Abstract
Previous studies have found higher levels of serum malondialdehyde (MDA) in hepatocellular carcinoma (HCC) patients compared to healthy controls and higher MDA concentrations in tumoral tissue of HCC patients than in non-tumoral tissue. However, the association between pre-transplant serum levels of MDA and survival in HCC patients after liver transplantation (LT) has not been described, and the aim of the present study was to determine whether such an association exists. In this observational study we measured serum MDA levels in 127 patients before LT. We found higher pre-LT serum MDA levels in 15 non-surviving than in 112 surviving patients one year after LT (p = 0.02). Exact binary logistic regression analysis revealed that pre-LT serum levels of MDA over 3.37 nmol/mL were associated with mortality after one year of LT (Odds ratio = 5.38; 95% confidence interval (CI) = from 1.580 to infinite; p = 0.007) adjusting for age of the deceased donor. The main finding of our study was that there is an association between serum MDA levels before LT for HCC and 1-year survival after LT.
Keywords: MDA, hepatocellular carcinoma, liver transplantation, mortality, outcome
1. Introduction
Hepatocellular carcinoma (HCC) is the most frequent primary malignancy in the liver, one of the most frequent malignancies and the second most frequent cause of cancer-related death in the world. Globally, there are approximately 600,000 new diagnoses of HCC each year and 750,000 deaths due to HCC. Liver transplantation (LT) is generally considered the treatment of choice for selected HCC patients since the primary tumor is removed and liver failure is treated [1,2,3,4,5,6,7,8,9,10].
Oxidative state has been suggested to play a role in the progression of chronic liver disease and in hepatocarcinogenesis. In addition, different antioxidant drugs have been shown to modulate oxidative stress and prevent the appearance of HCC [11,12,13,14].
Oxidative stress leads to peroxidation of membrane lipids, and this process generates a variety of end products, including malondialdehyde (MDA). MDA is a low-molecular weight aldehyde produced by the attack of free radicals to polyunsaturated fatty acids during cellular membrane phospholipid degradation. It is released into extracellular space and finally reaches the bloodstream. Thus, MDA has been used as a lipid oxidation biomarker [15,16].
Previous studies have reported higher serum levels of MDA in HCC patients than in healthy controls [17,18,19], and higher MDA concentrations in tumoral tissue of HCC patients than in non-tumoral tissue [20]. However, the association between pre-transplant serum levels of MDA and survival of HCC patients after liver transplantation (LT) has not been previously reported, and the objective of the present research was to study whether such an association exists.
2. Results
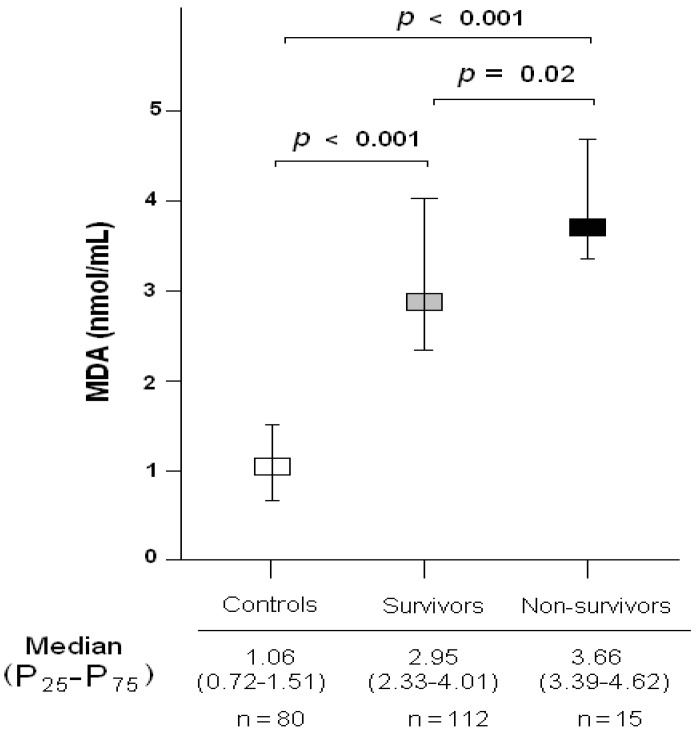
We found higher serum levels of MDA in both surviving and non-surviving patients at 1 year after LT for HCC than in healthy controls (p < 0.001, Figure 1). There were no significant differences in age or gender between patients and controls (Table 1).
Figure 1.
Serum malondialdehyde (MDA) levels in healthy controls, and in 1-year survivors and non-survivors undergoing liver transplantation for hepatocellular carcinoma. P25–P75 are percentile 25 and 75.
Table 1.
