Abstract
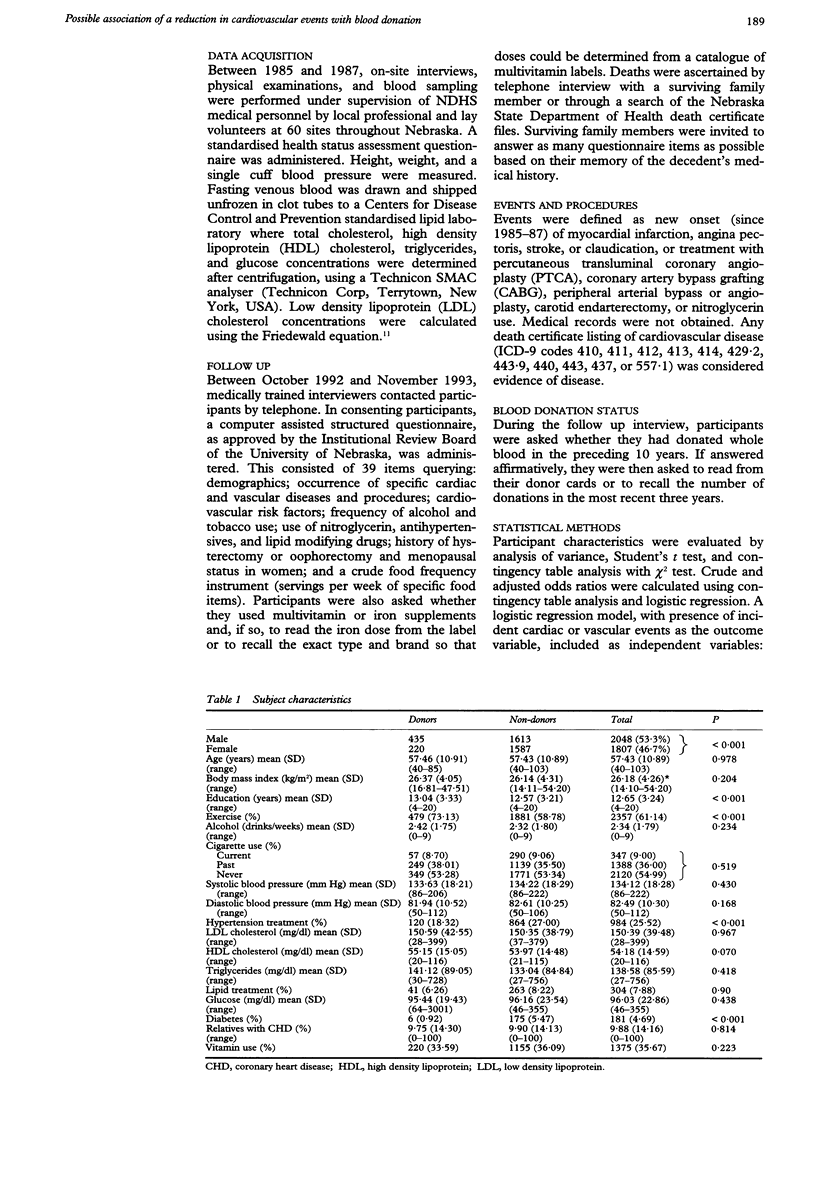
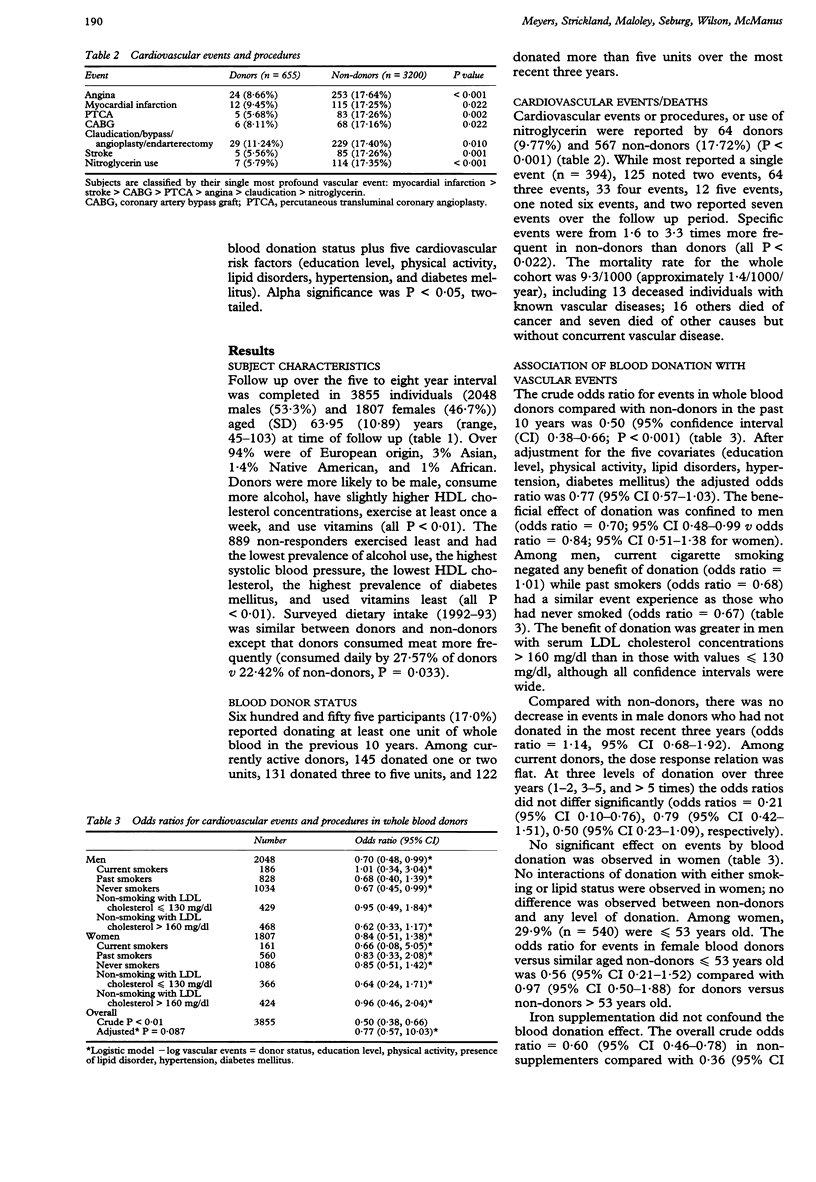
BACKGROUND: The iron hypothesis suggests that females are protected from atherosclerosis by having lower iron stores than men, thus limiting oxidation of lipids. OBJECTIVE: To test the iron hypothesis by comparing cardiovascular event rates in whole blood donors compared with nondonors. DESIGN: Prospective cohort with telephone survey follow up. SETTING: The State of Nebraska, USA. PARTICIPANTS: A sample was selected from the Nebraska Diet Heart Survey (NDHS) restricting for age > or = 40 years and absence of clinically apparent vascular diseases at time of enrollment in to NDHS (1985-87). MAIN OUTCOME MEASURES: The occurrence of cardiovascular events (myocardial infarction, angina, stroke), procedures (angioplasty, bypass surgery, claudication, endarterectomy), nitroglycerin use, or death (all cause mortality), and level of blood donation. RESULTS: Participants were 655 blood donors and 3200 non-donors who differed in education, physical activity, diabetes, and frequency of antihypertensive treatment; 889 were lost to follow up. Sixty four donors and 567 non-donors reported cardiovascular events (crude odds ratio = 0.50, 95% confidence interval (CI) 0.38-0.66). The benefit of donation was confined to non-smoking males (adjusted odds ratio 0.67, 95% CI 0.45-0.99). Benefit was limited to current donors (the most recent three years). No additional benefit resulted from donating more than once or twice over three years. CONCLUSION: In support of the iron hypothesis, blood donation in non-smoking men in this cohort was associated with reduced risk of cardiovascular events. A randomised clinical trial is warranted to confirm these findings as the observed personal health benefit of donation has public policy ramifications.
