 explants).
There was a significant influence of incubation time (p = 0.0010) and FB1 (p = 0.006) on separation force. No interaction of both factors was observed (p = 0.905).
Compared to the controls, a significantly decreased separation force was observed in explants incubated with FB1 for 24 h (Table 1). As an exception, incubation with 0.5 µg/mL FB1 did not lead to a reduced separation force.
Table 1.
Mean separation force (Newton (N)) of explants incubated with FB1 (0–10 µg/mL) for 24 h (n = 12).
| 24 h | |||
|---|---|---|---|
| FB1 (µg/mL) | Mean (N) | SD | p-Value |
| 0 | 21.0 | 8.8 | - |
| 0.125 | 13.4 | 7.1 | 0.007 |
| 0.25 | 13.1 | 9.1 | 0.016 |
| 0.5 | 12.6 | 4.1 | 0.084 |
| 1 | 11.5 | 6.1 | 0.000 |
| 2.5 | 12.7 | 5.6 | 0.003 |
| 5 | 12.9 | 6.4 | 0.004 |
| 10 | 14.3 | 7.7 | 0.005 |
After 48 h, only explants incubated with 1 µg/mL FB1 showed a significantly decreased separation force (Table S1). Incubation of explants with 10 µg/mL lipopolysaccharides (LPS; positive control) for 24 h led to a significant decrease of separation force (Figure S1).
2.4. Effects of FB1 Sphingolipid Metabolism
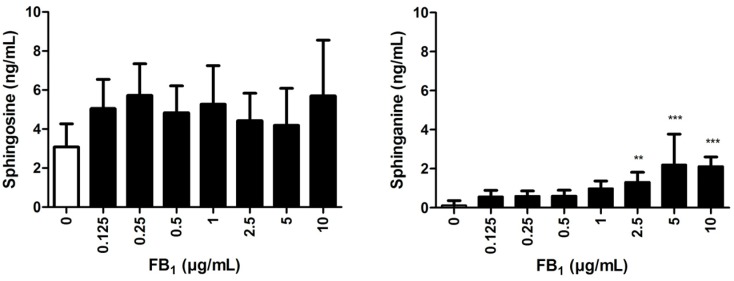
A LC-MS/MS method was used to determine the Sa and So concentrations in explant supernatants (n = 8) incubated for 24 h with FB1 (0–10 µg/mL).
A significant increase of the Sa concentration could be observed in supernatants of explants incubated with 2.5–10 µg/mL FB1 (Figure 3). There was no significant influence of any FB1 concentration on the So concentration.
Figure 3.
Sphingosine and sphinganine supernatant concentration of explants incubated with FB1 (0–10 µg/mL) for 24 h (n = 8). Error bars present standard deviation. ** p < 0.01; *** p < 0.001 compared to explants incubated without FB1.
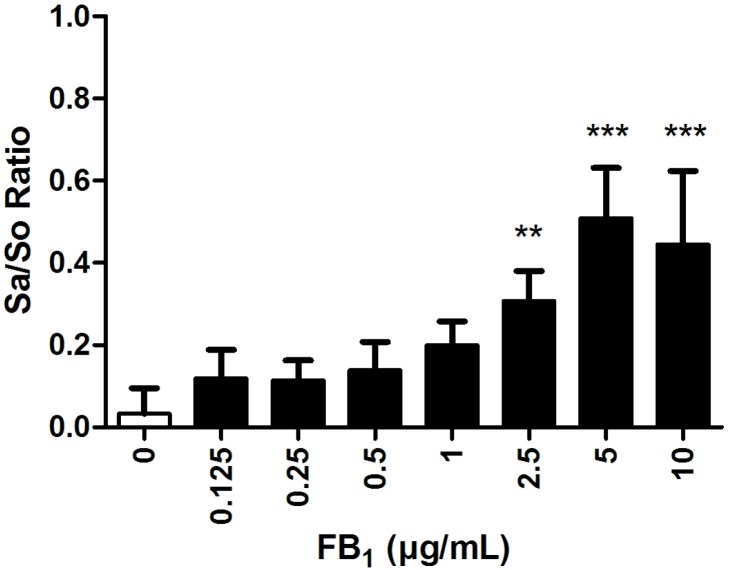
The Sa/So ratio was significantly increased in supernatants of explants incubated with 2.5–10 µg/mL FB1 (Figure 4). A concentration-dependent effect could be observed from 0.5 µg/mL and higher, except for explants incubated with 10 µg/mL.
Figure 4.
Sphinganine to sphingosine (Sa/So) ratio of explants incubated with FB1 (0–10 µg/mL) for 24 h (n = 8). Error bars present standard deviation. ** p < 0.01; *** p < 0.001 compared to explants incubated without FB1.