Demographic characteristics of healthy controls and patients with hepatocellular carcinoma (HCC) undergoing liver transplantation.
| Demographic Characteristics | Healthy Controls (n = 80) | HCC Patients (n = 127) | p-Value |
|---|---|---|---|
| Female gender—n (%) | 18 (22.5) | 20 (15.7) | 0.27 |
| Age—median years (P25–P75) | 56 (46–68) | 58 (52–62) | 0.71 |
| Serum malondialdehyde levels (nmol/mL)—median (P25–P75) | 1.06 (0.72–1.51) | 3.11 (2.39–4.17) | <0.001 |
Table 2 shows demographic and clinical variables of non-surviving (n = 15) and surviving patients (n = 112) at 1 year after LT. We found no differences between non-survivors and survivors regarding sex, age of LT recipients, ABO blood type, Child-Pugh score, model for end-stage liver disease (MELD) score, Milan criteria, serum alpha-fetoprotein (AFP) levels, portal hypertension, number of nodules, size of nodules, tumor differentiation, infiltration, microvascular invasion, macrovascular invasion, pre-LT treatment or LT technique. However, non-survivors at 1 year after LT had received organs from older deceased donors (p = 0.02) and showed higher serum levels of MDA (p = 0.02) compared to survivors.
Table 2.
Demographic and clinical characteristics of 1-year survivors and non-survivors undergoing liver transplantation for hepatocellular carcinoma.
| Demographic and Clinical Characteristics | Survivors at 1 Year (n = 112) | Non-Survivors at 1 Year (n = 15) | p-Value |
|---|---|---|---|
| Female gender—n (%) | 20 (17.9) | 0 | 0.13 |
| Age (years)—median (P25–P75) | 58 (52–62) | 56 (53–62) | 0.84 |
| Age of liver donor (years)—median (P25–P75) | 52 (36–63) | 62 (49–72) | 0.02 |
| ABO blood type—n (%) | |||
| A | 53 (47.3) | 6 (40.0) | 0.87 |
| B | 9 (8.0) | 2 (13.3) | |
| O | 45 (40.2) | 6 (40.0) | |
| AB | 5 (4.5) | 1 (6.7) | |
| Child-Pugh score—n (%) | |||
| A | 54 (48.2) | 10 (66.7) | 0.41 |
| B | 35 (31.3) | 3 (20.0) | |
| C | 23 (20.5) | 2 (13.3) | |
| MELD score—median (P25–P75) | 15 (11–18) | 15 (15–18) | 0.44 |
| Inside Milan criteria previously to LT—n (%) | 107 (95.5) | 14 (93.3) | 0.54 |
| Inside Milan criteria after LT—n (%) | 94 (83.9) | 11 (73.3) | 0.16 |
| Serum AFP (ng/dL)—median (P25–P75) | 8.0 (4.0–32.0) | 12.0 (4.8–164.9) | 0.42 |
| Portal hypertension—n (%) | 78 (69.6) | 11 (73.3) | 0.99 |
| Multinodular tumor—n (%) | 34 (30.4) | 5 (33.3) | 0.77 |
| Nodule size (cm)—median (P25–P75) | 3.0 (2.0–3.5) | 3.2 (1.7–4.6) | 0.83 |
| Degree of tumor differentiation—n (%) | |||
| Well | 84 (75.0) | 12 (80.0) | 0.55 |
| Moderate | 25 (22.3) | 2 (13.3) | |
| Poor | 3 (2.7) | 1 (6.7) | |
| Infiltration—n (%) | 36 (32.1) | 4 (26.7) | 0.77 |
| Microvascular invasion—n (%) | 24 (21.4) | 3 (20.0) | 0.99 |
| Macrovascular invasion—n (%) | 6 (5.4) | 0 | 0.99 |
| Treatment prior to LT—n (%) | 61 (54.1) | 10 (66.7) | 0.42 |
| Transplantation technique—n (%) | |||
| By-pass | 43 (38.4) | 6 (40.0) | 0.99 |
| Piggy back | 69 (61.6) | 9 (60.0) | |
| Serum MDA (nmol/mL)—median (P25–P75) | 2.95 (2.33–4.01) | 3.66 (3.39–4.62) | 0.02 |
MELD = model for end-stage liver disease; AFP = alpha-fetoprotein; MDA = malondialdehyde.
On exact binary logistic regression analysis, serum levels of MDA above 3.37 nmol/mL were associated with mortality after one year of LT (Odds Ratio = 5.38; 95% CI = from 1.580 to infinite; p = 0.007) adjusting for deceased donor age (Table 3).
Table 3.