Full text
PDF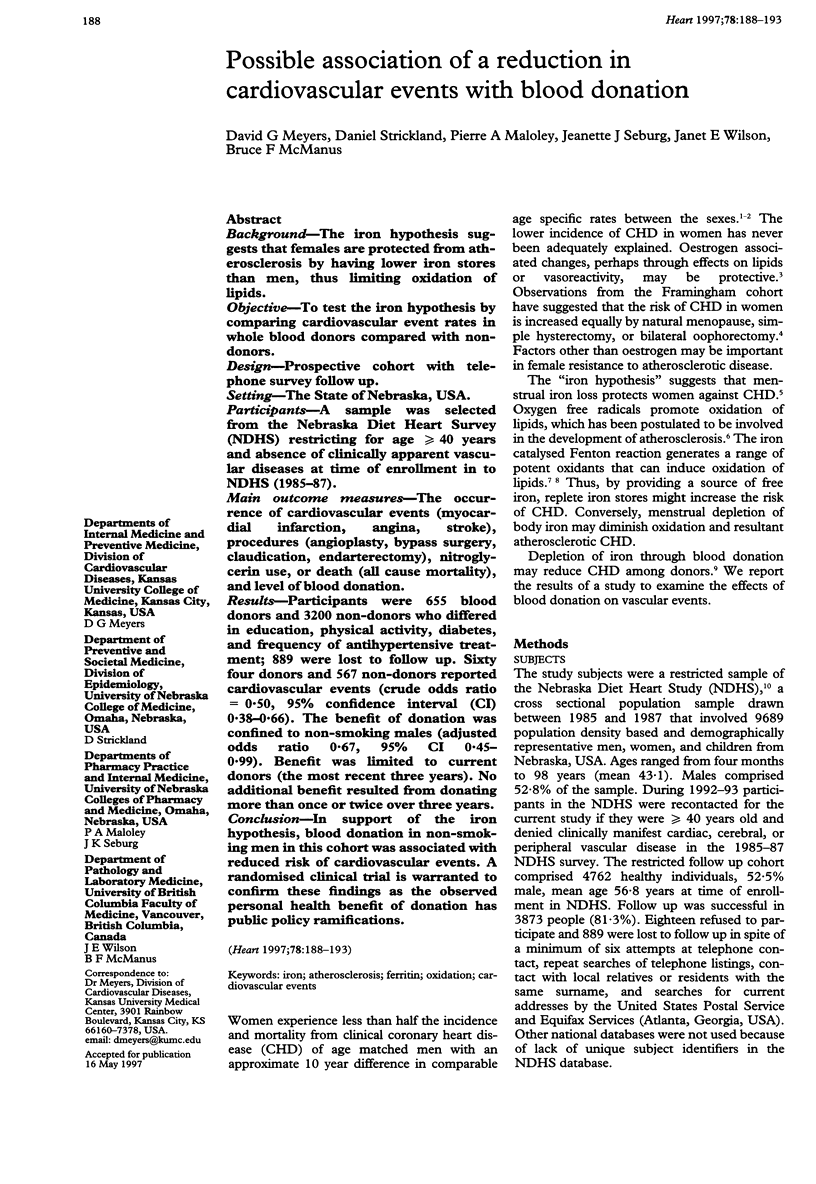
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bates E. R., Califf R. M., Stack R. S., Aronson L., George B. S., Candela R. J., Kereiakes D. J., Abbottsmith C. W., Anderson L., Pitt B. Thrombolysis and Angioplasty in Myocardial Infarction (TAMI-1) trial: influence of infarct location on arterial patency, left ventricular function and mortality. J Am Coll Cardiol. 1989 Jan;13(1):12–18. doi: 10.1016/0735-1097(89)90542-1. [DOI] [PubMed] [Google Scholar]
- Casale G., Bignamini M., de Nicola P. Does blood donation prolong life expectancy? Vox Sang. 1983;45(5):398–399. doi: 10.1111/j.1423-0410.1983.tb01935.x. [DOI] [PubMed] [Google Scholar]
- Cook J. D., Lipschitz D. A., Miles L. E., Finch C. A. Serum ferritin as a measure of iron stores in normal subjects. Am J Clin Nutr. 1974 Jul;27(7):681–687. doi: 10.1093/ajcn/27.7.681. [DOI] [PubMed] [Google Scholar]
- Cook J. D., Skikne B. S. Intestinal regulation of body iron. Blood Rev. 1987 Dec;1(4):267–272. doi: 10.1016/0268-960x(87)90028-2. [DOI] [PubMed] [Google Scholar]
- Davis J. W., Shelton L., Eigenberg D. A., Hignite C. E., Watanabe I. S. Effects of tobacco and non-tobacco cigarette smoking on endothelium and platelets. Clin Pharmacol Ther. 1985 May;37(5):529–533. doi: 10.1038/clpt.1985.83. [DOI] [PubMed] [Google Scholar]
- Finch C. A., Cook J. D., Labbe R. F., Culala M. Effect of blood donation on iron stores as evaluated by serum ferritin. Blood. 1977 Sep;50(3):441–447. [PubMed] [Google Scholar]
- Fuhrman B., Oiknine J., Aviram M. Iron induces lipid peroxidation in cultured macrophages, increases their ability to oxidatively modify LDL, and affects their secretory properties. Atherosclerosis. 1994 Nov;111(1):65–78. doi: 10.1016/0021-9150(94)90192-9. [DOI] [PubMed] [Google Scholar]
- Garry P. J., Koehler K. M., Simon T. L. Iron stores and iron absorption: effects of repeated blood donations. Am J Clin Nutr. 1995 Sep;62(3):611–620. doi: 10.1093/ajcn/62.3.611. [DOI] [PubMed] [Google Scholar]
- Goodwin J. F. Spectrophotometry of proline in plasma and urine. Clin Chem. 1972 May;18(5):449–453. [PubMed] [Google Scholar]
- Jacobs P., Wood L., Novitzky N. Intravenous gammaglobulin has no advantages over oral corticosteroids as primary therapy for adults with immune thrombocytopenia: a prospective randomized clinical trial. Am J Med. 1994 Jul;97(1):55–59. doi: 10.1016/0002-9343(94)90048-5. [DOI] [PubMed] [Google Scholar]