3. Discussion
The effects of mycotoxins in horses are poorly investigated compared to other species, e.g., pigs, broilers, or cows. Fumonisins have gathered certain interest in equine science due the detrimental effects of FB1 in horses. Still, only some case reports and a few scientific studies on the impact of FB1 on equine health are available. A recent study in 2015 reported an outbreak of fumonisin toxicosis in horses in Serbia [18]. Feed components such as maize and maize bran contained 8400 µg/kg and 7730 µg/kg fumonisins, respectively. Of 21 horses affected, 15 died and showed brain lesions typical for ELEM. There are several other publications, which reported cases of ELEM in horses in Europe, United States, and South Africa [11,19,20]. It has to be mentioned that concentrations of 1000 µg/kg can lead to symptoms of ELEM or death in horses [19]. Mycotoxin surveys demonstrate frequent occurrence of fumonisins in feedstuffs. Streit et al. [21] observed that 53% of feed and feed raw material were positive for fumonisins with a maximum concentration of 77,500 µg/kg. Another study by Liesner et al. [10] found 93% of commercial available horse feed preparations (n = 62) positive for fumonisins with a maximum concentration of 2200 µg/kg. Furthermore, effects of fumonisins might be potentiated by the co-occurrence of other mycotoxins in feed. Intriguingly, individual feed samples were reported to contain up to 69 fungal metabolites [22]. For the majority of these metabolites, no toxicological data in horses are available. In addition, the impact of long-term exposure to subclinical concentrations of FB1 (potentially affecting performance, fertility, or general health status) and the effects of FB1 on the equine hoof are yet unknown.
Hoof diseases are one of the most common reasons for lameness in horses. Laminitis, which is the most frequent hoof disease, affects up to 34% of horses [23]. In the United States alone, the monetary loss per year is estimated to be around $13 million. These losses include evaluation, treatment, and euthanization of horses after a diagnosis of laminitis [24]. One of the greatest challenges in preventing and treating laminitis is the multifactorial etiology. There is still a lack of knowledge about the main trigger factors and pathology of this disease. The study, therefore, focused on the effects of FB1 on hoof health.
First, the cytotoxic potential on dermal and epidermal hoof cells of FB1, the most relevant fumonisin derivative [25], was evaluated. Cells were isolated from hooves as there is no suitable equine cell line commercially available. Our results showed that there is no effect of FB1 concentrations up to 10 µg/mL (~14 µM) on dermal or epidermal cells for 24 and 48 h. Unfortunately, there are no reports available on the cytotoxic potential of FB1 in other equine cell lines. In general, the effects of FB1 seem to be dependent on factors such as concentrations used, cell types/line, and whether FB1 is added to proliferating or confluent cells. For example, FB1 did not evoke cytotoxicity in rat primary hepatocytes (50 µM, [26]), porcine primary endothelial cells (10–50 µM [27]), human fibroblasts (10–100 µM, [28]), or human astrocytes (10–100 µM, [29]). Notably, Kouadio et al. [30] determined no cytotoxic effects of FB1 in human intestinal cells with the neutral red assay, at concentrations up to 150 µM FB1, but measured an effect with the MTT assay at 21 µM FB1. These differences might be related to the assays focusing on different cell targets, thereby highlighting the relevance of the employed test system. As we could not observe an effect of FB1 on the viability of hoof cells with the neutral red assay as well, it will be interesting to investigate the cytotoxicity with assays focusing different cell targets. In addition, FB1 might induce apoptosis in hoof cells, which cannot be measured with the applied assay. Dietary exposure of rats to high FB1 concentrations (99–448,000 µg/kg) induced apoptosis in the kidney and liver of rats [31]. Furthermore, FB1 induced apoptosis in human neonatal keratinocytes and fibroblasts, in combination with decreased cell viability [32,33]. Hence, it will be important to assess the effect of FB1 on the number of apoptotic hoof cells.
As a next step, the influence of FB1 on the separation force of hoof explants was tested. The explant model offers the advantage to test a lot of different concentrations at once. However, one limitation of explant models is the limited lifespan of hoof tissue in vitro. Often, viability is not assessed in studies using explants, although this is rather important to ensure that decreased viability has no effect on obtained results. Our data showed that viability of explant was significantly decreased after 48 h, which confirms previous findings of our group [34]. Hence, we can conclude that explants should only be cultivated for 24 h as the lifespan of explants in vitro seems to be limited. Decreased viability will potentially affect other parameters as separation force and, therefore, experiments with extended incubation time should be evaluated with care.