Exact binary logistic regression analysis to predict mortality at 1 year after liver transplantation for hepatocellular carcinoma.
| Predictors | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Serum MDA levels > 3.37 nmol/mL | 5.38 | 1.580–infinite | 0.007 |
| Age of liver donor (age) | 1.04 | 1.003–infinite | 0.04 |
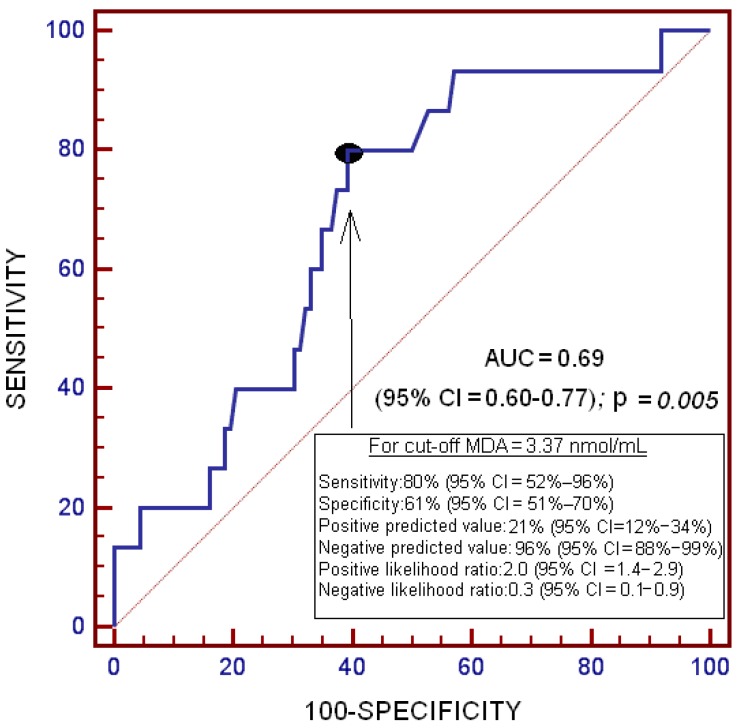
On receiver operator characteristic (ROC) analysis, the area under the curve (AUC) for serum levels of MDA to predict death at 1 year after LT was 0.69 (95% CI = 0.601–0.769; p = 0.005) (Figure 2).
Figure 2.
Receiver operator characteristic analysis using serum MDA levels as a predictor of death at 1 year after liver transplantation for hepatocellular carcinoma.
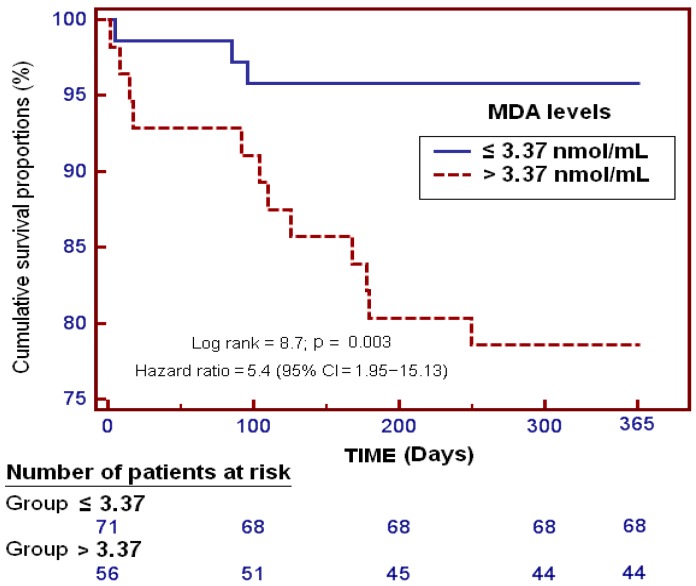
Kaplan–Meier survival curves showed that patients with serum levels of MDA above 3.37 nmol/mL had a higher probability of death at 1 year after LT (log-rank = 8.7; Odds Ratio = 5.4 (95% CI = 1.95–15.13); p = 0.003) than patients with lower serum levels of MDA (Figure 3).
Figure 3.
Survival curves at 1 year in patients undergoing liver transplantation for hepatocellular carcinoma using serum MDA levels higher or lower than 3.37 nmol/mL.
3. Discussion
The most relevant finding of the present study was an association between pre-LT serum levels of MDA and 1-year survival after LT. Pre-transplant serum levels of MDA were higher in non-surviving compared to surviving patients.
We observed higher pre-LT transplant serum levels of MDA in HCC patients than in healthy controls, which is consistent with the findings of previous investigators showing higher serum MDA levels in HCC patients than in healthy controls [17,18,19], in patients with chronic liver disease than in healthy controls [21,22], and the fact that HCC patients present higher free radical intensity in erythrocytes than healthy controls [23]. In addition, higher MDA concentrations have been found in the tumoral tissue of HCC patients than in non-tumoral tissue [20].
One-year survival after LT for HCC patients varies between 79% and 93% [24,25,26,27]; the survival rate in our study (88.2%) fell within this range.