- Kannel W. B., Hjortland M. C., McNamara P. M., Gordon T. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med. 1976 Oct;85(4):447–452. doi: 10.7326/0003-4819-85-4-447. [DOI] [PubMed] [Google Scholar]
- Kiechl S., Aichner F., Gerstenbrand F., Egger G., Mair A., Rungger G., Spögler F., Jarosch E., Oberhollenzer F., Willeit J. Body iron stores and presence of carotid atherosclerosis. Results from the Bruneck Study. Arterioscler Thromb. 1994 Oct;14(10):1625–1630. doi: 10.1161/01.atv.14.10.1625. [DOI] [PubMed] [Google Scholar]
- Koster J. F., Sluiter W. Is increased tissue ferritin a risk factor for atherosclerosis and ischaemic heart disease? Br Heart J. 1995 Mar;73(3):208–208. doi: 10.1136/hrt.73.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauffer R. B. Iron stores and the international variation in mortality from coronary artery disease. Med Hypotheses. 1991 Jun;35(2):96–102. doi: 10.1016/0306-9877(91)90030-3. [DOI] [PubMed] [Google Scholar]
- Ledue T. B., Craig W. J., Ritchie R. F., Haddow J. E. Influence of blood donation and iron supplementation on indicators of iron status. Clin Chem. 1994 Jul;40(7 Pt 1):1345–1346. [PubMed] [Google Scholar]
- Lerner D. J., Kannel W. B. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986 Feb;111(2):383–390. doi: 10.1016/0002-8703(86)90155-9. [DOI] [PubMed] [Google Scholar]
- Liao Y., Cooper R. S., McGee D. L. Iron status and coronary heart disease: negative findings from the NHANES I epidemiologic follow-up study. Am J Epidemiol. 1994 Apr 1;139(7):704–712. doi: 10.1093/oxfordjournals.aje.a117060. [DOI] [PubMed] [Google Scholar]
- Miller M., Hutchins G. M. Hemochromatosis, multiorgan hemosiderosis, and coronary artery disease. JAMA. 1994 Jul 20;272(3):231–233. [PubMed] [Google Scholar]
- Moore M., Folsom A. R., Barnes R. W., Eckfeldt J. H. No association between serum ferritin and asymptomatic carotid atherosclerosis. The Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol. 1995 Apr 15;141(8):719–723. doi: 10.1093/oxfordjournals.aje.a117493. [DOI] [PubMed] [Google Scholar]
- Morrison H. I., Semenciw R. M., Mao Y., Wigle D. T. Serum iron and risk of fatal acute myocardial infarction. Epidemiology. 1994 Mar;5(2):243–246. doi: 10.1097/00001648-199403000-00015. [DOI] [PubMed] [Google Scholar]
- Pedersen N. S., Morling N. Iron stores in blood donors evaluated by serum ferritin. Scand J Haematol. 1978 Jan;20(1):70–76. doi: 10.1111/j.1600-0609.1978.tb01556.x. [DOI] [PubMed] [Google Scholar]