When adding FB1 for 24 h to the explants, we measured a significant decrease of the separation force. LPS was used as positive control to validate the hoof explant model. Other studies have already shown that LPS is able to reduce separation force of explants [34,35]. As expected, also in our study incubation with 10 µg/mL LPS led to a significant reduction of separation force. At the moment, we cannot conclude on the definite cause that led to the FB1-mediated lamellar separation. There are only studies available showing a decrease in the separation force when explants were incubated with exotoxins [4,5] or endotoxins [34,35]. Exotoxins led to an increased matrix metalloproteinase (MMP) −2 and −9 activity, which leads to the separation of explants [4,36]. However, other MMPs in the lamellar tissue such as MMP-13 might also play an important role [37]. Beside possible activation of different enzymes like MMPs, FB1 might initiate inflammation processes, which cause destruction of the lamellar tissue. A study by Mammodi et al. [38], for example, showed that FB1 can induce inflammatory cytokine response in a gastric epithelial and a colon adenocarcinoma cell line.
In addition to lamellar tissue integrity, we evaluated the influence of FB1 on sphingolipid metabolism in explants. The Sa/So ratio was determined in supernatants of explants incubated with FB1 for 24 h only, due to the decreased viability of the control explants after 48 h incubation. We measured a significantly increased Sa/So ratio in supernatants of explants treated with FB1 (0.5–10 µg/mL). This effect was also concentration dependent except for explants treated with 10 µg/mL FB1 after 24 h. The observed effects on the Sa/So ratio in our study were linked to an increase of sphinganine concentration in explant supernatants. In many species, the Sa/So ratio has been described as sensitive biomarker for FB1 exposure [39,40]. FB1 is known to inhibit ceramide synthase, which, as a consequence, leads to intracellular accumulation of Sa, and also (to a minor extent) So. Accordingly, an increase of the serum Sa/So ratio was observed in horses exposed to 15,000–44,000 µg/kg FB1. This parameter might already be increased before clinical signs or alterations in serum levels of liver enzymes can be detected [15].
In our study, the disruption of the ceramide synthesis could be an explanation for the decreased lamellar tissue integrity we observed after FB1 exposure. Ceramides are important parts of the equine hoof tissue and can be found, e.g., in the intracellular spaces of keratinocytes [41]. The keratinized layer of the hoof tissue has an important role as effective barrier against environmental impacts and prevents water loss. There are no studies available which evaluated the effects of ceramide concentration on the pathology of hoof related diseases in horses. However, a study by Higuche et al. [17] described a significant correlation between ceramide concentration and hardness of the claws in healthy cows and cows with subclinical laminitis. Furthermore, a significant decrease in the hardness of the claw of cows with subclinical laminitis could also be observed. As keratinocytes synthesize ceramides, the decrease during subclinical laminitis might be caused by changes of the keratinocyte function due to inflammatory processes.
In general, in vitro systems are often less sensitive compared to in vivo studies as they present an isolated system (highly-controlled conditions) in the absence of other trigger factors. This is of special importance when it comes to the multifactorial etiology of laminitis.
FB1 concentrations used in our study were similar or even lower (0.17–13.85 µM) compared to those applied in other in vitro studies (5–100 µM). Even in in vivo studies, comparably high FB1 concentrations (exceeding the recommendation level for horses of 5,000 µg FB1/kg feed) are regularly used. Although such experiments might not always represent the conditions in the field they are, nevertheless, crucial to understand the mode of action of FB1.
It is difficult to compare the FB1 concentrations used in our study to the situation in vivo, as there are only a few publications available about recovery from the blood or from specific tissue. For example, Fodor et al. [42] detected 17.4 µg/kg FB1 accumulated in the liver, when piglets were fed with 45,000 µg/kg FB1 for 10 days. Administration of 10,000 µg/kg FB1 per os in rats led to plasma concentrations of 0.180 µg/mL [43]. In vervet monkeys, also concentrations of up to 0.210 µg/mL FB1 in the plasma could be measured after gavage of 6420 µg/kg body weight FB1 [44]. A single administration of 5000 µg/kg FB1 per os in weaning piglets led to plasma concentrations of 0.300 µg/mL after 2 h [45]. About half of this concentration (0.125 µg/mL) FB1 already significantly decreased separation force in our study and an eight times higher concentration led to a significant increase of the Sa/So ratio.
FB1 induced disruption of the ceramide metabolism might, therefore, cause structural changes in the explants, subsequently leading to a decreased separation force. However, the mechanism which induces lamellar destruction by FB1 has to be further investigated.
4. Conclusions
Our study indicates that FB1 has no cytotoxic effect on equine epidermal and dermal cells but impairs the sphingolipid metabolism of explants and reduces lamellar integrity. FB1 is probably not capable of inducing laminitis itself but it might have an effect on the development or on the severity of laminitis. Although further in vitro and in vivo studies are necessary to elucidate the effects of FB1 on the equine hoof in more detail, the potential impact of fumonisins on equine health was, once again, highlighted.