HCC patients with higher serum concentrations of derivatives of reactive oxygen metabolites (d-ROM) present more disease recurrence after curative treatment by radiofrequency ablation or surgical resection [28]. In addition, in patients before LT, non-survivors showed higher circulating lipid peroxide levels than survivors [29]. To our knowledge, the present study is the first to report lower pre-transplant serum MDA levels in survivors than non-survivors at 1 year after LT. In addition, it is the first to report an association between serum MDA levels before LT and 1-year post-transplant survival. These findings are consistent with the results of previous studies that have reported an association between circulating MDA levels and mortality in patients with brain trauma injury [30], brain infarction [31], and sepsis [32,33].
Taken together, our findings indicate that alteration of the oxidative state may be of great pathophysiological significance in HCC patients undergoing LT. Higher circulating levels of MDA in HCC patients than in healthy controls, and in 1-year non-survivors than in surviving patients, represents higher lipid peroxidation due to overproduction of reactive oxygen species (ROS) and reactive nitrogen species (RNS) caused by the imbalance between pro-oxidant and antioxidant systems.
Various factors have been linked with worse outcome in HCC patients undergoing LT, such as tumor size, tumor number, degree of differentiation, hepatic microvascular invasion, hepatic macrovascular invasion, serum alpha-fetoprotein (AFP) levels, outside Milan criteria and infiltration [7,34,35]. In the present study, however, we only found differences in liver donor age, which was lower in surviving patients compared to non-survivors at 1 year after LT.
The development of oxidant state modulators could be a new class of treatment for patients with HCC undergoing LT. The use of different antioxidant agents reduces MDA levels in animal models of sepsis [36,37,38,39] and of trauma brain injury [40,41,42], and also in clinical trials with asphyxiated newborn infants [43], septic newborns [44], adult burn patients [45], acute ischemic stroke patients [46,47,48], and trauma brain injury [49]. In addition, the administration of different antioxidant agents reduces mortality in clinical trials with adult burn patients [45], and trauma brain injury [49]. The potential role of oxidative state in hepatocarcinogenesis, and the use of drugs with antioxidant effects to prevent the development of HCC in patients with chronic liver disease have been suggested [11,12,13,14]. In addition, since non-surviving patients at 1 year showed higher pre-transplant serum MDA levels than surviving patients, the use of drugs with antioxidant effects could be a new treatment to improve the prognosis of those patients, especially those with higher oxidative state.
Our present study has some limitations. First, it was a single-center study and the results may not be extrapolated to patients treated at other institutions. Second, the determination of other compounds of antioxidant and oxidant states could be desirable to better evaluate this balance. Third, other potentially confounding factors not related to sickness (e.g., diet) could have affected MDA serum levels. Fourth, the association that we found between elevated serum MDA levels and reduced survival does not necessarily imply causality, and we have not analyzed the impact of drug modulators of oxidant state; thus, antioxidant drugs may not impact the prognosis.
4. Materials and Methods
4.1. Design
We performed a retrospective, observational, single-center study with prospective data collection from 127 HCC patients undergoing orthotopic LT from brain death donors in the period between January 1996 to August 2014 at the Hospital Universitario Nuestra Señora de Candelaria (Santa Cruz de Tenerife, Spain). The Institutional Review Board of the Hospital Universitario Nuestra Señora de Candelaria approved the study (permission code PI-33/15; persmission date 30 July 2015). Written informed consent was provided by patients or their family members.
4.2. Variables Recorded
The variables recorded for each patient were as follows: sex, age of LT recipient, age of LT donor, AB0 blood type, Child-Pugh score [50], model for end-stage liver disease (MELD) score [51] by hepatic function, Milan criteria [52] before and after LT, serum alpha-fetoprotein (AFP) levels, portal hypertension (assessed clinically or by hepatic venous pressure gradient), number of nodules, size of nodules, tumor differentiation, infiltration, microvascular invasion, macrovascular invasion, pre-LT treatment, LT technique, and serum MDA concentrations.
4.3. End-Point
The end-point was survival at 1 year after LT.
4.4. Blood Samples and Serum Malondialdehyde Level Analysis
Serum blood samples were collected from 127 patients with HCC before LT (approximately 2 h previous to LT) and from 80 healthy controls. We used the thiobarbituric acid-reactive substance (TBARS) method to determine serum levels of MDA levels, such as was described by Kikugawa et al. [53]. The pink complex of samples was extracted in n-butanol. The samples were deposited in 96-well plates and read at 535 nm using a microplate spectrophotometer reader (Benchmark Plus, Bio-Rad, Hercules, CA, USA). Serum concentrations of MDA were expressed in nmol/mL, and the assay detection limit was 0.079 nmol/mL. The coefficient of intra-assay variation was 1.82% and the coefficient of inter-assay variation was 4.01%. All determinations were carried out in the Physiology Department of the Medicine Faculty of La Laguna University (Santa Cruz de Tenerife, Spain) by laboratory technicians blinded to clinical data.