- Reddy B. R., Kloner R. A., Przyklenk K. Early treatment with deferoxamine limits myocardial ischemic/reperfusion injury. Free Radic Biol Med. 1989;7(1):45–52. doi: 10.1016/0891-5849(89)90099-3. [DOI] [PubMed] [Google Scholar]
- Regnström J., Tornvall P., Kallner A., Nilsson J., Hamsten A. Stored iron levels and myocardial infarction at young age. Atherosclerosis. 1994 Mar;106(1):123–125. doi: 10.1016/0021-9150(94)90089-2. [DOI] [PubMed] [Google Scholar]
- Reunanen A., Takkunen H., Knekt P., Seppänen R., Aromaa A. Body iron stores, dietary iron intake and coronary heart disease mortality. J Intern Med. 1995 Sep;238(3):223–230. doi: 10.1111/j.1365-2796.1995.tb00926.x. [DOI] [PubMed] [Google Scholar]
- Rimm E. B., Stampfer M. J., Ascherio A., Giovannucci E., Colditz G. A., Willett W. C. Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med. 1993 May 20;328(20):1450–1456. doi: 10.1056/NEJM199305203282004. [DOI] [PubMed] [Google Scholar]
- Rosamond W. D., Sprafka J. M., McGovern P. G., Nelson M., Luepker R. V. Validation of self-reported history of acute myocardial infarction: experience of the Minnesota Heart Survey Registry. Epidemiology. 1995 Jan;6(1):67–69. doi: 10.1097/00001648-199501000-00013. [DOI] [PubMed] [Google Scholar]
- Salonen J. T., Korpela H., Nyyssönen K., Porkkala E., Tuomainen T. P., Belcher J. D., Jacobs D. R., Jr, Salonen R. Lowering of body iron stores by blood letting and oxidation resistance of serum lipoproteins: a randomized cross-over trial in male smokers. J Intern Med. 1995 Feb;237(2):161–168. doi: 10.1111/j.1365-2796.1995.tb01156.x. [DOI] [PubMed] [Google Scholar]
- Salonen J. T., Nyyssönen K., Korpela H., Tuomilehto J., Seppänen R., Salonen R. High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation. 1992 Sep;86(3):803–811. doi: 10.1161/01.cir.86.3.803. [DOI] [PubMed] [Google Scholar]
- Shewmon D. A. Lipids, atherosclerosis, and the postmenopausal woman. A clinical perspective. Obstet Gynecol Clin North Am. 1994 Jun;21(2):337–355. [PubMed] [Google Scholar]
- Smith C., Mitchinson M. J., Aruoma O. I., Halliwell B. Stimulation of lipid peroxidation and hydroxyl-radical generation by the contents of human atherosclerotic lesions. Biochem J. 1992 Sep 15;286(Pt 3):901–905. doi: 10.1042/bj2860901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solymoss B. C., Marcil M., Gilfix B. M., Gelinas F., Poitras A. M., Campeau L. The place of ferritin among risk factors associated with coronary artery disease. Coron Artery Dis. 1994 Mar;5(3):231–235. doi: 10.1097/00019501-199403000-00008. [DOI] [PubMed] [Google Scholar]