5. Materials and Methods
5.1. Preparation of FB1 Stock Solution
Solid FB1 standard was purchased from Romer Labs (Tulln, Austria). The stock solution, containing 1168 µg/mL FB1, was prepared in distilled water, sterile filtrated (0.2 µm filter), and stored at 4 °C. FB1 stock solution was diluted with culture medium to yield a concentration of 0.125–10 µg/mL FB1 in the wells. Negative influence of solvent on explants was excluded.
5.2. Ethical Statement
Equine hooves were obtained from a local abattoir. No horse was killed for the purpose of tissue collection.
5.3. Animals
Forelimbs from five adult horses were obtained at a local abattoir. There was no information of age, gender, breed, or history of the horses available. Horses were killed by use of a penetrating captive bolt and subsequent exsanguination. Only forelimbs with healthy hooves were processed. The condition of hooves was assessed by macroscopic examination by a veterinarian and microscopic evaluation of lamella tissue. Isolated forelimbs were transported on ice to the laboratory. Transportation time to the laboratory did not exceed 120 min.
5.4. Preparation of Hoof Explants
Hooves were prepared and dissected as described in the literature by Reisinger et al. [34]. Immediately after preparation, explants were either used for isolation of primary hoof cells (cytotoxicity assays) or for direct incubation with different FB1 concentrations (lamellar separation tests).
5.5. Isolation, Cultivation, and Cytotoxicity Tests of Dermal and Epidermal Cells
Isolation of dermal and epidermal cells was performed as described by Reisinger et al. [35].
Cells were passaged and grown in T-75 flasks (Star Lab, Hamburg, Germany). Dermal cells were used until passage 18, while epidermal cells were only used until passage 10. Cells were seeded in 96 well plates (Eppendorf, Vienna, Austria) with a density of 4 × 104 cells and 200 µL medium per well. After two days, cells were incubated with FB1 (0–10 µg/mL) in triplicate for 24 and 48 h. Four independent experiments were performed for each incubation time and cell type, respectively.
The neutral red assay was performed according to the instructions of the manufacturer (Aniara, Columbus, OH, USA) to determine the cytotoxicity of increasing FB1 concentrations on epidermal and dermal cells. This viability assay is based on the ability of viable cells to incorporate and bind neutral red within lysosomes.
5.6. Cultivation, Viability, and Lamellar Separation (Force Transducer) of Hoof Explants
Explants were cultured with 1 mL medium at 37 °C and 5% CO2 in 24 well plates (IWAKI, Willich, Germany). D-MEM (4.5 g/L glucose; Life technologies, Vienna, Austria) supplemented with 100 U/mL nystatin (Life technologies) and 0.1 mg/L gentamicin (Life technologies) was used as the culture medium. Explants were cultured with different FB1 concentrations (0–10 µg/mL) for 24 h (quadruplicate per horse) or 48 h (triplicate per horse). As positive control, explants were incubated with 10 µg/mL lipopolysaccharides from Escherichia coli O55:B5 (Sigma, Vienna, Austria) [34] for 24 h (quadruplicate per horse). Thereafter, all explants were examined via microscope before proceeding with testing. Explants showing bacterial or fungal contamination were excluded from the results.
Explants were tested for their viability with the water soluble tetrazolium (WST-1) as described by Reisinger et al. [34]. A comparison between control explants (0 µg/mL FB1) for 24 (n = 12) and 48 h (n = 9) was performed. The force required for explant separation was measured by a calibrated force transducer as described by Reisinger et al. [34].
5.7. Sphinganine (Sa) and Sphingosine (So) Analysis via LC-MS/MS
Supernatants of explants incubated with FB1 (0–10 µg/mL) for 24 h were collected under sterile conditions in reaction tubes (Eppendorf). Tubes were stored at −20 °C until further processing. Supernatants were thawed; proteins were precipitated by addition of the four-fold volume of methanol (Sigma), and removed by centrifugation at 20,000× g for 10 min at room temperature. Thereafter, supernatants were evaporated to dryness in a SpeedVac (Genevac, Ipswich, UK) and reconstituted in 80% (v/w) methanol to the original sample volume.