4.5. Statistical Methods
Continuous variables are described as medians and interquartile ranges, and categorical variables as frequencies and percentages. We used Mann–Whitney U test for comparisons of continuous variables between surviving and non-surviving patients at 1 year after LT, and chi-square test for the comparisons of categorical variables between groups. We plotted a receiver operator characteristic (ROC) curve using serum levels of MDA as the prognostic variable and survival at 1 year after LT as the classification variable. Youden J index was used to select the cut-off prognostic value of serum MDA level. Youden J Index is defined as maximum (sensitivity c + specificity c −1), where c ranges over all possible criterion values [54]. Graphically, Youden J Index is the maximum vertical distance between the ROC curve and the diagonal line. Moreover, using the positive likelihood ratio (sensitivity/(1 − specificity)), the serum MDA level cut-off value is the same (3.37 nmol/mL). Survival analysis was carried out using Kaplan-Meier curves, and comparisons were performed by log-rank test using serum MDA levels lower/higher than 3.37 nmol/mL as the independent variable and survival at 1 year after LT as the dependent variable. Exact binary logistic regression analysis was carried out to determine the independent contribution of serum levels of MDA to predict death at 1 year after LT, controlling for deceased donor age. Since the number of events (death) was low (n = 15), the regression analysis only included two predictor variables, and those variables proving significant on bivariate analysis. We calculated odds ratio (OR) and 95% confidence intervals (CI) to measure the clinical impact of the predictor variables. Differences with a p value < 0.05 were considered to be statistically significant. All statistical analyses were carried out with SPSS 17.0 (SPSS Inc., Chicago, IL, USA) and MedCal 15.2.1 (Ostend, Belgium).
5. Conclusions
The major finding of our study was an association between serum levels of MDA before LT for HCC and 1-year survival after LT. Serum levels of MDA before LT were higher in non-surviving compared to surviving patients.
Abbreviations
| AFP | alpha-fetoprotein |
| AUC | area under curve |
| d-ROM | derivatives of reactive oxygen metabolites |
| HCC | hepatocellular carcinoma |
| LT | liver transplantation |
| MDA | malondialdehyde |
| ROC | receiver operator characteristic |
| ROS | reactive oxygen species |
| RNS | reactive nitrogen species |
| TBARS | thiobarbituric acid-reactive substance |
Author Contributions
Leonardo Lorente was responsible for the conception, design and coordination of the study; made substantial contributions to data acquisition, analysis and interpretation, and drafted the manuscript. Sergio T. Rodriguez, Pablo Sanz, Dácil Díaz, Antonia M. Moreno, Elisa Borja, María M. Martín, and Manuel A. Barrera made substantial contributions to data acquisition and provided useful suggestions. Pedro Abreu-González carried out the determination of serum MDA levels, and made substantial contributions to analysis and interpretation of data. Alejandro Jiménez made substantial contributions to analysis and interpretation of data. All authors have read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Bodzin A.S., Busuttil R.W. Hepatocellular carcinoma: Advances in diagnosis, management, and long term outcome. World J. Hepatol. 2015;7:1157–1167. doi: 10.4254/wjh.v7.i9.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guerrero-Misas M., Rodríguez-Perálvarez M., de la Mata M. Strategies to improve outcome of patients with hepatocellular carcinoma receiving a liver transplantation. World J. Hepatol. 2015;7:649–661. doi: 10.4254/wjh.v7.i4.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slotta J.E., Kollmar O., Ellenrieder V., Ghadimi B.M., Homayounfar K. Hepatocellular carcinoma: Surgeon’s view on latest findings and future perspectives. World J. Hepatol. 2015;7:1168–1183. doi: 10.4254/wjh.v7.i9.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomaa A.I., Waked I. Recent advances in multidisciplinary management of hepatocellular carcinoma. World J. Hepatol. 2015;7:673–687. doi: 10.4254/wjh.v7.i4.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark T., Maximin S., Meier J., Pokharel S., Bhargava P. Hepatocellular carcinoma: Review of epidemiology, screening, imaging diagnosis, response assessment, and treatment. Curr. Probl. Diagn. Radiol. 2015;44:479–486. doi: 10.1067/j.cpradiol.