- Steinberg D., Parthasarathy S., Carew T. E., Khoo J. C., Witztum J. L. Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med. 1989 Apr 6;320(14):915–924. doi: 10.1056/NEJM198904063201407. [DOI] [PubMed] [Google Scholar]
- Sullivan J. L. Blood donation may be good for the donor. Iron, heart disease, and donor recruitment. Vox Sang. 1991;61(3):161–164. doi: 10.1111/j.1423-0410.1991.tb00940.x. [DOI] [PubMed] [Google Scholar]
- Sullivan J. L. Iron and the sex difference in heart disease risk. Lancet. 1981 Jun 13;1(8233):1293–1294. doi: 10.1016/s0140-6736(81)92463-6. [DOI] [PubMed] [Google Scholar]
- Tuomainen T. P., Salonen R., Nyyssönen K., Salonen J. T. Cohort study of relation between donating blood and risk of myocardial infarction in 2682 men in eastern Finland. BMJ. 1997 Mar 15;314(7083):793–794. doi: 10.1136/bmj.314.7083.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wannamethee G., Perry I. J., Shaper A. G. Haematocrit, hypertension and risk of stroke. J Intern Med. 1994 Feb;235(2):163–168. doi: 10.1111/j.1365-2796.1994.tb01050.x. [DOI] [PubMed] [Google Scholar]
- Wannamethee G., Shaper A. G., Whincup P. H. Ischaemic heart disease: association with haematocrit in the British Regional Heart Study. J Epidemiol Community Health. 1994 Apr;48(2):112–118. doi: 10.1136/jech.48.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R. E., Zweier J. L., Flaherty J. T. Treatment with deferoxamine during ischemia improves functional and metabolic recovery and reduces reperfusion-induced oxygen radical generation in rabbit hearts. Circulation. 1991 Mar;83(3):1006–1014. doi: 10.1161/01.cir.83.3.1006. [DOI] [PubMed] [Google Scholar]
- Wingard D. L., Suarez L., Barrett-Connor E. The sex differential in mortality from all causes and ischemic heart disease. Am J Epidemiol. 1983 Feb;117(2):165–172. doi: 10.1093/oxfordjournals.aje.a113527. [DOI] [PubMed] [Google Scholar]
- van der Kraaij A. M., Mostert L. J., van Eijk H. G., Koster J. F. Iron-load increases the susceptibility of rat hearts to oxygen reperfusion damage. Protection by the antioxidant (+)-cyanidanol-3 and deferoxamine. Circulation. 1988 Aug;78(2):442–449. doi: 10.1161/01.cir.78.2.442. [DOI] [PubMed] [Google Scholar]