Sa and So were analyzed via LC–MS/MS as described by Grenier et al. [46] with some modifications. A Kinetex C18 column (2.6 µm, 100 Å 150 × 2.1 mm; Phenomenex, Torrance, CA, USA) was used for chromatographic separation on an Agilent 1290 series UHPLC system (Agilent, Waldbronn, Germany), with a flow rate of 0.25 mL/min and a linear gradient from 35% B to 100% B (eluent A: methanol/water/formic acid, 40/59.85/0.15 v/v/v; eluent B: methanol/formic acid 99.85/0.15). The injection volume was set to 2 µL. Tandem mass spectrometric detection was carried out on a 5500 Triple Quad system (AB Sciex, Framingham, MA, USA) after electrospray ionization in positive mode, using the following source parameters: curtain gas 40, collision gas 7, ion spray voltage 5500 V, source temperature 550 °C , GS1 50, GS2 50. The declustering potentials (DP), quantifier (quant) and qualifier (qual) transitions were DP 71 V, quant: m/z 300.3 to 282.3 (CE 15 eV), qual: m/z 300.3 to 252.2 (CE 23 eV) for So and DP 146 V, quant: m/z 302.3 to 284.3 (CE 19 eV), qual: m/z 302.3 to 60.1 (CE 21 eV) for Sa. Dwell time for all transitions was 50 ms. Analyst software version 1.6.2 (AB Sciex, 2013) was used for instrument control and data evaluation. Sa and So standards for external standard calibration functions were purchased form Avanti Polar Lipids, Inc. (Alabaster, AL, USA). The overall recovery was 90% ± 8% for Sa and 87% ± 8% for So, while the limit of quantitation was 0.3 µg/L for both analytes.
5.8. Statistical Analyses
Statistical evaluation was performed with IBM SPSS Statistics software (Version 19.0, IBM corp., New York, NY, USA, 2010). If data were normally distributed (Kolmogorov-Smirnov test), either t-test (unpaired, two-tailed) or ANOVA was performed with Dunnett’s test as a post hoc test. If data were not normally distributed, the Kruskal-Wallis test was used as a non-parametric test. Results were considered significant at p < 0.05.
Acknowledgments
The authors would like to thank the Austrian Research Promotion Agency (FFG) for funding this study. Furthermore, the authors like to thank Caroline Emsenhuber, Nora Schauerhuber, and Thomas Tymciw for performing the cytotoxicity tests and Petra Mayrhofer for Sa/So sample preparation.
Abbreviations
The following abbreviations are used in this manuscript:
| ELEM | Equine Leukoencephalomalacia |
| FB1 | Fumonisin B1 |
| LPS | Lipopolysaccharides |
| Sa | Sphinganine |
| So | Sphingosine |
| Sa/So ratio | Sphinganine-to-sphingosine ratio |
| WST | Water Soluble Tetrazolium |
Supplementary Materials
The following are available online at www.mdpi.com/2072-6651/8/4/89/s1, Table S1: Mean separation force (N) of explants incubated with FB1 (0–10 µg/mL) for 48 h (n = 9), Figure S1: Comparison of the separation force of explants treated with 10 µg/mL LPS (positive control) to control explants (negative control).
Author Contributions
Conceived and designed the experiments: N.R., I.D., V.N., S.S., G.S., E.M. Performed the experiments: N.R. Analyzed the data: N.R. Contributed reagents/materials/analysis tools: N.R., I.D. Wrote the paper: N.R., I.D., V.N., S.S., G.S., E.M.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.USDA . Lameness and laminitis in us horses. USDA Rural Development; Denver, CO, USA: 2000. [Google Scholar]
- 2.Bailey S.R., Adair H.S., Reinemeyer C.R., Morgan S.J., Brooks A.C., Longhofer S.L., Elliott J. Plasma concentrations of endotoxin and platelet activation in the developmental stage of oligofructose-induced laminitis. Vet. Immunol. Immunopathol. 2009;129:167–173. doi: 10.1016/j.vetimm.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Katz L.M., Bailey S.R. A review of recent advances and current hypotheses on the pathogenesis of acute laminitis. Equine Vet. J. 2012;44:752–761. doi: 10.1111/j.2042-3306.2012.00664.x. [DOI] [PubMed] [Google Scholar]
- 4.Mungall B.A., Pollitt C.C. Thermolysin activates equine lamellar hoof matrix metalloproteinases. J. Comp. Pathol. 2002;126:9–16. doi: 10.1053/jcpa.2001.0515. [DOI] [PubMed] [Google Scholar]