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Toyoda H., Kumada T., Tada T., Sone Y., Kaneok Y., Maeda A. Tumor markers for hepatocellular carcinoma: Simple and significant predictors of outcome in patients with HCC. Liver Cancer. 2015;4:126–136. doi: 10.1159/000367735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cescon M., Bertuzzo V.R., Ercolani G., Ravaioli M., Odaldi F., Pinna A.D. Liver transplantation for hepatocellular carcinoma: Role of inflammatory and immunological state on recurrence and prognosis. World J. Gastroenterol. 2013;19:9174–9182. doi: 10.3748/wjg.v19.i48.9174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Association for the Study of the Liver. European Organisation for Research and Treatment of Cancer EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Clavien P.A., Lesurtel M., Bossuyt P.M., Gores G.J., Langer B., Perrier A., OLT for HCC Consensus Group Recommendations for liver transplantation for hepatocellular carcinoma: An international consensus conference report. Lancet Oncol. 2012;13:e11–e22. doi: 10.1016/S1470-2045(11)70175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verslype C., Rosmorduc O., Rougier P., ESMO Guidelines Working Group Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012;23:vii41–vii48. doi: 10.1093/annonc/mds225. [DOI] [PubMed] [Google Scholar]
- 11.Takaki A., Yamamoto K. Control of oxidative stress in hepatocellular carcinoma: Helpful or harmful? World J. Hepatol. 2015;7:968–979. doi: 10.4254/wjh.v7.i7.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi J., Corder N.L., Koduru B., Wang Y. Oxidative stress and hepatic Nox proteins in chronic hepatitis C and hepatocellular carcinoma. Free Radic. Biol. Med. 2014;72:267–284. doi: 10.1016/j.freeradbiomed.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marra M., Sordelli I.M., Lombardi A., Lamberti M., Tarantino L., Giudice A., Stiuso P., Abbruzzese A., Sperlongano R., Accardo M., et al. Molecular targets and oxidative stress biomarkers in hepatocellular carcinoma: An overview. J. Transl. Med. 2011;9:171. doi: 10.1186/1479-5876-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoshida Y. Molecular signatures and prognosis of hepatocellular carcinoma. Minerva Gastroenterol. Dietol. 2011;57:311–322. [PubMed] [Google Scholar]
- 15.Draper H.H., Hadley M. Malondialdehyde determination as index of lipid peroxidation. Methods Enzymol. 1990;186:421–431. doi: 10.1016/0076-6879(90)86135-i. [DOI] [PubMed] [Google Scholar]
- 16.Dalle-Donne I., Rossi R., Colombo R., Giustarini D., Milzani A. Biomarkers of oxidative damage in human disease. Clin. Chem. 2006;52:601–623. doi: 10.1373/clinchem.2005.061408. [DOI] [PubMed] [Google Scholar]
- 17.Yahya R.S., Ghanem O.H., Foyouh A.A., Atwa M., Enany S.A. Role of interleukin-8 and oxidative stress in patients with hepatocellular carcinoma. Clin. Lab. 2013;59:969–976. doi: 10.7754/clin.lab.2012.120712. [DOI] [PubMed] [Google Scholar]
- 18.Zhao J., Zhao Y., Wang H., Gu X., Ji J., Gao C. Association between metabolic abnormalities and HBV related hepatocelluar carcinoma in Chinese: A cross-sectional study. Nutr. J. 2011;10 doi: 10.1186/1475-2891-10-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai S.M., Lin S.K., Lee K.T., Hsiao J.K., Huang J.C., Wu S.H., Ma H., Wu S.H., Tsai L.Y. Evaluation of redox statuses in patients with hepatitis B virus-associated hepatocellular carcinoma. Ann. Clin. Biochem. 2009;46:394–400. doi: 10.1258/acb.2009.009029. [DOI] [PubMed] [Google Scholar]
- 20.Czeczot H., Scibior D., Skrzycki M., Podsiad M. Glutathione and GSH-dependent enzymes in patients with liver cirrhosis and hepatocellular carcinoma. Acta Biochim. Pol. 2006;53:237–242. [PubMed] [Google Scholar]
- 21.Trevisani F., Caraceni P., Simoncini M., Micati M., Domenicali M., Dazzani F., Zambruni A., Stefanelli C., Grazi G., Nardo B., et al. Evidence of oxidative imbalance in long-term liver transplant patients. Dig. Liver Dis. 2002;34:279–284. doi: 10.1016/S1590-8658(02)80148-7. [DOI] [PubMed] [Google Scholar]
- 22.Thorat V.N., Suryakar A.N., Naik P., Tiwale B.M. Total antioxidant capacity and lipid peroxidation in liver transplantation. Indian J. Clin. Biochem. 2009;24:102–104. doi: 10.1007/s12291-009-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Váli L., Hahn O., Kupcsulik P., Drahos A., Sárváry E., Szentmihályi K., Pallai Z., Kurucz T., Sípos P., Blázovics A. Oxidative stress with altered element content and decreased ATP level of erythrocytes in hepatocellular carcinoma and colorectal liver metastases. Eur. J. Gastroenterol. Hepatol. 2008;20:393–398. doi: 10.1097/MEG.0b013e3282f495c7. [DOI] [PubMed] [Google Scholar]