- 5.Mungall B.A., Kyaw-Tanner M., Pollitt C.C. In vitro evidence for a bacterial pathogenesis of equine laminitis. Vet. Microbiol. 2001;79:209–223. doi: 10.1016/S0378-1135(00)00359-X. [DOI] [PubMed] [Google Scholar]
- 6.Klotz J.L., McDowell K.J. Tall fescue alkaloids cause vasoconstriction in equine medial palmar artery and vein. Anim. Sci. 2010;88:55. [Google Scholar]
- 7.McDowell K.J., Moore E.S., Parks A.G., Bush L.P., Horohov D.W., Lawrence L.M. Vasoconstriction in horses caused by endophyte-infected tall fescue seed is detected with doppler ultrasonography. J. Anim. Sci. 2013;91:1677–1684. doi: 10.2527/jas.2012-5852. [DOI] [PubMed] [Google Scholar]
- 8.Douthit T.L., Bormann J.M., Gradert K.C., Lomas L.W., DeWitt S.F., Kouba J.M. The impact of endophyte-infected fescue consumption on digital circulation and lameness in the distal thoracic limb of the horse. J. Anim. Sci. 2012;90:3101–3111. doi: 10.2527/jas.2011-4371. [DOI] [PubMed] [Google Scholar]
- 9.Voss K.A., Riley R.T. Fumonisin toxicity and mechanism of action: Overview and current perspectives. Food Saf. 2013;1:49–69. doi: 10.14252/foodsafetyfscj.2013006. [DOI] [Google Scholar]
- 10.Liesener K., Curtui V., Dietrich R., Martlbauer E., Usleber E. Mycotoxins in horse feed. Mycotoxin Res. 2010;26:23–30. doi: 10.1007/s12550-009-0037-8. [DOI] [PubMed] [Google Scholar]
- 11.Marasas W.F., Kellerman T.S., Gelderblom W.C., Coetzer J.A., Thiel P.G., van der Lugt J.J. Leukoencephalomalacia in a horse induced by fumonisin B1 isolated from Fusarium moniliforme. Onderstepoort J. Vet. Res. 1988;55:197–203. [PubMed] [Google Scholar]
- 12.Brownie C.F., Cullen J. Characterization of experimentally induced equine leukoencephalomalacia (ELEM) in ponies (Equus caballus): Preliminary report. Vet. Hum. Toxicol. 1987;29:34–38. [PubMed] [Google Scholar]
- 13.Foreman J.H., Constable P.D., Waggoner A.L., Levy M., Eppley R.M., Smith G.W., Tumbleson M.E., Haschek W.M. Neurologic abnormalities and cerebrospinal fluid changes in horses administered fumonisin B1 intravenously. J. Vet. Intern. Med. 2004;18:223–230. doi: 10.1892/0891-6640(2004)18<223:NAACFC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Ross P.F., Ledet A.E., Owens D.L., Rice L.G., Nelson H.A., Osweiler G.D., Wilson T.M. Experimental equine leukoencephalomalacia, toxic hepatosis, and encephalopathy caused by corn naturally contaminated with fumonisins. J. Vet. Diagn. Investig. 1993;5:69–74. doi: 10.1177/104063879300500115. [DOI] [PubMed] [Google Scholar]
- 15.Wang E., Ross P.F., Wilson T.M., Riley R.T., Merrill A.H., Jr. Increases in serum sphingosine and sphinganine and decreases in complex sphingolipids in ponies given feed containing fumonisins, mycotoxins produced by Fusarium moniliforme. J. Nutr. 1992;122:1706–1716. doi: 10.1093/jn/122.8.1706. [DOI] [PubMed] [Google Scholar]
- 16.Smith G.W., Constable P.D., Foreman J.H., Eppley R.M., Waggoner A.L., Tumbleson M.E., Haschek W.M. Cardiovascular changes associated with intravenous administration of fumonisin B1 in horses. Am. J. Vet. Res. 2002;63:538–545. doi: 10.2460/ajvr.2002.63.538. [DOI] [PubMed] [Google Scholar]
- 17.Higuchi H., Nakamura M., Kuwano A., Kasamatsu M., Nagahata H. Quantities and types of ceramides and their relationships to physical properties of the horn covering the claws of clinically normal cows and cows with subclinical laminitis. Can. J. Vet. Res. 2005;69:155–158. [PMC free article] [PubMed] [Google Scholar]
- 18.Jovanović M., Trailović D., Kukolj V., Nešić S., Marinković D., Nedeljković-Trailović J., Jakovac B., Milićević D. An outbreak of fumonisin toxicosis in horses in Serbia. World Mycotoxin J. 2015;8:1–6. doi: 10.3920/WMJ2014.1812. [DOI] [Google Scholar]
- 19.Ross P.F., Rice L.G., Reagor J.C., Osweiler G.D., Wilson T.M., Nelson H.A., Owens D.L., Plattner R.D., Harlin K.A., Richard J.L., et al. Fumonisin B1 concentrations in feeds from 45 confirmed equine leukoencephalomalacia cases. J. Vet. Diagn. Investig. 1991;3:238–241. doi: 10.1177/104063879100300310. [DOI] [PubMed] [Google Scholar]
- 20.Cerrillo G.N., Rodriguez F.S., Gordo L.G., de Mendoza Salcedo M.H., Cordero V.R. Clinical and pathological aspects of an outbreak of equine leukoencephalomalacia in spain. J. Veterinary Med. Ser. A. 1996;43:467–472. doi: 10.1111/j.1439-0442.1996.tb00476.x. [DOI] [PubMed] [Google Scholar]
- 21.Streit E., Naehrer K., Rodrigues I., Schatzmayr G. Mycotoxin occurrence in feed and feed raw materials worldwide: Long-term analysis with special focus on Europe and Asia. J. Sci. Food Agric. 2013;93:2892–2899. doi: 10.1002/jsfa.6225. [DOI] [PubMed] [Google Scholar]
- 22.Streit E., Schwab C., Sulyok M., Naehrer K., Krska R., Schatzmayr G. Multi-mycotoxin screening reveals the occurrence of 139 different secondary metabolites in feed and feed ingredients. Toxins. 2013;5:504–523. doi: 10.3390/toxins5030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wylie C.E., Collins S.N., Verheyen K.L., Richard Newton J. Frequency of equine laminitis: A systematic review with quality appraisal of published evidence. Vet. J. 2011;189:248–256. doi: 10.1016/j.tvjl.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 24.Moore R.M. Conquer laminitis by 2020. J. Equine Vet. Sci. 2010;30:74–76. doi: 10.1016/j.jevs.2010.01.044. [DOI] [Google Scholar]
- 25.Voss K.A., Riley R.T., Moore N.D., Burns T.D. Alkaline cooking (nixtamalisation) and the reduction in the in vivo toxicity of fumonisin-contaminated corn in a rat feeding bioassay. Food Addit. Contam. Part A. 2013;30:1415–1421. doi: 10.1080/19440049.2012.712064. [DOI] [PubMed] [Google Scholar]
- 26.Ribeiro D.H., Ferreira F.L., da Silva V.N., Aquino S., Correa B. Effects of aflatoxin B1 and fumonisin B1 on the viability and induction of apoptosis in rat primary hepatocytes. Int. J. Mol. Sci. 2010;11:1944–1955. doi: 10.3390/ijms11041944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramasamy S., Wang E., Hennig B., Merrill A.H., Jr. Fumonisin B1 alters sphingolipid metabolism and disrupts the barrier function of endothelial cells in culture. Toxicol. Appl. Pharmacol. 1995;133:343–348. doi: 10.1006/taap.1995.1159. [DOI] [PubMed] [Google Scholar]
- 28.Galvano F., Russo A., Cardile V., Galvano G., Vanella A., Renis M. DNA damage in human fibroblasts exposed to fumonisin B1. Food Chem. Toxicol. 2002;40:25–31. doi: 10.1016/S0278-6915(01)00083-7. [DOI] [PubMed] [Google Scholar]
- 29.Galvano F., Campisi A., Russo A., Galvano G., Palumbo M., Renis M., Barcellona M.L., Perez-Polo J.R., Vanella A. DNA damage in astrocytes exposed to fumonisin B1. Neurochem. Res. 2002;27:345–351. doi: 10.1023/A:1014971515377. [DOI] [PubMed] [Google Scholar]
- 30.Kouadio J.H., Mobio T.A., Baudrimont I., Moukha S., Dano S.D., Creppy E.E. Comparative study of cytotoxicity and oxidative stress induced by deoxynivalenol, zearalenone or fumonisin B1 in human intestinal cell line Caco-2. Toxicology. 2005;213:56–65. doi: 10.1016/j.tox.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 31.Tolleson W.H., Dooley K.L., Sheldon W.G., Thurman J.D., Bucci T.J., Howard P.C. The mycotoxin fumonisin induces apoptosis in cultured human cells and in livers and Kidneys of rats. Adv. Exp. Med. Biol. 1996;392:237–250. doi: 10.1007/978-1-4899-1379-1_21. [DOI] [PubMed] [Google Scholar]
- 32.Tolleson W.H., Melchior W.B., Jr., Morris S.M., McGarrity L.J., Domon O.E., Muskhelishvili L., James S.J., Howard P.C. Apoptotic and anti-proliferative effects of fumonisin B1 in human keratinocytes, fibroblasts, esophageal epithelial cells and hepatoma cells. Carcinogenesis. 1996;17:239–249. doi: 10.1093/carcin/17.2.239. [DOI] [PubMed] [Google Scholar]
- 33.Tolleson W.H., Couch L.H., Melchior W.B., Jr., Jenkins G.R., Muskhelishvili M., Muskhelishvili L., McGarrity L.J., Domon O., Morris S.M., Howard P.C. Fumonisin B1 induces apoptosis in cultured human keratinocytes through sphinganine accumulation and ceramide depletion. Int. J. Oncol. 1999;14:833–843. doi: 10.3892/ijo.14.5.833. [DOI] [PubMed] [Google Scholar]