- 24.Teng F., Wang G.H., Tao Y.F., Guo W.Y., Wang Z.X., Ding G.S., Shi X.M., Fu Z.R. Criteria-specific long-term survival prediction model for hepatocellular carcinoma patients after liver transplantation. World J. Gastroenterol. 2014;20:10900–10907. doi: 10.3748/wjg.v20.i31.10900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dumitra S., Salleh I., Alabbad S.I., Barkun J.S., Dumitra T.C., Coutsinos D., Metrakos P.P., Hassanain M., Paraskevas S., Chaudhury P., et al. Hepatitis C infection and hepatocellular carcinoma in liver transplantation: A 20-year experience. HPB. 2013;15:724–731. doi: 10.1111/hpb.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martínez Ares D., Suárez López F.J., Souto Ruzo J., Otero Ferreiro A., Gómez Gutiérrez M., González Conde B., Fernández Sellés C., Gala López B., Arnal Monreal F., Vázquez Iglesias J.L. Liver transplantation in patients with hepatocellular carcinoma: Factors implicated in tumor relapse. Rev. Esp. Enferm. Dig. 2004;96:22–31. doi: 10.4321/S1130-01082004000100004. [DOI] [PubMed] [Google Scholar]
- 27.Ninomiya M., Shirabe K., Facciuto M.E., Schwartz M.E., Florman S.S., Yoshizumi T., Harimoto N., Ikegami T., Uchiyama H., Maehara Y. Comparative study of living and deceased donor liver transplantation as a treatment for hepatocellular carcinoma. J. Am. Coll. Surg. 2015;220:297–304. doi: 10.1016/j.jamcollsurg.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 28.Suzuki Y., Imai K., Takai K., Hanai T., Hayashi H., Naiki T., Nishigaki Y., Tomita E., Shimizu M., Moriwaki H. Hepatocellular carcinoma patients with increased oxidative stress levels are prone to recurrence after curative treatment: A prospective case series study using the d-ROM test. J. Cancer Res. Clin. Oncol. 2013;139:845–852. doi: 10.1007/s00432-013-1389-1. [DOI] [PubMed] [Google Scholar]
- 29.Liu C., Zhou X.S., Geng Q.M. Evaluation oxygen free radicals related index before liver transplantation to forejudge prognosis. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2003;15:560–562. [PubMed] [Google Scholar]
- 30.Lorente L., Martín M.M., Abreu-González P., Ramos L., Argueso M., Cáceres J.J., Solé-Violán J., Lorenzo J.M., Molina I., Jiménez A. Association between serum malondialdehyde levels and mortality in patients with severe brain trauma injury. J. Neurotrauma. 2015;32:1–6. doi: 10.1089/neu.2014.3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lorente L., Martín M.M., Abreu-González P., Ramos L., Argueso M., Solé-Violán J., Riaño-Ruiz M., Jiménez A. Serum malondialdehyde levels in patients with malignant middle cerebral artery infarction are associated with mortality. PLoS ONE. 2015;10:500. doi: 10.1371/journal.pone.0125893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lorente L., Martín M.M., Abreu-González P., Domínguez-Rodríguez A., Labarta L., Díaz C., Solé-Violán J., Ferreres J., Borreguero-León J.M., Jiménez A., et al. Prognostic value of malondialdehyde serum levels in severe sepsis: A multicenter study. PLoS ONE. 2013;8:500. doi: 10.1371/journal.pone.0053741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorente L., Martín M.M., Abreu-González P., Domínguez-Rodriguez A., Labarta L., Díaz C., Solé-Violán J., Ferreres J., Cabrera J., Igeño J.C., et al. Sustained high serum malondialdehyde levels are associated with severity and mortality in septic patients. Crit. Care. 2013;17 doi: 10.1186/cc13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Varona M.A., Del Pino J.M., Barrera M., Arranz J., Hernández B.M., Perez H.F., Padilla J., Fuentes J.S., Aguirre A., Mendez S., et al. Hepatocellular carcinoma and liver transplantation: A 12-year experience. Transpl. Proc. 2009;41:1005–1008. doi: 10.1016/j.transproceed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 35.Varona M.A., Soriano A., Aguirre-Jaime A., Garrido S., Oton E., Diaz D., Portero J., Bravo P., Barrera M.A., Perera A. Risk factors of hepatocellular carcinoma recurrence after liver transplantation: Accuracy of the α-fetoprotein model in a single-center experience. Transpl. Proc. 2015;47:84–89. doi: 10.1016/j.transproceed.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 36.Sener G., Toklu H., Kapucu C., Ercan F., Erkanli G., Kaçmaz A., Tilki M., Yeğen B.C. Melatonin protects against oxidative organ injury in a rat model of sepsis. Surg. Today. 2005;35:52–59. doi: 10.1007/s00595-004-2879-1. [DOI] [PubMed] [Google Scholar]
- 37.Carrillo-Vico A., Lardone P.J., Naji L., Fernández-Santos J.M., Martín-Lacave I., Guerrero J.M., Calvo J.R. Beneficial pleiotropic actions of melatonin in an experimental model of septic shock in mice: Regulation of pro-/anti-inflammatory cytokine network, protection against oxidative damage and anti-apoptotic effects. J. Pineal Res. 2005;39:400–408. doi: 10.1111/j.1600-079X.2005.00265.x. [DOI] [PubMed] [Google Scholar]
- 38.Lowes D.A., Webster N.R., Murphy M.P., Galley H.F. Antioxidants that protect mitochondria reduce interleukin-6 and oxidative stress, improve mitochondrial function, and reduce biochemical markers of organ dysfunction in a rat model of acute sepsis. Br. J. Anaesth. 2013;110:472–480. doi: 10.1093/bja/aes577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paskaloğlu K., Sener G., Kapucu C., Ayanoğlu-Dülger G. Melatonin treatment protects against sepsis-induced functional and biochemical changes in rat ileum and urinary bladder. Life Sci. 2004;74:1093–1104. doi: 10.1016/j.lfs.2003.07.038. [DOI] [PubMed] [Google Scholar]
- 40.Kerman M., Cirak B., Ozguner M.F., Dagtekin A., Sutcu R., Altuntas I., Delibas N. Does melatonin protect or treat brain damage from traumatic oxidative stress? Exp. Brain Res. 2005;163:406–410. doi: 10.1007/s00221-005-2338-2. [DOI] [PubMed] [Google Scholar]
- 41.Horakova L., Onrejickova O., Barchrrata K., Vajdova M. Preventive effect of several antioxidants after oxidative stress on rat brain homogenates. Gen. Physiol. Biophys. 2000;19:195–205. [PubMed] [Google Scholar]
- 42.Ozsüer H., Görgülü A., Kiriş T., Cobanoğlu S. The effects of memantine on lipid peroxidation following closed-head trauma in rats. Neurosurg. Rev. 2005;28:143–147. doi: 10.1007/s10143-004-0374-1. [DOI] [PubMed] [Google Scholar]
- 43.Fulia F., Gitto E., Cuzzocrea S., Reiter R.J., Dugo L., Gitto P., Barberi S., Cordaro S., Barberi I. Increased levels of malondialdehyde and nitrite/nitrate in the blood of asphyxiated newborns: Reduction by melatonin. J. Pineal Res. 2001;31:343–349. doi: 10.1034/j.1600-079X.2001.310409.x. [DOI] [PubMed] [Google Scholar]
- 44.Gitto E., Karbownik M., Reiter R.J., Tan D.X., Cuzzocrea S., Chiurazzi P., Cordaro S., Corona G., Trimarchi G., Barberi I. Effects of melatonin treatment in septic newborns. Pediatr. Res. 2001;50:756–760. doi: 10.1203/00006450-200112000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Sahib A.S., Al-Jawad F.H., Alkaisy A.A. Effect of antioxidants on the incidence of wound infection in burn patients. Ann. Burns Fire Dis. 2010;23:199–205. [PMC free article] [PubMed] [Google Scholar]
- 46.Ullegaddi R., Powers H.J., Gariballa S.E. B-group vitamin supplementation mitigates oxidative damage after acute ischaemic stroke. Clin. Sci. 2004;107:477–484. doi: 10.1042/CS20040134. [DOI] [PubMed] [Google Scholar]
- 47.Ullegaddi R., Powers H.J., Gariballa S.E. Antioxidant supplementation enhances antioxidant capacity and mitigates oxidative damage following acute ischaemic stroke. Eur. J. Clin. Nutr. 2005;59:1367–1373. doi: 10.1038/sj.ejcn.1602248. [DOI] [PubMed] [Google Scholar]
- 48.Ullegaddi R., Powers H.J., Gariballa S.E. Antioxidant supplementation with or without B-group vitamins after acute ischemic stroke: A randomized controlled trial. J. Parent. Enter. Nutr. 2006;30:108–114. doi: 10.1177/0148607106030002108. [DOI] [PubMed] [Google Scholar]
- 49.Saniova B., Drobny M., Lehotsky J., Sulaj M., Schudichova J. Biochemical and clinical improvement of cytotoxic state by amantadine sulphate. Cell. Mol. Neurobiol. 2006;26:1475–1482. doi: 10.1007/s10571-006-9033-0. [DOI] [PubMed] [Google Scholar]
- 50.Pugh R.N., Murray-Lyon I.M., Dawson J.L., Pietroni M.C., Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 51.Kamath P.S., Wiesner R.H., Malinchoc M., Kremers W., Therneau T.M., Kosberg C.L., D’Amico G., Dickson E.R., Kim W.R. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 52.Mazzaferro V., Regalia E., Doci R., Andreola S., Pulvirenti A., Bozzetti F., Montalto F., Ammatuna M., Morabito A., Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 1996;334:693–699. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 53.Kikugawa K., Kojima T., Yamaki S., Kosugi H. Interpretation of the thiobarbituric acid reactivity of rat liver and brain homogenates in the presence of ferric ion and ethylediaminotetraacetic acid. Anal. Biochem. 1992;202:249–255. doi: 10.1016/0003-2697(92)90102-D. [DOI] [PubMed] [Google Scholar]
- 54.Youden W.J. An index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]