- 34.Reisinger N., Schaumberger S., Nagl V., Hessenberger S., Schatzmayr G. Milk thistle extract and silymarin inhibit lipopolysaccharide induced lamellar separation of hoof explants in vitro. Toxins. 2014;6:2962–2974. doi: 10.3390/toxins6102962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reisinger N., Schaumberger S., Nagl V., Hessenberger S., Schatzmayr G. Concentration dependent influence of lipopolysaccharides on separation of hoof explants and supernatant lactic acid concentration in an ex vivo/in vitro laminitis model. PLoS One. 2015;10 doi: 10.1371/journal.pone.0143754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pollitt C.C., Pass M.A., Pollitt S. Batimastat (BB-94) inhibits matrix metalloproteinases of equine laminitis. Equine Vet. J. Suppl. 1998;30 doi: 10.1111/j.2042-3306.1998.tb05130.x. [DOI] [PubMed] [Google Scholar]
- 37.Wang L., Pawlak E.A., Johnson P.J., Belknap J.K., Alfandari D., Black S.J. Expression and activity of collagenases in the digital laminae of horses with carbohydrate overload-induced acute laminitis. J. Vet. Intern. Med. 2014;28:215–222. doi: 10.1111/jvim.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahmoodi M., Alizadeh A.M., Sohanaki H., Rezaei N., Amini-Najafi F., Khosravi A.R., Hosseini S.K., Safari Z., Hydarnasab D., Khori V. Impact of fumonisin B1 on the production of inflammatory cytokines by gastric and colon cell lines. Iran. J. Allergy Asthma Immunol. 2012;11:165–173. [PubMed] [Google Scholar]
- 39.Riley R.T., An N.H., Showker J.L., Yoo H.S., Norred W.P., Chamberlain W.J., Wang E., Merrill A.H., Jr., Motelin G., Beasley V.R., et al. Alteration of tissue and serum sphinganine to sphingosine ratio: An early biomarker of exposure to fumonisin-containing feeds in pigs. Toxicol. Appl. Pharmacol. 1993;118:105–112. doi: 10.1006/taap.1993.1015. [DOI] [PubMed] [Google Scholar]
- 40.Hahn I., Nagl V., Schwartz-Zimmermann H.E., Varga E., Schwarz C., Slavik V., Reisinger N., Malachova A., Cirlini M., Generotti S., et al. Effects of orally administered fumonisin B1 (FB1), partially hydrolysed FB1, hydrolysed FB1 and N-(1-deoxy-d-fructos-1-yl) FB1 on the sphingolipid metabolism in rats. Food Chem. Toxicol. 2015;76:11–18. doi: 10.1016/j.fct.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 41.Golden G.M., Guzek D.B., Kennedy A.H., McKie J.E., Potts R.O. Stratum corneum lipid phase transitions and water barrier properties. Biochemistry. 1987;26:2382–2388. doi: 10.1021/bi00382a045. [DOI] [PubMed] [Google Scholar]
- 42.Fodor J., Balogh K., Weber M., Miklos M., Kametler L., Posa R., Mamet R., Bauer J., Horn P., Kovacs F., et al. Absorption, distribution and elimination of fumonisin B1 metabolites in weaned piglets. Food Addit. Contam. A Chem. Anal. Control Expo. Risk Assess. 2008;25:88–96. doi: 10.1080/02652030701546180. [DOI] [PubMed] [Google Scholar]
- 43.Martinez-Larranaga M.R., Anadon A., Diaz M.J., Fernandez-Cruz M.L., Martinez M.A., Frejo M.T., Martinez M., Fernandez R., Anton R.M., Morales M.E., et al. Toxicokinetics and oral bioavailability of fumonisin B1. Vet. Hum. Toxicol. 1999;41:357–362. [PubMed] [Google Scholar]
- 44.Shephard G.S., Thiel P.G., Sydenham E.W., Savard M.E. Fate of a single dose of 14C-labelled fumonisin B1 in vervet monkeys. Nat. Toxins. 1995;3:145–150. doi: 10.1002/nt.2620030305. [DOI] [PubMed] [Google Scholar]
- 45.Dilkin P., Direito G., Simas M.M., Mallmann C.A., Correa B. Toxicokinetics and toxicological effects of single oral dose of fumonisin B1 containing fusarium verticillioides culture material in weaned piglets. Chem. Biol. Interact. 2010;185:157–162. doi: 10.1016/j.cbi.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 46.Grenier B., Schwartz-Zimmermann H.E., Caha S., Moll W.D., Schatzmayr G., Applegate T.J. Dose-dependent effects on sphingoid bases and cytokines in chickens fed diets prepared with fusarium verticillioides culture material containing fumonisins. Toxins. 2015;7:1253–1272. doi: 10.3390/toxins7041253. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.